Abstract
Appropriate birth spacing improves the outcomes of children and mothers, but spacing intervals are short in sub-Saharan African countries. This paper investigates one of the behavioural mechanisms behind the short intervals by studying the impact of foetus loss including miscarriage and stillbirth. Since most of these pregnancy losses result from a genetic abnormality in the fertile egg, they can be considered random conditional on factors such as maternal age and fixed effects. We find that a pregnancy loss experience leads to a mechanical increase in the next birth spacing interval that includes the loss and the next conception. More importantly, we also find that a pregnancy loss brings about a decrease in the intervals for all subsequent births and that the shortening effect does not disappear throughout the mother’s life. Much of the shortening effect is explained once we introduce an individual-specific indicator for the realised probability of pregnancy loss. These results imply that pregnancy loss affects birth spacing by making mothers overestimate their probability of losing their unborn children. They further suggest a belief updating mechanism where mothers update their subjective probability of losing a pregnancy based on the results of their own pregnancies.



Similar content being viewed by others
Notes
World Development Indicators by World Bank, retrieved on the 19th of September 2022, at http://databank.worldbank.org/data/reports.aspx?source=world-development-indicators. Variable codes are SP.DYN.TFRT.IN for the total fertility rate, SH.STA.MMRT for the maternal mortality rate, and SP.DYN.IMRT.IN for the infant mortality rate.
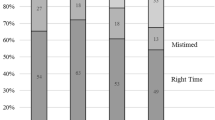
This paper considers a birth spacing interval appropriate if it is within the range recommended by the World Health Organization (2007), namely, two to five years between the end of a pregnancy and the next conception. Since approximately two-thirds of pregnancies have a spacing interval shorter than the lower bound, we mainly consider whether the interval is shorter than that. For more detail, see Section 3.
One of the pathways through which birth spacing can affect subsequent outcomes is through birth weight. Appropriate birth spacing is shown to increase birth weight (e.g., Rosenzweig & Wolpin, 1988), which in turn improves socioeconomic outcomes throughout one’s life (Behrman & Rosenzweig, 2004; Bharadwaj et al., 2018; Black et al., 2007; Fletcher, 2011).
Other previous studies have shown that birth spacing and more general fertility patterns are explained by socioeconomic factors such as female education, wages, contraception, macroeconomic conditions, and the gender of the previous child (Bhalotra, 2010; Heckman & Walker, 1990; Kim, 2010; Pimentel et al., 2020).
Another issue is the number of losses a woman experiences. Recurrent losses are relatively rarer but more likely to be caused by nongenetic factors (Ford & Schust, 2009). We consider the robustness of our results to recurrent losses using secondary data (see Supplementary Materials Section S.II) and their consistency with our proposed mechanism of the birth spacing behavioural change (Section 6 and Supplementary Materials Fig. S.I.1).
Chromosomal abnormalities, therefore, can be caused by both men and women. However, the extra chromosome, one of the most commonly reported causes of chromosomal abnormality, is mostly of maternal origin (Larsen et al., 2013). Therefore, although not strictly perfect, it may be enough to control for maternal characteristics in our particular context.
Examples include antiphospholipid, antinuclear, and antithyroid antibodies.
Examples include hypothyroidism.
See Table 1 for the full list of datasets used for the study.
The DHS uses different versions of questionnaires, and only versions four and higher collected information on pregnancy loss. We thus make use of the DHS data that use questionnaire version four or higher.
The DHS questionnaire has the following question: ‘Have you ever had a pregnancy that miscarried, was or ended in a stillbirth?’ However, the recode manual (Demographic and Health Surveys, 2013) describes the variable as ‘[w]hether the respondent ever had a pregnancy that terminated in a miscarriage, abortion, or still birth, i.e., did not result in a live birth.’ Therefore, we inserted the seemingly missing ‘abortion’ and enclosed it with square brackets.
For details, see Section 5.2 and Supplementary Materials Section S.II.
The WHO defines birth spacing as the interval between the end of a pregnancy and the conception of the next pregnancy (World Health Organization, 2007). Since our DHS data do not contain information about the length of gestation, we cannot compute a birth spacing measure consistent with the WHO definition. This difference is, however, unlikely to invalidate our econometric analysis, unless the length of gestation for pregnancies conceived after pregnancy loss systematically differs from that of pregnancies before the loss. We are unaware of the convincing literature that suggests a systematic change in premature births after losing a pregnancy.
