Abstract
Valvular heart disease is associated with an increased thromboembolic risk. Impaired fibrinolysis was reported in severe aortic stenosis (AS). Little is known about fibrinolysis in mitral stenosis (MS). We sought to compare fibrinolysis impairment in AS and MS. We studied 121 individuals scheduled for elective aortic valve (AV) or mitral valve (MV) surgery for AS (n = 76) or MS (n = 45), in order to compare fibrinolysis impairment. Fibrinolytic capacity was assessed by determination of clot lysis time (t50%) and fibrinolysis inhibitors, including plasma plasminogen activator inhibitor-1 (PAI-1) antigen (PAI-1:Ag) and activity, thrombin-activatable fibrinolysis inhibitor (TAFI) antigen and activity. Prolonged t50% (+ 29%), elevated TAFI activity (+ 12%), TAFI:Ag (+ 21%), and PAI-1:Ag (+ 84%) were observed in patients with MS, compared with those with AS. t50% Correlated with mean and maximal MV gradients (r = 0.43, p < 0.0001 and r = 0.39, p < 0.0001, respectively), but not with AV gradients. Mean and maximal MV gradients correlated with TAFI activity and PAI:Ag. Patients with permanent atrial fibrillation (AF; 35 with MS and 5 with AS) had longer t50% (by 22%, p = 0.0002) and higher PAI-1:Ag (by 74%, p < 0.0001) than the remainder. In the whole group, postoperative drainage volumes correlated inversely with PAI-1:Ag (r = − 0.22, p = 0.02). MS is associated with more pronounced impairment of global fibrinolytic capacity than AS at the stage of surgical intervention, which is in part driven by AF. Our findings suggest that hypofibrinolysis might be implicated in the progression of MS and its thromboembolic complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
Valvular heart disease is associated with increased thromboembolic risk
-
Degenerative mitral stenosis is associated with more pronounced impairment of global fibrinolytic capacity than aortic stenosis at the stage of surgical intervention
-
Atrial fibrillation contributes to fibrinolysis impairment in mitral stenosis
-
The role of fibrinolysis in pathology and progression of valvular disorders and their thromboembolic complications needs to be investigated
Introduction
Valvular heart disease (VHD) remains a key public health problem worldwide. Degenerative aortic stenosis (AS) is common in developed countries, and its prevalence increases with age [1]. The mechanisms involved in the development of AS resemble the ones involved in the development of coronary artery atherosclerosis [2]. Mitral stenosis (MS), on the other hand, is related to the structural abnormality of the mitral valve (MV) apparatus, and can be a distant sequel of rheumatic fever, or may result from severe non-rheumatic degenerative mitral annular calcification [3]. Mitral annular calcification is present in up to 10% of elderly patients, and MS develops in 1–2% of this group [3, 4]. It has been shown that atherosclerotic risk factors are associated with mitral annular calcification leading to MS [5]. Based on the 2015 Society of Thoracic Surgeons Adult Cardiac Surgery Database Report, isolated aortic valve replacement (AVR) was performed in 21,921 patients, while isolated mitral valve replacement (MVR) in 5180 cases in United States alone [6].
Blood coagulation leads to thrombin-mediated conversion of fibrinogen to fibrin. Fibrin clots composed of tightly packed thin fibers with small pores are relatively resistant to lysis [7] and such prothrombotic clot phenotype has been shown in multiple disease states, such as myocardial infarction (MI) [8] or ischemic stroke [9]. Although the research on AS is most frequently focused on calcification, in 2013 our group documented impaired fibrinolysis in 74 patients with severe AS, evidenced by prolonged plasma fibrin clot lysis time (CLT) and increased plasma plasminogen activator inhibitor-1 (PAI-1), as compared to controls [10]. CLT was positively correlated with the valve leaflet thickness, the degree of valve calcification, valvular fibrin and PAI-1 expression [10].
