Abstract
Cytokines serve important functions in controlling host immunity. Cells involved in the synthesis of these polypeptide mediators have evolved highly regulated processes to ensure that production is carefully balanced. In inflammatory and immune disorders, however, mis-regulation of the production and/or activity of cytokines is recognized as a major contributor to the disease process, and therapeutics that target individual cytokines are providing very effective treatment options in the clinic. Leukocytes are the principle producers of a number of key cytokines, and these cells also express numerous members of the purinergic P2 receptor family. Studies in several cellular systems have provided evidence that P2 receptor modulation can affect cytokine production, and mechanistic features of this regulation have emerged. This review highlights three separate examples corresponding to (1) P2Y6 receptor mediated impact on interleukin (IL)-8 production, (2) P2Y11 receptor-mediated affects on IL-12/23 output, and (3) P2X7 receptor mediated IL-1β posttranslational processing. These examples demonstrate important roles of purinergic receptors in the modulation of cytokine production. Extension of these cellular observations to in vivo situations may lead to new therapeutic strategies for treating cytokine-mediated diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
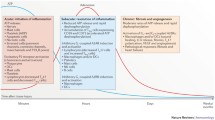
Cytokines comprise a heterogeneous group of polypeptides that mediate a variety of biological responses following their binding to specific receptors on target cells and tissues. Historically, cytokines (including lymphokines) were identified as leukocyte-derived soluble mediators that, when added to other leukocytes and/or to non-leukocyte targets, altered cellular behavior. Today, however, we realize that individual cytokines can be generated by cells of immune as well as non-immune origin, and that these polypeptides orchestrate a complex system of checks and balances controlling host immune and inflammatory processes. Our understanding of the importance that cytokines and cytokine signaling mechanisms serve in host defense mechanisms has been bolstered by the identification of genetic mutations within cytokine and/or cytokine receptor signaling complex genes that profoundly affect pathogen susceptibility [1, 2]. Likewise, genetically engineered mice that lack individual cytokines and/or cytokine receptors have provided a greater understanding of the capabilities possessed by these signaling molecules for promoting inflammatory and autoimmune states [3]. Moreover, the critical importance served by cytokines in mediating inflammation and autoimmunity has been underscored by the recent success of anti-cytokine biologics in the treatment of inflammatory diseases such as rheumatoid arthritis (RA) and Crohn’s disease. For example, agents that neutralize tumor necrosis factor (TNF) α (Enbrel, Remicade and Humira) have dramatically improved the treatment of RA [4–6]. In addition, the natural interleukin (IL)-1 receptor antagonist (Kineret) provides therapeutic benefit to RA patients and is reported to yield remarkable clinical outcomes when administered to patients suffering from a group of rare hereditary autoinflammatory disorders such as Muckle-Wells syndrome [7–9]. Ongoing clinical trials with agents that target IL-12 likewise are showing encouraging efficacy in the treatment of psoriasis and Crohn’s disease [10, 11], and the list of anti-cytokine therapies entering clinical trials grows regularly [6]. Thus, cytokines and the signaling pathways engaged after they bind to receptors on cells represent attractive therapeutic targets for intervention of human autoimmune and inflammatory diseases. Studies over the past decade have suggested that purinergic receptor function, involving both P2Y and P2X family members, can modulate cytokine production and/or activity. This review focuses on several cellular systems where purinergic modulation of cytokine production has been demonstrated and mechanistic explanations have been sought. The cited studies signify that nucleotide receptor-mediated signaling can affect output of several important cytokines. In this context, pharmacological modulation of P2 receptors may represent a new therapeutic modality for treatment of cytokine-mediated disease processes in the future.
Leukocyte expression of nucleotide receptors
Essentially all leukocyte populations express members of the P2 purinergic receptor superfamily; several recent reviews have detailed receptor expression patterns and the reader is directed to these for a more complete description [12, 13]. Human monocytes, for example, express mRNA encoding P2Y1, P2Y2, P2Y4, P2Y6, P2X1 and P2X7 receptors [14–16]. Human lymphocytes similarly express mRNAs encoding P2Y1, P2Y2, P2Y4, P2Y6 receptors and members of the P2X family, including P2X7, are detected in both B and T-lymphocyte populations [15, 17–21]. Circulating human neutrophils express P2Y4 and P2Y6 mRNAs, and the P2X7 receptor is reported to be present in these cells [22]. Human eosinophils and murine mast cells also are reported to contain the P2X7 receptor [23, 24] as are rodent peritoneal macrophages [25, 26]; historically, many ATP-dependent responses observed using murine macrophages were associated with activation of the P2Z receptor [27, 28]. Cloning and characterization of the P2X7 receptor revealed that this polypeptide possessed functional attributes previously ascribed to the P2Z receptor [29, 30]. Thus, reference to the P2Z receptor was discontinued in favor of the P2X7 receptor designation. Murine spleen macrophages, as well as the macrophage-like cell line J774, express multiple P2X and P2Y subtypes [31]. Murine and rat microglial cells, the brain’s macrophage, also abundantly express P2X7 receptors [32, 33].
A functional consequence often attendant to activation of the P2X7 receptor is the opening of a nonselective pore that is permeable to large fluorescent molecules such as YoPro Yellow. Interestingly, the ability of monocytes and monocyte-like cells to demonstrate this pore activity is influenced by conditions under which these cells are cultured, suggesting that functional output of the P2X7 receptor can be regulated [34–36]. Human monocytes demonstrate a change in receptor functionality without a corresponding change in the level of receptor mRNA expression, suggesting that receptor function can be regulated via posttranslational mechanisms [16].
Dendritic cells, which specialize in antigen presentation and are key producers of cytokines involved in maintenance of acquired immunity, also express members of the P2 receptor superfamily. Human monocyte-derived dendritic cells are reported to express mRNA for P2Y1, P2Y2, P2Y4, P2Y5, P2Y6, P2Y10, P2Y11, and P2Y13 from the P2Y receptor side of the family and P2X1, P2X4, P2X5, and P2X7 from the P2X receptor lineage [37–39]. Murine dendritic cell lines also express the P2X7 receptor [40].
P2Y receptor-dependent regulation of cytokine production
P2Y6 receptor-mediated effects
The P2Y6 receptor is selectively activated via UDP [41], and effects observed with this nucleotide often are attributed to activation of this receptor. Several studies have linked P2Y6 function to IL-8 expression, a cytokine originally isolated as a neutrophil chemotactic factor and now designated as a member of the CXC family of chemokines [42]. IL-8 functions to promote influx of neutrophils to sites of injury and/or infection, and overproduction of IL-8 may contribute to several pathophysiological conditions including chronic lung inflammation and cancer [43]. When human monocytic THP-1 cells are treated with UDP, IL-8 output is enhanced and prior treatment of the cells with a P2Y6 antisense oligonucleotide attenuates the magnitude of the cytokine response [44]. Likewise, P2Y6 receptor transfected 1321N cells secrete greater levels of IL-8 in response to UDP challenge than do their non-transfected counterparts [44]. Similarly, human promonocytic U937 cells stably transfected with human P2Y6 receptor secrete IL-8 when stimulated with UDP [45]. P2Y6 receptor-transfected U937 cells also generate TNFα and the chemokines MCP-1 and IP-10 in response to UDP activation. In contrast, UDP-challenged P2Y6 receptor 1321N cell transfectants produce IL-8 but not other cytokine products [45]. The distinct response patterns displayed by the two transfected cell lines suggest that the cellular context in which the P2Y6 receptor is placed impacts the pattern of cytokines/chemokines expressed. Interestingly, output of IL-8 from LPS stimulated THP-1 cells is decreased when apyrase is included in the cell culture medium [44], suggesting that nucleotides are released in response to LPS activation and these, in turn, activate purinergic receptors in an autocrine type of mechanism.