The statistics in Table 2 are at the pregnancy level such that multiple births are counted as one observation. In this case, child sex is technically undefined for multiple births. We code 1 for a male single birth, 2 for a female single birth, and 3 for multiple births. The statistic for ’1 if child male’ indicates the share of male single births. Noting the possible selection of women who carry multiple births to term (Bhalotra & Clarke, 2016), we primarily focus on birth (multiple births are counted as one observation) in our main analysis, while we confirm the robustness of our conclusion when we count each child as one observation.
Since the WHO recommends a pregnancy interval of at least two years (between the onset of a new pregnancy and the end of the previous pregnancy), we compute the recommendation as equivalent to two years plus nine months or 33 months.
For example, consider woman j who experienced a pregnancy loss after two live births but never afterwards. For this woman, we have \({D}_{3,j}^{{{{\rm{post}}}},1}=1\) since her third live birth (subscript i = 3) is her 1st live birth after her loss experience (superscript l = 1). Similarly, we have \({D}_{4,j}^{{{{\rm{post}}}},2}=1\) since her fourth live birth (i = 4) is her 2nd live birth after her loss experience (l = 2).
When we present the estimation results, we write L1 ≡ {1}, L2 ≡ {1, 2+}, L3 ≡ {1, 2, 3+}, and L4 ≡ {1, 2, 3, 4+}.
Caution is warranted in this specification, however, as the interpretation of δ1 parameters in Eq. (3) slightly differs from that in Eq. (2). The coefficient estimates for δ1 in Eq. (3) represent postloss changes in birth spacing relative to the last preloss birth, while those in Eq. (2) represent changes relative to the average preloss birth.
The covariates include age dummies, age at birth k dummies, years of education dummies, region dummies, religion dummies, and ethnicity dummies.
The average number of births for women aged over 40 or 45 years is between seven and eight; see Table 3.
In the main analyses, we decompose the changes in birth spacing intervals for the first, second, third, and all subsequent births after the loss episode.
We find a small and insignificant coefficient estimate for Dpost,4 for women with years since pregnancy loss less than the median that substantially differs from that for women with years since pregnancy loss equal to or greater than the median. This is likely to accompany a compositional change such that women with four or more live births within a short period of time since pregnancy loss could be very different from the other sample women even conditional on woman FEs.
The interval between the loss and the birth of the next child is likely to be shortened as well, although it is obscured by the mechanical lengthening effect on the birth spacing interval that encompasses the loss.
The coefficient for \({D}^{{{{\rm{pre}}}},4-}\) is statistically significantly estimated. We speculate that this statistical significance involves the compositional change in women for whom the dummy can become one. As we discuss below, the median number of preloss births is only two in our data. Pregnancy behaviours of women with such a large number of preloss births may considerably differ from other women even after conditional on woman FEs.
See Supplementary Materials Section S.II for more details.
We thank an anonymous referee for suggesting this analysis.
We thank an anonymous referee for suggesting this analysis.
Comparison of legal abortion leniency across countries is not straightforward since abortion leniency can be multifaceted and not strictly along an ordered scale. As in Singh et al. (2018), countries are usually aligned with an ordinal scale (i.e., prohibited altogether, permitted to save the mother’s life, permitted in addition to preserve her physical health, permitted further to preserve her mental health, permitted even further for socioeconomic reasons, permitted altogether). However, there can be exceptional grounds on which abortion may be legally permitted (e.g., when a pregnancy results from rape or incest and when a foetus is found to possess serious impairment in utero). The importance of these exceptional grounds relative to the above ordinal scale can considerably differ across countries.
For example Lybbert et al. (2007), reported that herders in eastern Africa are found to update their expectations when they obtain a low-rainfall forecast; Oster (2018) showed evidence of and examined the mechanism for the increase in pertussis vaccination following local outbreaks; and some studies (e.g., Ando et al., 2017; Fink & Stratmann, 2015) investigated whether housing prices near nuclear power plants in countries such as Sweden and the U.S. changed after the nuclear plant blast in Fukushima in 2011.
See Supplementary Materials Section S.III for a more formal discussion.
As an illustration, consider that woman j experiences two live births, a loss, and another two live births in this order. For her, the realised probabilities of pregnancy loss before the second, third and fourth live births are z2,j = 0, z3,j = 1/3, and z4,j = 1/4, respectively (note that the third live birth is realised at her fourth pregnancy). Technically, zij corresponds to the prior belief with an assumption that the prior is formed as the mean of a beta distribution \({{{\mathcal{B}}}}({a}_{ij},{b}_{ij})\), where \({a}_{ij}={D}_{ij}^{{{{\rm{post}}}}}\) and bij = i − 1.
