Abstract
Purpose
Studies show that patients with obstructive sleep apnea (OSA) are more likely than the general population to have psychological disorders such as depression. However, it is less clear how OSA treatment affects this association. This meta-analysis aimed to assess whether or not continuous positive airway pressure (CPAP) and mandibular advancement devices (MADs) reduce depression symptoms in patients with OSA.
Methods
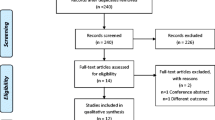
We searched Pubmed, Embase, Web of Science, and Cochrane Library from creating the databases until November 2022. Our analysis included RCTs that examined CPAP and MAD treatment effectiveness for depression in patients with OSA.
Results
We identified 17 CPAP studies comprising 1,931 patients for inclusion in the meta-analysis. The results of the meta-analysis using a fixed effects model found that CPAP improved depressed mood in patients with OSA relative to controls (SMD = 0.27;95% CI:0.18,0.36), with small heterogeneity among trials (I2 = 8.1% < 50%, P = 0.359). We performed subgroup analyses on three factors: the length of trial follow-up, patient adherence data, and depression assessment scales. The meta-analysis also identified six MAD studies involving 315 patients. According to this analysis, there was no heterogeneity between studies (I2 = 0%, P = 0.748). MADs did not significantly improve depression symptoms compared to controls, indicating a combined effect of SMD = 0.07 (95% CI: − 0.15,0.29), P > 0.05.
Conclusion
The present findings confirm that CPAP may improve depressive symptoms in patients with OSA. However, the review results suggest that MADs have no significant effect on depressive symptoms in patients with OSA, a finding that is different from the results of previous meta-analyses.









Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
References
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an american academy of sleep medicine clinical practice guideline. J J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506
Xia F, Sawan M (2021) Clinical and research solutions to manage obstructive sleep apnea: a review. J Sensors (Basel) 21(5). https://doi.org/10.3390/s21051784
Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM et al (2009) Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J J Clin Sleep Med 5(3):263–276
Qaseem A, Dallas P, Owens DK, Starkey M, Holty JE, Shekelle P (2014) Diagnosis of obstructive sleep apnea in adults: a clinical practice guideline from theAmerican College of Physicians. J Ann Intern Med 161(3):210–220. https://doi.org/10.7326/m12-3187
Greenstone M, Hack M (2014) Obstructive sleep apnoea. J Bmj 348:g3745. https://doi.org/10.1136/bmj.g3745
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. J Lancet Respir Med 7(8):687–698. https://doi.org/10.1016/s2213-2600(19)30198-5
Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N, Mehra R, Bozkurt B, Ndumele CE, Somers VK (2021) Obstructive sleep apnea and cardiovascular disease: a scientific statement from the american heart association. J Circulation 144(3):e56–e67. https://doi.org/10.1161/cir.0000000000000988
Reutrakul S, Mokhlesi B (2017) Obstructive sleep apnea and diabetes: a state of the art review. J Chest 152(5):1070–1086. https://doi.org/10.1016/j.chest.2017.05.009
Vaessen TJ, Overeem S, Sitskoorn MM (2015) Cognitive complaints in obstructive sleep apnea. J Sleep Med Rev 19:51–58. https://doi.org/10.1016/j.smrv.2014.03.008
Appleton SL, Vakulin A, McEvoy RD, Vincent A, Martin SA, Grant JF, Taylor AW, Antic NA, Catcheside PG, Wittert GA et al (2015) Undiagnosed obstructive sleep apnea is independently associated with reductions in quality of life in middle-aged, but not elderly men of a population cohort. J Sleep Breath 19(4):1309–1316. https://doi.org/10.1007/s11325-015-1171-5
Gupta MA, Simpson FC (2015) Obstructive sleep apnea and psychiatric disorders: a systematic review. J J Clin Sleep Med 11(2):165–175. https://doi.org/10.5664/jcsm.4466
McCarron RM, Shapiro B, Rawles J, Luo J (2021) Depression. J Ann Intern Med 174(5):ITC65–ITC80. https://doi.org/10.7326/AITC202105180
Wang J, Wu X, Lai W, Long E, Zhang X, Li W, Zhu Y, Chen C, Zhong X, Liu Z et al (2017) Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. J BMJ Open 7(8):e017173. https://doi.org/10.1136/bmjopen-2017-017173
