Abstract
Objectives
To explore the prevalence of obstructive sleep apnea (OSA) and the association between the adenoma granulation patterns and OSA in patients with acromegaly.
Methods
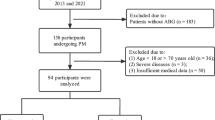
An overnight polysomnography (PSG) assessment was carried out on participants with acromegaly. Results classified participants into a non-OSA group, mild to moderate OSA group, and severe OSA group. Morphological and biochemical analyses were performed. Demographic, clinical, biochemical, and polysomnographic data were compared among the three groups. Using logistic regression models, the risk of OSA in acromegalic subjects was estimated.
Results
OSA was reported in 36 of 49 patients (74%) with acromegaly. Contrasted with the non-OSA group, OSA patients had a larger proportion of the densely granulated (DG) pattern. The OSA groups with DG acromegaly had a smaller maximum tumor diameter and Vol/2 than those with the sparsely granulated (SG) pattern. Furthermore, a higher growth hormone (GH) level (45.0 ± 36.9 vs 18.6 ± 15.8, P = 0.047) and GH index (28.4 ± 13.8 vs 6.6 ± 8.2, P = 0.003) were found in DG acromegaly patients with severe OSA. Additionally, there was a trend toward higher standardized insulin-like growth factor 1 (IGF-1) in patients with DG acromegaly than in those with SG acromegaly in the severe OSA group. After adjusting for potential confounding variables, the DG pattern was correlated with the risk of OSA (OR = 14.84, 95%CI 1.36–162.20, P = 0.027) in patients with acromegaly.
Conclusions
The findings indicate that a high prevalence of OSA exists in patients with acromegaly, and the DG pattern may be a risk factor for OSA in acromegaly.

Similar content being viewed by others
References
Melmed S (2006) Acromegaly. N Engl J Med 355(24):2558–2573
Colao A et al (2019) Acromegaly. Nat Rev Dis Primers 5(1):20
Guo X et al (2018) Characteristics of the upper respiratory tract in patients with acromegaly and correlations with obstructive sleep apnoea/hypopnea syndrome. Sleep Med 48:27–34
Rodrigues MP et al (2008) Craniofacial abnormalities, obesity, and hormonal alterations have similar effects in magnitude on the development of nocturnal hypoxemia in patients with acromegaly. J Endocrinol Invest 31(12):1052–1057
Kashine S et al (2012) Characteristics of sleep-disordered breathing in Japanese patients with acromegaly. Endocr J 59(1):31–38
Kaw R et al (2012) Postoperative complications in patients with obstructive sleep apnea. Chest 141(2):436–441
Apnea ASOA (2014) Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology 120(2):268–286
Franklin KA, Lindberg E (2015) Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis 7(8):1311–1322
Vannucci L et al (2013) Assessment of sleep apnea syndrome in treated acromegalic patients and correlation of its severity with clinical and laboratory parameters. J Endocrinol Invest 36(4):237–242
Castellani C et al (2016) Morphological study of upper airways and long-term follow-up of obstructive sleep apnea syndrome in acromegalic patients. Endocrine 51(2):308–316
Davi MV, Giustina A (2012) Sleep apnea in acromegaly: a review on prevalence, pathogenetic aspects and treatment. Expert Rev Endocrinol Metab 7(1):55–62
Wagenmakers MA et al (2015) Three-dimensional facial analysis in acromegaly: a novel tool to quantify craniofacial characteristics after long-term remission. Pituitary 18(1):126–134
Wolters TLC et al (2020) The course of obstructive sleep apnea syndrome in patients with acromegaly during treatment. J Clin Endocrinol Metab 105(1):290–304
Akirov A et al (2019) The clinicopathological spectrum of acromegaly. J Clin Med 8(11):1962
Kiseljak-Vassiliades K et al (2015) Growth hormone tumor histological subtypes predict response to surgical and medical therapy. Endocrine 49(1):231–241
Bakhtiar Y et al (2010) Relationship between cytokeratin staining patterns and clinico-pathological features in somatotropinomae. Eur J Endocrinol 163(4):531–539
Fougner SL et al (2012) Adenoma granulation pattern correlates with clinical variables and effect of somatostatin analogue treatment in a large series of patients with acromegaly. Clin Endocrinol 76(1):96–102
Roemmler J et al (2012) Elevated incidence of sleep apnoea in acromegaly—correlation to disease activity. Sleep Breath 16(4):1247–1253