Equivalently, \({z}_{ij}^{l}\) can also be considered the interaction term between zij and \({D}_{ij}^{{{{\rm{post}}}},l}\).
For instance, for woman p with one live birth before pregnancy loss, \({z}_{i,p}^{l}\) for l = 1, 2, ... takes values \({z}_{1,p}^{1}=1/(1+1)=1/2,{z}_{2,p}^{2}=1/3,{z}_{3,p}^{3}=1/4,{z}_{4,p}^{4}=1/5,...\) where \({z}_{1,p}^{1}\) represents the realised loss probability associated with her second live birth. This is the end of the first birth interval (i = 1) and coincides with the first postloss parity (l = 1); \({z}_{2,p}^{2}\) represents the same probability associated with the third live birth, which is the end of the second birth interval (i = 2), as well as the second postloss parity (l = 2), and so on. On the other hand, woman q with four preloss births has \({z}_{4,q}^{1}=1/(4+1)=1/5,{z}_{5,q}^{2}=1/6,{z}_{6,q}^{3}=1/7,{z}_{7,q}^{4}=1/8,...\). Observe that the overall birth spacing index, i, differs between woman p and q at the first postloss parity, where l = 1 due to the differing numbers of preloss births, which creates the variation in zl.
While it is possible to depict different trajectories for women with all different numbers of preloss births, we show the cases for women with one and four preloss births for brevity. The trajectories for women with other numbers of preloss births provide qualitatively the same conclusion.
Trivially, the calculated changes for l ≥ 4 are \({\hat{\delta }}_{1}^{4+}+{\hat{\beta }}^{4+}{z}^{l}\).
The positive coefficient estimate for Dpost,4+ may appear unusual. Note that for a woman with two preloss births, the change in birth spacing due to realised probability is −82.14 × (1/6) = −13.69. The positive coefficient offsets this large effect, and the total change in the spacing interval is −13.69 + 5.94 = −7.75, which compares reasonably with the estimates from the specification without the realised loss probability in Table 4.
These results must be interpreted carefully as the information about multiple loss experiences is available only for women whose most recent birth was within the previous five years.
Interestingly, using data from Norway Markussen and Strøm (2022) found that the number of children after miscarriage caught up faster at the first parity than at later parities. This also appears consistent with our findings and the belief updating hypothesis. We thank an anonymous referee for suggesting this reference.
For example, another hypothesis might be that women with many more preloss births may not adjust their spacing intervals because they are more likely to have achieved their fertility goals before pregnancy loss. Our use of woman fixed effects likely addresses the possible impact of fertility goal heterogeneity. Additionally, the fertility goal hypothesis does not seem to be fully consistent with our results showing that women with as many as four preloss births do respond to pregnancy loss, although it does have the potential to explain their lesser adjustment (Figs. 2 and 3). Unfortunately, we cannot rigorously test this hypothesis, as the data have no information about the measurement of fertility goals before fertility onset. We thank an anonymous referee for suggesting this alternative mechanism.
References
Ando, M., Dahlberg, M., & Engström, G. (2017). The risks of nuclear disaster and its impact on housing prices. Economics Letters, 154, 13–16. http://linkinghub.elsevier.com/retrieve/pii/S0165176517300629
Behrman, J. R., & Rosenzweig, M. R. (2004). Returns to birthweight. Review of Economics and Statistics, 86, 586–601. https://doi.org/10.1162/003465304323031139
Bhalotra, S. (2010). Fatal fluctuations? Cyclicality in infant mortality in India. Journal of Development Economics, 93, 7–19. https://linkinghub.elsevier.com/retrieve/pii/S0304387809000388
Bhalotra, S., & Clarke, D. (2016). The Twin Instrument. IZA Discussion Paper, 10405, 107
Bhalotra, S., & van Soest, A. (2008). Birth-spacing, fertility and neonatal mortality in India: Dynamics, frailty, and fecundity. Journal of Econometrics, 143, 274–290. http://linkinghub.elsevier.com/retrieve/pii/S0304407607002138
Bharadwaj, P., Lundborg, P., & Rooth, D.-O. (2018). Birth weight in the long run. Journal of Human Resources, 53, 189–231. https://doi.org/10.3368/jhr.53.1.0715-7235R