Impaired fibrinolysis is usually driven by increased levels and/or enhanced function of its inhibitors. PAI-1 is a key regulator of fibrinolysis that controls the plasmin-generating activity of tissue-type plasminogen activator and urokinase-type plasminogen activator [11]. PAI-1 expression is found in as many as in 69% of the human AS valves [12]. Another fibrinolysis inhibitor, thrombin activatable fibrinolysis inhibitor (TAFI), which cleaves C-terminal lysine and arginine residues from partially degraded fibrin, thereby attenuating efficient plasminogen activation, has also been shown to be elevated in AS patients [13]. Clinical relevance of varying levels of circulating fibrinolysis inhibitors in VHD is unclear due to the paucity of data. It has been reported in a study on 28 individuals with severe MS that blood coagulation activation and fibrinolytic activity assessed using plasma D-dimer levels were increased in MS, compared with controls [14]. Marin et al. showed impaired fibrinolysis in 24 MS patients, compared with 18 controls, as reflected by elevated PAI-1 (both in patients with atrial fibrillation [AF] and in sinus rhythm), without assessment of the overall fibrinolytic plasma capacity [15].
To the best of our knowledge, there are no studies comparing the functional status of the fibrinolytic system between different degenerative valvular disorders. We sought to compare the fibrinolytic system activity in patients with late-stage degenerative AS (a degenerative valvular disease with high-velocity flow) with patients with degenerative MS (a group with a stenotic valvular condition with lower flow velocity). A multimodal approach was employed, which included assessment of global fibrinolytic capacity and fibrinolysis inhibitors.
Methods
Patients
From February 2013 to April 2014 we recruited 121 individuals scheduled for elective valvular surgery due to degenerative AS or MS. All patients were assessed preoperatively by a local ‘heart team’, and the surgery was conducted according to the ‘heart team’ indication.
The exclusion criteria were: rheumatic etiology of VHD (to exclude the confounding effect of inflammation), ongoing infective endocarditis, combined AV and MV replacement procedure, emergency surgery, root dilation requiring aortic surgery, prior cardiac surgery, MI or percutaneous coronary intervention (PCI) followed by dual antiplatelet therapy within 1 month prior to enrolment, renal failure (serum creatinine > 177 µmol/L), prior bleeding diathesis, arterial or venous thromboembolic events within the previous 6 months, known cancer, any chronic inflammatory disease. Concomitant CABG, as well as current anticoagulant therapy were not used as exclusion criteria. Necessity for concomitant valve repair (due to secondary mitral regurgitation [MR] in AS, and tricuspid regurgitation [TR] in MS) was not used as an exclusion criterion. In-hospital cardiovascular death was defined as death due to cardiovascular diseases, occurring during the same hospitalization.
Echocardiography was performed by an experienced cardiologist on a Toshiba APLIO 80 (Toshiba, Tokyo, Japan) ultrasound machine. AS was defined as severe when mean transvalvular pressure gradient was ≥ 40 mmHg and/or AV area was ≤ 1 cm2. All enrolled AS patients had to be symptomatic. MS was deemed a surgical indication in a symptomatic patient when MV area was ≤ 1.5 cm2 [16]. Valve regurgitation was graded with color Doppler flow analysis using the following scale: none (0), trivial (1), mild (2), moderate (3) and severe (4). If a patient was on oral vitamin K antagonist (VKA) therapy prior to operation, it was stopped 5 days before admission, and perioperative bridging with low molecular weight heparin (LMWH) was initiated. A regimen of 1 mg/kg enoxaparin twice daily was applied in all cases.
The study was performed in accordance with the Declaration of Helsinki, and received approval of the Jagiellonian University Ethical Committee. All patients provided their written informed consent.
Operative management
All patients underwent standardized anaesthesia and received median sternotomy. Cardio-pulmonary bypass (CPB) was performed at moderate hypothermia (esophageal temperature, 32 °C) using a non-pulsatile roller pump (Jostra Medizintechnik AG, Hirrlingen, Germany) and a 40 µm arterial blood filter (Jostra Medizintechnik AG, Hirrlingen, Germany), with blood flow at 2.0–2.4 l/min/m2, and mean arterial pressure at 40–60 mmHg. Aortic valve anatomy was confirmed intraoperatively by a surgeon in AS. Tranexamic acid was administered in two doses (20 mg/kg i.v. after sternotomy, and 20 mg/kg i.v. after the end of CPB) in all cases. All patients were transferred to the intensive care unit (ICU) for postoperative ventilation, and extubated following standard criteria.
