Abstract
The Helping to End Addiction Long-term (HEAL) Prevention Collaborative (HPC) is designed to expedite the development of programs aimed at preventing opioid misuse and opioid use disorder (OUD) in older adolescents and young adults (ages 16–30). Funded by the National Institutes of Health Office of the Director (ODP-NIH), the HPC includes ten outcome studies that focus on distinct interventions to determine their effectiveness and real-world applicability. Also included is a coordinating center at RTI International that supports the individual projects. This commentary highlights the scientific and practical significance of this cooperative and its promise for facilitating the production and implementation of successful interventions. Attributes such as novel program designs, advanced methodologies, addressing unique characteristics of diverse populations, and real-time analysis of data and costs make this cooperative highly innovative. We note, however, that papers in this Supplemental Issue did not specifically address the persistent need to obtain stronger effect sizes than those achieved to date. Existing data captured earlier in development (< 16 years of age) are uncovering interactive neurocognitive and social-contextual mechanisms underlying the phenomena we wish to prevent. HPC projects could be guided by this information to incorporate developmentally appropriate measures of mechanisms shown previously to be influential in targeted outcomes and determine how they are impacted by specific components of their interventions. This mechanistic information can provide a roadmap for constructing interventions that are more precision-based and, thus, more likely to yield greater benefits for a larger number of recipients. Furthermore, an understanding of underlying mechanism(s) promises to shed light on the sources of heterogeneity in outcomes for further intervention refinement. It is quite possible, if not probable, that meaningful measures of underlying processes will reveal subtypes—some with very high effect sizes and others that are much lower—directly enabling program refinements to more directly target mechanisms that portend and explain less favorable outcomes. Described herein is a full-spectrum translational approach which promises to significantly boost effect sizes, a key objective that should be reached prior to scaling.
Similar content being viewed by others
Introduction
The Helping to End Addiction Long-term (HEAL) Prevention Collaborative (HPC) substantively differs from previous efforts to develop Substance Use Disorder (SUD) preventive interventions in several fundamental ways. The programs are innovatively designed, with particular attention to specific risk characteristics (e.g., high level of exposure to adverse conditions) that frequently occur in subpopulations considered to be at elevated risk for SUD. In addition, the implementation process was accelerated to expedite the transition from program development, refinement, and to efficacy testing and scaling in real-world settings. Notably, social and racial justice concerns, as well as policy issues, are prioritized throughout the research process. The following sections briefly overview the considerable advancements HPC proffer. We then critique the cooperative and call attention to the need for improved understanding of how interventions work, for whom, why, and under what circumstances to improve effect sizes before they are scaled at the community, systems, or population level. As a basis for our critique, we first lay out the translational prevention science framework proposed by Fishbein et al. (2016) for reference throughout subsequent sections.
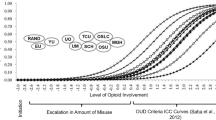
The full spectrum of translational research presented here sequences prevention science into six different phases, as indicated by T0–T5, with the objective to facilitate application of basic science to practice and policy (Fig. 1). According to this model, prevention science should build from a discovery phase (T0) whereby mechanisms that characterize and underlie the phenomena we seek to prevent are delineated. The basic science might be neurobiological in nature or from any other discipline (e.g., behavioral and social science, epidemiology, economics, or developmental psychology) that delves into malleable processes or contexts that give rise to behavioral and mental health issues. Discoveries at this phase are subsequently applied to the development of interventions that more precisely target those malleable mechanisms to improve effect sizes (T1); currently, preventive interventions achieve modest effects at best. Each subsequent step builds progressively in both a stepwise and interactive fashion. Programs that result from the T0 to T1 phase are then subjected to efficacy and effectiveness trials (T2) which reveal heterogeneity in outcomes in need of further explication. That exercise should involve a return to the basic science (i.e., back-translation) to shed light on subtype differences with implications for further program refinement.