The mechanism by which the P2Y6 receptor activates cytokine output has received limited investigation. The P2Y6 receptor is a Gq-coupled receptor [13, 46, 47] and thus is expected to promote activation of phospholipase C leading to the generation of inositol-1,4,5-triphosphate and elevation of intracellular Ca2+ levels. In P2Y6 receptor expressing THP-1 cells, the extracellular signal-regulated kinase (ERK) antagonist PD98059 impairs UDP-induced IL-8 output whereas the p38 stress kinase antagonist SB203580 is without effect. Thus, in this system the P2Y6 receptor-induced rise in intracellular Ca2+ appears to be coupled to an ERK-activated signaling cascade leading to IL-8 expression [44]. In osteoclasts, activation of the P2Y6 receptor via UDP or the selective receptor agonist INS48823 induces a transient rise in intracellular Ca2+ and activation of the transcription factor NF-κB [48]. Although cytokine output was not examined in the osteoclast system, activation of NF-κB often is associated with expression of cytokine genes [49] and oscillations in intracellular Ca2+ concentrations have been linked to activation of this transcription factor [50].
With respect to inflammatory disease processes, no specific role for P2Y6 receptors has been reported. However, tissue sections obtained from patients with inflammatory bowel disease are reported to contain T-cells within inflammatory lesions possessing enhanced expression of the P2Y6 receptor [51]. As such, P2Y6 receptor expression on T-cells may be upregulated at sites of inflammation and/or T-cells expressing this receptor may be preferentially recruited to these sites.
P2Y11 receptor-mediated effects impact dendritic cell function
The P2Y11 receptor prefers ATP as it’s ligand, and the non-hydrolyzable ATP analog ATPγS often is employed in vitro as a surrogate ligand; the latter is not, however, a selective agonist of the P2Y11 receptor [41, 47]. P2Y11 receptor modulation of cytokine generation has been studied in some detail with human dendritic cells, with production of IL-12 being a major focus of these studies. IL-12 is composed of two distinct subunits, p40 and p35, which are covalently linked via an intermolecular disulfide bond to form the biologically active p70 species [52–54]. A related cytokine, IL-23, is composed of the same p40 subunit covalently bound to a unique p19 subunit [53, 54]. IL-12 and IL-23 are produced in abundance by activated antigen presenting cells such as monocytes and dendritic cells. When bound to target receptors on T-lymphocytes and natural killer (NK) cells, IL-12 activates interferon (IFN)γ output, alters T-cell development, and affects NK cell killer activity [55]. IL-23 also activates T-cells and promotes IFNγ output, but in this case the responding lymphocytes appear to represent a unique subpopulation of memory T-cells specializing in the production of the proinflammatory cytokine IL-17 [56, 57]. Together, IL-12 and IL-23 cooperate to shift the immune system toward a T helper (Th)1 state that is characteristic of inflammatory diseases such as RA and inflammatory bowel disease [58].
Application of ATP to human monocyte-derived dendritic cells (i.e., monocytes cultured for 6 days in the presence of granulocyte macrophage colony stimulating factor and IL-4) originally was reported to enhance expression of several cell surface molecules and to increase output of IL-12; this ATP effect was augmented by co-stimulation with TNFα [59]. Likewise, ATP but not UTP was reported to enhance expression of CXC chemokine receptor 4 by dendritic cells [60]. In these studies, the nature of the specific P2 receptor subtype(s) responsible for the dendritic cell cytokine response was not addressed.
While the above studies suggested that nucleotides may directly regulate cytokine output, more recent studies conducted with dendritic cells have focused on the role of extracellular nucleotides as modulators of cytokine output induced by other stimuli. For example, treatment of human monocyte-derived dendritic cells with either LPS or CD40 ligand promotes secretion of IL-1α, IL-1β, TNFα, IL-6, and IL-12 (p70), and co-addition of ATP (250 μM) along with the activation stimulus inhibits cytokine output [61]. In this same dendritic cell system, ATP does not inhibit output of IL-10 or IL-1 receptor antagonist, two cytokines possessing anti-inflammatory properties. The dendritic cell purinergic receptor responsible for the cytokine modulatory effects was not identified in this system, but the effect of ATP was mimicked by ADP but not by UTP.
In contrast to the simple pattern of cytokine inhibition noted above, other studies conducted with monocyte-derived dendritic cells suggest that the response elicited by extracellular nucleotides is complex in nature and dependent on the quantity of cytokine produced. For example, monocyte-derived dendritic cells treated with TNFα or LPS generate greater quantities of IL-12 when simultaneously challenged with ATP (the ELISA kit employed in this study measured both IL-12p40 and IL-12p70). Comparison of the effectiveness of several ATP analogs suggests that the P2Y11 receptor is responsible for enhancing cytokine expression [62]. In an extension of these findings, monocyte-derived macrophages were activated with a panel of different agonists (TNFα, LPS, or soluble CD40 ligand) in the absence or presence of ATPγS [63]. At agonist concentrations yielding low levels of IL-12p40 and TNFα output, ATPγS (200 μM) increases secreted levels of these two polypeptides. However, at agonist concentrations yielding higher levels of IL-12p40 and TNFα output, ATPγS inhibits their output. Notably, LPS (but not TNFα or CD40) stimulates secretion of the bioactive, heterodimeric form of IL-12 (i.e., IL-12p70) and ATPγS antagonizes IL-12p70 output at all tested LPS concentrations. It is known from other studies that the p40 and p35 subunits of IL-12 can be regulated independently [64]; lack of coordinated synthesis may help to explain why ATPγS can enhance IL-12p40 but inhibit IL-12p70 output in response to LPS challenge.
The ATP response observed in the dendritic cell system assumes an even greater complexity when the output of IL-12 and IL-23 are compared. Human monocyte-derived dendritic cells activated with intact E. coli produce both IL-12 and IL-23. In response to this challenge, IL-12p40, IL-12p35, and IL-23p19 message levels increase and levels of IL-12 and IL-23 released extracellularly increase accordingly [65]. Addition of ATP (250 μM) to the medium during bacterial challenge decreases IL-12p40 and IL-12p35 message levels but increases IL-23 message levels. Likewise, whereas E. coli-induced secretion of IL-12p70 and IL-12p40 from dendritic cells is inhibited by ATP, secretion of bioactive IL-23 is enhanced. Since both IL-12 and IL-23 share the IL-12p40 subunit, the opposite effects achieved by ATP with respect to output of these two cytokines is somewhat surprising. However, this may reflect that synthesis of the p40 subunit can exceed that of the p19 subunit and secretion of the bioactive IL-23 heterodimer requires simultaneous expression of both subunits [66]. ATPγS and AR-C67085 (a synthetic nucleotide analog) are more potent than ATP at inhibiting E. coli-induced output of IL-12p70 and IL-12p40. In contrast, these two nucleotides are ineffective as enhancers of IL-23; ADP, however, is as effective as ATP at enhancing E. coli-induced IL-23 output. On this basis, it was concluded that the P2Y11 receptor is responsible for the nucleotide-mediated antagonism of IL-12 production whereas a separate, ADP-sensitive P2 receptor subtype is responsible for promoting IL-23 production [65].
Sorting out the identity of P2 receptors that mediate the aforementioned effects of nucleotides on dendritic cell cytokine output is complicated by the existence of cell surface nucleotidases such as CD39 [37]. These enzymes can act on exogenously added nucleotides to generate metabolites that may possess altered selectivity for P2 receptors relative to the parent nucleotide originally added to the culture medium. In this light, it is interesting to note that ADP and several related nucleotides also are reported to inhibit IL-12p70, IL-12p40, and TNFα output from LPS-activated dendritic cells [67]. Based on the inability of ADP to act as an agonist of the P2Y11 receptor and the nature of the signaling response induced by this nucleotide, the cytokine modulatory effects induced by ADP in this system may reflect activation of a novel dendritic cell P2 receptor subtype [67].