Laboratory investigations
Fasting blood samples were collected from an antecubital vein with minimal stasis at 6–8 a.m. on the day of surgery, prior to the onset of any surgery-related procedures. Plasma samples were centrifuged within 30 min of collection, frozen, and stored in aliquots at − 80 °C until assayed. Routine methods were used for standard laboratory parameters. Commercially available enzyme-linked immunoabsorbent assays were used to determine plasma PAI-1 antigen (PAI-1:Ag; Hyphen, Neuville, France), PAI-1 activity (PAI-1:Act; American Diagnostica, Stamford, CT, USA) and TAFI antigen (Stachrom TAFI, Diagnostica Stago, Asnieres, France). Plasma TAFI activity was measured by a chromogenic assay using the ACTICHROME® Plasma TAFI Activity Kit (American Diagnostica, Stamford, CT, USA). We also measured activated and inactivated TAFI antigen in plasma (TAFIa/TAFIai; Diagnostica Stago, Asnieres, France), plasmin-α-2-antiplasmin complexes (PAP; DRG Instruments, Marburg, Germany) and platelet factor 4 (PF4; R&D Systems, Minneapolis, MN, USA).
Clot lysis assay
Plasmin-mediated fibrinolysis in the presence of recombinant tissue plasminogen activator (rtPA) (Boehringer Ingelheim, Ingelheim, Germany) was evaluated as previously described [17, 18]. Briefly, 100 µL of citrated plasma was diluted with 100 µL of a buffer (0.05 mol/L Tris–HCl, 0.15 mol/L NaCl, pH 7.4), containing 20 mmol/L calcium chloride, 1 U/mL human thrombin (Sigma-Aldrich), and 14 µmol/L rtPA. The assembly kinetics was monitored by spectrophotometry at 405 nm, in duplicate. Lysis time was defined as the time required for a 50% decrease in fibrin clot absorbance (t50%) and was chosen as a marker of the clot susceptibility to fibrinolysis. The interassay and intraassay coefficients of variation were below 6%.
Statistical analysis
The study was powered to have an 80% chance of detecting a 25% intergroup difference in t50% using a p-value of 0.05, based on the values of these parameters in the published article [19]. In order to demonstrate such a difference or greater in this variable, 20 patients were required in each group. The patient enrollment continued until a sufficient number of MS patients was met. Continuous variables were presented as mean ± standard deviation (SD) or median and quartiles, as appropriate. Categorical variables were presented as counts and percentages. The Shapiro–Wilk test was used to test the normality of continuous variables. To examine the differences between two independent groups Student’s t-test or Mann–Whitney U test were used, as appropriate. The χ2 test or Fischer’s exact test was used for categorical variables. To assess linear correlation between variables, the Pearson correlation coefficient (Pearson’s r) for normally distributed variables or Spearman’s rank correlation coefficient (Spearman’s rho) for non-normally distributed variables were calculated. Linear regression was used to test the influence of MS, AF and VKA use on t50%. These variables were tested in simple regression, and then put together into a multiple model. Statistical analysis was performed with STATISTICA 12.0 (StatSoft, Tulsa, OK). Two sided p-values < 0.05 were considered statistically significant.
Results
Patient characteristics
A total of 97 patients (46% men) with preserved left ventricular function were included in the study. Seventy-six patients (63%) underwent surgery for AS (26 had a bicuspid valve), and 45 (37%) for MS, and the clinical and echocardiographic characteristics of both groups are presented in Table 1. MS patients had lower BMI, were more often diagnosed with AF, had a history of stroke and were treated with VKA, while AS patients more often had hypertension, hypercholesterolemia and CAD, and received aspirin, ACEI and statins. MS patients were in higher New York Heart Association class, had mildly decreased left ventricular systolic function, and demonstrated higher values of INR and APTT (Table 1.).
Operative and postoperative characteristics are presented in Table 2. MS patients required a shorter aortic cross-clamping, and more frequently received a mechanical valve, but did not differ from AS patients in terms of re-exploration for bleeding, transfusions or early mortality.
