ABSTRACT
Purpose
RNA nanoparticles derived from the three-way junction (3WJ) of the pRNA of bacteriophage phi29 DNA packaging motor were previously found to be thermodynamically stable. As the nanoparticles could have potential in ocular drug delivery, the objectives in the present study were to investigate the distribution of pRNA nanoparticles after subconjunctival injection and examine the feasibility to deliver the nanoparticles to the cells of cornea and retina.
Methods
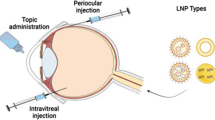
Alexa647-labeled pRNA nanoparticles (pRNA-3WJ and pRNA-X) and double-stranded RNA (dsRNA) were administered via subconjunctival injection in mice. Alexa647 dye was a control. Topical administration was performed for comparison. Ocular clearance of pRNA nanoparticles and dsRNA after the injection was assessed using whole-body fluorescence imaging of the eyes. The numbers of cells in the ocular tissues with nanoparticle cell internalization were determined in fluorescence microscopy of dissected eye tissues.
Results
After subconjunctival injection, pRNA nanoparticles and dsRNA were observed to distribute into the eyes and cleared through the lymph. pRNA-3WJ, pRNA-X, and dsRNA were found in the cells of the conjunctiva, cornea, and sclera, but only pRNA-X was in the cells of the retina. Topical administration was not effective in delivering the nanoparticles to the eye.
Conclusions
The pRNA nanoparticles were delivered to the cells in the eye via subconjunctival injection, and cell internalization was achieved in the cornea with pRNA-3WJ and pRNA-X and in the retina with pRNA-X. Only the X-shape pRNA-X could enter the retina.











Similar content being viewed by others
REFERENCES
Fattal E, Bochot A. Ocular delivery of nucleic acids: antisense oligonucleotides, aptamers and siRNA. Adv Drug Deliv Rev. 2006;58:1203–23.
Pieramici DJ, Rabena MD. Anti-VEGF therapy: comparison of current and future agents. Eye (Lond). 2008;22:1330–6.
de Smet MD, Meenken CJ, van den Horn GJ. Fomivirsen—a phosphorothioate oligonucleotide for the treatment of CMV retinitis. Ocul Immunol Inflamm. 1999;7:189–98.
Ng EW, Shima DT, Calias P, Cunningham Jr ET, Guyer DR, Adamis AP. Pegaptanib, a targeted anti-VEGF aptamer for ocular vascular disease. Nat Rev Drug Discov. 2006;5:123–32.
FDA. A safety and efficacy study of E10030 (anti-PDGF pegylated aptamer) plus Lucentis for neovascular age-related macular degeneration, Clinicaltrials.gov, 2012, NCT01089517.
Lee SS, Robinson MR. Novel drug delivery systems for retinal diseases. A review. Ophthalmic Res. 2009;41:124–35.
Guo P, Zhang C, Chen C, Garver K, Trottier M. Inter-RNA interaction of phage phi29 pRNA to form a hexameric complex for viral DNA transportation. Mol Cell. 1998;2:149–55.
Guo P. The emerging field of RNA nanotechnology. Nat Nanotechnol. 2010;5:833–42.
Guo P, Haque F, Hallahan B, Reif R, Li H. Uniqueness, advantages, challenges, solutions, and perspectives in therapeutics applying RNA nanotechnology. Nucleic Acid Ther. 2012;22:226–45.
Haque F, Shu D, Shu Y, Shlyakhtenko LS, Rychahou PG, Evers BM, et al. Ultrastable synergistic tetravalent RNA nanoparticles for targeting to cancers. Nano Today. 2012;7:245–57.
Liu J, Guo S, Cinier M, Shlyakhtenko LS, Shu Y, Chen C, et al. Fabrication of stable and RNase-resistant RNA nanoparticles active in gearing the nanomotors for viral DNA packaging. ACS Nano. 2011;5:237–46.
Shu D, Shu Y, Haque F, Abdelmawla S, Guo P. Thermodynamically stable RNA three-way junction for constructing multifunctional nanoparticles for delivery of therapeutics. Nat Nanotechnol. 2011;6:658–67.
Macha S, Mitra AK. Ocular pharmacokinetics in rabbits using a novel dual probe microdialysis technique. Exp Eye Res. 2001;72:289–99.
