Abstract
Do physicians behave rationally when facing a new disease? This study assesses physicians’ ambiguity attitudes towards the future severity of the COVID-19 pandemic in its early stages and the financial market in the US using an incentive-compatible online experiment. Our findings indicate that physicians demonstrate significant deviations from expected utility, characterized by a modest degree of ambiguity aversion and pronounced levels of likelihood insensitivity. While physicians generally show less insensitivity to uncertainty compared to the general public, both groups exhibited similar levels of irrationality when dealing with the ambiguity surrounding the COVID-19 severity. These results underscore the necessity for debiasing strategies among medical professionals, especially in managing real-world uncertainties, with a specific focus on mitigating likelihood insensitivity.
Similar content being viewed by others
1 Introduction
Owing to the nature of their work, physicians are often required to deal with uncertainties and must rely on their expertise to make decisions delegated to them (Kerr et al., 2008; Mohan & Phillips, 2011; Verma et al., 2014). Relevant uncertainty may stem from imperfect scientific evidence regarding the effectiveness of the medical interventions (Manski, 2010, 2017, 2021), idiosyncratic preferences of the patients, or unknown properties of the new or rarely recorded diseases (Fujii & Osaki, 2019). In many such situations, a physician lacks the necessary information to quantify the probabilistic nature of the problem through a single probability distribution. This type of uncertainty is referred to as “ambiguity”.Footnote 1 It is in contrast to the other type of uncertainty, referred to as “risk”, that characterizes situations in which the exact probabilities of events are known (Cerreia-Vioglio et al., 2013).
Attitudes towards ambiguity have a significant impact on various medical decisions (e.g., Berger et al., 2013; Courbage & Peter, 2021; Fujii & Osaki, 2019). To illustrate, consider two treatment options: a conventional, well-established treatment with a known risk-benefit profile, and a newer, innovative treatment with an uncertain risk-benefit profile. Ambiguity averse individuals might prefer the conventional treatment, even if the innovative treatment can offer better expected outcomes, because they feel more comfortable with the known probability distributions associated with the conventional treatment.
This study examines physicians’ decision-making under ambiguity. We provide the first measure of physicians’ ambiguity attitudes towards natural sources using a revealed-preference experiment with real incentives, using two model-free indexes applicable to most ambiguity models (Baillon et al., 2021). We aim to contribute to the growing body of literature regarding the role of uncertainty attitudes in the health domain. While previous studies have primarily focused on risky situations (Galizzi et al., 2016; Nebout et al., 2018; Massin et al., 2018; Attema et al., 2019; van der Pol & Ruggeri, 2008) and more recently on ambiguous situations related to artificial sources (Attema et al., 2018), our study investigates how physicians, as experts in the health domain, make decisions when faced with uncertainty stemming from both health-related and non-health-related natural events.
Medical experts’ ambiguity attitudes have a direct impact on the quality of medical decisions made in highly uncertain, complex, and rapidly changing environments, such as during a new pandemic outbreak (Berger et al., 2021). It is important to understand how medical experts approach novel uncertain situations, and whether they make rational choices or follow expected utility theory. Understanding the decision-making processes of medical experts can inform health-related policies in challenging circumstances. This understanding can also highlight areas where further research is necessary and provide valuable insights into preparing medical experts for uncertain and rapidly changing environments.
The notion of “rational choice” in decision-making under ambiguity is a subject of debate. The Subjective Expected Utility (SEU) framework, which was built on the work of Ramsey (1931), de Finetti (1937), and von Neumann and Morgenstern (1944), is widely appreciated for its normative appeal (Fishburn, 1981; Savage, 1954). SEU asserts that decision-makers carefully consider all available information, assign subjective probabilities to events, and make choices that maximize the expected utility based on these probabilities and the outcomes of events. According to SEU, rational decision-makers should be ambiguity neutral, meaning they should not discriminate between situations with a clear probability distribution and those without.
However, SEU requires decision-makers to assign probabilities to unknowns, which can be challenging in practice. Additionally, it does not account for the level of confidence that people have in their probabilistic assessments. Therefore, some decision theorists argue that ambiguity aversion could be rational because rationality may not necessitate the ability to assign probabilities to unknown events. For example, Gilboa, Postlewaite, and Schmeidler (2008, 2009, 2012), Gilboa and Marinacci (2013), and Mukerji (2009) challenge the Bayesian notion of rationality due to its inability to express ignorance. They argue that the ability to express ignorance is not a mistake, and therefore ambiguity aversion can be interpreted as a pure preference.
Considering these opposing arguments, a benchmark is needed to establish a broader and more inclusive understanding of rationality. To achieve this, we distinguish a decision-maker’s ambiguity aversion from her insensitivity towards ambiguous events and study these two components separately (Chateauneuf et al., 2007; Ghirardato & Marinacci, 2002). Specifically, ambiguity aversion decision-makers tend to undervalue uncertain events regardless of their likelihoods, whereas those who are likelihood insensitive tend to treat events of different levels of likelihoods as roughly the same. This tendency results in ambiguity seeking for low likelihood scenarios and reinforces ambiguity aversion for high likelihood scenarios. While the (ir)rationality of ambiguity aversion remains a subject of debate, likelihood insensitivity is widely considered irrational and indicative of cognitive limitations (Dimmock et al., 2015; Dimmock et al., 2016; Einhorn & Hogarth, 1985; Gonzalez & Wu, 1999). This is because insensitive agents would assign greater weight to events in isolation than when combined, making them susceptible to money pump exploitation (Baillon & Emirmahmutoglu, 2018) and net Sharpe ratio losses (Dimmock et al., 2021). We will assess medical experts’ rationality through the lens of both SEU theory and likelihood insensitivity.
