Abstract
Purpose
Obstructive sleep apnea (OSA) is now highly prevalent but largely undiagnosed. Quality of life is an indicator of both the impact of undiagnosed OSA and the need for strategies to increase OSA diagnosis. We determined age-related impacts of undiagnosed OSA on health-related quality of life (HRQL) and whether this was independent of sleepiness and comorbidities.
Methods
In 2010–2012, 837 participants from the Men Androgen Inflammation Lifestyle Environment and Stress Study (population cohort n = 1869, ≥40 years, Adelaide, Australia), without a prior OSA diagnosis underwent full in-home polysomnography (Embletta X100) and completed the Epworth Sleepiness Scale and SF-36 questionnaire. The effects of the apnea-hypopnea index (AHI) on SF-36 physical (PCS) and mental (MCS) component summary scores and standardized SF-36 scale z-scores were estimated using multiple linear regression adjusted for major comorbidities and sleepiness, stratified by age.
Results
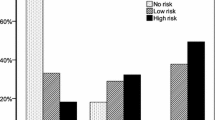
Men ≤69 years demonstrated significant (p < 0.05) decrements/event increase in AHI in PCS score [unstandardized B coefficient (SE) = −0.068 (0.023)], physical functioning, role physical, general health, and vitality z-scores in fully adjusted models. Severe OSA (AHI ≥30) was associated with significant reductions in PCS [B = −4.1 (1.1)] and MCS score [B = −3.6 (1.2)] independent of sleepiness and comorbidities which were attenuated but persisted in men <69 years without depression. In men aged ≥70 years, statistically significant AHI-associated impairments were generally not seen.
Conclusions
Undiagnosed OSA was a major independent contributor to HRQL impairments in men <69 years. Improved strategies to identify undiagnosed OSA are indicated that may require a reduced focus on daytime sleepiness.

Similar content being viewed by others
References
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–14
Ward KL, Hillman DR, James A, Bremner AP, Simpson L, Cooper MN, Palmer LJ, Fedson AC, Mukherjee S (2013) Excessive daytime sleepiness increases the risk of motor vehicle crash in obstructive sleep apnea. J Clin Sleep Med 9(10):1013–21
Baldwin CM, Griffith KA, Nieto FJ, O’Connor GT, Walsleben JA, Redline S (2001) The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep 24(1):96–105
Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ (2006) Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 3, CD001106
Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A (2005) Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab 90(8):4510–5
Kapur V, Strohl KP, Redline S, Iber C, O’Connor G, Nieto J (2002) Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath 6(2):49–54
Kendzerska T, Mollayeva T, Gershon AS, Leung RS, Hawker G, Tomlinson G (2014) Untreated obstructive sleep apnea and the risk for serious long-term adverse outcomes: a systematic review. Sleep Med Rev 18(1):49–59
Centers for Disease Control and Prevention. Health-Related Quality of Life (HRQOL) Concepts. http://www.cdc.gov/hrqol/concept.htm Accessed 29 Sep 2014
U.S. Department of Health and Human Services. Healthy People 2020. Healthy People 2020 Framework. The Vision, Mission, and Goals of Healthy People 2020. Overarching Goals. http://www.healthypeople.gov/sites/default/files/HP2020Framework.pdf. Accessed 29 Sep 2014
Moyer CA, Sonnad SS, Garetz SL, Helman JI, Chervin RD (2001) Quality of life in obstructive sleep apnea: a systematic review of the literature. Sleep Med 2(6):477–91
Finn L, Young T, Palta M, Fryback DG (1998) Sleep-disordered breathing and self-reported general health status in the Wisconsin Sleep Cohort Study. Sleep 21(7):701–6
Baldwin CM, Ervin AM, Mays MZ, Robbins J, Shafazand S, Walsleben J, Weaver T (2010) Sleep disturbances, quality of life, and ethnicity: the Sleep Heart Health Study. J Clin Sleep Med 6(2):176–83
Silva GE, An MW, Goodwin JL, Shahar E, Redline S, Resnick H, Baldwin CM, Quan SF (2009) Longitudinal evaluation of sleep-disordered breathing and sleep symptoms with change in quality of life: the Sleep Heart Health Study (SHHS). Sleep 32(8):1049–57
Khan A, Harrison SL, Kezirian EJ, Ancoli-Israel S, O’Hearn D, Orwoll E, Redline S, Ensrud K, Stone KL, Osteoporotic Fractures in Men Study Research Group (2013) Obstructive sleep apnea during rapid eye movement sleep, daytime sleepiness, and quality of life in older men in osteoporotic fractures in men (MrOS) sleep study. J Clin Sleep Med 9(3):191–8
Martinez-Garcia MA, Soler-Cataluna JJ, Roman-Sanchez P, Gonzalez V, Amoros C, Montserrat JM (2009) Obstructive sleep apnea has little impact on quality of life in the elderly. Sleep Med 10(1):104–11