Mechanistic features attendant to P2Y11 receptor activation have been investigated and changes to intracellular cAMP concentrations appear important to the cytokine modulatory response. The P2Y11 receptor employs both Gq- and Gs-type G-proteins in mediating signaling [47]; the P2Y11 receptor is unique amongst P2 receptors in its ability to employ Gs and, in turn, to activate adenylate cyclase. Activation of adenylate cyclase and the associated rise in cAMP levels appear to be responsible for both the ATP-induced rise in IL-23 and decline in IL-12 from E. coli-induced human dendritic cells. This conclusion is based on several observations. First, substitution of prostaglandin E2 (PGE2) for ATP in the dendritic cell system produces a similar outcome with respect to inhibition of IL-12 and augmention of IL-23 output [63, 65]. PGE2 signals via G-protein-coupled prostaglandin receptors, and two of these receptors, EP2 and EP4, transmit signals via Gs [68]. Studies conducted in genetically altered mice support the involvement of the EP4 receptor in mediating the inhibitory effect on IL-12 production; LPS-activated bone marrow-derived macrophages derived from wild-type mice but not from EP4 receptor-deficient animals produce less IL-12 in the presence of PGE2 [69]. Second, activation of other G protein coupled receptors (GPCRs) that engage adenylate cyclase, such as histamine (H2) and adenosine A2a receptors, inhibit IL-12 output [70]. Third, the ability of ATP analogs to alter IL-12 output correlates with their impact on intracellular cAMP levels [62]. Finally, treatment of E. coli-activated dendritic cells with forskolin, an agent that activates adenylate cyclase independently of GPCR activation, also inhibits IL-12 (protein) output while enhancing IL-23p19 (message) expression [65]. In view of the ability of the aforementioned agents to elevate cAMP and to produce reciprocal effects on IL-12 and IL-23 output from dendritic cells, it is surprising that ATPγS and AR-C67085, two effective agonists of the P2Y11 receptor, cause inhibition of IL-12 output without enhancing IL-23 expression [65]. Notably, ADP is able to enhance IL-23p19 message expression by E. coli-activated dendritic cells [65]. The reciprocal effects observed with respect to production of IL-12 and IL-23 in the presence of ATP, therefore, may reflect activation of the P2Y11 receptor by ATP and, as a result of hydrolysis of the added ATP via ecto-nucleotidases, simultaneous activation of a novel type of P2 receptor that is activated via ADP and coupled to Gs.
Although dendritic cell cytokine output is well documented to be subject to regulation via nucleotides in vitro, there is little information to suggest that this type of regulation takes place in vivo. A recent report noted, however, that intradermal injection of ATPγS into mice results in an enhanced contact hypersensitivity response, and this effect may be achieved as a result of activation of Langerhans cells, a subclass of dendritic cells [71]. Murine Langerhans cells, like other dendritic cells, express the ecto-nucleotidase CD39, and CD39-deficient mice display an exacerbated skin inflammatory response when irritant chemicals such as croton oil are applied topically [72].
P2X receptor-dependent regulation of cytokine production
With the exception of the P2X7 receptor, functional responses attendant to activation of P2X receptor family members are not generally associated with cytokine modulation. Members of this family certainly can impact inflammatory processes as evidenced by the attenuated pain responses observed following administration of selective P2X3 receptor antagonists to rodents [73]. These effects, however, are not directly linked to cytokine output but, rather, to effects associated with modulation of sensory afferent neurons. Therefore, a discussion of how P2X receptors affect cytokine output is limited in scope to the role of the P2X7 receptor. Although selective agonists and/or antagonists of the P2X7 receptor have to this point not been available, the P2X7 receptor possesses atypical features that often allow its function to be implicated during in vitro studies. Most notable amongst these features is the requirement that high ATP concentrations, often in excess of 500 μM, be employed to achieve receptor activation when cells are maintained in physiological media. Benzoylbenzoyl-ATP (BZATP) often is employed as an agonist of the P2X7 receptor. Although this agent is reported to be a more effective agonist than ATP [74], it is not specific for the P2X7 receptor [75]. Likewise, oxidized ATP often is employed as an antagonist of the P2X7 receptor [76], but this agent also acts in a P2 receptor-independent manner [77].
P2X7 receptor-mediated effects
As noted earlier, the P2X7 receptor is present on a number of leukocyte populations including monocytes and tissue macrophages. When challenged appropriately, cells of monocyte/macrophage lineage are abundant producers of proinflammatory cytokines including IL-1 and TNFα. With respect to TNFα output, both enhancing and inhibitory responses have been associated with P2X7 receptor activation. Cultured rat microglia treated with 1 mM ATP, for example, increase expression of TNFα mRNA and secrete this proinflammatory cytokine [78]. In this cellular system, the TNFα-enhancing effect of ATP is dependent on an influx of extracellular calcium, and is suppressed by inhibitors of ERK (PD098059) and p38 (SB203580) mitogen activated kinases. Likewise, ATP is reported to enhance TNFα output from murine RAW 264.7 macrophages both in the absence and presence of LPS [79]; the purinergic receptor responsible for this effect in RAW cells is unknown. On the other hand, ATP is reported to inhibit TNFα release from LPS-activated murine peritoneal macrophages [80]; this antagonism does not appear to result from activation of the P2X7 receptor as UTP and UDP mimic the action of ATP but are not P2X7 receptor agonists. Similarly, ATP inhibits LPS-induced release of TNFα from rat cortical astrocytes [81]. In this cellular system mM concentrations of ATP are required for the biological response, and the effect of ATP is mimicked by BZATP, properties consistent with involvement of the P2X7 receptor. Thus, the net effect observed with respect to ATP’s ability to modulate TNFα output is dependent on the cellular context.
The most extensively studied cytokine modulatory role involving the P2X7 receptor relates to its ability to promote IL-1β posttranslational processing. IL-1β is a multifaceted proinflammatory cytokine produced predominantly by cells of the monocyte/macrophage lineage [82]. Resting monocytes and macrophages do not constitutively produce IL-1β, but following challenge with an activating stimulus such as LPS, these cells rapidly engage in the production of large quantities of proIL-1β. This precursor polypeptide (31 to 35 kDa in mass) must be proteolytically processed by caspase-1 to generate the mature biologically active 17 kDa cytokine species [83–85]. Importantly, proIL-1β lacks a leader sequence and, as a result, the newly synthesized polypeptides accumulate intracellularly within the cytosol of LPS-activated cells. In contrast to IL-1β, caspase-1 is constitutively expressed by monocytes and macrophages; this cysteine protease also resides in the cytoplasm as an inactive zymogen [86]. In the absence of additional stimulation, only a very low percentage of the newly synthesized proIL-1β polypeptides produced by LPS-treated cells is processed by caspase-1 and released extracellularly [87]. However, in the presence of an appropriate activation stimulus, procaspase-1 is converted to its catalytically active form, proIL-1β subsequently is cleaved to its mature 17 kDa species, and the mature cytokine is released extracellularly where it can engage receptors on target cells; a number of agents have been reported to facilitate this posttranslational processing in vitro including various toxins [88–92], defensin-like peptides [93, 94], and K+ ionophores [95–97].
David Chaplin and his group first demonstrated that ATP can act as a trigger to promote IL-1β posttranslational processing from LPS-activated murine peritoneal macrophages [98]. When incubated in the absence of ATP, LPS-activated macrophages labeled with [35S]methionine were shown to possess abundant quantities of the 35 kDa proIL-1β polypeptide, but radiolabeled cytokine products were not released extracellularly. Following addition of ATP to the medium, however, the LPS-activated/[35S]methionine-labeled cells released IL-1β to the medium and the majority of the externalized cytokine was efficiently converted to the mature 17 kDa species. The ATP-treated macrophages also released the cytoplasmic enzyme lactate dehydrogenase (LDH) and possessed a DNA fragmentation profile that was characteristic of an apoptotic cellular response. Although the identity of the receptor responsible for mediating these effects was not addressed, the high concentration of ATP employed (5 mM) suggested P2X7 receptor involvement. The ability of ATP to promote IL-1β posttranslational processing by murine peritoneal macrophages is not limited to in vitro cultures. Mice primed with LPS in vivo contain peritoneal macrophages that are laden with proIL-1β, but lavage of the peritoneal cavities of these mice yields minimal quantities of the mature cytokine species. Following a subsequent intraperitoneal injection of ATP into the LPS-primed animals, however, large quantities of mature IL-1β are recovered in the lavage fluids [99]. Thus, ATP acts as an effective agonist of IL-1β posttranslational processing both in vitro and in vivo.