The full translational spectrum of prevention science. The translational prevention science framework developed by Fishbein et al. (2016) overlayed on the conception for the HEAL cooperative. The framework is comprised of six different phases (T0–T5) of program development that should be trauma-informed in their scope. The HPC projects focus primarily on T2–T4. Modeling bio-behavioral mechanisms (e.g., levels of stress reactivity, neurocognitive functioning, inhibitory transmitter GABA, and neuroinflammation (Andersen, 2022)) impacted by adverse social determinants of health and that may mediate intervention effects on pathways to OUD is strongly recommended
Once effectiveness has been established, interventions are then applied in real-world settings to determine best fit in the context of the target population with attention to community level and cultural characteristics, preferences, and stated needs (T3). Further dissemination and scaling can occur with some confidence of their ability to improve overall outcomes in an acceptable and accessible format. At the T4 level, there is consensus by the scientific community that the body of knowledge and best practices developed are evidence-based and worthy of translation to policy and public audiences. And finally, at the T5 level, a “culture of prevention” or “normalization” process becomes an achievable goal—one that the USA has yet to reach. This framework is mapped to each of the attributes of the HPC, as designated by the phase of translation in parentheses (e.g., T2).
Streamlining the Translational Process
HPC projects are designed to generate prevention programs that can be disseminated and scaled at the conclusion of the 5-year funding period. These “fast-tracked” projects move through T1 to T4 translation by collecting data on efficacy, economic costs, and implementation, simultaneously. The goal is to have dissemination-ready interventions by the end of their outcome evaluation, reducing the time from development to real-world implementation by about one-third. The more common trajectory is to document efficacy and then effectiveness of a program before conducting a cost–benefit analysis or moving directly to its systematic delivery in real-world settings, such as communities.
Each of the HPC-funded projects described in this special issue is to be commended for their novel approach to facilitate rapid translation of new preventive and treatment interventions. Within the HPC, it was incumbent upon investigators to first identify key factors that hamper innovation and progress. The paper by Ridenour and colleagues (Ridenour et al., 2022) describes how investigators coordinated across studies by standardizing methodologies and measurement instruments. Harmonization of methods and measures allows for direct comparisons across studies and, while this task appears simple on its face, few investigators engage in this exercise, determining their research designs and methodologies based largely on personal perspectives and experiences. The ability to make comparisons across HPC projects allows the uniqueness of each intervention to shine by shedding light on which programs had the greatest impacts on specific types of opioid use and users. In his review of the entire HPC cooperative, Ridenour reveals how consensus was reached by investigators in areas such as variables considered to be of most importance to maximize generalizability of successful interventions for stakeholders in the opioid space. Harmonization of instruments across projects lends itself to identifying common ingredients associated with measurable benefits, thus providing valuable data for secondary analyses to accomplish this aim. Furthermore, Patel et al. (2022) discuss ways in which the HPC overcame barriers to progress for optimal execution of the studies. It should be noted, however, that the projects were not designed to isolate program components primarily responsible for exerting an impact. The review by Yule et al. (in press) identifies several ongoing projects that examine interventions at the individual, parenting, and school levels. Understanding what factors prove to be effective would help to optimize intervention design for any given population (backtranslation from T2 to T0 and then T1).
The fast-tracking nature of the HPC further addresses economic challenges that often impede the expeditious scaling of prevention programs. Included in the HPC were economic analyses conducted for each project that considered the long-term impacts on communities from a cost–benefit perspective. This broad approach is not feasible in the HPC as most of the collaborative studies lack sufficient data. Rather, the analyses rely on a cross-research project analysis with the intended outcome to provide critical guidance to inform decision-making by policy makers and providers (T4).
Dunlap et al. (2022) further describe how members of the consortium collaborated on cost sharing aspects of data collection, analysis, and the start-up of a program and its delivery. While the economic strategies employed are relatively small scale in these early studies, the implications of scaling and real-world implementation are discussed. Individuals within the prevention field have established that several evidence-based interventions are cost and time efficient in the long-term while significantly benefitting recipients. Success of the short-term gains generated by collaboration and cost-sharing achieved by shared methodologies and intentions to harmonize data in the early phases of the HPC may further compel greater investments in preventive interventions as a counterbalance with opioid use disorder (OUD) treatment programs. To paraphrase Benjamin Franklin, “an ounce of prevention is worth a pound of cure;” this adage recognizes the need for increased funding streams to develop, implement, scale, and sustain these programs but has yet to be realized.