We present evidence concerning ambiguity attitudes of physicians towards the future severity of the COVID-19 pandemic in its early stages and the financial market in the US using an incentive-compatible online experiment. Our experiment was conducted in April 2020 when the knowledge about the pandemic was preliminary so that the tasks involve novel uncertainty. The results indicate that physicians exhibit a significant deviation from expected utility. Although they are only slightly ambiguity averse, they show substantial insensitivity towards changes in likelihood of ambiguous events, which can be interpreted as being irrational. In addition, while physicians demonstrate a superior ability to handle uncertainty regarding stock market performance, they exhibit a similar degree of irrationality compared to the general public when dealing with the ambiguity related to COVID-19. In other words, physicians still exhibit substantial deviation from rationality, even in their own field of expertise. These findings suggest that the multifaceted nature of the new pandemic, the evolving scientific understanding, and the absence of clear-cut solutions may lead to similar irrational behaviors among experts as those observed in the general public. Moreover, they highlight the importance of debiasing strategies to improve physicians’ rationality under ambiguity.
The paper is structured as follows: Section 2 reviews the literature and outlines our contributions; Section 3 introduces our measurements of ambiguity attitudes; Sections 4 and 5 detail the implementation of the experiment and present the empirical results; finally, Section 6 summarizes the results, discusses the theoretical and empirical implications of our study, and addresses its limitations.
2 Related literature
This article is closely related to three strands of literature. The first related strand concerns the characterization of ambiguity attitude towards natural events, which refers to real-world events or circumstances that are uncertain. Examples of natural events include health events, financial investments, weather patterns, etc. Ambiguity aversion was first demonstrated through an artificial scenario, the Ellsberg’s paradox (Ellsberg, 1961). In one version of the Ellsberg experiment, a decision-maker is faced with choosing between two urns: Urn 1 containing 50 red and 50 black balls, and Urn 2 containing an unknown number of red and black balls. The decision-maker wins an award if they choose the urn and a ball of a color specified by them is drawn. Ambiguity aversion can be identified by the preference for betting on events with known odds (Urn 1) over betting on events with unknown odds (Urn 2). However, ambiguity attitudes might be domain dependent. To obtain accurate reflection of people’s attitudes towards uncertainty, many researchers, including Ellsberg himself, have emphasized the importance to study ambiguity through events generated by natural sources, in contrast to the artificial ones such as the Ellsberg urn (Camerer & Weber, 1992; Ellsberg, 2011; Heath & Tversky, 1991).
The impact of ambiguity attitudes has been shown in various health-related decisions, such as preventive behaviors (Baillon et al., 2022; Courbage & Peter, 2021), test and treatment selection (Berger et al., 2013; Cassidy & Manski, 2019; Manski, 2013, 2018) and willingness-to-pay for health improvement (Fujii & Osaki, 2019). These findings are based on theoretical assumptions about decision-makers’ ambiguity attitudes in the health domain, but lack direct empirical evidence due to the difficulty in measuring ambiguity attitudes towards natural events (Trautmann & van de Kuilen, 2015). This study aims to fill this gap by conducting a revealed-preference experiment to directly characterize ambiguity attitudes towards health events.
The second strand focuses on the debate around the rationality of ambiguity aversion, which has intrigued many pioneering scholars, and is still not fully resolved (Ellsberg, 1963; Gilboa & Schmeidler, 1989; Klibanoff et al., 2005; Raiffa, 1961; Stahl, 2014). From a theoretical standpoint, while the SEU framework is widely appreciated for its normative appeal (Fishburn, 1981; Savage, 1954), some prominent researchers such as Gilboa, Postlewaite, and Schmeidler (2008, 2009, 2012), Gilboa and Marinacci (2013) and Mukerji (2009) argue that rational decision-makers may violate Savage axioms, and thus violate EU by expressing ambiguity aversion. Nonetheless, recent experimental studies by Halevy (2007), Chew, Miao, and Zhong (2017), Abdellaoui, Klibanoff, and Placido (2015), and Aydogan et al. (2023) show a close relationship between ambiguity aversion and the incapability to reduce compound risk, suggesting that ambiguity aversion may reflect cognitive limitation.
To address these differing perspectives, this study applies the method introduced by Baillon et al. (2018), which relies on two model-free indices to measure ambiguity attitudes for natural events—ambiguity aversion that captures the aversion to unknown probabilities relative to known probabilities, and likelihood insensitivity that captures insensitivity towards changes in the likelihoods assigned to the state of nature. Separating those two components allows for a more inclusive benchmark of rationality.
The third strand concerns ambiguity attitudes of experts. While it is commonly assumed that experts, such as physicians, have more information compared to laypeople, there is conflicting evidence on their susceptibility to behavioral biases. While some studies suggest that professional traders are less likely to show certain biases, such as preference reversals (List, 2002), the endowment effect (List, 2003, 2004), and ambiguity aversion (Hogarth & Kunreuther, 1989), others indicate that being an expert does not necessarily mean being more rational than laypeople. For instance, experts may exhibit similar levels of loss aversion (Pope & Schweitzer, 2011) and ambiguity aversion (Holm et al., 2013; Berger & Bosetti, 2019), and sometimes even greater levels of myopic loss aversion than others (Haigh & List, 2005).
Relative to these studies, we measure a highly relevant but rare sample of experts, physicians, and compare their rationality under ambiguity with those of the laypeople. As information asymmetry exists, physicians often act as agents for their patients. In clinical settings, it is difficult to observe physicians’ pure beliefs since their suggestions may involve their concern about the patients’ adherence and claims for malpractice (Mendel et al., 2010). Our experimental design provides a unique opportunity to gather evidence on physicians’ ambiguity attitudes when they are representing themselves rather than their patients. By doing so, it will be possible to distinguish between whether the suboptimal decisions made by physicians are due to deviating from a rational benchmark or due to considering the sentiments of the general public. This distinction is important for determining the appropriate debiasing intervention, whether it be targeted at the physicians or improved physician-patient communication.
3 Measurement
3.1 Separating subjective beliefs
Controlling for subjective beliefs is essential for measuring ambiguity attitudes. For example, consider a decision-maker who finds that receiving $10 if it rains tomorrow is as good as receiving $10 with a 40% chance. In this case, if her subjective belief of raining tomorrow is precisely 40%, we would classify her as ambiguity neutral. However, if she believes that the probability of raining tomorrow is 80% (or 20%), then her preference would indicate ambiguity aversion (or seeking).