Subsequent studies demonstrated that ATP is an effective stimulus for promoting IL-1β posttranslational processing by a number of different cell types including human monocytes/macrophages [100–102] and human and mouse microglial cells [103–105]. In all cases, the cytokine response requires concentrations of ATP >1 mM, a requirement consistent with activation of the P2X7 receptor. Involvement of the P2X7 receptor is further supported by the observation that KN62 inhibits ATP-induced IL-1β posttranslational processing by LPS-activated human monoctyes [102]; this agent is a potent inhibitor of P2X7 receptor-mediated functions [106, 107]. Furthermore, an antibody generated against the P2X7 receptor blocks ATP-induced IL-1β release from LPS-activated human monocytes [108]. Analysis of peritoneal macrophages obtained from mice genetically engineered to lack the P2X7 receptor provided the final piece of evidence that P2X7 receptor function is necessary for ATP-induced IL-1β posttranslational processing [26]. Macrophages obtained from both wild type and P2X7-deficient mice generate equivalent quantities of newly synthesized proIL-1β in response to LPS challenge. However, in the absence of a secondary stimulus neither macrophage population releases mature IL-1β to the medium. Following treatment with 5 mM ATP, wild type but not P2X7 receptor-deficient macrophages externalize large quantities of mature IL-1β. In contrast, both macrophage populations release mature IL-1β when treated with the potassium ionophore nigericin, indicating that the P2X7 receptor-deficient macrophages are competent to process proIL-1β but absence of the P2X7 receptor prevents them from doing so when challenged with ATP [26].
Signaling pathways associated with P2X7 receptor activation
Mechanistic elements engaged as a result of P2X7 receptor activation that are responsible for initiating IL-1β posttranslational processing are not completely understood, but studies to date have provided insight into this atypical secretory process. ATP acting via the P2X7 receptor activates a number of intracellular kinases including members of the MAP kinase family ERK and JNK [23, 109–112], Rho effector kinases [113, 114], and the protein tyrosine kinase p56lck [115]. Correspondingly, increased phosphorylation of various intracellular polypeptides including the receptor itself are observed post-ATP activation [116–118]. P2X7 receptor operation also is associated with activation of various transcription factors [119, 120], enhanced production of reactive oxygen species [121], mitochondrial membrane depolarization [122], and activation of phospholipase D [123]. It remains to be established whether any of these changes are required for IL-1β posttranslational processing, although a Ca2+-independent phospholipase inhibitor (bromoenol lactone) and a tyrosine kinase inhibitor (AG-126) are reported to inhibit ATP-induced IL-1β output [124, 125]. As a ligand-gated ion channel, the P2X7 receptor also promotes rapid changes in ionic homeostasis following its activation [126]. Prolonged ligation of the receptor can result in complete membrane depolarization, a process that is likely to involve opening of the P2X7 receptor operated pore [126]. In several cellular systems, a rise in intracellular Ca2+ promoted by the P2X7 receptor is necessary for IL-1β posttranslational processing [127, 128]. Similarly, K+ efflux mediated via P2X7 receptor activation in LPS-stimulated monocytes and macrophages is necessary for efficient IL-1β posttranslational processing [96, 97, 100, 101, 125, 127]. Simply increasing the medium K+ ion concentration can completely inhibit ATP-induced IL-1β output [96, 100, 101, 129]; as such, K+ efflux appears to serve a key role in the cellular process.
How these changes to intracellular K+ and Ca2+ ion levels regulate IL-1β posttranslational processing remains to be established. In the case of K+, the P2X7 receptor-induced changes may facilitate activation of caspase-1. As noted earlier, procaspase-1 is expressed constitutively by monocytes and macrophages and resides in the cytoplasmic compartment as a latent zymogen. Ligation of the P2X7 receptor leads to rapid activation of caspase-1 and, like mature IL-1β, the activated protease is released to the medium [130]. Recent studies have indicated that activation of procaspase-1 requires assembly of a large protein scaffold termed the inflammasome [131, 132]. Components of the inflammasome may include a NALP (NALP1, 2 or 3), the speck like protein ASC, and procaspase-5 [132–135]. The importance of ASC in ATP-induced IL-1β posttranslational processing is highlighted by the demonstration that LPS-activated peritoneal macrophages isolated from ASC-deficient mice fail to generate mature IL-1β in response to ATP challenge [136]. In a resting cell, the NALP polypeptide appears to exist in an inactive monomeric conformation, but this polypeptide may undergo a conformational change in response to an appropriate effector leading to its association with ASC and procaspases [135]. This association involves several protein-protein interaction domains including PYRIN and caspase recruitment domains (CARDs). The resulting protein ensemble positions the procaspases in close proximity leading to their proteolytic activation [135]. Studies of inflammasome assembly using broken cell preparations have demonstrated that extracts prepared from cells briefly treated with mM concentrations of ATP are more effective at generating mature caspase-1 and mature IL-1β than are comparable extracts prepared from non-ATP treated cells. Moreover, when the ATP treatment is performed in the presence of high extracellular K+ (thus limiting K+ efflux from the ATP-treated cells), the resultant inflammasome activity in the cell-free extract is reduced [125]. These findings, therefore, suggest that K+ efflux may facilitate inflammasome assembly and/or its activation.
As noted above, changes in intracellular Ca2+ levels also contribute to IL-1β posttranslational processing. ATP-induced changes in intracellular Ca+2 may result from Ca2+ entry via P2X receptors as well as from Ca2+ release from intracellular stores mediated via P2Y receptors. In LPS-activated mouse peritoneal macrophages, Ca2+ release from intracellular stores is required for ATP-induced IL-1β maturation and release, but in this system the cytokine response does not require Ca2+ influx from the medium [127]. Likewise, ATP-induced IL-1β output from LPS-activated human monocytes is unaffected by removal of extracellular Ca2+ [129]. However, LPS-activated human THP-1 cells [137] and HEK293 engineered to express both the P2X7 receptor and mature IL-1β [128] require influx of extracellular Ca2+ for optimal cytokine output. Therefore, the nature of the Ca2+ requirement is dependent on the type of cell being analyzed. Interestingly, a recent study concluded that opening of the P2X7 receptor-activated pore is dependent on Ca2+ [138]. Although a role for the pore in IL-1β posttranslational processing has not been established, perhaps the Ca2+ requirement for IL-1 maturation and release relates to this activity. Moreover, Ca2+ influx via the P2X7 receptor recently was linked to a pseudoapoptotic state characterized by phosphatidylserine movements within the plasma membrane and to cytoskeletal disruption and zeiotic membrane distortions [139].
Externalization of mature IL-1β following P2X7 receptor activation
A number of different mechanisms have been proposed to explain how mature IL-1β is released to the extracellular environment following ATP stimulation. LPS-activated murine peritoneal macrophages and human monocytes exposed to mM concentrations of ATP in vitro release mature IL-1β via a process that is accompanied by release of the cytoplasmic marker enzyme LDH [98, 140]. Although the kinetics of appearance of LDH within the medium of ATP-treated mouse peritoneal macrophages lags behind the appearance of mature IL-1β [140], release of the former to the medium suggests that plasma membrane latency is lost during the ATP-induced process. Thus, one mechanism proposed for the release of mature IL-1β is that the producing cell dies, possibly via an apoptotic-like process, and intracellular components are released passively from the cell following disruption of the plasma membrane [98]. On the other hand, evidence exists to suggest that release of mature IL-1β is a facilitated process. For example, release of mature IL-1β from LPS-activated murine macrophages in response to ATP challenge is blocked by non-selective agents that are known to antagonize transport function of ABC1, a membrane-bound protein that functions in cholesterol transport [141]. On this basis, ABC1 was proposed to facilitate transport of mature IL-1β [141]. Moreover, when LPS-activated THP-1 cells are treated with 300 μM BZATP, microvesicles which contain bioactive IL-1β are rapidly shed from the cell surface [137]. A similar process has been reported to occur in mixed cultures of rat primary astrocytes and microglia [142]. In this case, ATP released from astrocytes appears to promote shedding of microvesicles from neighboring microglia containing IL-1β. Details of how the shed microvesicles subsequently release their content of cytokine have yet to be defined. An even more elaborate system for externalization of mature IL-1β has been proposed based on immunohistochemical observations that co-localized proIL-1β and lysosomal enzymes within cytoplasmic vesicles [143, 144]. In response to ATP, these vesicles appear to fuse with the plasma membrane via a process that is triggered by K+ depletion and dependent on phospholipase activation [144]. To what extent each of these different mechanisms contributes to the release of IL-1β in vivo remains to be established.