Fibrinolysis
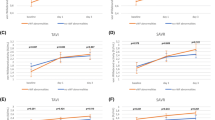
In MS, t50% was prolonged (+ 29%), TAFI activity (+ 12%), TAFI:Ag (+ 21%), and PAI-1:Ag (+ 69%) were elevated, when compared with AS subjects (Fig. 1; Table 2.). No differences in fibrinogen, d-dimer or PAP levels were noted. In the whole cohort (n = 121), t50%, TAFI activity and PAI-1:Ag positively correlated with MV (but not AV) gradients (Fig. 2.). t50% correlated also with MR degree (r = 0.29, p = 0.001).
In all patients (n = 121), there was a positive association between t50% and PAI-1:Ag (r = 0.21, p = 0.02), and negative between t50% and PAP (r = − 0.45, p < 0.0001). PAI-1:Ag and PAP correlated with BMI (r = 0.28, p = 0.002 and r = 0.22, p = 0.01, respectively).
Preoperative APTT correlated inversely with PAI-1:Ag (r = − 0.20, p = 0.03) and TAFIa/TAFIai (r = − 0.19, p = 0.04).
Preoperative fibrinogen was correlated with TAFI:Ag (r = 0.18, p = 0.047) and TAFIa/TAFIai (r = 0.25, p = 0.008). TAFIa/TAFIai was also associated with creatinine (r = 0.27, p < 0.004) and age (r = 0.45, p < 0.0001). In AV patients, patients with bicuspid aortic valve, compared with those with normal anatomy, apart from being younger (63 [60–67] vs. 72 [64–76] years, respectively, p = 0.002), and having lower body mass index (26.0 [23.8–29.4] vs. 28.9 [26.4–32.0] kg/m2, respectively, p = 0.006), had lower TAFI activity (36.6 ± 11.0 vs. 43.3 ± 14.4%, respectively, p = 0.046), but did not differ regarding t50% and other parameters.
Comorbidities
Patients with permanent AF (35 with MS and 5 with AS) had longer t50% than individuals without documented AF (16.0 [13.1–22.6] vs. 13.1 [10.1–16.3] min, p = 0.0002) and higher PAI-1:Ag (23.4 [15.9–31.4] vs. 13.4 [9.7–19.4] ng/mL, p < 0.0001). Patients with paroxysmal AF (n = 5) had higher PAI-1:Ag than individuals without documented AF (24.6 [19.0–25.2] vs. 13.4 [9.7–19.4] ng/mL, p = 0.03).
To verify the influence of MS on t50% in the presence of persistent AF and VKA use, linear regression was utilized. In univariate analysis, all variables were significant (MS: b = 4.91, adjusted R2 = 0.17, p < 0.0001; AF: b = 2.54, adjusted R2 = 0.06, p = 0.005; VKA: b = 4.50, adjusted R2 = 0.14, p < 0.0001). In multivariate analysis (final model, adjusted R2 = 0.18, p < 0.0001), only MS was the predictor of t50% (b = 3.42, p = 0.01).
Surgical outcomes
There were no intergroup differences in the early mortality rate, re-exploration for bleeding and the length of ICU stay. The fatal cases (n = 7) did not differ from survivors with regard to TAFI and t50%, but had lower PAI-1 activity (5.3 [4.1–12.6] vs. 11.5 [6.5–19.3] IU/dL, respectively, p = 0.04).
A median postoperative chest tube drainage volume was 440 ml with no AS–MS intergroup difference (Table 2.). In patients who required re-exploration for bleeding the median chest-tube output was more than twofold higher than in remaining patients (1120 [650–2000] vs. 420 [320–590] mL, respectively; p = 0.0002). In the whole group (n = 121) the postoperative drainage volumes correlated inversely with platelet count (r = − 0.29, p = 0.002), BMI (r = − 0.25, p = 0.007), fibrinogen (r = − 0.26, p = 0.006) and PAI-1:Ag (r = − 0.22, p = 0.02). Patients with high drainage volumes (≥ 1000 mL; n = 8, 7%), compared with those with lower volumes (n = 113) had lower PAI-1:Ag (by 40%, p = 0.02), but there were no differences in any other parameters.