When dealing with artificial sources of uncertainty, such as Ellsberg urns, the influence of subjective beliefs can be handled in two ways. Subjective beliefs of events can either be assumed to be equal in absence of color preferenceFootnote 2 or controlled through experimental design, which may include multiple bets or allowing participants to select the winning color. However, when the decision concerns natural sources of uncertainty, the subjective likelihood beliefs related to the events of interest are unknown, making it difficult to calibrate the benchmark of ambiguity neutrality. Our measurement relies on a series of “matching probabilities”. For any fixed price x, we find the matching probability m of event E through the following indifference:
Receiving amount x under event E is as good as receiving amount x with probability m.
As demonstrated by the example of betting on rain, the matching probability of a single event is an insufficient indicator of ambiguity attitudes. To overcome this issue, we adopt Baillon et al. (2018)’s method to simultaneously consider the matching probabilities of an event and its complement (e.g., raining and not raining tomorrow) so that beliefs cancel out. Since the subjective beliefs of complementary events by definition always add up to one, the difference between the summation of the two matching probabilities and one reveals an overall propensity or aversion towards ambiguity. In this way, subjective beliefs are separated from ambiguity attitudes.
Notably, the two indexes are constructed without committing to any specific decision model under uncertainty. In fact, as shown by Baillon et al. (2021), the two indexes generalize and unify almost all indexes in the existing literature. This includes models such as the smooth model (Klibanoff et al., 2005), and various multiple prior models (Chateauneuf et al., 2007; Gul & Pesendorfer, 2015), which we explain in detail in subsequent sections.
3.2 Ambiguity aversion
Specifically, we consider three mutually exclusive and exhaustive nonnull events \({E}_{1}\), \({E}_{2}\), and \({E}_{3}\), where \({E}_{ij}\) denotes the union \({E}_{i}\cup {E}_{j}\) and \(i\ne j\). Every \({E}_{i}\) is a single event, and every \({E}_{ij}\) is a composite event. Under ambiguity neutrality, the matching probability of an event, say \(m\left({E}_{1}\right)\), and its complement, \(m\left({E}_{23}\right)\), will add up to one, but under ambiguity aversion (seeking), the sum will fall below (rise above) one. The difference between the sum and one can be taken as the degree of aversion. We take the average of this difference over three events. Formally, the ambiguity aversion index is defined as:
where \({m}_{i}=m\left({E}_{i}\right)\), \({m}_{ij}=m\left({E}_{ij}\right)\), \(\stackrel{-}{{m}_{S}}=({m}_{1}+{m}_{2}+{m}_{3})/3\) for the average single-event matching probability, and \(\stackrel{-}{{m}_{c}}=({m}_{12}+{m}_{23}+{m}_{13})/3\) for the average composite-event matching probability. Under ambiguity neutrality, \({m}_{i}=P\left({E}_{i}\right)\) and \({m}_{ij}=P\left({E}_{i}\right)+P\left({E}_{j}\right)\) for some additive subjective probability measure \(P\). Then \(\stackrel{-}{{m}_{S}}=1/3\) and \(\stackrel{-}{{m}_{c}}=2/3\), implying \(b=0\). Ambiguity aversion is maximal when the matching probabilities of all events are zero, which results in \(b=1\), and is minimal when the matching probabilities of all events are one, which results in \(b=-1\).
The ambiguity aversion index b is an ambiguity premium, reflecting decision-makers’ willing to pay (in probability units) to avoid ambiguity. It is a global measure of ambiguity aversion, which does not allow for ambiguity attitudes to vary across the likelihood domain. However, empirical studies have found that ambiguity aversion might be larger for likely events than events of moderate likelihood, and turns into ambiguity seeking for low likelihood events (Trautmann & van de Kuilen, 2015; Kocher et al., 2018; L’Haridon et al., 2018). Therefore, we need a second index to capture this characteristic.
3.3 Likelihood insensitivity
We consider another index that captures the extent to which matching probabilities and event weights regress towards fifty-fifty, with low likelihoods overvalued and high likelihoods undervalued. This tendency leads to reduced differences \(\stackrel{-}{{m}_{c}}-\stackrel{-}{{m}_{S}}\), that is, reduced discrimination between intermediate levels of likelihood. It reflects insufficient responsiveness of matching probabilities to changes in the likelihoods of events.
After normalization, the ambiguity-generated insensitivity (a-insensitivity) index is defined as:
Under ambiguity neutrality, with perfect discrimination between single and composite events, \(\stackrel{-}{{m}_{S}}=1/3\) and \(\stackrel{-}{{m}_{c}}=2/3\), resulting in a difference of 1/3. Ambiguity neutrality is calibrated, giving \(a=0\). In the most extreme case of complete insensitivity, no distinction is made between levels of likelihoods as all events are taken as having the same odds, resulting in \(\stackrel{-}{{m}_{c}}-\stackrel{-}{{m}_{S}}=0\), and hence \(a=1\).
An alternative way to understand the insensitivity index is by considering the perspective of the alpha-maxmin model (Ghirardato et al., 2004). We can examine a tractable subclass of this model (Baillon et al., 2017; Chateauneuf et al., 2007; Dimmock et al., 2015) that operates on the assumption that a decision-maker’s perception of the ambiguity in \(\rho\) is reflected through a set of priors built by \(\epsilon\)-contamination (Ellsberg, 1961) around their subjective belief \({\rho }_{0}\). This means that the decision-maker not only considers \({\rho }_{0}\) but also all other \(\rho\) around \({\rho }_{0}\) given by \(\left(1-\epsilon \right) {\rho }_{0} \le \rho \le \epsilon +(1-\epsilon ) {\rho }_{0}\), assigning a confidence weight of \(1-\epsilon\) to \({\rho }_{0}\) and a weight \(\epsilon\) to the extreme situations of 0 and 1. Dimmock et al. (2015) has shown that \(\epsilon\) equals to the insensitivity index \(a\) and captures the size of the priors, reflecting the perceived ambiguity in the specific decision-making context.