Black, S. E., Devereux, P. J., & Salvanes, K. G. (2007). From the cradle to the labor market? The effect of birth weight on adult outcomes. Quarterly Journal of Economics, 122, 409–439
Brown, S. (2008). Miscarriage and its associations. Seminars in Reproductive Medicine, 26, 391–400. https://doi.org/10.1055/s-0028-1087105
Buckles, K. S., & Munnich, E. L. (2012). Birth spacing and sibling outcomes. Journal of Human Resources, 47, 613–642. http://jhr.uwpress.org/content/47/3/613.short
Conde-Agudelo, A., Rosas-Bermúdez, A., & Kafury-Goeta, A. C. (2006). Birth spacing and risk of adverse perinatal outcomes: A meta-analysis. Journal of American Medical Association, 295, 1809–1823. http://archinte.jamanetwork.com/article.aspx?articleid=202711
Dadi, A. F. (2015). A systematic review and meta-analysis of the effect of short birth interval on infant mortality in Ethiopia. PLoS ONE, 10, e0126759. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0126759
Delavande, A. (2014). Probabilistic expectations in developing countries. Annual Review of Economics, 6, 1–20. https://doi.org/10.1146/annurev-economics-072413-105148
Demographic and Health Surveys. (2013). Standard Recode Manual for DHS 6. https://dhsprogram.com/pubs/pdf/DHSG4/Recode6_DHS_22March2013_DHSG4.pdf
Dupas, P. (2011). Health behavior in developing countries. Annual Review of Economics, 3, 425–449. https://doi.org/10.1146/annurev-economics-111809-125029
Fink, A., & Stratmann, T. (2015). U.S. housing prices and the Fukushima nuclear accident. Journal of Economic Behavior & Organization, 117, 309–326. http://linkinghub.elsevier.com/retrieve/pii/S0167268115001961
Fletcher, J. M. (2011). The medium term schooling and health effects of low birth weight: Evidence from siblings. Economics of Education Review, 30, 517–527. https://linkinghub.elsevier.com/retrieve/pii/S0272775710001779
Ford, H. B., & Schust, D. J. (2009). Recurrent pregnancy loss: Etiology, diagnosis, and therapy. Reviews in Obstetrics and Gynecology, 2, 76. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2709325/
Heckman, J. J., Holtz, V. J., & Walker, J. R. (1985). New evidence on the timing and spacing of births. American Economic Review, 75, 179–184
Heckman, J. J., & Walker, J. R. (1990). The relationship between wages and income and the timing and spacing of births: Evidence from Swedish longitudinal data. Econometrica, 58, 1411. http://www.jstor.org/stable/2938322?origin=crossref
Hertwig, R., Barron, G., Weber, E. U., & Erev, I. (2004). Decisions from experience and the effect of rare events in risky choice. Psychological Science, 15, 534–539
Hotz, V. J., McElroy, S. W., & Sanders, S. G. (2005). Teenage childbearing and its life cycle consequences exploiting a natural experiment. Journal of Human Resources, 40, 683–715. http://jhr.uwpress.org/content/XL/3/683.short
Karimi, A. (2014). The spacing of births and women’s subsequent earnings: Evidence from a natural experiment. Institute for Evaluation of Labour Market and Education Policy. https://www.econstor.eu/handle/10419/106299
Kim, J. (2010). Women’s education and fertility: An analysis of the relationship between education and birth spacing in Indonesia. Economic Development and Cultural Change, 58, 739–774
Larsen, E. C., Christiansen, O. B., Kolte, A. M., & Macklon, N. (2013). New insights into mechanisms behind miscarriage. BMC Medicine, 11, 154
Lybbert, T. J., Barrett, C. B., McPeak, J. G., & Luseno, W. K. (2007). Bayesian herders: Updating of rainfall beliefs in response to external forecasts. World Development, 35, 480–497. http://linkinghub.elsevier.com/retrieve/pii/S0305750X0600218X
Maitra, P., & Pal, S. (2008). Birth spacing, fertility selection and child survival: Analysis using a correlated hazard model. Journal of Health Economics, 27, 690–705. http://linkinghub.elsevier.com/retrieve/pii/S0167629607000975
Markussen, S., & Strøm, M. (2022). Children and labor market outcomes: Separating the effects of the first three children. Journal of Population Economics, 35, 135–167. https://doi.org/10.1007/s00148-020-00807-0
Miller, A. R. (2011). The effects of motherhood timing on career path. Journal of Population Economics, 24, 1071–1100. https://doi.org/10.1007/s00148-009-0296-x
Mira, P. (2007). Uncertain infant mortality, learning, and life-cycle fertility. International Economic Review, 48, 809–846. https://doi.org/10.1111/j.1468-2354.2007.00446.x