Discussion
The novel finding of this study is that individuals suffering from MS (at the stage requiring surgical intervention) have more impaired global efficiency of fibrinolysis, compared with subjects with AS, as reflected by longer t50%, higher activity of TAFI, and higher levels of PAI-1.
We report a positive association of t50% with both maximal and mean transvalvular MV gradients, as well as with the degree of MR. We also observed the association of TAFI activity and PAI-1:Ag with transvalvular MV gradients. These associations point to the connection between MS and impairment of fibrinolysis.
While several tests to assess global plasma fibrinolytic activity are available, we used a plasma-based test, in which a thrombin-induced fibrin clot is lysed by exogenously added rt-PA at relatively high concentrations. This approach was successfully applied in previous papers [17, 18, 20, 21]. In contrast to the assay previously used by our group in AS patients [10], the current method does not use tissue factor, and the rtPA concentrations are higher. Based on previous reports, t50% may be more sensitive to detect the impact of PAI-1 on fibrin clot properties [20]. Our findings supported this observation by showing that PAI-1:Ag is positively correlated with t50% values.
In patients with VHD, we found that inhibition of fibrinolysis was modulated most notably by the presence of AF, a prothrombotic condition, involving increased thrombin generation and fibrinogen concentrations [22, 23]. Marin et al. reported higher levels of PAI-1 in patients with MS who also had AF, as compared with MS patients in normal sinus rhythm [15]. We observed higher PAI-1 levels, along with prolonged t50%, in subjects with AF (TAFI activity was unaffected by AF, and modulated only by MS incidence). Our findings are in line with the recent paper by Drabik et al., who reported prolonged CLT and increased PAI-1 levels in subjects with non-valvular AF [24]. Impaired fibrinolysis, improved by oral anticoagulants, was also reported by other investigators exploring fibrinoysis in AF [25, 26]. Only few patients with progressed MS will present without AF, and AF contributes to blood stasis in the left atrium in the setting of MV stenosis—another component in Virchow’s triad equation. The observation that even in MS patients AF is a potent enough factor to significantly alter fibrinolysis provides additional evidence for the necessity of anticoagulation in this disorder. Nevertheless, MS was a predictor of t50% independently of AF in this study.
The preoperative history of VKA therapy in both groups warrants a comment. While the groups differed regarding VKA use, it is unlikely that VKAs influenced the results of t50% test, markedly elevated in MS patients. Previously, the permeability of the fibrin network was shown to rise in parallel to elevations of INR and shortening of CLT in AF patients [25], thus, it could be expected that in the setting of VKA use, t50% would be shorter. Also LMWHs prolong clot formation and increase the clot susceptibility to lysis [27], and as all anticoagulated patients in this study received LMWH bridging prior to operation, t50% shortening could be expected. That notwithstanding, patients with MS, who in this study were most often subjected to anticoagulation, also had the most “prothrombotic” fibrin clot phenotype (and longest t50%). One might speculate that the effects of VKAs and LMWHs on clot susceptibility to lysis are, arguably, abolished by MS and AF. On the other hand, our findings point to the importance of anticoagulation in MS, especially with concomitant AF. The prothrombotic state, as presented by us, is associated with MS, to some extent irrespectively of AF. Further studies are needed to verify the hypothesis that patients with advanced MS, but with no documented AF, would benefit from anticoagulant therapy, and to indicate which treatment modality would be most beneficial.