ATP’s ability to promote IL-1β posttranslational processing in vitro via the P2X7 receptor is well documented, but evidence demonstrating that the P2X7 receptor functions in this capacity in vivo is limited. Moreover, no evidence has thus far been presented to suggest that P2X7 receptor levels and/or activity are altered in human inflammatory diseases. A number of single nucleotide polymorphisms have been identified in the human P2X7 receptor gene [145–151] and these can lead to impaired ATP-induced IL-1β (and IL-18) posttranslational processing in vitro [152, 153]. Thus, it will be of great interest to determine whether individuals possessing these functionally impaired P2X7 receptor phenotypes are less susceptible to inflammatory disorders. Two independent P2X7 receptor-deficient mouse lines have been generated [26, 154]. Although these receptor-deficient mice are overtly normal, when subjected to various challenges they display attenuated inflammatory responses. For example, after treatment with a panel of anticollagen antibodies to induce an RA-like disease state, joints recovered from wild type mice display a more pronounced inflammatory cell infiltrate and greater cartilage destruction than do joints recovered from P2X7 receptor-deficient mice [26]. In similar murine models of arthritis, administration of neutralizing anti-IL-1 antibodies are known to suppress the inflammatory response [155–157]. Therefore, the protection afforded by deletion of the P2X7 receptor is consistent with the knockout mice possessing a diminished capacity to generate mature IL-1β. Indeed, following intraplantar injection of Freund’s complete adjuvant, extracts of the injected paws obtained from wild type mice contain greater levels of IL-1β than do comparable extracts obtained from P2X7 receptor-deficient mice [154]. Moreover, P2X7 receptor-deficient mice display less hypersensitivity to the adjuvant challenge than do their wild type counterparts. These in vivo disease model studies, therefore, suggest that antagonism of the P2X7 receptor may offer a novel therapeutic approach for the treatment of inflammatory disorders. As several pharmaceutical companies appear to be engaged in a search for antagonists of the P2X7 receptor [158–160], the ability to selectively modulate this receptor pharmacologically in animal models and man may soon be possible.
Abbreviations
- LPS:
-
lipopolysaccharide
- RA:
-
rheumatoid arthritis
- IL:
-
interleukin
- TNF:
-
tumor necrosis factor
- IFN:
-
interferon
- ERK:
-
extracellular signal regulated kinase
- LDH:
-
lactate dehydrogenase
- PGE2 :
-
prostaglandin E2
- GPCR:
-
G protein coupled receptor
- BZATP:
-
benzoylbenzoyl-ATP
References
Fischer A (2001) Primary immunodeficiency diseases: an experimental model for molecular medicine. Lancet 357:1863–869
Casanova J-L, Abel L (2004) The human model: a genetic dissection of immunity to infection in natural conditions. Nat Rev Immunol 4:55–6
Billiau A, Heremans H, Matthys P (2003) The use of cytokine knockouts in animal models of autoimmune disease. In: Fantuzzi G (ed) Cytokine knockouts, 2nd edn. Humana, Totowa, NJ, pp 33–5
Bathon JM, Martin RW, Fleischman RM et al (2000) A comparison of etanercept and methotrexate in patients with early rheumatoid arthritis. N Engl J Med 343:1586-1593
Lipsky PE, van der Heijde DM, St. Clair EW et al (2000) Infliximab and methotrexate in the treatment of rheumatoid arthritis. Anti-tumor necrosis factor trial in rheumatoid arthritis with concomitant therapy study group. N Engl J Med 343:1594–602
Doan T, Massarotti E (2005) Rheumatoid arthritis: an overview of new and emerging therapies. J Clin Pharmacol 45:751–62
Cohen S, Hurd E, Cush J et al (2002) Treatment of rheumatoid arthritis with Ankinra, a recombinant human interleukin-1 receptor antagonist, in combination with methotrexate. Arthritis Rheum 46:614–24
Hawkins PN, Lachmann HJ, Aganna E et al (2004) Spectrum of clinical features in Muckle-Wells syndrome and response to Anakinra. Arthritis Rheum 50:607–12
Lovell DJ, Bowyer SL, Solinger AM (2005) Interleukin-1 blockade by Anakinra improves clinical symptoms in patients with neonatal-onset multisystem inflammatory disease. Arthritis Rheum 52:1283–286
Kauffman CL, Aria N, Toichi E et al (2004) A phase I study evaluating the safety, pharmacokinetics, and clinical response of a human IL-12 p40 antibody in subjects with plaque psoriasis. J Invest Dermatol 123:1037–044
Mannon PJ, Fuss IJ, Mayer L et al (2004) Anti-interleukin-12 antibody for active Crohn’s disease. N Engl J Med 351:2069–079
Di Virgilio F, Chiozzi P, Ferrari D et al (2001) Nucleotide receptors: an emerging family of regulatory molecules in blood cells. Blood 97:587–00
Di Virgilio F, Baricordi OR, Romagnoli R et al (2005) Leukocyte P2 receptors: a novel target for anti-inflammatory and anti-tumor therapy. Curr Drug Targets: Cardiovasc Hematol Disord 5:85–9
Dubyak GR, Cliffor EE, Humphreys BD et al (1996) Expression of multiple ATP receptor subtypes during the differentiation and inflammatory activation of myeloid leukocytes. Drug Dev Res 39:269–78
Jin J, Dasari VR, Sistare FD et al (1998) Distribution of P2Y2 receptor subtypes on haematopoietic cells. Br J Pharmacol 123:789–94
Gudipaty L, Humphreys BD, Buell G et al (2001) Regulation of P2X7 nucleotide receptor function in human monocytes by extracellular ions and receptor density. Am J Physiol Cell Physiol 280:C943–C953
Wiley JS, Dubyak GR (1989) Extracellular adenosine triphosphate increases cation permeability of chronic lymphocytic leukemic lymphocytes. Blood 73:1316–323
Gu B, Bendall LJ, Wiley JS (1998) Adenosine triphosphate-induced shedding of CD23 and L-selectin (CD62L) from lymphocytes is mediated by the same receptor but different metalloproteases. Blood 92:946–51
Gu BJ, Zhnag WY, Bendall LJ et al (2000) Expression of P2X7 purinoceptors on human lymphocytes and monocytes: evidence for non-functional P2X7 receptors. Am J Physiol Cell Physiol 279:C1189–C1197
Sluyter R, Barden JA, Wiley JS (2001) Detection of P2X purinergic receptors on human B lymphocytes. Cell Tissue Res 304:231–36
Adinolfi E, Melchiorri L, Falzoni S et al (2002) P2X7 receptor expression in evolutive and indolent forms of chronic B lymphocytic leukemia. Blood 99:706–08
Suh B-C, Kim J-S, Namgung U et al (2001) P2X7 nucleotide receptor mediation of membrane pore formation and superoxide generation in human promyelocytes and neutrophils. J Immunol 166:6754–763
Bulanova E, Budagian V, Orinska Z et al (2005) Extracellular ATP induces cytokine expression and apoptosis through P2X7 receptor in murine mast cells. J Immunol 174:3880–890
Idzko M, Panther E, Bremer HC et al (2003) Stimulation of P2 purinergic receptors induces the release of eosinophil cationic protein and interleukin-8 from human eosinophils. Br J Pharmacol 138:1244–250
Chen Y-W, Donnelly-Roberts DL, Namovic MT et al (2005) Pharmacological characterization of P2X7 receptors in rat peritoneal macrophages. Inflamm Res 54:119–26
Solle M, Labasi J, Perregaux DG et al (2001) Altered cytokine production in mice lacking P2X7 receptors. J Biol Chem 276:125–32
Sung S-SJ, Young JD-E, Origlio AM et al (1985) Extracellular ATP perturbs transmembrane ion fluxes, elevates cytosolic [Ca2+], and inhibits phagocytosis in mouse macrophages. J Biol Chem 260:13442–3449
