Abstract
Objectives
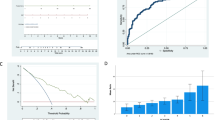
The use of non-intubated uroflowmetry, PVR, prostate volume, and I-PSS are the most commonly used tools for the evaluation of patients with BPH. In this prospective study, we elucidated the correlation between BOO as rated by pressure-flow study in men with LUTS attributed to BPH and those parameters.
Methods
Over a period of 2 years 460 men above the age of 45 years old (mean age 60.46 ± 9.4) were prospectively included in this study. Symptoms were evaluated using the International Prostate Symptom Score, and digital rectal examination, prostate-specific antigen, and transrectal ultrasound were done. The urodynamic evaluation included uroflowmetry, filling cystometry, and voiding cystometry with the plotting of pressure-flow study according to Lin-PURR (Schäfer’s nomogram). The correlation coefficient was calculated between these variables.
Results
The correlation of other objective parameters with total score was not much better. The Spearman’s correlation coefficient were − 0.09, 0.07 and − 0.1 for prostate weight, post voiding residual urine and maximum free flow rate respectively. Correlations between Schäfer’s grade and Qmax, PVR and prostate volume were found to be weak to fair correlation (r values were − 0.4, 0.18, and 0.39 respectively).
Conclusion
Objective non-invasive parameters most commonly used in the evaluation of men with LUTS attributed to BPH have limited correlation with obstruction, as diagnosed by pressure flow nomogram.




Similar content being viewed by others
Data availability
Available.
Abbreviations
- BPH:
-
Benign prostatic hyperplasia
- LUTS:
-
Lower urinary tract symptoms
- BOO:
-
Bladder outflow obstruction
- I-PSS:
-
International prostate symptom score
- Q max :
-
Maximum flow rate
- P det Q max :
-
Detrusor pressure at maximum flow
- Lin PURR:
-
Linear passive urethral resistance relation
- PVR:
-
Post-voiding residual urine
- TRUS:
-
Transrectal ultrasound
- DRE:
-
Digital rectal examination
- PSA:
-
Prostate-specific antigen
References
Garraway WM, Collins GN, Lee RJ (1991) High prevalence of benign prostatic hypertrophy in the community. Lancet 338:469–471
Maruschke M, Protzel C, Hakenberg OW (2009) How to make the diagnosis of benign prostatic disease. Eur Urol Suppl 8:490–495
Reynard JM, Yang Q, Donovan JL, Peters TJ, Schafer W, de la Rosette JJ, Dabhoiwala NF, Osawa D, Lim AT, Abrams P (1998) The ICS-‘BPH’ Study: uroflowmetry, lower urinary tract symptoms and bladder outlet obstruction. Br J Urol 82(5):619–623
Kuo HC (1999) Clinical prostate score for diagnosis of bladder outlet obstruction by prostate measurements and uroflowmetry. Urology 54(1):90–96
Terris MK, Stamey TA (1991) Determination of prostate volume by transrectal ultrasound. J Urol 145:984–987
Mangera A, Chapple C (2014) Modern evaluation of lower urinary tract symptoms in 2014. Curr Opin Urol 24:15–20
Griffiths DJ (1996) Pressure- flow studies of micturition. Urol Clin N Am 23:279–297
Schäfer W, Rubben H, Noppeney R, Deutz F-J (1989) Obstructed and unobstructed prostatic obstruction. W J Urol 6:198–203
Schäfer W (1983) The contribution of the bladder outlet to the relation between pressure and flow during micturition. In: Hinman F (ed) Benign prostatic hypertrophy. Springer-Verlag, New York, pp 470–482
Abrams P, Blaivas JB, Stanton SL, Andersen JT (1989) The standardization of terminology of lower urinary tract function W. J Urol 6:233–245
Schäfer W, Abrams P, Liao L et al (2002) Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 21(3):261–274
Wadie BS, Ibrahim EH, de la Rosette JJ, Gomha MA, Ghoneim MA (2001) The relationship of the International Prostate Symptom Score and objective parameters for diagnosing bladder outlet obstruction. Part I: when statistics fail. J Urol 165:32–34
Wadie BS, el-HE E, Gomha MA (2002) The relationship of detrusor instability and symptoms with objective parameters used for diagnosing bladder outlet obstruction: a prospective study. J Urol 168:132–134
Colton T (1974) Regression and correlation. In: Colton T (ed) Statistics in medicine. Little, Brown and Company, Boston, pp 189–217 (Chapt.6)
Bosch JLHR, Hop WCJ, Kirkels WJ, Schröder FH (1995) The International Prostate Symptom Score in a community- based sample of men between 55 and 74 years of age: prevalence and correlation of symptoms with age, prostate volume, flow rate, and residual urine volume. Br J Urol 75(5):622–630
Nitti VW, Kim Y, Combs AJ (1994) Correlation of the American Urological Association symptom index in patients with suspected benign prostatic hyperplasia. Neurourol Urodyn 13(5):521–527
Netto NR Jr, D’Ancona CAL, de Lima ML (1996) Correlation between the International Prostate Symptom Score and a pressure-flow study in the evaluation of symptomatic benign prostatic hyperplasia. J Urol 155(1):200–202
Rosier PFWM, de Wildt MJAM, Wijkstra H, Debruyne FFMJ, de La Rosette JMCH (1996) Clinical diagnosis of bladder outlet obstruction in patients with benign prostatic enlargement and lower urinary tract symptoms: development and urodynamic validation of a clinical prostate score for the objective diagnosis of bladder outlet obstruction. J Urol 155(5):1649–1654
Ko DSC, Fenster HN, Chambers K, Sullivan L, Jens M, Goldenberg SL (1995) The correlation of multichannel urodynamic pressure-flow studies and the American Urological Association symptom index in the evaluation of benign prostatic hyperplasia. J Urol 154:396–398
van Venrooij GEPM, Boon TA (1996) The value of symptom score, quality of life score, maximal urinary flow rate, residual volume and prostate size for the diagnosis of obstructive benign prostatic hyperplasia: a urodynamic analysis. J Urol 155(6):2014–2018
Funding
Institutional.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wadie, B.S. How correlated is BOO with different objective parameters commonly used in evaluation of BPH: a prospective study. Int Urol Nephrol 53, 635–640 (2021). https://doi.org/10.1007/s11255-020-02707-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02707-4