Following a yearlong discussion with patients, advocates, academic experts, private sector leaders, and federal partners, NIH identified areas where funding could have the greatest impact on the opiate epidemic. Included among the key findings to emerge from the discourse is the need for improved communication and coordination with community stakeholders and a greater consideration of the unique environments (e.g., home, school, treatment settings) and populations (T3) that are targeted in the development and dissemination of prevention strategies (T1 to T3). By including the community in cooperative research projects during the early stages of developing the HPC, Perry et al. (2022) demonstrate that the resulting program design has increased acceptability and wider dissemination, thereby facilitating scale-up to more communities. The blueprint can then be applied with other geographic areas, sectors, organizations, and populations, with customizations that reflect community needs, preferences, values, and norms. Aherns et al. (2022) and other authors emphasize that interventions for any given population with any measure of success must work within the community or system in which youths are involved to ensure representativeness, cultural sensitivity, and uptake. This community-based participatory feature of the HPC sets it apart from the bulk of studies by providing a platform for key stakeholders to actively partner with researchers to ensure solutions are embraced by and acceptable and relevant to all parties.
Special Populations At-Risk for SUD/OUD
Papers in this special issue signal that the HPC will spur the development of a continuum of care (T3-T4) that progresses from primary-universal programming to indicated-tertiary approaches, particularly for populations at high risk for mental health problems and early or escalating substance use predictive of later OUD (e.g., Cance et al., 2022; Yule et al., 2022). Issues unique to specific populations that require address in the construction and implementation of programs are discussed in detail in several of the papers, including juvenile justice populations (Aherns et al., 2022), adolescents and young adults with mental health issues (Yule et al., 2022), and Native Americans and Alaskans (Komro et al., 2022). For example, Ahrens and colleagues (Aherns et al., 2022) carried out an in-depth analysis of the needs of justice-involved youth. Their study adopted an ecological framework of justice involvement to examine level of opioid use in the context of varying approaches to implementation and a determination of effectiveness and sustainability across different programs. A summary is provided about factors that can influence the uptake, acceptability, and effectiveness of interventions, including prevailing issues, such as COVID-19, discriminatory practices, the role of stakeholders, and adaptability of these programs. The study focusing on young people with mental health issues (Yule et al., 2022), a potent predictor of SUD/OUD, aimed to develop interventions designed to attenuate symptoms and address precipitating factors, such as exposure to child maltreatment and other sources of trauma (T1).
The research designs employed enabled investigators to statistically parse out how various factors—such as the implementation process, individual demographics, and prevailing conditions—contributed to intervention success in the context of the unique characteristics of these populations. Although these conditions are important moderators, there are other malleable factors that could be considered to guide development of program components more specifically targeted to underlying mechanisms and, ultimately, improve effect sizes. Of particular relevance here, given the focus on three special populations, is that marginalized and minoritized groups experience significantly higher rates of adversity (e.g., structural racism, poverty, child maltreatment, trauma, community violence, food insecurity, and other social determinants of health (SDOH)) than more privileged populations (Beech et al., 2021). Thus, the question is whether SDOH effects on factors such as neurodevelopment, cognitive functioning, and stress physiology moderate intervention outcomes; subtypes with developmental delays or dysregulated stress responses, for example, may exhibit poorer outcomes that could benefit from more targeted program components.
Placing HPC Projects in the Context of a Full Translational Model
The HPC possesses numerous attributes that will not only advance the field of substance abuse but may prove to positively impact populations specifically targeted. Notwithstanding, knowledge generated during the T0 phase of research regarding interactions between neural, behavioral, and contextual factors is reviewed within this issue, although more information from the basic sciences is needed to significantly improve the clinical utility, reach and effectiveness of interventions their projects are designed to achieve. We recommend two approaches that build from the HPC to fully capitalize on the iterative translational process. First, follow-up studies that collect biobehavioral measuresFootnote 1 to identify malleable, biobehavioral mediators of programs promise to inform the design and ongoing evaluation of interventions that most effectively move vital mechanistic needles, revealing in the process characteristics of recipients who exact the greatest or fewest benefits. Refinements to the interventions can then be guided by the evidence to positively impact a larger number of recipients. Second, HPC projects could take into account existing data collected during earlier developmental stages, prior to substance use onset, that are reflective of processes underlying key predictors of SUD and that theoretically or empirically map to program components; i.e., the program’s active ingredients can be expected to alter those mechanisms in exerting their effects. Research conducted prior to substance use onset that characterizes pathways to SUD may inform more precise targeting by HPC projects in subsequent investigations. This strategy could, in essence, cover the full course of child, adolescent, and emerging adulthood development without modifying the HPC framework. Guided by mechanistic research conducted to date, projects could clarify the progression of underlying generators and contexts within which substance use initiation and sustainment of that vulnerability to OUD subsequently occurs.