Berezovsky DE, Patel SR, McCarey BE, Edelhauser HF. In vivo ocular fluorophotometry: delivery of fluoresceinated dextrans via transscleral diffusion in rabbits. Invest Ophthalmol Vis Sci. 2011;52:7038–45.
Li SK, Lizak MJ, Jeong EK. MRI in ocular drug delivery. NMR Biomed. 2008;21:941–56.
Kim SH, Lutz RJ, Wang NS, Robinson MR. Transport barriers in transscleral drug delivery for retinal diseases. Ophthalmic Res. 2007;39:244–54.
Urtti A. Challenges and obstacles of ocular pharmacokinetics and drug delivery. Adv Drug Deliv Rev. 2006;58:1131–5.
Gaudana R, Jwala J, Boddu SH, Mitra AK. Recent perspectives in ocular drug delivery. Pharm Res. 2009;26:1197–216.
Maurice D. Review: practical issues in intravitreal drug delivery. J Ocul Pharmacol Ther. 2001;17:393–401.
Dastjerdi MH, Sadrai Z, Saban DR, Zhang Q, Dana R. Corneal penetration of topical and subconjunctival bevacizumab. Invest Ophthalmol Vis Sci. 2011;52:8718–23.
Bejjani RA, BenEzra D, Cohen H, Rieger J, Andrieu C, Jeanny JC, et al. Nanoparticles for gene delivery to retinal pigment epithelial cells. Mol Vis. 2005;11:124–32.
Bourges JL, Gautier SE, Delie F, Bejjani RA, Jeanny JC, Gurny R, et al. Ocular drug delivery targeting the retina and retinal pigment epithelium using polylactide nanoparticles. Invest Ophthalmol Vis Sci. 2003;44:3562–9.
Andrieu-Soler C, Halhal M, Boatright JH, Padove SA, Nickerson JM, Stodulkova E, et al. Single-stranded oligonucleotide-mediated in vivo gene repair in the rd1 retina. Mol Vis. 2007;13:692–706.
Chopra P, Hao J, Li SK. Iontophoretic transport of charged macromolecules across human sclera. Int J Pharm. 2010;388:107–13.
Wen H, Hao J, Li SK. Characterization of human sclera barrier properties for transscleral delivery of bevacizumab and ranibizumab. J Pharm Sci. 2013;102:892–903.
Demetriades AM, Deering T, Liu H, Lu L, Gehlbach P, Packer JD, et al. Trans-scleral delivery of antiangiogenic proteins. J Ocul Pharmacol Ther. 2008;24:70–9.
Amaral J, Fariss RN, Campos MM, Robison Jr WG, Kim H, Lutz R, et al. Transscleral-RPE permeability of PEDF and ovalbumin proteins: implications for subconjunctival protein delivery. Invest Ophthalmol Vis Sci. 2005;46:4383–92.
Kim SH, Galban CJ, Lutz RJ, Dedrick RL, Csaky KG, Lizak MJ, et al. Assessment of subconjunctival and intrascleral drug delivery to the posterior segment using dynamic contrast-enhanced magnetic resonance imaging. Invest Ophthalmol Vis Sci. 2007;48:808–14.
Lee SJ, He W, Robinson SB, Robinson MR, Csaky KG, Kim H. Evaluation of clearance mechanisms with transscleral drug delivery. Invest Ophthalmol Vis Sci. 2010;51:5205–12.
Li SK, Molokhia SA, Jeong EK. Assessment of subconjunctival delivery with model ionic permeants and magnetic resonance imaging. Pharm Res. 2004;21:2175–84.
Lee TW, Robinson JR. Drug delivery to the posterior segment of the eye II: development and validation of a simple pharmacokinetic model for subconjunctival injection. J Ocul Pharmacol Ther. 2004;20:43–53.
Kim SH, Csaky KG, Wang NS, Lutz RJ. Drug elimination kinetics following subconjunctival injection using dynamic contrast-enhanced magnetic resonance imaging. Pharm Res. 2008;25:512–20.
Kim H, Robinson MR, Lizak MJ, Tansey G, Lutz RJ, Yuan P, et al. Controlled drug release from an ocular implant: an evaluation using dynamic three-dimensional magnetic resonance imaging. Invest Ophthalmol Vis Sci. 2004;45:2722–31.