Furthermore, plasma PAI-1 was associated with enhanced bleeding after cardiac surgery in a study by Ozolina et al. on 79 cardiosurgical patients (as few as 29 underwent valvular surgery) [28]. We demonstrated that plasma PAI-1:Ag is inversely correlated with chest-tube output. Yet, even with significant differences in PAI-1:Ag between AS and MS patients, we failed to show any differences in drainage volumes. Our results confirm that fibrinolysis is a contributor to post-operative blood loss after cardiac surgery, but not potent enough to reveal clinical effects after elective valvular surgery. It should be mentioned that the bleeding tendency in AS [29] is largely driven by the imbalance in von Willebrand factor high molecular weight multimers [30]. In our study, the postoperative blood loss was also associated with preoperative fibrinogen level, PLT and BMI. Among the factors like fibrinogen or PLT, the cardiosurgical bleeding and transfusion risk scores consequently list low BMI/body weight as a risk factor [31]. Interestingly, PAI-1:Ag and BMI were positively associated in our study, and this association is in line with previous reports [32]. Inhibition of fibrinolysis has long been a target of strategies aimed at bleeding reduction in cardiac surgery, but there is no obvious consensus on the antifibrinolytic therapy in cardiac surgery. Our results suggest that different groups of patients might require a different antifibrinolytic regimen for optimal outcomes, with adjustment according to the diagnosis-dependent activity of fibrinolysis.
In the current report, along with t50%, we studied TAFI, another important fibrinolysis inhibitor, using three assays [33]. This aspect of fibrinolyis was not studied yet in the context of VHD. TAFI:Ag measures all forms of TAFI in plasma: pro-TAFI, active and inactivated TAFI. TAFI:Act reflects only the active form of TAFI, while TAFIa/TAFIai reflects the ratio of active and inactivated TAFI levels (the latter: form of TAFI following the completion of its biological function of C-terminal arginine and lysine cleavage from partially degraded fibrin). A novel observation in the current study is that the MS is associated with higher TAFI activity than AS, and this finding is independent of AF presence. The similar TAFIa/TAFIai values might be explained by “compensatory” changes in inactivated TAFI levels in both groups, leading to similar ratios. A role of TAFI in hypofibrinolysis in valvular disorders warrants further studies.
Limitations
The MS and AS groups are representative to patients in everyday practice, however they were not matched, and differed in some aspects. MS subjects are underrepresented, although this reflects the trends in open heart surgery, with a high prevalence of AS in patients requiring surgical intervention [6]. Still, small sample size of MS patients might be a reason for underpowering. Long term follow-up to seek for thrombotic complications was beyond the scope of the current study. Despite sharing many risk factors [2, 5], degenerative AS and MS likely differ in the underlying pathology. Most MS patients had AF.
Conclusions
We demonstrated that degenerative MS is associated with more pronounced impairment of global fibrinolytic capacity than AS at the stage of surgical intervention. AF likely contributes to fibrinolysis impairment in MS, but the role of fibrinolysis in valvular disorders in terms of progression of the disease and thromboembolic complications requires further studies. The relationship between the preoperative fibrinolysis activation, antifibrinolytic treatment, and postoperative outcomes in cardiac surgery needs to be investigated.
References
Carabello BA, Paulus WJ (2009) Aortic stenosis. Lancet 373:956–966. https://doi.org/10.1016/S0140-6736(09)60211-7
Yetkin E, Waltenberger J (2009) Molecular and cellular mechanisms of aortic stenosis. Int J Cardiol 135:4–13. https://doi.org/10.1016/j.ijcard.2009.03.108
Nishimura RA, Vahanian A, Eleid MF, Mack MJ (2016) Mitral valve disease–current management and future challenges. Lancet 387:1324–1334. https://doi.org/10.1016/s0140-6736(16)00558-4