Steinberg TH, Newman AS, Swanson JA et al (1987) ATP4- permeabilizes the plasma membrane of mouse macrophages to fluorescent dyes. J Biol Chem 262:8884–888
Surprenant A, Rassendren F, Kawashima E et al (1996) The cytolytic P2Z receptor for extracellular ATP identified as a P2X receptor (P2X7). Science 272:735–38
Chessell IP, Simon J, Hibell AD et al (1998) Cloning and functional characterization of the mouse P2X7 receptor. FEBS Lett 439:26–0
Coutinho-Silva R, Ojcius DM, Gorecki DC et al (2004) Multiple P2X and P2Y receptor subtypes in mouse J774, spleen and peritoneal macrophages. Biochem Pharmacol 69:641–55
Ferrari D, Chiozzi P, Falzoni S et al (1997) ATP-mediated cytotoxicity in microglial cells. Neuropharmacology 36:1295–301
Collo G, Neidhart S, Kawashima E et al (1997) Tissue distribution of the P2X7 receptor. Neuropharmacology 36:1277–283
Hickman SE, El Khoury J, Greenberg S et al (1994) P2Z adenosine triphosphate receptor activity in cultured human monocyte-derived macrophages. Blood 84:2452–456
Falzoni S, Munerati M, Ferrari D et al (1995) The purinergic P2Z receptor of human macrophage cells. Clin Invest 95:1207–216
Humphreys BD, Dubyak GR (1996) Induction of the P2Z/P2X7 nucleotide receptor and associated phospholipase activity by lipopolysaccharide and IFN-γ in the human THP-1 monocytic cell line. J Immunol 157:5627–637
Berchtold S, Ogilvie ALJ, Bogdan C et al (1999) Human monocyte derived dendritic cells express functional P2X and P2Y receptors as well as ecto-nucleotidases. FEBS Lett 458:424–28
Ferrari D, La Sala A, Chiozzi P et al (2000) The P2 purinergic receptors of human dendritic cells: identification and coupling to cytokine release. FASEB J 14:2466–476
Zhang FL, Luo L, Gustafson E et al (2002) P2Y13: identification and characterization of a novel Gαi-coupled ADP receptor from human and mouse. J Pharmacol Exp Ther 301:705–13
Mutini C, Falzoni S, Ferrari D et al (1999) Mouse dendritic cells express the P2X7 purinergic receptor: characterization and possible participation in antigen presentation. J Immunol 163:1958–965
Ralevic V, Burnstock G (1998) Receptors for purines and pyrimidines. Pharmacol Rev 50:413–92
Luster AD (1998) Chemokines-chemotactic cytokines that mediate inflammation. N Engl J Med 338:436–55
Mukaida N (2003) Pathophysiological roles of interleukin-8/CXCL8 in pulmonary diseases. Am J Physiol Lung Cell Mol Physiol 284:L566–L577
Warny M, Aboudola S, Robson SC et al (2001) P2Y6 nucleotide receptor mediates monocyte interleukin-8 production in response to UDP or lipopolysaccharide. J Biol Chem 276:26051–6056
Cox MA, Gomes B, Plamer K et al (2005) The pyrimidinergic P2Y6 receptor mediates a novel release of proinflammatory cytokines and chemokines in monocytic cells stimulated with UDP. Biochem Biophys Res Commun 330:467–73
Dubyak GR, el-Moatassim C (1993) Signal transduction via P2-purinergic receptors for extracellular ATP and other nucleotides. Am J Physiol 265:C577–C606
Boeynaems J-M, Communi D, Gonzalez NS et al (2005) Overview of the P2 receptors. Semin Thromb Hemost 31:139–49
Korcok J, Raimundo LN, Du X et al (2005) P2Y6 nucleotide receptors activate NF-κB and increase survival of osteoclasts. J Biol Chem 280:16909–6915
Baeuerle PA, Henkel T (1994) Function and activation of NF-κB in the immune system. Annu Rev Immunol 12:141–79
Dolmetsch RE, Xu K, Lewis RS (1998) Calcium oscillations increase the efficiency and specificity of gene expression. Nature 392:933–36
Somers GR, Hammett FMA, Trute L et al (1998) Expression of the P2Y6 purinergic receptor in human T cells infiltrating inflammatory bowel disease. Lab Invest 78:1375–383
Trinchieri G (2003) Interleukin-12 and the regulation of innate resistance and adaptive immunity. Nat Rev Immunol 3:133–46
Trinchieri G, Pflanz S, Kastelein RA (2003) The IL-12 family of heterodimeric cytokines: new players in the regulation of T cell responses. Immunity 19:641–44
Langrish CL, McKenzie BS, Wilson NJ et al (2004) IL-12 and IL-23: master regulators of innate and adaptive immunity. Immunol Rev 202:96–05
Watford WT, Hissong BD, Bream JH et al (2004) Signaling by IL-12 and IL-23 and the immunoregulatory roles of STAT4. Immunol Rev 202:139–56
Aggarwal S, Ghilardi N, Xie M-H et al (2003) Interleukin-23 promotes a distinct CD4 T cell activation state characterized by the production of interleukin-17. J Biol Chem 278:1910–914
Langrish CL, Chen Y, Blumenschein WM et al (2005) IL-23 drives pathogenic T cell population that induces autoimmune inflammation. J Exp Med 201:233–40
Moss RB, Moll T, El-Kalay M et al (2005) Th1/Th2 cells in inflammatory disease states: therapeutic implications. Expet Opin Biol Ther 4:1887–896
Schnurr M, Then F, Galambos P et al (2000) Extracellular ATP and TNF-α synergise in the activation and maturation of human dendritic cells. J Immunol 165:4704–709
la Salla A, Sebastiani S, Ferrari D et al (2002) Dendritic cells exposed to extracellular adenosine triphosphate acquire the migratory properties of mature cells and show a reduced capacity to attract type 1 T lymphocytes. Blood 99:1715-1722
la Sala A, Ferrari D, Corinti S et al (2001) Extracellular ATP induces a distorted maturation of dendritic cells and inhibits their capacity to initiate Th1 responses. J Immunol 166:1611-1617
Wilkin F, Duhant X, Bruyns C et al (2001) The P2Y11 receptor mediates the ATP-induced maturation of human monocyte-derived dendritic cells. J Immunol 166:7172–177
Wilkin F, Stordeur P, Goldman M et al (2002) Extracellular adenine nucleotides modulate cytokine production by human monocyte-derived dendritic cells: dual effect on IL-12 and stimulation of IL-10. Eur J Immunol 32:2409–417
D’Andrea A, Rengaraju M, Valiante NM et al (1992) Production of natural killer cell stimulatory factor (interleukin 12) by peripheral blood mononuclear cells. J Exp Med 176:1387–398
Schnurr M, Toy T, Shin A et al (2005) Extracellular nucleotide signaling by P2 receptors inhibits IL-12 and enhances IL-23 expression in human dendritic cells: a novel role for the cAMP pathway. Blood 105:1582–589
Oppmann B, Lesley R, Blom B et al (2000) Novel p19 protein engages IL-12p40 to form a cytokine, IL-23, with biological properties similar as well as distinct from IL-12. Immunity 13:715–25
Marteau F, Communi D, Boeynaems J-M et al (2004) Involvement of multiple P2Y receptors and signaling pathways in the action of adenine nucleotide diphosphates on human monocyte-derived dendritic cells. J Leukoc Biol 76:796–03
Narumiya S, Sugimoto Y, Ushikubi F (1999) Prostanoid receptors: structures, properties, and functions. Physiol Rev 79:1193–225
Nataraj C, Thomas DW, Tilley SL et al (2001) Receptors for prostaglandin E2 that regulate cellular immune responses in the mouse. J Clin Invest 108:1229–235
Braun MC, Kelsall BL (2001) Regulation of interleukin-12 production by G-protein-coupled receptors. Microbes Infect 3:99–07
Granstein RD, Ding W, Huang J et al (2005) Augmentation of cutaneous immune responses by ATPγS: purinergic agonists define a novel class of immunologic adjuvants. J Immunol 174:7725–731
Mizumoto N, Kumamoto T, Robson SC et al (2002) CD39 is the dominant Langehans cell-associated ecto-NTPDase: modulatory roles in inflammation and immune responsiveness. Nat Med 8:358–65
Jarvis MF, Burgard EC, McGaraughty S et al (2002) A-317491, a potent and selective non-nucleotide antagonist of P2X3 and P2X2/3 receptors, reduces chronic inflammatory and neuropathic pain in the rat. Proc Nat Acad Sci 99:17179–7184
