Abstract
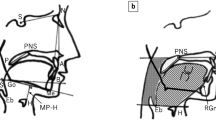
Pathogenesis and long-term outcome of obstructive sleep apnea syndrome (OSAS) in acromegalic patients are still under debate. The aim of the study was to assess the prevalence and long-term follow-up of a series of acromegalic patients with OSAS and to investigate site, degree, and possible causes of upper airway obstruction by morphological study. Cross-sectional and longitudinal study was conducted in 58 acromegalic patients (33 active, 25 controlled) with polysomnography in all subjects, repeated in 25 patients with OSAS, and echocardiography. Morphological study including fiberoptic nasopharyngoscopy with the Müller maneuver (FNMM), magnetic resonance imaging (MRI), with 3-dimensional (3D) elaboration was also performed. The prevalence of OSAS was 58.6 % in the whole series: 63.6 % in the active group and 52 % in the controlled one. Left ventricular hypertrophy was more prevalent in patients with OSAS. OSAS improved in 62.5 % of active patients after achieving hormonal control, whereas it persisted or got worse in 66.6 % of the controlled ones. The uvula and tongue base were the main site of obstruction assessed by FNMM. Uvula diameters obtained by MRI study correlated with the severity of upper airway collapse assessed by FNMM and tongue measure with apnea–hypopnea index (p = 0.044). A greater narrowing and a smaller total volume of upper airways were confirmed by 3D-MRI in patients with more severe OSAS. Uvula and tongue hypertrophy plays a relevant role in the pathogenesis and severity of OSAS. Intensive treatment of acromegaly needs to be promptly adopted in order to reverse it.



Similar content being viewed by others
References
R.R. Grunstein, K.Y. Ho, C.E. Sullivan, Sleep apnea in acromegaly. Ann. Intern. Med. 115, 527–532 (1991)
L.M. Fatti, M. Sacchi, A.I. Pincelli, E. Lavezzi, F. Cavagnini, Prevalence and pathogenesis of sleep apnea and lung disease in acromegaly. Pituitary 4, 259–262 (2001)
V. Weiss, K. Sonka, M. Pretl, S. Dostalova, J. Klozar, P. Kambousek, J. Marek, T. Haas, Prevalence of the sleep apnea syndrome in acromegaly population. J. Endocrinol. Investig. 23, 515–519 (2000)
T. Pekkarinen, M. Partinen, R. Pelkonen, M. Iivanainen, Sleep apnoea and daytime sleepiness in acromegaly: relationship to endocrinological factors. Clin. Endocrinol. 27, 649–654 (1987)
W. Hochban, K. Ehlenz, R. Conradt, U. Brandenburg, Obstructive sleep apnoea in acromegaly: the role of craniofacial changes. Eur. Respir. J. 14, 196–202 (1999)
M.V. Davi’, L. Dalle Carbonare, A. Giustina, M. Ferrari, A. Frigo, V.L. Cascio, G. Francia, Sleep apnoea syndrome is highly prevalent in acromegaly and only partially reversible after biochemical control of the disease. Eur. J. Endocrinol. 159(5), 533–540 (2008)
M.V. Davi’, A. Giustina, Sleep apnea in acromegaly: a review on prevalence, pathogenetic aspects and treatment. Expert Rev. Endocrinol. Metab. 7(1), 55–62 (2012)
P. Attal, P. Chanson, Endocrine aspects of obstructive sleep apnea. J. Clin. Endocrinol. Metab. 95, 483–495 (2010)
F.R. Van Haute, G.F. Taboada, L.L. Corrêa, G.A. Lima, R. Fontes, A.P. Riello, M. Dominaci, M.R. Gadelha, Prevalence of sleep apnea and metabolic abnormalities in patients with acromegaly and analysis of cephalometric parameters by magnetic resonance imaging. Eur. J. Endocrinol. 158, 459–465 (2008)
D. Chemla, P. Attal, L. Maione, A.S. Veyer, G. Mroue, D. Baud, S. Salenave, P. Kamenicky, S. Bobin, P. Chanson, Impact of successful treatment of acromegaly on overnight heart rate variability and sleep apnea. J. Clin. Endocrinol. Metab. 99(8), 2925–2931 (2014)
A. Giustina, F.F. Casanueva, F. Cavagnini, P. Chanson, D. Clemmons, L.A. Frohman, R. Gaillard, K. Ho, P. Jaquet, D.L. Kleinberg, S.W. Lamberts, G. Lombardi, M. Sheppard, C.J. Strasburger, M.L. Vance, J.A. Wass, S. Melmed, Consensus: diagnosis and treatment of acromegaly complications. J. Endocrinol. Investig. 26, 1242–1247 (2003)