Key Predictors to Increase Clinical Significance
Elucidating individual differences in responsivity via a translational research approach is essential if our aims are to (1) improve the course of a vulnerable trajectory; (2) do so with clinical utility, not just statistical reliability; and (3) ultimately exert significant population level effects. To date, even the most efficacious preventive interventions do not benefit a substantial number of recipients, effect sizes are not indicative of the extent or nature of response variability and therefore provide limited information. To broaden and strengthen program effects, we must systematically apply what we know about the etiological underpinnings of risk behaviors to the refinement of existing programs by identifying and targeting malleable individual characteristics and contextual processes that affect behavioral change. For example, incorporating information about the impacts of exposure to early adversity on developmental trajectories that, in turn, aggravates propensity to opiate misuse later in life demands that programs intervene earlier in the developmental trajectory and with greater specificity.
Normalizing Vulnerable Developmental Trajectories
The Need for Additional T0 Research
Neglecting to explore the fundamental generators of the problems associated with SUD is a missed opportunity that may only lead to partial solutions. One question is whether innovation can truly proceed without T0 to T1 incremental science. The literature is replete with studies of vulnerability and resiliency factors that landscape has been well-excavated. What is lacking, however, are investigations of malleable underlying conditions that mediate developmental trajectories to SUD/OUD and how that information can guide theoretically and empirically driven hypotheses about how specific program components impact those mechanisms. Interventions can then be designed to include ingredients likely to be potent in affecting influential mechanisms and, in turn, ultimate outcomes.
Detecting and Addressing Risk for SUD/OUD Earlier in Development
Indeed, we suggest that there may be common mechanistic clues across these special populations that could offer a roadmap to constructing interventions that more potently move the needle in underlying generators of the phenomena we wish to prevent. For example, the consistent finding that minoritized, underserved, and marginalized groups in our society have greater prevalence of adverse SDOHs is a thread to be explored (Beech et al., 2021). Chronic adversity can harm development of neural circuits that undergird cognitive control over emotion reactivity, stress responses, and healthy relationships (McEwen, 2016), as well as sensitivity to abusable substances (Johnston et al., 2016). The importance of this T0 scientific research is especially pronounced when considering that children often targeted by preventive interventions are at-risk by virtue of exposure adverse SDOHs, e.g., poverty, racism, and child maltreatment. These readily identifiable antecedent conditions that impact infant, child, and adolescent development in ways that influence susceptibility to SUD/OUD (Hefferman et al., 2000; Naqavi et al., 2011) likely represent key commonalities that were not consistently addressed across the HPC projects. A critical consideration for prevention efforts overall is that there are developmental windows of opportunity to intervene, between the time of exposure to adversity and the onset of the SUD/OUD (Andersen & Teicher, 2009; Teicher et al., 2009). Additional factors that further increase risk for SUD/OUD in these populations are the use of painkillers: the odds for painkiller use increases 47% for each additional adverse childhood experience (ACE) experienced by middle and high school children (Forster et al., 2017), being female (Lei et al., 2018), possibly the type of adversity (Andersen & Teicher, 2009), and co-occurring mental health issues (e.g., Yule et al., 2022 in press). An accounting of how individuals are differentially vulnerable (or resilient) to SUD/OUD as a function of adverse experiences and exposures (T0) is critical to identify mechanisms that also portend favorable versus poor responsivity to intervention (T0 to T2).