An insensitivity index of 0 indicates a singleton prior, akin to situations of risk where the decision-maker is “certain” about their belief. On the other hand, an insensitivity index of 1 suggests that the decision-maker perceives full ambiguity and considers the entire domain. For example, in our context, a decision-maker with an insensitivity index \(a\) or \(\epsilon\) equaling 1 interprets the situation as extremely ambiguous, acknowledging that “the disease is not transmissible at all” and “the disease can infect the whole population” are both possible.
3.4 What is the rational ambiguity attitude?
The EU benchmark requires a = b = 0. Having a and b closer to 0 entails being closer to EU, and therefore, more rational. On the other hand, the inclusive benchmark of rationality distinguishes between ambiguity aversion and likelihood insensitivity, allowing for some degree of ambiguity aversion while still requiring likelihood sensitivity. Following this benchmark, full rationality requires a = 0, but has no restriction on b since ambiguity aversion is considered a pure preference. Smaller a indicates less insensitivity, therefore more rationality.
4 Experiment
We recruited physicians and non-physicians in the US through the online survey platform Qualtrics. The platform collects socioeconomic and demographic information of their panelists, allowing researchers to specify the characteristics of their target sample. The experiment was conducted during April 6, 2020–April 16, 2020. The sources of uncertainty concern the future severity of COVID-19 (specifically, the daily number of confirmed cases in the US) and the stock market performance (Dow Jones Industrial Average Index).
4.1 Participants
We collected a sample of 127 physicians and 130 non-physicians.Footnote 3 Our sample covers 35 of the 50 US states. The physician and non-physician samples were recruited via the same platform that host deeply profiled and validated professionals, and the required data were collected in parallel. The platform verified physicians’ identity by calling their employers for confirmation.
In an ideal situation, epidemiologists, physicians specialized in aspiration pneumonia or infectious diseases would be the preferred candidates for investigating the specialists’ ambiguity attitude in the context of COVID-19. However, due to the tremendous difficulty and high costs associated with collecting physician samples during the COVID-19 outbreak, this approach has become unfeasible for us to pursue. Nevertheless, it is essential to recognize that physicians, regardless of their specific specialization, maintain their status as experts when compared to the general public. As such, they provide a valuable proxy for investigating experts’ ambiguity attitudes within specialized fields.
The average response time is about 20 min. All participants received a participation fee paid directly by the survey platforms. Our cost of recruiting each physician exceeded $100, while that associated with non-physicians was about $6 per person. The exact amount of participation fee the platforms paid to each participant was not disclosed to us.
4.2 Incentives
In addition to the participation fee, each participant received the outcome of her decision in one question randomly drawn at the end of the experiment to provide real incentives for the decisions, with stakes of USD 10 (see Online Appendix B for details of the random incentive). The stake is comparable to those adopted in other studies measuring ambiguity attitudes of non-student samples (Dimmock et al., 2016).
In laboratories, experimenters randomly select payments transparently and allow the participants to verify the process, removing potential doubts or confusion. However, conducting such verification can be challenging in online experiments. To address this issue, we utilized the US National Institute of Standards and Technology Randomness Beacon, which publishes a random 128-digit hexadecimal number every minute.Footnote 4 We announce in the experiment that we would use the output value from the Randomness Beacon generated at April 22, 2020, 15:00 (Central European Time, GMT + 2), to implement the random incentive payment procedure. This includes determining which question to pay for randomly and implementing the risky prospect with different probabilities. This approach ensured transparency and verifiability in the procedure.Footnote 5 For further details on the implementation process and the information provided to the participants, please refer to Online Appendix B.
4.3 Stimuli
The elicitation comprised six matching probabilities for each uncertainty source. The experiment started with a training phase, whereby participants were asked two questions to familiarize themselves with the stimuli. It ended by repeating a randomly selected question from those presented a moment ago to test for consistency.
In each question, participants were asked to consider a specific event and choose between two options. We adopted choice lists to elicit matching probabilities for both sources (COVID-19 severity and stock market performance), with the order of the two sources counterbalanced. As the standards of “new case” may vary, participants were told that, when evaluating their responses, we would consider the number of confirmed new cases in the US announced by WHO in the daily reports (a link to the reports was provided on the experimental page). Figure 1 presents the experimental page to elicit the matching probability of an event concerning the future severity of the COVID-19 in the US.
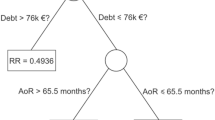
To elicit ambiguity attitudes towards each uncertainty source, we considered a triple of mutually exclusive and exhaustive single events and their compositions (Table 1 shows the events). We carefully selected the partition to prevent \({E}_{1}\), \({E}_{2}\), or \({E}_{3}\) from being highly implausible and treated as null events. For each uncertainty source, we measured the matching probabilities of all six single and composite events. At the end of the experiment, participants were required to provide their socioeconomic characteristics.
5 Results
5.1 Reliability and consistency
Participants could only start the experiment after they had correctly answered a comprehension question. We introduce this question to test our participants’ understanding of the consequences of their choices, ensuring that they understood the incentive (see full experimental instructions in Online Appendix A).
To evaluate data quality, we randomly selected an event for each source of uncertainty and elicited the matching probability of this event a second time to test for consistency. We analyze the consistency of the matching probability by comparing repeated elicitations. Pairwise comparisons based on the full sample and the physician and non-physician subsamples all indicate no significant difference between the repeated elicitations (p > 0.1 for Wilcoxon paired tests, paired t-tests, and Kolmogorov-Smirnov tests). As no statistically significant differences between the first and second elicitation of these matching probabilities were noted, the first matching probability elicited for each event was adopted in the remainder of the analysis.
5.2 Descriptive results
The descriptive statistics of the physician and non-physician samples are presented in Table 2. Comparing the two subgroups, physicians are more likely to be male, slightly older, have financial investment experience, and exhibit higher levels of education and income than the non-physician sample.