Launois SH, Pepin JL, Levy P (2007) Sleep apnea in the elderly: a specific entity? Sleep Med Rev 11(2):87–97
Lavie L, Lavie P (2006) Ischemic preconditioning as a possible explanation for the age decline relative mortality in sleep apnea. Med Hypotheses 66(6):1069–73
Lavie P, Lavie L (2009) Unexpected survival advantage in elderly people with moderate sleep apnoea. J Sleep Res 18(4):397–403
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O’Connor GT, Rapoport DM, Redline S, Resnick HE, Robbins JA, Shahar E, Unruh ML, Samet JM (2009) Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 6(8), e1000132
Grant JF, Martin SA, Taylor AW, Wilson DH, Araujo A, Adams RJ, Jenkins A, Milne RW, Hugo GJ, Atlantis E, Wittert GA (2014) Cohort profile: the Men Androgen Inflammation Lifestyle Environment and Stress (MAILES) Study. Int J Epidemiol 43:1040–53
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–5
Iber C, Ancoli Israel S, Chesson Jr A, Quan S (2007) The AASM manual for the scoring of sleep and associated events. Westchester, IL: Am Acad Sleep Med
Ruehland WR, Rochford PD, O’Donoghue FJ, Pierce RJ, Singh P, Thornton AT (2009) The new AASM criteria for scoring hypopneas: impact on the apnea hypopnea index. Sleep 32(2):150–7
Ware J, Kosinski M, Keller S (1994) SF-36 physical and mental health summary scales: a users’ manual. The Health Institute, Boston
Kazis LE, Anderson JJ, Meenan RF (1989) Effect sizes for interpreting changes in health status. Med Care 27(3 Suppl):S178–89
Peppard PE, Szklo-Coxe M, Hla KM, Young T (2006) Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med 166(16):1709–15
Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA, Young T, Pickering TG (2005) Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation 111(5):614–21
Jennum P, Ibsen R, Kjellberg J (2014) Social consequences of sleep disordered breathing on patients and their partners: a controlled national study. Eur Respir J 43(1):134–44
Craig SE, Kohler M, Nicoll D, Bratton DJ, Nunn A, Davies R, Stradling J (2012) Continuous positive airway pressure improves sleepiness but not calculated vascular risk in patients with minimally symptomatic obstructive sleep apnoea: the MOSAIC randomised controlled trial. Thorax 67(12):1090–6
Gagnadoux F, le Vaillant M, Paris A, Pigeanne T, Chollet S, Masson P, Bizieux-Thaminy A, Humeau M-P, Meslier N, The IRSR sleep cohort group (2013) Adherence to positive airway pressure in non-sleepy patients with obstructive sleep apnoea. Eur Respir J 42(3):863–66
Antic NA, Catcheside P, Buchan C, Hensley M, Naughton MT, Rowland S, Williamson B, Windler S, McEvoy RD (2011) The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep 34(1):111–9
Funding
National Health and Medical Research Council of Australia grant number 627227; The Resmed Foundation, CA, USA. Embla Systems, CO, contributed a number of Embletta X100 devices for the duration of the study.
Conflict of interest
RA has received research funding from the National Health and Medical Research Council of Australia, and the ResMed Foundation, and nonfinancial support from Embla Systems, CO.
AV has received research funding from the National Health and Medical Research Council of Australia.
RDM has received research funding from the National Health and Medical Research Council of Australia, the ResMed Foundation, Philips Respironics, and Fisher and Paykel, equipment donations from ResMed, Philips Respironics and SomnoMed, and lecture fees from Philips Respironics.
NA has received research funding from the National Health and Medical Research Council of Australia, Philips Respironics, and Fisher and Paykel, equipment donations from ResMed, Philips Respironics and SomnoMed, and lecture fees and payment for development of educational presentations from ResMed.
PC has received research funding from the National Health and Medical Research Council of Australia, and the Australian Research Council, equipment support from Philips Respironics and AirLiquide Healthcare.
AT has received research funding from the National Health and Medical Research Council of Australia.
GW has received research funding from the National Health and Medical Research Council of Australia and the ResMed Foundation, and non-financial support from Embla Systems, Colorado.
SM, JG, and SA have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 51 kb)
Rights and permissions
About this article
Cite this article
Appleton, S.L., Vakulin, A., McEvoy, R.D. et al. Undiagnosed obstructive sleep apnea is independently associated with reductions in quality of life in middle-aged, but not elderly men of a population cohort. Sleep Breath 19, 1309–1316 (2015). https://doi.org/10.1007/s11325-015-1171-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1171-5