Gargett CE, Cornish JE, Wiley JS (1997) ATP, a partial agonist for the P2Z receptor of human lymphocytes. Br J Pharmacol 122:911–17
Bianchi BR, Lynch KJ, Touma E et al (1999) Pharmacological characterization of recombinant human and rat P2X receptor subtypes. Eur J Pharmacol 376:127–38
Murgia M, Hanau S, Pizzo P et al (1993) Oxidized ATP; an irreversible inhibitor of the macrophage purinergic P2X receptor. J Biol Chem 268:8199–203
Beigi RD, Kertesy SB, Aquilina G et al (2003) Oxidized ATP (oATP) attenuates proinflammatory signaling via P2 receptor-independent mechanisms. Br J Pharmacol 140:507–19
Hide I, Tanaka M, Inoue A et al (2000) Extracellular ATP triggers tumor necrosis factor-α release from rat microglia. J Neurochem 75:965–72
Tonetti M, Sturla L, Giovine M et al (1995) Extracellular ATP enhances mRNA levels of nitric oxide synthase and TNFα in lipopolysaccharide-treated RAW 264.7 murine macrophages. Biochem Biophys Res Commun 214:125–30
Hasko G, Kuhel DG, Salzman AL et al (2000) ATP suppression of interleukin-12 and tumour necrosis factor-α release from macrophages. Br J Pharmacol 129:909–14
Kucher BM, Neary JT (2005) Bi-functional effects of ATP/P2 receptor activation on tumor necrosis factor-alpha release in lipopolysaccharide-stimulated astrocytes. J Neurochem 92:525–35
Dinarello CA (1998) Interleukin-1, interleukin-1 receptors and interleukin-1 receptor antagonist. Int Rev Immunol 16:457–99
Cerretti DP, Lozlosky CJ, Mosley B et al (1992) Molecular cloning of the interleukin-1β converting enzyme. Science 256:97–00
Thornberry NA, Bull HG, Calaycay JR et al (1992) A novel heterodimeric cysteine protease is required for interleukin-1β processing in monocytes. Nature 356:768–74
Kuida K, Lippke JA, Ku G et al (1995) Altered cytokine export and apoptosis in mice deficient in interleukin-1β converting enzyme. Science 267:2000–002
Ayala JM, Yamin TT, Egger LA et al (1994) IL-1β-converting enzyme is present in monocytic cells as an inactive 45 kDa precursor. J Immunol 153:2592–599
Hogquist KA, Unanue ER, Chaplin DD (1991) Release of IL-1 from mononuclear phagocytes. J Immunol 147:2181–186
Bhakdi S, Muhly M, Korom S et al (1990) Effects of Escherichia coli hemolysin on human monocytes. J Clin Invest 85:1746-1753
Walev I, Weller U, Strauch S et al (1996) Selective killing of human monocytes and cytokine release provoked by sphingomyelinase (beta-toxin) of Staphylococcus aureus. Infect Immun 64:2974–979
Verhoef PA, Kertesy SB, Estacion M et al (2004) Maitotoxin induces biphasic interleukin-1β secretion and membrane blebbing in murine macrophages. Mol Pharmacol 66:909–20
Cordoba-Rodriguez R, Fang H, Lankford CSR et al (2004) Anthrax lethal toxin rapidly activates caspase-1/ICE and induces extracellular release of interleukin (IL)-1β and IL-18. J Biol Chem 279:20563–0566
Kelk P, Claesson R, Hanstrom L et al (2005) Abundant secretion of bioactive interleukin-1β by human monocytes induced by Actinobacillus actinomycetemcomitans leukotoxin. Infect Immun 73:453–58
Perregaux D, Bhavsar K, Contillo L et al (2002) Antimicrobial peptides initiate IL-1β posttranslational processing: a novel role beyond innate immunity. J Immunol 168:3024–032
Elssner A, Duncan M, Gavrilin M et al (2004) A novel P2X7 receptor activator, the human cathelicidin-derived peptide LL37, induces IL-1β processing and release. J Immunol 172:4987–994
Perregaux D, Barberia J, Lanzetti AJ et al (1992) IL-1β maturation: evidence that mature cytokine formation can be induced specifically by nigericin. J Immunol 149:1294–303
Walev I, Reske K, Palmer M et al (1995) Potassium-inhibited processing of IL-1β in human monocytes. EMBO J 14:1607–614
Cheneval D, Ramage P, Kastelic T et al (1998) Increased mature interleukin-1β (IL-1β) secretion from THP- cells induced by nigericin is a result of activation of p45 IL-1β-converting enzyme processing. J Biol Chem 273:17846–7851
Hogquist KA, Nett MA, Unanue ER et al (1991) Interleukin 1 is processed and released during apoptosis. Proc Natl Acad Sci 88:8485–489
Griffiths RJ, Stam EJ, Downs J et al (1995) ATP induces the release of IL-1 from LPS primed cells in vivo. J Immunol 154:2821–828
Perregaux D, Gabel CA (1994) Interleukin1-β maturation and release in response to ATP and nigericin. J Biol Chem 269:15195–5203
Ferrari D, Chiozzi P, Falzoni S et al (1997) Extracellular ATP triggers IL-1β release by activating the purinerigic P2Z receptor on human macrophages. J Immunol 159:1451–458
Grahames CBA, Michel AD, Chessell IP et al (1999) Pharmacological characterization of ATP- and LPS-induced IL-1β release in human monocytes. Br J Pharmacol 127:1915–921
Ferrari D, Villalba M, Chiozzi P et al (1996) Mouse microglial cells express a plasma membrane pore gated by extracellular ATP. J Immunol 156:1531–539
Ferrari D, Chiozzi P, Falzoni S et al (1997) Purinergic modulation of interleukin-1β release from microglial cells stimulated with bacterial endotoxin. J Exp Med 185:1–
Rampe D, Wang L, Ringheim GE (2004) P2X7 receptor modulation of β-amyloid- and LPS-induced cytokine secretion from human macrophages and microglia. J Neuroimmunol 147:56–1
Gargett CE, Wiley JS (1997) The isoquinoline derivative KN-62: a potent antagonist of the P2Z-receptor of human lymphoctytes. Br J Pharmacol 122:911–17
Humphreys BD, Virginio C, Surprenant A et al (1998) Isoquinolines as antagonists of the P2X7 nucleotide receptor: high selectivity for the human versus rat receptor homologues. Mol Pharmacol 54:22–2
Buell G, Chessell IP, Michel AD et al (1998) Blockade of human P2X7 receptor function with a monoclonal antibody. Blood 92:3521–528
Bradford MD, Soltoff SP (2002) P2X7 receptors activate protein kinase (MAPK) downstream of protein kinase C. Biochem J 366:745–55
Amstrup J, Novak I (2003) P2X7 receptor activates extracellular signal-regulated kinases ERK1 and ERK2 independently of Ca2+ influx. Biochem J 374:51–1
Auger R, Motta I, Benihoud K et al (2005) A role for mitogen-activated protein kinaseErk1/2 activation and non-selective pore formation in P2X7 receptor-mediated thymocyte death. J Biol Chem 280:28142–8151
Humphreys BD, Rice J, Kertesy SB et al (2000) Stress-activated protein kinase/JNK activation and apoptotic induction by the macrophage P2X7 nucleotide receptor. J Biol Chem 275:26792–6798
Verhoef PA, Estacion M, Schilling W et al (2003) P2X7 receptor-dependent blebbing and the activation of Rho-effector kinases, caspases, and IL-1β release. J Immunol 170:5728–738
Pfeiffer ZA, Aga M, Prabhu U et al (2004) The neucleotide receptor P2X7 mediates actin reorganization and membrane blebbing in RAW 264.7 macrophages via p38 MAP kinase and Rho. J Leukoc Biol 75:1173–182
Budagian V, Bulanova E, Brovko L et al (2003) Signaling through P2X7 receptor in human T cells involves p56lck, MAP kinases, and transcription factors AP-1 and NF-κB. J Biol Chem 278:1549–560
Adinolfi E, Kim M, Young MT et al (2003) Tyrosine phosphorylation of HSP90 within the P2X7 receptor complex negatively regulates P2X7 receptors. J Biol Chem 278:37344–7351
Feng Y-H, Wang L, Wang Q et al (2005) ATP stimulates GRK-3 phosphorylation and B-arrestin-2-dependent internalization of P2X7 receptor. Am J Physiol 288:C1342–C1356
Kim M, Jian LH, Wilson HL et al (2001) Proteomic and functional evidence for a P2X7 receptor signaling complex. EMBO J 20:6347–358