Figure 2 displays the physician and non-physician participants’ raw matching probabilities to the uncertain events (as detailed in Table 1). There is more variation in the matching probabilities of different uncertain events given by physicians (represented by the light blue bars) than in those given by non-physicians (represented by the dark green bars), suggesting that physicians distinguish between different uncertain events than non-physicians do.
5.3 Ambiguity attitude indexes
Using these matching probabilities of three single events and three composite events, we calculate the indexes that capture the individual’s ambiguity attitudes, as elaborated in Sections 3.2 and 3.3. As a result, for each participant, we obtain two pairs of indexes \(a\) and \(b\), one pair capturing the participant’s ambiguity attitude towards COVID-19 severity and the other pair capturing the participant’s ambiguity attitude towards the stock market performance during the same time window.
Table 3 displays OLS regression results with the two indexes as the dependent variable. In Columns 1–4 on the left panel, the ambiguity aversion index b is regressed in linear models with errors clustered by individuals. Column 1 demonstrates that both physicians and non-physicians are modestly ambiguity averse, as the intercept is significantly different from 0. The magnitude of ambiguity aversion is indistinguishable either between the physician and non-physician groups or between the two sources of ambiguity. Columns 2 and 3 replicated the results including the fixed effects of the date and state of data collection, without or with demographic control variables.
Column 3 shows that the degree of ambiguity aversion is strongly predicted by the participants’ education attainment. Participants with a graduate degree (Master, JD, MD, or PhD) are much less ambiguity averse than those without one. In addition, ambiguity aversion is also marginally correlated with age, with younger participants being less ambiguity averse than elder participants. The coefficients remain highly consistent when we exclude the physician dummy (Column 4), suggesting that the effect of the physician dummy is not driven by the differences in demographic variables between physicians and non-physicians.
In Columns 5–8 on the right panel, the ambiguity insensitivity index a is regressed in linear models with errors clustered by individuals. Column 5 shows that the participants exhibit severe a-insensitivity, as the intercept is significantly positive and indistinguishable from 1. In contrast to the homogeneous ambiguity aversion index, the a-insensitivity differs substantially between the physician and non-physician groups, with physicians demonstrating significantly less insensitivity towards changes in likelihoods. In addition, participants are less insensitive towards likelihood changes in the COVID source. Although the interaction term between physician and Source COVID is not significant, linear hypothesis testing reveal that the sum of the main effect of Physician and the interaction term of Physician × Source COVID becomes indistinguishable from zero, suggesting that physicians exhibit less likelihood insensitivity than the general public when facing uncertainty in the stock market source, but not when facing uncertainty in the COVID source.
Columns 6 and 7 replicated the results by including the fixed effects of the date and state of data collection, and without or with demographic control variables. Column 7 shows that a-insensitivity is only marginally correlated to income and education. The significant levels of the coefficients do not change when we exclude the physician dummy (Column 8), suggesting that the difference between physicians and non-physicians regarding their a-insensitivity is unlikely to be driven by the difference in socioeconomic backgrounds of the two groups.
6 Summary and discussion
Are physicians rational under ambiguity? It is a critical question as the insights gained from this inquiry have significant implications for assessing the reliability of health-related decisions made in uncertain contexts and determining the necessity of providing additional decision-support tools to assist physicians. This, in turn, can contribute to enhancing patient care and health outcomes. Our study illuminates this matter by examining the ambiguity attitudes of both physicians and non-physicians in the face of ongoing natural events. Using an incentive-compatible experiment to collect data, we have calculated the two indexes representing ambiguity aversion and likelihood insensitivity.
6.1 Physician rationality under ambiguity
Under SEU, rationality necessitates both indexes to be zero. Our findings indicate that neither physicians nor non-physicians meet this standard of rationality when facing natural sources of uncertainty. Despite their extensive training and access to more information, physicians, akin to our non-physician participants, significantly diverge from SEU norms. This divergence is characterized by a modest degree of ambiguity aversion and pronounced levels of likelihood insensitivity.
Comparing physicians and non-physicians, we observed no significant difference in their levels of ambiguity aversion. However, a notable disparity was found in their likelihood insensitivity. By considering a modified criterion for rationality allows for non-zero ambiguity aversion and emphasizes zero likelihood insensitivity as the primary measure, our data confirm that physicians are more rational than non-physicians when handling uncertainty from natural sources.
The analysis becomes more intricate when differentiating between the sources of uncertainty. Interestingly, our participants showed less insensitivity, though still high in absolute value, towards the COVID-19 scenario compared to the stock market. This could be caused by extensive media coverage and public discourse of the pandemic. However, it is noteworthy that physicians do not appear to handle uncertainty regarding the future severity of COVID-19 with greater rationality than the general public. This finding suggests that the advantage physicians hold in managing uncertainty is source-dependent. While they generally outperform the public in traditional domains, this edge may diminish in novel health crises where the public exhibits heightened rationality.
6.2 Theoretical implications
Our findings underscore the necessity of utilizing both ambiguity aversion and likelihood insensitivity indexes to fully capture the dimensions of ambiguity attitudes. Sole reliance on ambiguity aversion risks misinterpretation and overlooks significant variances among participant groups and uncertainty sources—differences that become apparent only through the lens of the insensitivity index.
Our results also reveal two distinct influences on likelihood insensitivity: the nature of information sources and variations across individuals, thereby enriching our comprehension of likelihood insensitivity. Previous research has associated likelihood insensitivity with cognitive limitations (Grevenbrock et al., 2021; L’Haridon & Vieider, 2019) and with manipulation of cognitive capacities (Baillon et al., 2018; Choi et al., 2022). Our findings corroborate these studies, as we observed a marked disparity in likelihood insensitivity between physicians and non-physicians, indicating that physicians possess a cognitive edge in dealing with uncertainty.
The observed variation in likelihood insensitivity across different sources of natural uncertainty suggests that this index extends beyond mere cognitive capacity. Our study found that participants exhibited less insensitivity towards uncertainties stemming from COVID-19 compared to those related to the stock market. This pattern indicates that insensitivity encompasses not only the decision-makers’ ability to differentiate likelihoods but also their subjective judgment about the inherent uncertainties unique to each source. Aligning with findings from laboratory studies that demonstrate how artificial sources of uncertainty influence likelihood insensitivity (de Bruin et al., 2000; Hey & Pace, 2014), our research underscores the source-dependent nature of likelihood insensitivity in the context of natural events.