Malhi GS, Mann JJ (2018) Depression. J Lancet 392(10161):2299–2312. https://doi.org/10.1016/S0140-6736(18)31948-2
Garbarino S, Bardwell WA, Guglielmi O, Chiorri C, Bonanni E, Magnavita N (2020) Association of Anxiety and Depression in Obstructive Sleep Apnea Patients: A Systematic Review and Meta-Analysis. J Behav Sleep Med 18(1):35–57. https://doi.org/10.1080/15402002.2018.1545649
Kerner NA, Roose SP (2016) Obstructive Sleep Apnea is Linked to Depression and Cognitive Impairment: Evidence and Potential Mechanisms. J Am J Geriatr Psychiatry 24(6):496–508. https://doi.org/10.1016/j.jagp.2016.01.134
Penninx BW, Milaneschi Y, Lamers F, Vogelzangs N (2013) Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. J BMC Med 11:129. https://doi.org/10.1186/1741-7015-11-129
Semelka M, Wilson J, Floyd R (2016) Diagnosis and treatment of obstructive sleep apnea in adults. J Am Fam Phys 94(5):355–360
Giles TL, Lasserson TJ, Smith B, White J, Wright JJ, Cates CJ (2006) Continuous positive airways pressure for obstructive sleep apnoea in adults. J Cochrane Database Syst Rev (3). https://doi.org/10.1002/14651858.CD001106.pub3
Redline S, Adams N, Strauss ME, Roebuck T, Winters M, Rosenberg C (1998) Improvement of mild sleep-disordered breathing with CPAP compared with conservative therapy. J Am J Respir Crit Care Med 157(3 Pt 1):858–865. https://doi.org/10.1164/ajrccm.157.3.9709042
Engleman HM, Cheshire KE, Deary IJ, Douglas NJ (1993) Daytime sleepiness, cognitive performance and mood after continuous positive airway pressure for the sleep apnoea/hypopnoea syndrome [Journal article]. J Thorax 48(9):911–914
Povitz M, Bolo CE, Heitman SJ, Tsai WH, Wang J, James MT (2014) Effect of treatment of obstructive sleep apnea on depressive symptoms: systematic review and meta-analysis. J PLoS Med 11(11):e1001762. https://doi.org/10.1371/journal.pmed.1001762
Yang X, Yang J, Yang C, Niu L, Song F, Wang L (2020) Continuous positive airway pressure can improve depression in patients with obstructive sleep apnoea syndrome: a meta-analysis based on randomized controlled trials. J J Int Med Res 48(3):300060519895096. https://doi.org/10.1177/0300060519895096
Mok Y, Melehan KL, Phillips CL, Yee BJ, Miller C, Grunstein RR, Bartlett D, Liu PY, Wong KK, Hoyos CM (2020) Does CPAP treat depressive symptoms in individuals with OSA? An analysis of two 12-week randomized sham CPAP-controlled trials. J Sleep Med 73:11–14. https://doi.org/10.1016/j.sleep.2020.04.021
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, Chervin RD (2015) Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J J Clin Sleep Med 11(7):773–827. https://doi.org/10.5664/jcsm.4858
Mickelson SA (2020) Oral Appliances for Snoring and Obstructive Sleep Apnea. J Otolaryngol Clin North Am 53(3):397–407. https://doi.org/10.1016/j.otc.2020.02.004
Naismith SL, Winter VR, Hickie IB, Cistulli PA (2005) Effect of oral appliance therapy on neurobehavioral functioning in obstructive sleep apnea: a randomized controlled trial. J J Clin Sleep Med 1(4):374–380
Barnes M, McEvoy RD, Banks S, Tarquinio N, Murray CG, Vowles N, Pierce RJ (2004) Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. J Am J Respir Crit Care Med 170(6):656–664. https://doi.org/10.1164/rccm.200311-1571OC
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Bmj 372:n71. https://doi.org/10.1136/bmj.n71
Saunamaki T, Jehkonen M (2007) Depression and anxiety in obstructive sleep apnea syndrome: a review. J Acta Neurol Scand 116(5):277–288. https://doi.org/10.1111/j.1600-0404.2007.00901.x
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. J Med Care 30(6):473–483
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2019) Cochrane handbook for systematic reviews of interventions, 2nd edn. John Wiley & Sons, Chichester
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D et al (2004) Grading quality of evidence and strength of recommendations. J Bmj 328(7454):1490. https://doi.org/10.1136/bmj.328.7454.1490
Engleman HM, Martin SE, Deary IJ, Douglas NJ (1997) Effect of CPAP therapy on daytime function in patients with mild sleep apnoea/hypopnoea syndrome [Article]. J Thorax 52(2):114–119. https://doi.org/10.1136/thx.52.2.114