Kanjanauthai S, Nasir K, Katz R, Rivera JJ, Takasu J, Blumenthal RS, Eng J, Budoff MJ (2010) Relationships of mitral annular calcification to cardiovascular risk factors: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 213:558–562. https://doi.org/10.1016/j.atherosclerosis.2010.08.072
Sud K, Agarwal S, Parashar A, Raza MQ, Patel K, Min D, Rodriguez LL, Krishnaswamy A, Mick SL, Gillinov AM, Tuzcu EM, Kapadia SR (2016) Degenerative mitral stenosis: unmet need for percutaneous interventions. Circulation 133:1594–1604. https://doi.org/10.1161/circulationaha.115.020185
Society of Thoracic Surgeons Executive Summary Adult Cardiac Surgery Database for 2015. http://www.sts.org/sites/default/files/documents/2015Harvest4_ExecutiveSummary.pdf
Undas A (2014) Fibrin clot properties and their modulation in thrombotic disorders. Thromb Haemost 112:32–42. https://doi.org/10.1160/th14-01-0032
Undas A, Szuldrzynski K, Stepien E, Zalewski J, Godlewski J, Tracz W, Pasowicz M, Zmudka K (2008) Reduced clot permeability and susceptibility to lysis in patients with acute coronary syndrome: effects of inflammation and oxidative stress. Atherosclerosis 196:551–557. https://doi.org/10.1016/j.atherosclerosis.2007.05.028
Undas A, Podolec P, Zawilska K, Pieculewicz M, Jedlinski I, Stepien E, Konarska-Kuszewska E, Weglarz P, Duszynska M, Hanschke E, Przewlocki T, Tracz W (2009) Altered fibrin clot structure/function in patients with cryptogenic ischemic stroke. Stroke 40:1499–1501. https://doi.org/10.1161/STROKEAHA.108.532812
Natorska J, Wypasek E, Grudzien G, Sadowski J, Undas A (2013) Impaired fibrinolysis is associated with the severity of aortic stenosis in humans. J Thromb Haemost 11:733–740. https://doi.org/10.1111/jth.12122
Nordt TK, Peter K, Ruef J, Kubler W, Bode C (1999) Plasminogen activator inhibitor type-1 (PAI-1) and its role in cardiovascular disease. Thromb Haemost 82(Suppl 1):14–18
Kochtebane N, Alzahrani AM, Bartegi A (2014) Expression of uPA, tPA, and PAI-1 in calcified aortic valves. Biochem Res Int. https://doi.org/10.1155/2014/658643
Kolasa-Trela R, Fil K, Wypasek E, Undas A (2015) Exercise stress testing enhances blood coagulation and impairs fibrinolysis in asymptomatic aortic valve stenosis. J Cardiol 65:501–507. https://doi.org/10.1016/j.jjcc.2014.07.019
Zaki A, Salama M, El Masry M, Abou-Freikha M, Abou-Ammo D, Sweelum M, Mashhour E, Elhendy A (2000) Immediate effect of balloon valvuloplasty on hemostatic changes in mitral stenosis. Am J Cardiol 85:370–375
Marin F, Roldan V, Monmeneu JV, Bodi V, Fernandez C, de Burgos FG, Marco P, Sogorb F (1999) Prothrombotic state and elevated levels of plasminogen activator inhibitor-1 in mitral stenosis with and without atrial fibrillation. Am J Cardiol 84:862–864
Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Baron-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Lung B, Lancellotti P, Pierard L, Price S, Schafers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M (2012) Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg 42:S1–44. https://doi.org/10.1093/ejcts/ezs455
Gajos G, Konieczynska M, Zalewski J, Undas A (2015) Low fasting glucose is associated with enhanced thrombin generation and unfavorable fibrin clot properties in type 2 diabetic patients with high cardiovascular risk. Cardiovasc Diabetol 14:44. https://doi.org/10.1186/s12933-015-0207-2
Undas A, Zalewski J, Krochin M, Siudak Z, Sadowski M, Pregowski J, Dudek D, Janion M, Witkowski A, Zmudka K (2010) Altered plasma fibrin clot properties are associated with in-stent thrombosis. Arterioscler Thromb Vasc Biol 30:276–282. https://doi.org/10.1161/atvbaha.109.194936
Zabczyk M, Hondo L, Krzek M, Undas A (2013) High-density cholesterol and apolipoprotein AI as modifiers of plasma fibrin clot properties in apparently healthy individuals. Blood Coagul Fibrinolysis 24:50–54. https://doi.org/10.1097/MBC.0b013e32835a083c