Norton, M. (2005). New evidence on birth spacing: Promising findings for improving newborn, infant, child, and maternal health. International Journal of Gynecology & Obstetrics, 89, S1–S6. https://doi.org/10.1016/j.ijgo.2004.12.012
Oster, E. (2018). Does disease cause vaccination? Disease outbreaks and vaccination response. Journal of Health Economics, 57, 90–101. https://linkinghub.elsevier.com/retrieve/pii/S016762961730440X
Pimentel, J., et al. (2020). Factors associated with short birth interval in low- and middle-income countries: A systematic review. BMC Pregnancy and Childbirth, 20, 156. https://doi.org/10.1186/s12884-020-2852-z
Rosenzweig, M. R., & Wolpin, K. I. (1988). Heterogeneity, intrafamily distribution, and child health. The Journal of Human Resources, 23, 437. http://www.jstor.org/stable/145808?origin=crossref
Rutstein, S. O. (2005). Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: Evidence from the demographic and health surveys. International Journal of Gynecology & Obstetrics, 89, S7–S24. https://doi.org/10.1016/j.ijgo.2004.11.012
Silver, R. M., et al. (2007). Work-up of stillbirth: A review of the evidence. American Journal of Obstetrics and Gynecology, 196, 433–444. http://linkinghub.elsevier.com/retrieve/pii/S0002937806024136
Simpson, J. L. (2007). Causes of fetal wastage. Clinical Obstetrics and Gynecology, 50, 10–30
Singh, S., Remez, L., Sedgh, G., Kwok, L., & Onda, T. (2018). Abortion worldwide 2017: Uneven progress and unequal access. Tech. Rep., Guttmacher Institute, New York
Smits, L., Pedersen, C., Mortensen, P., & van Os, J. (2004). Association between short birth intervals and schizophrenia in the offspring. Schizophrenia Research, 70, 49–56. https://linkinghub.elsevier.com/retrieve/pii/S0920996403003281
Tomer, Y. (2014). Mechanisms of autoimmune thyroid diseases: From genetics to epigenetics. Annual Review of Pathology: Mechanisms of Disease, 9, 147–156. https://doi.org/10.1146/annurev-pathol-012513-104713
van den Berg, M. M., van Maarle, M. C., van Wely, M., & Goddijn, M. (2012). Genetics of early miscarriage. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease, 1822, 1951–1959. http://linkinghub.elsevier.com/retrieve/pii/S0925443912001494
van Soest, A., & Saha, U. R. (2018). Relationships between infant mortality, birth spacing and fertility in Matlab, Bangladesh. PLoS ONE, 13, e0195940. https://doi.org/10.1371/journal.pone.0195940
Vogl, T. S. (2013). Marriage institutions and sibling competition: Evidence from South Asia. The Quarterly Journal of Economics, 128, 1017–1072. https://academic.oup.com/qje/qje/article/1850653/Marriage
Whitworth, A., & Stephenson, R. (2002). Birth spacing, sibling rivalry and child mortality in India. Social Science & Medicine, 55, 2107–2119. https://linkinghub.elsevier.com/retrieve/pii/S0277953602000023
World Health Organization. (2007). Report of a WHO technical consultation on birth spacing. Tech. Rep. WHO/RHR/07.1, World Health Organization, Geneva, Switzerland
Acknowledgements
We thank two anonymous referees, Alistair Munro, Stephan Litschig, Yoshito Takasaki, Shamma Alam, Sayaka Nakamura, Santos Silva, Santosh Kumar, Yuya Kudo, and seminar participants at the Emerging State Project Young Scholar’s Workshop at GRIPS, Tokyo Labour Economics Workshop 20th Conference, the 12th Applied Microeconometrics Conference at Hitotsubashi, Centre for the Study of African Economies 2018 Conference, Health, Development and Labour Workshop at Hitotsubashi, Japanese Economic Association 2018 Spring Meeting, German Economic Association Research Group on Development Economics 2018 Annual Conference, Hayami Conference 2018, and South Africa Medical Research Council for the helpful comments and suggestions.
Funding
This work was financially supported by the Japan Society for the Promotion of Science, Grant Numbers 25101002, 15H02619, and 18J11688.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This paper is only under review at the Review of Economics of the Household.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagashima, M., Yamauchi, C. Pregnant in haste? The impact of foetus loss on birth spacing and the role of subjective probabilistic beliefs. Rev Econ Household 21, 1409–1431 (2023). https://doi.org/10.1007/s11150-023-09664-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11150-023-09664-8