6.3 Real-world implications
Our study uncovers a significant degree of irrationality in physicians’ decision-making under uncertainty, signaling an urgent need for improvement and targeted interventions, particularly in addressing likelihood insensitivity.
Our study underscores the dual nature of likelihood insensitivity, highlighting two distinct factors: decision-makers’ cognitive limitations and the lack of comprehensive information regarding the uncertainty source. Therefore, a two-pronged approach is essential for effective intervention. Firstly, addressing cognitive limitations involves enhancing decision-makers’, especially physicians’, understanding of likelihoods. They should be made aware of their likelihood insensitivity bias and encouraged to adopt decision-support tools, such as decision trees and expected utility calculators. Incorporating these tools as standard elements in medical practices dealing with significant ambiguity is imperative. Furthermore, considering that complex decision environments can strain cognitive resources, we suggest alleviating the time pressures experienced by physicians, recognizing that although some situations naturally impose time constraints, it is important to make concerted efforts to mitigate these pressures whenever possible. Studies have shown that such pressures contribute to increased insensitivity (Baillon et al., 2018; Choi et al., 2022).
Secondly, to mitigate insensitivity arising from information scarcity, especially in novel uncertainty sources, we need innovative approaches. An initial approach to tackle this issue involves supplying accessible preliminary records of the uncertain events’ outcomes. This method has proven effective in reducing insensitivity towards the performance of stock market Initial Public Offerings in a laboratory experiment (Baillon et al., 2017).
6.4 Limitation and future research
Our study was conducted during the early stages of the COVID-19 pandemic, primarily to uncover physicians’ ambiguity attitudes towards an unfolding public health crisis at the moment. However, this period was also marked by heightened pressure on physicians, a factor known to impede cognitive abilities. Future research should investigate whether our findings remain consistent under normal circumstances, where such pressures are less pronounced. Furthermore, it would be insightful to examine the dynamic evolution of physicians’ sensitivity to uncertainty as scientific progress unveils more information about the novel virus. While this line of inquiry is compelling, it extends beyond the purview of our current investigation, yet it represents a significant opportunity for future scholarly exploration.
To align our study with existing literature, we utilized the stock market as a traditional source of uncertainty, a choice informed by its frequent use in pioneering studies on natural sources of uncertainty with various populations (e.g., Baillon et al., 2017; Dimmock et al., 2016, 2021). It would be insightful to explore whether physicians exhibit more rational behavior when dealing with medical uncertainties within their areas of expertise, compared to their responses to a novel pandemic like COVID-19. Future studies following this path could expand upon our findings to delve deeper into physicians’ ambiguity attitudes towards different health-related sources of uncertainty. Ideally, with a larger pool of medical participants, future research could specifically target medical specialists, focusing on uncertainty sources that align closely with their specialized fields of knowledge.
Notes
“Deep uncertainty” is an alternative term for ambiguity (Kocher et al., 2018).
The power test suggested a sample size of at least 108 per group, with power being 0.8, the effect size of the difference between physicians and non-physicians in the a index being 0.15, and the standard deviation of a being 0.44. According to the study conducted by Dimmock et al. (2016) using the Dutch representative sample, the standard deviation of the a index is 0.44 (Table 3), and a change of 0.15 in the a index corresponds to about 1% point change of stock market participation probability, with an economic effect of a €7840 change in financial assets per person.
It has been used under various contexts, such as selecting test and control groups for clinical trials, selecting random government officials for financial audits, and assigning court cases to random judges.
Chark, Chew, and Zhong (2020) also used publicly observable future random events for implementing random incentive payments. They employed the outcomes of the China Welfare Lottery and China Sports Lottery as publicly verifiable source of randomness.
References
Abdellaoui, M., Baillon, A., Placido, L., & Wakker, P. P. (2011). The rich domain of uncertainty: Source functions and their experimental implementation. American Economic Review, 101(2), 695–723.
Abdellaoui, M., Klibanoff, P., & Placido, L. (2015). Experiments on compound risk in relation to simple risk and to ambiguity. Management Science, 61(6), 1306–1322.
Attema, A. E., Bleichrodt, H., & L’Haridon, O. (2018). Ambiguity preferences for health. Health Economics, 27(11), 1699–1716.
Attema, A. E., L’Haridon, O., & van de Kuilen, G. (2019). Measuring multivariate risk preferences in the health domain. Journal of Health Economics, 64, 15–24.
Aydogan, I., Berger, L., Bosetti, V., & Liu, N. (2023). Three layers of uncertainty. Journal of European Economic Association, 21(5), 2209–2236.
Baillon, A., & Emirmahmutoglu, A. (2018). Zooming in on ambiguity attitudes. International Economic Review, 59(4), 2107–2131.
Baillon, A., Bleichrodt, H., Keskin, U., L’Haridon, O., & Li, C. (2017). The effect of learning on ambiguity attitudes. Management Science, 64(5), 2181–2198.
Baillon, A., Huang, Z., Selim, A., & Wakker, P. P. (2018). Measuring ambiguity attitudes for all (natural) events. Econometrica, 86(5), 1839–1858.
Baillon, A., Bleichrodt, H., Li, C., & Wakker, P. P. (2021). Belief hedges: Measuring ambiguity for all events and all models. Journal of Economic Theory, 198, 105353.
Baillon, A., Bleichrodt, H., Emirmahmutoglu, A., Jaspersen, J., & Peter, R. (2022). When risk perception gets in the way: Probability weighting and underprevention. Operations Research, 70(3), 1371–1392.
Berger, L., Bleichrodt, H., & Eeckhoudt, L. (2013). Treatment decisions under ambiguity. Journal of Health Economics, 32(3), 559–569.
Berger, L., & Bosetti, V. (2019). Are policymakers ambiguity averse. The Economic Journal, 130(626), 331–355.