Statistical Power Gained by Targeting Underlying Mechanisms to Improve Clinical Utility
Bypassing the translation of basic science findings (T0) to program development (T1) carries the risk of generating and disseminating additional interventions with small to modest effects. For the most part, the HPC studies examined factors commonly thought to influence intervention response, including baseline characteristics of individuals (e.g., aggression, academic aptitude), families (e.g., household income, parent–child relationship), communities (e.g., economic stability, access to social services), and, throughout implementation, the quality of that process. The review by Yule et al. (2022) of the ongoing preventive intervention studies scratch the surface of how HPC projects can specifically or differentially target mechanisms that play a role in divergent pathways to an equifinal outcome. As such, while the goal of the HPC projects was reduce OUD risk, the measurable impact at the community or population level may not be achievable. Rather, the preliminary HPC studies show that smaller than desired effects were observed that may (or may not) be accounted for by the interventions impacting only subgroups that may (or may not) be at greatest risk for OUD.
The collection of additional biomarkers reflective of instrumental mechanistic processes and that are malleable may allow for more precise targeting and, thus, more potent effects in any given subgroup. This translational research process promises to improve effect sizes using smaller samples and would further facilitate the mapping of programs’ components to key neurodevelopmental mechanisms (e.g., neurobiological, cognitive, physiological, behavioral) to the phenomena of interest, such as conduct problems or traumatic stress symptoms (T0). This strategy engenders a deeper understanding of the evidence-based response to intervention. Then, with adjustments for predictive factors previously identified at baseline, isolating influential substrates that portend differential responsivity becomes possible.
Stakeholder Interests
Prioritizing research activities within the 6-phase translation framework described above emphasizes the criticality of interactive and multi-directional models with integral input from all vested interests, including local prevention coalitions and other community stakeholders, educators, practitioners, health care professionals, and funders. Throughout the T0, T1, and T2 phases of research, stakeholder involvement is necessary to avoid the pitfalls commonly observed in studies that do not consider the values and expressed needs of populations that are targeted. Investigators, no different from the general lay public, bring to the fore their own biases and lenses from which they see the world and their research approach. Also, socio-economic frameworks that serve to perpetrate adversity and disparities are part of the catchment of individuals at-risk for OUD and needs to be considered. This full-circle environment suggests that if we want to speed-up the development and implementation of prevention programs, individuals who are the recipients of intervention and all those who influence the process must be involved in the earlier stages of program development and clinical trials.
The Future of Prevention: Biomarkers to Consider
Exciting developments in the field of neuroscience with pertinence to the prevention of SUD/OUD are on the horizon. For example, the research establishing a strong connection between trauma, brain change, and propensity for addiction offers some tantalizing clues as to which biological processes are alterable by adverse SDOHs and might be amenable to specific intervention components if appropriately targeted (Elton et al., 2019; McEwen, 2016; Strathearn et al., 2019). And importantly, given rapid change in biology throughout development, we are learning that intervening before the neurobehavioral cascade to substance use accelerates during adolescence is warranted and imperative (Andersen & Teicher, 2009). This body of research further dictates that we focus on positive SDOHs that can be reinforced by well-designed programs and, even more impactfully, system-level and policy change. Such a strategy moves us away from “deficits models” that suggest young people with mental health and substance use problems are somehow defective due to individual-level attributes or environmental influences, and toward of better understanding of how to restructure our environments.
One intriguing example are findings of “hidden talents” in children living in threatening, unsafe, and trauma-filled environments. Research conducted by Bruce Ellis and collaborators (Ellis et al., 2022; Frankenhuis et al., 2020) suggests that children raised in harsh and unpredictable environments develop hypervigilance, memory for negative emotional or stressful events, and heightened attunement to social situations and relationships, creativity, cognition for identifying resources from their environment, reward responsivity, and ability to switch between tasks. These “hidden talents” are currently not addressed in US classrooms; thus, children who live under threatening circumstances and/or have experienced trauma often fall behind. This issue is particularly salient during the COVID-19 crisis. Educational practices that leverage trauma-adapted learning strategies may more effectively reach these children and prevent them from falling through the cracks. Extending from that logic, although the research is still in nascent phase, evidence is emerging that these factors can further mediate intervention responsivity (Ellis et al., 2022; Frisman et al., 2008). Such findings have tremendous potential to provide program developers with information critical to optimizing program design. As these fundamental gaps are filled, interventions can be tailored to more effectively promote adaptive behaviors and reduce risk for SUD and schools and communities can be strengthened to reduce exposure to adversities in the first place (Fishbein, 2021).