Ferrari D, Wesselborg S, Baurer MKA et al (1997) Extracellular ATP activates transcription factor NF-kB through the P2Z purinoreceptor by selectively targeting NF-κB p65 (RelA). J Cell Biol 139:1635–643
Ferrari D, Stroh C, Schulze-Osthoff K (1999) P2X7/P2Z purinoreceptor-mediated activation of transcription factor NFAT in microglial cells. J Biol Chem 274:13205–3210
Parvathenani LK, Tertyshnikova S, Creco CR et al (2003) P2X7 mediates superoxide production in primary microglia and is up-regulated in a transgenic mouse model of Alzheimer’s disease. J Biol Chem 278:13309–3317
Garcia-Marcos M, Fontanils U, Aguirre A et al (2005) Role of sodium in mitochondrial membrane depolarization induced by P2X7 receptor activation in submandibular glands. FEBS Lett 579:5407–413
Humphreys BD, Dubyak GR (1996) Induction of the P2X/P2X7 nucleotide receptor and associated phospholipase D activity by lipopolysaccharide and IFNγ in the human THP-1 monocytic cell line. J Immunol 157:5627–637
Mehta VB, Hart J, Wewers MD (2001) ATP-stimulated release of interleukin (IL)-1β and IL-18 requires priming by lipopolysaccharide and is independent of caspase-1 cleavage. J Biol Chem 276:3820–826
Kahlenberg JM, Dubyak GR (2003) Mechanisms of caspase-1 activation by P2X7 receptor-mediated K+ release. Am J Physiol 286:C1100–C1108
North RA (2002) Molecular physiology of P2X receptors. Physiol Rev 82:1013–067
Brough D, Le Feuvre RA, Wheeler RD et al (2003) Ca2+ stores and Ca2+ entry differentially contribute to the release of IL-1β and IL-1α from murine macrophages. J Immunol 170:3029–036
Gudipaty L, Munetz J, Verhoef PA et al (2003) Essential role for Ca2+ in regulation of IL-1β secretion by P2X7 nucleotide receptor in monocytes, macrophages, and HEK293 cells. Am J Phyisol 285:C286–C299
Perregaux DG, Gabel CA (1998) Human monocyte stimulus-coupled IL-1β posttranslational processing: modulation via monovalent cations. Am J Physiol 275:C1538–C1547
Laliberte RE, Eggler J, Gabel CA (1999) ATP treatment of human monocytes promotes caspase-1 maturation and externalization. J Biol Chem 274:36944–6951
Martinon F, Burns K, Tschopp J (2002) The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-1β. Mol Cell 10:417–26
Tschopp J, Martinon F, Burns K (2003) NALPS: a novel protein family involved in inflammation. Nat Rev Mol Cell Biol 4:95–04
Dowds TA, Masumoto J, Zhu L et al (2004) Cryopyrin-induced interleukin 1β secretion in monocytic cells. J Biol Chem 279:21924–1928
Bruey JM, Rruey-Sedano N, Newman R et al (2004) PAN1/NALP2/PYPAF2, an inducible inflammatory mediator that regulates NF-κB and caspase-1 activation in macrophages. J Biol Chem 279:51897–1907
Martinon F, Tschopp J (2004) Inflammatory caspases: linking an intracellular innate immune system to autoinflammatory diseases. Cell 117:561–74
Mariathasan S, Newton K, Monack DM et al (2004) Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf. Nature 430:213–18
MacKenzie A, Wilson HL, Kiss-Toth E et al (2001) Rapid secretion of interleukin-1β by microvesicle shedding. Immunity 8:825–35
Faria RX, DeFarias FP, Alves LA (2005) Are second messengers crucial for opening the pore associated with P2X7 receptor? Am J Physiol 288:C260–C271
Mackenzie AB, Young MT, Adinolfi E et al (2005) Pseudoapoptosis induced by brief activation of ATP-gated P2X7 receptors. J Biol Chem 280:33968–3976
Perregaux DG, Gabel CA (1998) Post-translational processing of murine IL-1: evidence that ATP-induced release of IL-1α and IL-1β occurs via a similar mechanism. J Immunol 160:2469–477
Hamon Y, Luciani M-F, Becq F et al (1997) Interleukin-1β secretion is impaired by inhibitors of the ATP binding cassette transporter, ABC1. Blood 90:2911–915
Bianco F, Pravettoni E, Colombo A et al (2005) Astrocyte-derived ATP induces vesicle shedding and IL-1β release from microglia. J Immunol 174:7268–277
Andrei C, Dazzi C, Lotti L et al (1999) The secretory route of the leaderless protein interleukin 1β involves exocytosis of endolysosome-related vesicles. Mol Biol Cell 10:1463–475
Andrei C, Margiocco P, Poggi A et al (2005) Phospholipases C and A2 control lysosome-mediated IL-1β secretion: implications for inflammatory processes. Proc Natl Acad Sci 101:9745–750
Wiley JS, Dao-Ung LP, Gu BJ et al (2002) A loss-of function polymorphic mutation in the cytolytic P2X7 receptor gene and chronic lymphocytic leukemia: a molecular study. Lancet 359:1114–119
Li CM, Campbell SJ, Kumararatne DS et al (2002) Response heterogeneity of human macrophages to ATP is associated with P2X7 receptor expression but not to polymorphisms in the P2RX7 promoter. FEBS Lett 531:127–31
Zhang LY, Ibbotson RE, Orchard JA et al (2003) P2X7 polymorphism and chronic lymphocytic leukaemia: lack of correlation with incidence, survival and abnormalities of chromosome 12. Leukemia 17:2097–100
Le Stunff H, Auger R, Kanellopoulos J et al (2004) The Pro-451 to Leu polymorphism within the C-terminal tail of P2X7 receptor impairs cell death but not phospholipase D activation in murine thymocytes. J Biol Chem 279:16918–6926
Skarratt KK, Fuller SJ, Sluyter R et al (2005) A 5–intronic splice site polymorphism leads to a null allele of the P2X7 gene in 1–% of the Caucasian population. FEBS Lett 579:2675–678
Cabrini G, Falzoni S, Forchap SL et al (2005) A His-155 to Tyr polymorphism confers gain-of-function to the human P2X7 receptor of human leukemic lymphocytes. J Immunol 175:82–9
Gu BJM, Sluyter R, Skarratt KK et al (2004) An Arg307 to Gln polymorphism within the ATP-binding site causes loss of function of the human P2X7 receptor. J Biol Chem 279:31287–1295
Sluyter R, Shemon AN, Wiley JS (2004) Glu496 to Ala polymorphism in the P2X7 receptor impairs ATP-induced IL-1β release from human monocytes. J Immunol 172:3399–405
Sluyter R, Dalitz JG, Wiley JS (2004) P2X7 receptor polymorphism impairs extracellular adenosine 5–triphosphate-induced interleukin-18 release from human monocytes. Genes Immun 5:588–91
Chessell IP, Hatcher JP, Bountra C et al (2005) Disruption of the P2X7 purinoceptor gene abolishes chronic inflammatory and neuropathic pain. Pain 114:386–96
Joosten LA, Helsen MM, Saxne T et al (1999) IL-1α/β blockade prevents cartilage and bond destruction in murine type II collagen-induced arthritis, whereas TNFα blockade only ameliorates joint inflammation. J Immunol 163:5049–055
Williams RO, Marinova-Mutafchieva L, Feldmann M et al (2000) Evaluation of TNFα and IL-1 blockade in collagen-induced arthritis and comparison with combined anti-TNFα/anti-CD4 therapy. J Immunol 165:7240–245
Kagari T, Doi H, Shimozato T (2002) The importance of IL-1β and TNFα, and the noninvolvement of IL-6, in the development of monoclonal antibody-induced arthritis. J Immunol 169:1459–466
Baxter A, Bent J, Bowers K et al (2003) Hit-to-lead studies: the discovery of potent adamantine amide P2X7 receptor antagonists. Bioorg Med Chem Lett 13:4047–050
Merriman GH, Ma L, Shum P et al (2005) Synthesis and SAR of novel 4,5-diarylimidazolines as potent P2X7 receptor antagonists. Bioorg Med Chem Lett 15:435–38
Romagnoli R, Baraldi PG, Di Virgilio F (2005) Recent progress in the discovery of antagonists acting at P2X7 receptor. Expert Opin Ther Pat 15:271–87
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Gabel, C.A. P2 purinergic receptor modulation of cytokine production. Purinergic Signalling 3, 27–38 (2007). https://doi.org/10.1007/s11302-006-9034-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-006-9034-y