Berger, L., Berger, N., Bosetti, V., Gilboa, I., Hansen, L. P., Jarvis, C., & Smith, R. D. (2021). Rational policymaking during a pandemic. Proceedings of the National Academy of Sciences, 118(4), e2012704118.
de Bruin, W. B., Fischhoff, B., Millstein, S. G., & Halpern-Felsher, B. L. (2000). Verbal and numerical expressions of probability: ‘It’s a fifty–fifty chance’. Organizational Behavior and Human Decision Processes, 81(1), 115–131.
Camerer, C., & Weber, M. (1992). Recent developments in modeling preferences: Uncertainty and ambiguity. Journal of Risk and Uncertainty, 5(4), 325–370.
Cassidy, R., & Manski, C. F. (2019). Tuberculosis diagnosis and treatment under uncertainty. Proceedings of the National Academy of Sciences 116(46), 22990–22997.
Cerreia-Vioglio, S., Maccheroni, F., Marinacci, M., & Montrucchio, L. (2013). Ambiguity and robust statistics. Journal of Economic Theory, 148(3), 974–1049.
Chark, R., Chew, S. H., & Zhong, S. (2020). Individual preference for longshots. Journal of the European Economic Association, 18(2), 1009–1039.
Chateauneuf, A., Eichberger, J., & Grant, S. (2007). Choice under uncertainty with the best and worst in mind: Neo-additive capacities. Journal of Economic Theory, 137(1), 538–567.
Chew, S. H., Miao, B., & Zhong, S. (2017). Partial Ambiguity. Econometrica, 85(4), 1239–1260.
Choi, S., Kim, J., Lee, E., & Lee, J. (2022). Probability weighting and cognitive ability. Management Science, 68(7), 5201–5215.
Courbage, C., & Peter, R. (2021). On the effect of uncertainty on personal vaccination decisions. Health Economics, 30(11), 2937–2942.
Dimmock, S. G., Kouwenberg, R., & Wakker, P. P. (2016). Ambiguity attitudes in a large representative sample. Management Science, 62(5), 1363–1380.
Dimmock, S. G., Kouwenberg, R., Mitchell, O. S., & Peijnenburg, K. (2015). Estimating ambiguity preferences and perceptions in multiple prior models: Evidence from the field. Journal of Risk and Uncertainty, 51(3), 219–244.
Dimmock, S. G., Kouwenberg, R., Mitchell, O. S., & Peijnenburg, K. (2016). Ambiguity aversion and household portfolio choice puzzles: Empirical evidence. Journal of Financial Economics, 119(3), 559–577.
Dimmock, S. G., Kouwenberg, R., Mitchell, O. S., & Peijnenburg, K. (2021). Household portfolio underdiversification and probability weighting: Evidence from the field. The Review of Financial Studies, 34(9), 4524–4563.
Einhorn, H. J., & Hogarth, R. M. (1985). Ambiguity and uncertainty in probabilistic inference. Psychological Review, 92(4), 433–461.
Ellsberg, D. (1961). Risk, ambiguity, and the Savage axioms. The Quarterly Journal of Economics, 75(4), 643–669.
Ellsberg, D. (1963). Risk, ambiguity, and the Savage axioms: Reply. The Quarterly Journal of Economics, 77(2), 336–342.
Ellsberg, D. (2011). Introduction to the symposium issue: Notes on the origins of the Ellsberg Urns. Economic Theory 48(2), 221–227.
de Finetti, B. (1937). La prévision: Ses lois logiques, Ses sources subjectives. Annales De L’institut Henri Poincaré, 7(1), 1–68.
Fishburn, P. C. (1981). Subjective expected utility: A review of normative theories. Theory and Decision, 13(2), 139–199.
Fujii, Y., & Osaki, Y. (2019). The willingness to pay for health improvement under comorbidity ambiguity. Journal of Health Economics, 66, 91–100.
Galizzi, M. M., Miraldo, M., Stavropoulou, C., & van der Pol, M. (2016). Doctor-patient differences in risk and time preferences: A field experiment. Journal of Health Economics, 50(2), 171–182.
Ghirardato, P., & Marinacci, M. (2002). Ambiguity made precise: A comparative foundation. Journal of Economic Theory, 102(2), 251–289.
Ghirardato, P., Maccheroni, F., & Marinacci, M. (2004). Differentiating ambiguity and ambiguity attitude. Journal of Economic Theory, 118(2), 133–173.
Gilboa, I., Postlewaite, A. W., & Schmeidler, D. (2008). Probability and uncertainty in economic modeling. Journal of Economic Perspectives, 22(3), 173–188.
Gilboa, I., Postlewaite, A., & Schmeidler, D. (2009). Is it always rational to satisfy Savage’s axioms? Economics and Philosophy, 25(3), 285–296.
Gilboa, I., Postlewaite, A., & Schmeidler, D. (2012). Rationality of belief or: Why Savage’s axioms are neither necessary nor sufficient for rationality. Synthese, 187(1), 11–31.
Gilboa, I., & Marinacci, M. (2013). Ambiguity and the bayesian paradigm. In D. Acemoglu, M. Arellano, & E. Dekel (eds.), Advances in Economics and Econometrics: Theory and Applications, Tenth World Congress of the Econometric Society. Cambridge University Press.
Gilboa, I., & Schmeidler, D. (1989). Maxmin Expected Utility with Non-unique Prior. Journal of Mathematical Economics, 18(2), 141–153.
Gonzalez, R., & Wu, G. (1999). On the shape of the probability weighting function. Cognitive Psychology, 38(1), 129–166.
Grevenbrock, N., Groneck, M., Ludwig, A., & Zimper, A. (2021). Cognition, optimism, and the formation of age-dependent survival beliefs. International Economic Review, 62(2), 887–918.
Gul, F., & Pesendorfer, W. (2015). Hurwicz expected utility and subjective sources. Journal of Economic Theory, 159(Part A), 465–488.
Haigh, M. S., & List, J. A. (2005). Do professional traders exhibit myopic loss aversion? An experimental analysis. Journal of Finance, 60(1), 523–534.