A parallel and growing line of research indicates that neurobiological mechanisms are shared between trauma-exposed population and individuals with OUD, information that can be used to predict heightened risk for OUD. First, elevated neuroinflammation (interleukin-6 (IL-6)) and low levels of the inhibitory neurotransmitter GABA contribute to OUD and occur after adversity exposure (Andersen, 2022). Secondly, the timing of adversity exposure may have important implications for understanding elevated risk. Exposure to adversity at different stages of development exerts differential effects on the emergent the neural network architecture and circuits that undergird emotion and behavioral self-regulatory skills (Nusslock & Miller, 2016). Third, maturational processes during adolescence unmask earlier effects of abuse that can help to identify optimal periods of intervention. Based on the National Survey on Drug Use and Health (2002), we determined that 50% of heroin use was initiated by 18 years of age while the initiation of other drugs (stimulants, inhalants, and hallucinogens) earlier than age 18 on average (Andersen & Teicher, 2009). These data raise the possibility that a window of opportunity to prevent opiate use is more protracted in this population. Finally, the type of adversity exposure may also selectively identify individuals at high-risk for opiate use. Emotional abuse, relative to neglect or sexual abuse, has the highest odds ratio of association to OUD (Santo et al., 2021). Additional forms of abuse, including verbal abuse, witnessing domestic violence, physical abuse, and more, each can have their own unique impact although they often co-occur (Diamond et al., 2020). More work is needed to determine if predictive relationships exist between these factors and risk for OUD. Determining whether effective intervention can (1) attenuate associations between adversity and neurodevelopment and (2) lead to improved social functioning would provide strong causal evidence of these linkages and elucidate more specific targets for intervention (Diamond et al., 2020). Also, research is needed to delineate mechanisms that explain resilience in the face of early adversity in those subpopulations (Cay et al., 2022).
Conclusions
Overall, the HPC promises to expedite the research to practice and policy process, from phases T1 to T4. These focused programs purport that advancements they spur will lead to improved effect sizes, thereby exerting greater benefits than traditional, incremental approaches of T0-T3. However, we propose that a combination of strategies is necessary to accomplish that goal. Achieving greater precision requires a theoretical model of intervention effects that identifies malleable bio-behavioral mechanisms and social-contextual processes that account for outcome variability; T0 to T1 offer vital information to clarify the underlying generators of the initiation and maintenance of vulnerability to OUD throughout the lifespan. Translational studies that integrate etiological findings from the developmental neurosciences into biomarkers, social learning theory, and prevention science have potential to elucidate mechanisms of effects that will inform ways in which interventions can be developed anew or refined to broaden and strengthen their ability to prevent later OUD.
Further enhancements to the HPC framework that fundamentally account for basic science findings (T0) and their import for program development (T1), as well as a determination of sources of heterogeneity in outcomes to guide program refinements (T2) will increase efficacy of resultant interventions. With that promise is a greater potential to move the needle in functional indicators that are reflective of change in developmental trajectories. As such, its significance as a blueprint for future program design, implementation, scalability, and sustainability will substantially improve, as will evidence-based systems and policy reforms.
Data Availability
No data are provided in this commentary.
Change history
06 November 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11121-023-01597-z
Notes
It was noted that an IRB declined inclusion of biological data, a barrier that can be overcome with the proper safeguards and documentation of the significant body of research that collects such data from human participants.
References
Aherns, K., Aalsma, M., Haggerty, K., Kelleher, K., Knight, D. K., Joseph, J., & Tolou-Shams, M. (2022). A spectrum of intervention studies to prevent opioid use and substance use disorder in justice-involved youth. Prevention Science.