Marshall NS, Neill AM, Campbell AJ, Sheppard DS (2005) Randomised controlled crossover trial of humidified continuous positive airway pressure in mild obstructive sleep apnoea. J Thorax 60(5):427–432. https://doi.org/10.1136/thx.2004.032078
Barnes M, Houston D, Worsnop CJ, Neill AM, Mykytyn IJ, Amanda KAY, Trinder J, Saunders NA, Douglas Mcevoy R, Pierce RJ (2002) A randomized controlled trial of continuous positive airway pressure in mild obstructive sleep apnea [Article]. J Am J Respir Crit Care Med 165(6):773–780. https://doi.org/10.1164/ajrccm.165.6.2003166
Antic NA, Catcheside P, Buchan C, Hensley M, Naughton MT, Rowland S, Williamson B, Windler S, McEvoy RD (2011) The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. J Sleep 34(1):111–119. https://doi.org/10.1093/sleep/34.1.111
Aarab G, Lobbezoo F, Hamburger HL, Naeije M (2011) Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnea: a randomized, placebo-controlled trial. J Respiration 81(5):411–419. https://doi.org/10.1159/000319595
Batool-Anwar S, Goodwin JL, Kushida CA, Walsh JA, Simon RD, Nichols DA (2016) Impact of continuous positive airway pressure (CPAP) on quality of life in patients with obstructive sleep apnea (OSA) [Journal article]. J J Sleep Res 25(6):731–738
Jenkinson C, Davies RJO, Mullins R, Stradling JR (1999) Comparison of therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: A randomised prospective parallel trial [Article]. J Lancet 353(9170):2100–2105. https://doi.org/10.1016/S0140-6736(98)10532-9
Yu BH, Ancoli-Israel S, Dimsdale JE (1999) Effect of CPAP treatment on mood states in patients with sleep apnea. J J Psychiatr Res 33(5):427–432. https://doi.org/10.1016/s0022-3956(99)00020-5
Montserrat JM, Ferrer M, Hernandez L, Farré R, Vilagut G, Navajas D, Badia JR, Carrasco E, De Pablo J, Ballester E (2001) Effectiveness of CPAP treatment in daytime function in sleep apnea syndrome: a randomized controlled study with an optimized placebo. J Am J Respir Crit Care Med 164(4):608–613. https://doi.org/10.1164/ajrccm.164.4.2006034
Blanco J, Zamarrón C, Abeleira Pazos MT, Lamela C, Suarez Quintanilla D (2005) Prospective evaluation of an oral appliance in the treatment of obstructive sleep apnea syndrome. J Sleep Breath 9(1):20–25. https://doi.org/10.1007/s11325-005-0003-4
Bardwell WA, Norman D, Ancoli-Israel S, Loredo JS, Lowery A, Lim W, Dimsdale JE (2007) Effects of 2-week nocturnal oxygen supplementation and continuous positive airway pressure treatment on psychological symptoms in patients with obstructive sleep apnea: a randomized placebo-controlled study. J Behav Sleep Med 5(1):21–38. https://doi.org/10.1207/s15402010bsm0501_2
Haensel A, Norman D, Natarajan L, Bardwell WA, Ancoli-Israel S, Dimsdale JE (2007) Effect of a 2 week CPAP treatment on mood states in patients with obstructive sleep apnea: a double-blind trial. J Sleep Breath 11(4):239–244. https://doi.org/10.1007/s11325-007-0115-0
Lam B, Sam K, Mok WY, Cheung MT, Fong DY, Lam JC, Lam DC, Yam LY, Ip MS (2007) Randomised study of three non-surgical treatments in mild to moderate obstructive sleep apnoea. J Thorax 62(4):354–359. https://doi.org/10.1136/thx.2006.063644
Petri N, Svanholt P, Wildschiodtz G, Winkel P (2008) Mandibular advancement appliance for obstructive sleep apnoea: results of a randomised placebo controlled trial using parallel group design. J J Sleep Res 17:157–157
Siccoli MM, Pepperell JC, Kohler M, Craig SE, Davies RJ, Stradling JR (2008) Effects of continuous positive airway pressure on quality of life in patients with moderate to severe obstructive sleep apnea: data from a randomized controlled trial. J Sleep 31(11):1551–1558. https://doi.org/10.1093/sleep/31.11.1551
Craig SE, Kohler M, Nicoll D, Bratton DJ, Nunn A, Davies R, Stradling J (2012) Continuous positive airway pressure improves sleepiness but not calculated vascular risk in patients with minimally symptomatic obstructive sleep apnoea: the MOSAIC randomised controlled trial. J Thorax 67(12):1090–1096. https://doi.org/10.1136/thoraxjnl-2012-202178
Lee IS, Bardwell W, Ancoli-Israel S, Loredo JS, Dimsdale JE (2012) Effect of three weeks of continuous positive airway pressure treatment on mood in patients with obstructive sleep apnoea: a randomized placebo-controlled study. J Sleep Med 13(2):161–166. https://doi.org/10.1016/j.sleep.2011.09.005