Amrite AC, Kompella UB. Size-dependent disposition of nanoparticles and microparticles following subconjunctival administration. J Pharm Pharmacol. 2005;57:1555–63.
Amrite AC, Edelhauser HF, Singh SR, Kompella UB. Effect of circulation on the disposition and ocular tissue distribution of 20 nm nanoparticles after periocular administration. Mol Vis. 2008;14:150–60.
Chang JH, Garg NK, Lunde E, Han KY, Jain S, Azar DT. Corneal neovascularization: an anti-VEGF therapy review. Surv Ophthalmol. 2012;57:415–29.
Ishikawa S, Hirata A, Nakabayashi J, Iwakiri R, Okinami S. Neuroprotective effect of small interfering RNA targeted to caspase-3 on rat retinal ganglion cell loss induced by ischemia and reperfusion injury. Curr Eye Res. 2012;37:907–13.
Williams KA, Klebe S. Gene therapy for corneal dystrophies and disease, where are we? Curr Opin Ophthalmol. 2012;23:276–9.
Henry SP, Miner RC, Drew WL, Fitchett J, York-Defalco C, Rapp LM, et al. Antiviral activity and ocular kinetics of antisense oligonucleotides designed to inhibit CMV replication. Invest Ophthalmol Vis Sci. 2001;42:2646–51.
Li W, Szoka Jr FC. Lipid-based nanoparticles for nucleic acid delivery. Pharm Res. 2007;24:438–49.
Abdelmawla S, Guo S, Zhang L, Pulukuri SM, Patankar P, Conley P, et al. Pharmacological characterization of chemically synthesized monomeric phi29 pRNA nanoparticles for systemic delivery. Mol Ther. 2011;19:1312–22.
de Fougerolles A, Vornlocher HP, Maraganore J, Lieberman J. Interfering with disease: a progress report on siRNA-based therapeutics. Nat Rev Drug Discov. 2007;6:443–53.
Kim DH, Rossi JJ. Strategies for silencing human disease using RNA interference. Nat Rev Genet. 2007;8:173–84.
Seth S, Johns R, Templin MV. Delivery and biodistribution of siRNA for cancer therapy: challenges and future prospects. Ther Deliv. 2012;3:245–61.
Rozema DB, Lewis DL, Wakefield DH, Wong SC, Klein JJ, Roesch PL, et al. Dynamic PolyConjugates for targeted in vivo delivery of siRNA to hepatocytes. Proc Natl Acad Sci U S A. 2007;104:12982–7.
Nguyen QD, Schachar RA, Nduaka CI, Sperling M, Basile AS, Klamerus KJ, et al. Dose-ranging evaluation of intravitreal siRNA PF-04523655 for diabetic macular edema (the DEGAS study). Invest Ophthalmol Vis Sci. 2012;53:7666–74.
ACKNOWLEDGMENTS AND DISCLOSURES
This paper is dedicated to Dr. Stephen J. Ryan, the founder of the Arnold and Mabel Beckman Initiative for Macular Research. The research was supported in part by NCI Cancer Nanotechnology Platform Partnership Program: RNA Nanotechnology for Cancer Therapy, as the NIH U01 CA151648 program directed by Peixuan Guo; and Beckman Initiative for Macular Research Grant 1108 (to Peixuan Guo) as well as 1210 (to David Gamm and Dan Shu). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH. Funding to P. Guo's Endowed Chair in Nanobiotechnology position is by the William Fairish Endowment Fund. P. Guo is a co-founder of Kylin Therapeutics, Inc., and Biomotor and Nucleic Acid Nanotechnology Development Corp. Ltd.. The authors thank Drs. Winston W-Y. Kao and Ying Xia for providing the AxioCam Observer Z1 microscopes in the study; Dr. Jinsong Hao for her technical support; and Dr. Jiukuan Hao for helpful discussion. The authors also thank Drs. Maria B. Grant for collaboration and discussion; David Gamm, Michael Boulton, and Mark Humayun for constructive comments and inspiring discussion.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feng, L., Li, S.K., Liu, H. et al. Ocular Delivery of pRNA Nanoparticles: Distribution and Clearance After Subconjunctival Injection. Pharm Res 31, 1046–1058 (2014). https://doi.org/10.1007/s11095-013-1226-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-013-1226-x