Andersen, S. L. (2022). Neuroinflammation, early-life adversity, and brain development. Harvard Review of Psychiatry, 30(1), 24–39. https://doi.org/10.1097/HRP.0000000000000325
Andersen, S. L., & Teicher, M. H. (2009). Desperately driven and no brakes: Developmental stress exposure and subsequent risk for substance abuse. Neuroscience and Biobehavioral Reviews, 33(4), 516–524. https://doi.org/10.1016/j.neubiorev.2008.09.009
Beech, B. M., Ford, C., Thorpe, R. J., Jr., Bruce, M. A., & Norris, K. C. (2021). Poverty, racism, and the public health crisis in America. Frontiers in Public Health, 9, 699049. https://doi.org/10.3389/fpubh.2021.699049
Cance, J. D., Adams, E. T., D’Amico, E. J., Palimaru, A., Fernandes, C. S. F., Fiellin, L. E., & Deeds, B. (2022). Leveraging the full continuum of care to prevent opioid use disorder.
Cay, M., Gonzalez-Heydrich, J., Teicher, M. H., van der Heijden, H., Ongur, D., Shinn, A. K., & Upadhyay, J. (2022). Childhood maltreatment and its role in the development of pain and psychopathology. Lancet: Child and Adolescent Health, 6(3), 195–206. https://doi.org/10.1016/S2352-4642(21)00339-4
Diamond, R. M., Brown, K. S., & Miranda, J. (2020). Impact of COVID-19 on the perinatal period through a biopsychosocial systemic framework. Contemporary Family Therapy, 42(3), 205–216. https://doi.org/10.1007/s10591-020-09544-8
Dunlap, L., Kuklinski, M. R., Cowell, A., McCollister, K. E., Bowser, D. M., Campbell, M., & Yilmazer, T. (2022). Economic evaluation design within the HEAL Prevention Cooperative. Prevention Science.
Ellis, B. J., Abrams, L. S., Masten, A. S., Sternberg, R. J., Tottenham, N., & Frankenhuis, W. E. (2022). Hidden talents in harsh environments. Developmental Psychopathology, 34(1), 95–113. https://doi.org/10.1017/S0954579420000887
Elton, A., Stanger, C., James, G. A., Ryan-Pettes, S., Budney, A., & Kilts, C. D. (2019). Intertemporal decision-making-related brain states predict adolescent drug abuse intervention responses. NeuroImage: Clinical, 24, 101968. https://doi.org/10.1016/j.nicl.2019.101968
Fishbein, D. (2021). The pivotal role of prevention science in this syndemic. Prevention Science, 22, 94–99.
Fishbein, D. H., Ridenour, T. A., Stahl, M., & Sussman, S. (2016). The full translational spectrum of prevention science: Facilitating the transfer of knowledge to practices and policies that prevent behavioral health problems. Translational Behavioral Medicine, 6(1), 5–16. https://doi.org/10.1007/s13142-015-0376-2
Forster, M., Gower, A. L., Borowsky, I. W., & McMorris, B. J. (2017). Associations between adverse childhood experiences, student-teacher relationships, and non-medical use of prescription medications among adolescents. Addictive Behaviors, 68, 30–34. https://doi.org/10.1016/j.addbeh.2017.01.004
Frankenhuis, W. E., Young, E. S., & Ellis, B. J. (2020). The hidden talents approach: Theoretical and methodological challenges. Trends in Cognitive Sciences, 24(7), 569–581. https://doi.org/10.1016/j.tics.2020.03.007
Frisman, L., Ford, J., Lin, H. J., Mallon, S., & Chang, R. (2008). Outcomes of trauma treatment using the TARGET model. Journal of Groups in Addiction & Recovery, 3(3–4), 285–303. https://doi.org/10.1080/15560350802424910
Heffernan, K., Cloitre, M., Tardiff, K., Marzuk, P. M., Portera, L., & Leon, A. C. (2000). Childhood trauma as a correlate of lifetime opiate use in psychiatric patients. Addictive Behaviors, 25(5), 797–803. https://doi.org/10.1016/s0306-4603(00)00066-6
Johnston, J. H., Linden, D. E., & van den Bree, M. B. (2016). Combining stress and dopamine based models of addiction: Towards a psycho-neuro-endocrinological theory of addiction. Current Drug Abuse Reviews, 9(1), 61–74.