A. Colao, D. Ferone, P. Marzullo, G. Lomabardi, Systemic complications of acromegaly: epidemiology, pathogenesis and management. Endocr. Rev. 25, 102–152 (2004)
S.P. Patil, H. Schneider, A.R. Schwartz, P.L. Smith, Adult obstructive sleep apnea: pathophysiology and diagnosis. Chest 132, 325–337 (2007)
J.M. Marin, S.J. Carrizo, E. Vincente, A.G. Agusti, Long-term cardiovascular outcomes in men with obstructive sleep apnea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365, 1046–1053 (2005)
A.S. Shamsuzzaman, B.J. Gersh, V.K. Somers, Obstructive sleep apnea: implications for cardiac and vascular disease. J. Am. Med. Assoc. 290, 1906–1914 (2003)
H.K. Yaggi, J. Concato, W.N. Kerman, J.H. Lichtman, L.M. Brass, V. Mohsenin, Obstructive sleep apnea as a risk factor for stroke and death. N. Engl. J. Med. 353, 2034–2041 (2005)
S. Isono, N. Saeki, A. Tanaka, T. Nishino, Collapsibility of passive pharynx in patients with acromegaly. Am. J. Respir Crit. Care Med. 160, 64–68 (1999)
M.S.M. Ip, K.C.B. Tan, W.C.G. Peh, K.S.L. Lam, Effects of Sandostatin Lar on sleep apnoea in acromegaly: correlation with computerized tomographic cephalometry and hormonal activity. Clin. Endocrinol. 55, 477–483 (2001)
S. Dostalova, K. Sonka, Z. Smahel, V. Weiss, J. Marek, D. Horinek, Craniofacial abnormalities and their relevance for sleep apnoea syndrome aetiopathogenesis in acromegaly. Eur. J. Endocrinol. 144, 491–497 (2001)
B.L. Herrmann, T.E. Wessendorf, W. Ajaj, S. Kahlke, H. Teschler, K. Mann, Effects of octreotide on sleep apnoea and tongue volume (magnetic resonance imaging) in patients with acromegaly. Eur. J. Endocrinol. 151, 309–315 (2004)
American Academy of Sleep Medicine Task Force Report, Sleeprelated breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22, 667–689 (1999)
D.J. Terris, M.M. Hanasono, Y.C. Liu, Reliability of the Muller maneuver and its association with sleep-disordered breathing. Laryngoscope 110(11), 1819–1823 (2000)
F. Rosenow, S. Reuter, U. Deuss, B. Szelies, R.D. Hilgers, W. Winkelmann, W.D. Heiss, Sleep apnoea in treated acromegaly: relative frequency and predisposing factors. Clin. Endocrinol. 45, 563–569 (1996)
L. Sze, C. Schmid, K.E. Bloch, R. Bernays, M. Brandle, Effect of transsphenoidal surgery on sleep apnoea in acromegaly. Eur. J. Endocrinol. 156, 321–329 (2007)
T. Young, J. Skatrud, P.E. Peppard, Risk factors for obstructive sleep apnea in adults. J. Am. Med. Assoc. 291, 2013–2016 (2004)
P.V. Tishler, E.K. Larkin, M.D. Schluchter, S. Redline, Incidence of sleep-disordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep-disordered breathing. J. Am. Med. Assoc. 289, 2230–2237 (2003)
L. Katznelson, Alterations in body composition in acromegaly. Pituitary 12, 136–142 (2009)
G. Tolis, N.G. Angelopoulos, E. Katounda, G. Rombopoulos, V. Kaltzidou, D. Kalt, A. Protonotariou, A. Lytras, Medical treatment of acromegaly: comorbidities and their reversibility by somatostatin analogs. Neuroendocrinology 83, 249–257 (2006)
N.M. Punjabi, V.Y. Polotsky, Disorders of glucose metabolism in sleep apnea. J. Appl. Physiol. 99, 1998–2007 (2005)
C. Rajasoorya, I.M. Holdaway, P. Wrightson, D.J. Scott, H.K. Ibbertson, Determinants of clinical outcome and survival in acromegaly. Clin. Endocrinol. 41, 95–102 (1994)
R. Wolk, V.K. Somers, Cardiovascular consequences of obstructive sleep apnea. Clin. Chest Med. 24, 195–205 (2003)
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Castellani, C., Francia, G., Dalle Carbonare, L. et al. Morphological study of upper airways and long-term follow-up of obstructive sleep apnea syndrome in acromegalic patients. Endocrine 51, 308–316 (2016). https://doi.org/10.1007/s12020-015-0659-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0659-x