Gronostaj K, Richter P, Nowak W, Undas A (2013) Altered plasma fibrin clot properties in patients with digestive tract cancers: links with the increased thrombin generation. Thromb Res 131:262–267. https://doi.org/10.1016/j.thromres.2012.11.033
Ząbczyk M, Undas A (2017) Plasma fibrin clot structure and thromboembolism: clinical implications. Pol Arch Intern Med 127:873–881. https://doi.org/10.20452/pamw.4165
Roldan V, Marin F, Blann AD, Garcia A, Marco P, Sogorb F, Lip GY (2003) Interleukin-6, endothelial activation and thrombogenesis in chronic atrial fibrillation. Eur Heart J 24:1373–1380
Li-Saw-Hee FL, Blann AD, Gurney D, Lip GY (2001) Plasma von Willebrand factor, fibrinogen and soluble P-selectin levels in paroxysmal, persistent and permanent atrial fibrillation. Effects of cardioversion and return of left atrial function. Eur Heart J 22:1741–1747. https://doi.org/10.1053/euhj.2000.2531
Drabik L, Wolkow P, Undas A (2015) Denser plasma clot formation and impaired fibrinolysis in paroxysmal and persistent atrial fibrillation while on sinus rhythm: association with thrombin generation, endothelial injury and platelet activation. Thromb Res 136:408–414. https://doi.org/10.1016/j.thromres.2015.05.028
Zabczyk M, Blomback M, Majewski J, Karkowski G, Wallen HN, Undas A, He S (2015) Assays of fibrin network properties altered by VKAs in atrial fibrillation - importance of using an appropriate coagulation trigger. Thromb Haemost 113:851–861. https://doi.org/10.1160/th14-07-0591
Zabczyk M, Majewski J, Lelakowski J (2011) Thromboembolic events are associated with prolonged clot lysis time in patients with permanent atrial fibrillation. Pol Arch Med Wewn 121:400–407
Konigsbrugge O, Weigel G, Quehenberger P, Pabinger I, Ay C (2018) Plasma clot formation and clot lysis to compare effects of different anticoagulation treatments on hemostasis in patients with atrial fibrillation. Clin Exp Med. https://doi.org/10.1007/s10238-018-0490-9
Ozolina A, Strike E, Jaunalksne I, Krumina A, Bjertnaes LJ, Vanags I (2012) PAI-1 and t-PA/PAI-1 complex potential markers of fibrinolytic bleeding after cardiac surgery employing cardiopulmonary bypass. BMC Anesthesiol 12:27. https://doi.org/10.1186/1471-2253-12-27
Vincentelli A, Susen S, Le Tourneau T, Six I, Fabre O, Juthier F, Bauters A, Decoene C, Goudemand J, Prat A, Jude B (2003) Acquired von Willebrand syndrome in aortic stenosis. N Engl J Med 349:343–349. https://doi.org/10.1056/NEJMoa022831
Natorska J, Mazur P, Undas A (2016) Increased bleeding risk in patients with aortic valvular stenosis: from new mechanisms to new therapies. Thromb Res 139:85–89. https://doi.org/10.1016/j.thromres.2016.01.016
Vuylsteke A, Pagel C, Gerrard C, Reddy B, Nashef S, Aldam P, Utley M (2011) The Papworth Bleeding Risk Score: a stratification scheme for identifying cardiac surgery patients at risk of excessive early postoperative bleeding. Eur J Cardiothorac Surg 39:924–930. https://doi.org/10.1016/j.ejcts.2010.10.003
Verschuur M, Jellema A, Bladbjerg EM, EJ MF, Mensink RP, Moller L, Vos HL, de Maat MP (2005) The plasminogen activator inhibitor-1 (PAI-1) promoter haplotype is related to PAI-1 plasma concentrations in lean individuals. Atherosclerosis 181:275–284. https://doi.org/10.1016/j.atherosclerosis.2005.01.036
Mosnier LO, von dem Borne PA, Meijers JC, Bouma BN (1998) Plasma TAFI levels influence the clot lysis time in healthy individuals in the presence of an intact intrinsic pathway of coagulation. Thromb Haemost 80:829–835
Acknowledgements
This work was supported by a grant from the Polish Ministry of Science (N N402 383338 to Anetta Undas) and a Grant from the National Science Centre (2012/05/N/NZ5/00846 to Piotr Mazur).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures were in accordance with the ethical standards of the institutional ethical committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mazur, P., Myć, J., Natorska, J. et al. Impaired fibrinolysis in degenerative mitral and aortic valve stenosis. J Thromb Thrombolysis 46, 193–202 (2018). https://doi.org/10.1007/s11239-018-1687-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-018-1687-1