Diaferia G, Badke L, Santos-Silva R, Bommarito S, Tufik S, Bittencourt L (2013) Effect of speech therapy as adjunct treatment to continuous positive airway pressure on the quality of life of patients with obstructive sleep apnea. J Sleep Med 14(7):628–635. https://doi.org/10.1016/j.sleep.2013.03.016
McMillan A, Bratton DJ, Faria R, Laskawiec-Szkonter M, Griffin S, Davies RJ, Nunn AJ, Stradling JR, Riha RL, Morrell MJ (2014) Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. J Lancet Respir Med 2(10):804–812. https://doi.org/10.1016/s2213-2600(14)70172-9
Dalmases M, Solé-Padullés C, Torres M, Embid C, Nuñez MD, Martínez-Garcia M, Farré R, Bargalló N, Bartrés-Faz D, Montserrat JM (2015) Effect of CPAP on Cognition, Brain Function, and Structure Among Elderly Patients With OSA: A Randomized Pilot Study. J Chest 148(5):1214–1223. https://doi.org/10.1378/chest.15-0171
Marklund M, Carlberg B, Forsgren L, Olsson T, Stenlund H, Franklin KA (2015) Oral Appliance Therapy in Patients With Daytime Sleepiness and Snoring or Mild to Moderate Sleep Apnea: A Randomized Clinical Trial. J JAMA Intern Med 175(8):1278–1285. https://doi.org/10.1001/jamainternmed.2015.2051
Martínez-García M, Chiner E, Hernández L, Cortes JP, Catalán P, Ponce S, Diaz JR, Pastor E, Vigil L, Carmona C et al (2015) Obstructive sleep apnoea in the elderly: role of continuous positive airway pressure treatment [Journal Article; Clinical Trial Protocol]. J Eur Respir J 46(1):142–151. https://doi.org/10.1183/09031936.00064214
Aarab G, Nikolopoulou M, Ahlberg J, Heymans MW, Hamburger HL, de Lange J, Lobbezoo F (2017) Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnea: a randomized, placebo-controlled trial on psychological distress. J Clin Oral Investig 21(7):2371–2378. https://doi.org/10.1007/s00784-016-2045-3
Ponce S, Pastor E, Orosa B, Oscullo G, Catalan P, Martinez A, Hernandez L, Muriel A, Chiner E, Martinez-Garcia MA et al (2019) The role of CPAP treatment in elderly patients with moderate obstructive sleep apnoea: a multicentre randomised controlled trial. J Eur Respir J 54(2):Article 1900518. https://doi.org/10.1183/13993003.00518-2019
Wimms AJ, Kelly JL, Turnbull CD, McMillan A, Craig SE, O’Reilly JF, Nickol AH, Hedley EL, Decker MD, Willes LA et al (2020) Continuous positive airway pressure versus standard care for the treatment of people with mild obstructive sleep apnoea (MERGE): a multicentre, randomised controlled trial [Journal Article; Clinical Trial Protocol]. J Lancet Respir Med 8(4):349–358. https://doi.org/10.1016/S2213-2600(19)30402-3
Luz GP, Badke L, Nery LE, Silva LO, Guimaraes TM, Coelho G, Millani A, Alves RG, Kase C, Tufik S et al (2022) Effect of CPAP vs. mandibular advancement device for excessive daytime sleepiness, fatigue, mood, sustained attention, and quality of life in patients with mild OSA [Journal article]. J Sleep Breath. https://doi.org/10.1007/s11325-022-02694-z
Gupta MA, Simpson FC, Lyons DC (2016) The effect of treating obstructive sleep apnea with positive airway pressure on depression and other subjective symptoms: a systematic review and meta-analysis. J Sleep Med Rev 28:55–68. https://doi.org/10.1016/j.smrv.2015.07.002
Funding
This work was supported by the Natural Science Foundation of Gansu Province (21JR1RA074).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Registration
This meta-analysis has been registered with PROSPERO, registration number CRD42022377501.
What is known
1. CPAP and MADs can improve many symptoms and disease severity in patients with OSA.
What is new
1. CPAP can reduce depressive symptoms in OSA patients, and MADs cannot significantly improve depressed mood in OSA patients.
2. When the duration of CPAP intervention was between 4 and 8 weeks and when used CPAP over 4 h per night, depressive symptoms in patients with OSA improved more markedly.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, W., Li, L., Zhang, S. et al. Effects of CPAP and Mandibular Advancement Devices on depressive symptoms in patients with obstructive sleep apnea: a meta-analysis of randomized controlled trials. Sleep Breath 27, 2123–2137 (2023). https://doi.org/10.1007/s11325-023-02829-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02829-w