Komro, K. A., D’Amico, E. J., Dickerson, D. L., Skinner, J. R., Johnson, C. L., Kominsky, T. K., & Etz, K. (2022). Culturally responsive opioid and other drug prevention for American Indian/Alaska Native people: A comparison of reservation- and urban-based approaches. Prevention Science.
Lei, Y., Xi, C., Li, P., Luo, M., Wang, W., Pan, S., & Lu, C. (2018). Association between childhood maltreatment and non-medical prescription opioid use among Chinese senior high school students: The moderating role of gender. Journal of Affective Disorders, 235, 421–427. https://doi.org/10.1016/j.jad.2018.04.070
McEwen, B. S. (2016). In pursuit of resilience: Stress, epigenetics, and brain plasticity. Annals of the New York Academy of Sciences, 1373(1), 56–64. https://doi.org/10.1111/nyas.13020
Naqavi, M. R., Mohammadi, M., Salari, V., & Nakhaee, N. (2011). The relationship between childhood maltreatment and opiate dependency in adolescence and middle age. Addiction and Health, 3(3–4), 92–98. https://www.ncbi.nlm.nih.gov/pubmed/24494122
National Survey on Drug Use and Health. (2002). (NSDUH-2002-DS0001) | SAMHDA (samhsa.gov).
Nusslock, R., & Miller, G. E. (2016). Early-life adversity and physical and emotional health across the lifespan: A neuroimmune network hypothesis. Biological Psychiatry, 80(1), 23–32. https://doi.org/10.1016/j.biopsych.2015.05.017
Patel, S. V., Cance, J. D., Bonar, E. E., Carter, P. M., Dickerson, D. L., Fiellin, L. E., & Lambdin, B. H. (2022). Accelerating solutions for the overdose crisis: An effectiveness-implementation hybrid protocol for the HEAL Prevention Cooperative. Prevention Science.
Perry et al. (2022). Community stakeholder engagement in the development and dissemination of opioid prevention strategies. Prevention Science.
Ridenour, T. A., Cruden, G., Yang, Y., Bonar, E., Rodriguez, A., Saavedra, L., & Fernandes, C. S. (2022). Methodological strategies for harmonizing the heal prevention cooperative’s distinct outcomes studies. Prevention Science, in press.
Santo Jr, T., Campbell, G., Gisev, N., Tran, L. T., Colledge, S., Di Tanna, G. L., & Degenhardt, L. (2021). Prevalence of childhood maltreatment among people with opioid use disorder: A systematic review and meta-analysis. Drug amd Alcohol Dependence, 219, 108459. https://doi.org/10.1016/j.drugalcdep.2020.108459
Strathearn, L., Mertens, C. E., Mayes, L., Rutherford, H., Rajhans, P., Xu, G., Potenza, M. N., & Kim, S. (2019). Pathways relating the neurobiology of attachment to drug addiction. Frontiers in Psychiatry, 10, 737. https://doi.org/10.3389/fpsyt.2019.00737
Teicher, M. H., Samson, J. A., Polcari, A., & Andersen, S. L. (2009). Length of time between onset of childhood sexual abuse and emergence of depression in a young adult sample: A retrospective clinical report. Journal of Clinical Psychiatry, 70(5), 684–691. https://doi.org/10.4088/jcp.08m04235
Yule, A. M., Fernandes, C. S. F., Stormshak, E. A., Yang, Y., Shelley, L., Fiellin, L. E., & Bonar, E. A. (2022). Multidisciplinary strategies for preventing opioid misuse and escalation by targeting mental health symptoms and conditions. Prevention Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
N/A
Informed Consent
N/A
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: the affiliation details for authors Susan L. Andersen and Diana H. Fishbein were incorrectly given as 'The National Prevention Science Coalition to Improve Lives, State College, Oakland, CA 94609, USA' but should have been 'The National Prevention Science Coalition to Improve Lives, Oakland, CA 94609, USA'. Full information regarding the corrections made can be found in the erratum/correction for this article.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Andersen, S.L., Fishbein, D.H. Commentary: Improving the Effectiveness and Utility of the Helping to End Addiction Long-Term (HEAL) Prevention Cooperative: A Full Translational Framework. Prev Sci 24 (Suppl 1), 111–118 (2023). https://doi.org/10.1007/s11121-022-01477-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11121-022-01477-y