Guo X et al (2018) The posterior pharyngeal wall thickness is associated with OSAHS in patients with acromegaly and correlates with IGF-1 levels. Endocrine 61(3):526–532
Parolin M et al (2020) Obstructive sleep apnea in acromegaly and the effect of treatment: a systematic review and meta-analysis. J Clin Endocrinol Metab 105(3):dgz116
Katznelson L et al (2014) Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99(11):3933–3951
Zhu H et al (2017) Reference ranges for serum insulin-like growth factor I (IGF-I) in healthy Chinese adults. PLOS ONE 12(10):e0185561
Bonneville JF (2016) Magnetic resonance imaging of pituitary tumors. Front Horm Res 45:97–120
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 14(6):540–545
Berry R, Rita B, Charlene G (2017) AASM scoring manual updates for 2017 (Version 2.4). J Clin Sleep Med 5(13):665–666
Annamalai AK et al (2013) A Comprehensive study of clinical, biochemical, radiological, vascular, cardiac, and sleep parameters in an unselected cohort of patients with acromegaly undergoing presurgical somatostatin receptor ligand therapy. J Clin Endocrinol Metab 98(3):1040–1050
Tsoy UA et al (2015) Clinical features of sleep-related breathing disorders in patients with acromegaly. Ter Arkh 87(4):47
Senaratna CV et al (2017) Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev 34:70–81
Vouzouneraki K et al (2018) Temporal relationship of sleep apnea and acromegaly: a nationwide study. Endocrine 62(2):456–463
Turan O et al (2018) Airway and sleep disorders in patients with acromegaly. Clin Respir J 12(3):1003–1010
Pivonello R et al (2017) Complications of acromegaly: cardiovascular, respiratory and metabolic comorbidities. Pituitary 20(1):46–62
Davi’ MV et al (2008) Sleep apnoea syndrome is highly prevalent in acromegaly and only partially reversible after biochemical control of the disease. Eur J Endocrinol 159(5):533–540
Bruwier A et al (2011) Acromegaly and sleep apnea: Cephalometric evaluations. Ann Endocrinol 72(3):211–217
Chennaoui M, Leger D, Gomez-Merino D (2020) Sleep and the GH/IGF-1 axis: consequences and countermeasures of sleep loss/disorders. Sleep Med Rev 49:101223
Weiss V et al (2000) Prevalence of the sleep apnea syndrome in acromegaly population. J Endocrinol Invest 23(8):515–519
Horvath E, Kovacs K (2006) Pathology of acromegaly. Neuroendocrinology 83(3–4):161–165
Hochban W et al (1999) Obstructive sleep apnoea in acromegaly: the role of craniofacial changes. Eur Respir J 14(1):196
Cadieux RJ et al (1982) Endoscopic findings in sleep apnea associated with acromegaly. J Clin Endocrinol Metab 55(1):18–22
Akkoyunlu ME et al (2013) Does hormonal control obviate positive airway pressure therapy in acromegaly with sleep-disordered breathing? Respir Med 107(11):1803–1809
Wennberg A et al (2019) Sleep disorders and cognitive dysfunction in acromegaly. Endocrine 66(3):634–641
Choi E et al (2016) The severity of sleep disordered breathing induces different decrease in the oxygen saturation during rapid eye movement and non-rapid eye movement sleep. Psychiatry Investig 13(6):652
Sharma SK et al (2007) Obesity, and not obstructive sleep apnea, is responsible for metabolic abnormalities in a cohort with sleep-disordered breathing. Sleep Med 8(1):12–17
Leistner SM et al (2015) Reduced sleep quality and depression associate with decreased quality of life in patients with pituitary adenomas. Eur J Endocrinol 172(6):733–743
Acknowledgements
The authors thank the sleep technologists (Ruirui Yuan, Juan Wen and Xing Yang) at the Sleep Medicine Center, Tangdu Hospital of the Fourth Military Medical University.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
The Tangdu Hospital Ethics Committee approved this study.
Informed consent
All participants signed informed consent forms before enrollment.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xianchao Zhao and Lijun Heng are co-first authors of the article.
Rights and permissions
About this article
Cite this article
Zhao, X., Heng, L., Qu, Y. et al. Densely granulated adenoma pattern is associated with an increased risk of obstructive sleep apnea in patients with acromegaly. Sleep Breath 26, 1381–1387 (2022). https://doi.org/10.1007/s11325-021-02468-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02468-z