Halevy, Y. (2007). Ellsberg revisited: An experimental study. Econometrica, 75(2), 503–536.
Heath, C., & Tversky, A. (1991). Preference and belief: Ambiguity and competence in choice under uncertainty. Journal of Risk and Uncertainty, 4(1), 5–28.
Hey, J. D., & Pace, N. (2014). The explanatory and predictive power of non two-stage-probability theories of decision making under ambiguity. Journal of Risk and Uncertainty, 49(1), 1–29.
Hogarth, R. M., & Kunreuther, H. (1989). Risk, ambiguity, and insurance. Journal of Risk and Uncertainty, 2(1), 5–35.
Holm, H. J., Opper, S., & Nee, V. (2013). Entrepreneurs under uncertainty: An economic experiment in China. Management Science, 59(7), 1671–1687.
Kerr, E. A., Zikmund-Fisher, B. J., Klamerus, M. L., Subramanian, U., Hogan, M. M., & Hofer, T. P. (2008). The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Annals of Internal Medicine, 148(10), 717–727.
Klibanoff, P., Marinacci, M., & Mukerji, S. (2005). A smooth model of decision making under ambiguity. Econometrica, 73(6), 1849–1892.
Kocher, M. G., Lahno, A. M., & Trautmann, S. T. (2018). Ambiguity aversion is not universal. European Economic Review, 101(C), 268–283.
L’Haridon, O., & Vieider, F. M. (2019). All over the map: A worldwide comparison of risk preferences. Quantitative Economics, 10(1), 185–215.
L’Haridon, O., Vieider, F. M., Aycinena, D., Bandur, A., Belianin, A., Cingl, L., Kothiyal, A., & Martinsson, P. (2018). Off the charts: Massive unexplained heterogeneity in a global study of ambiguity attitudes. Review of Economics and Statistics, 100(4), 664–677.
List, J. A. (2002). Preference reversals of a different kind: The ‘more is less’ phenomenon. American Economic Review, 92(5), 1636–1643.
List, J. A. (2003). Does market experience eliminate market anomalies. The Quarterly Journal of Economics, 118(1), 41–71.
List, J. A. (2004). Neoclassical theory versus prospect theory: Evidence from the marketplace. Econometrica, 72(2), 615–625.
Manski, C. F. (2010). Vaccination with partial knowledge of external effectiveness. Proceedings of the National Academy of Sciences, 107(9), 3953–3960.
Manski, C. F. (2013). Diagnostic testing and treatment under ambiguity: Using decision analysis to inform clinical practice. Proceedings of the National Academy of Sciences, 110(6), 2064–2069.
Manski, C. F. (2017). Mandating vaccination with unknown indirect effects. Journal of Public Economic Theory, 19(3), 603–619.
Manski, C. F. (2018). Credible ecological inference for medical decisions with personalized risk assessment. Quantitative Economics, 9(2), 541–569.
Manski, C. F. (2021). Vaccination planning under uncertainty, with application to Covid-19. National Bureau of Economic Research Working Paper No. w28446.
Massin, S., Nebout, A., & Ventelou, B. (2018). Predicting medical practices using various risk attitude measures. The European Journal of Health Economics, 19(6), 843–860.
Mendel, R., Hamann, J., Traut-Mattausch, E., Bühner, M., Kissling, W., & Frey, D. (2010). What would you do if you were me, Doctor?’: Randomised trial of psychiatrists’ personal v. professional perspectives on treatment recommendations. The British Journal of Psychiatry, 197(6), 441–447.
Mohan, A. V., & Phillips, L. S. (2011). Clinical inertia and uncertainty in medicine. Journal of the American Medical Association, 306(4), 383–384.
Mukerji, S. (2009). Foundations of ambiguity and economic modelling. Economics & Philosophy, 25(3), 297–302.
Nebout, A., Cavillon, M., & Ventelou, B. (2018). Comparing GPs’ risk attitudes for their own health and for their patients’: A troubling discrepancy? BMC Health Services Research, 18, 283.
von Neumann, J., & Morgenstern, O. (1944). The theory of games and Economic Behavior. Princeton University Press.
van der Pol, M., & Ruggeri, M. (2008). Is risk attitude outcome specific within the health domain? Journal of Health Economics, 27(3), 706–717.
Pope, D. G., & Schweitzer, M. E. (2011). Is Tiger Woods loss averse? Persistent bias in the face of experience, competition, and high stakes. American Economic Review, 101(1), 129–157.
Raiffa, H. (1961). Risk, ambiguity, and the savage axioms: Comment. The Quarterly Journal of Economics, 75(4), 690–694.
Ramsey, F. P. (1931). Truth and Probability. The foundations of Mathematical and other logical essays. Routledge and K. Paul.
Savage, L. J. (1954). The foundations of statistics. Wiley.
Stahl, D. O. (2014). Heterogeneity of ambiguity preferences. Review of Economics and Statistics, 96(4), 609–617.
Trautmann, S. T., & van de Kuilen, G. (2015). Ambiguity attitudes. The Wiley Blackwell Handbook of Judgment and decision making. Blackwell.
Verma, A. A., Razak, F., & Detsky, A. S. (2014). Understanding choice: Why physicians should learn Prospect Theory. Journal of the American Medical Association, 311(6), 571–572.
Acknowledgements
The authors acknowledge financial support from the China National Science Foundation (Grant 72103015, Grant 72250065, Grant 72373092) and Shanghai Shuguang Foundation (Grant 18SG30), and the Program for Innovative Research Team at Shanghai University of Finance and Economics. The funding sources had no involvement in conducting of the study or in the decision to submit the article for publication. In the course of preparing this manuscript, the authors employed the ChatGPT service for textual refinement. All content was subsequently scrutinized and revised by the authors, who are solely responsible for ensuring the veracity and scholarly rigor of the content within this publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gao, Y., Huang, Z., Liu, N. et al. Are physicians rational under ambiguity?. J Risk Uncertain 68, 183–203 (2024). https://doi.org/10.1007/s11166-023-09425-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11166-023-09425-z