Abstract
Purpose
Preoperative risk stratification for patients undergoing metastatic brain tumor resection (MBTR) is based on established tumor-, patient-, and disease-specific risk factors for outcome prognostication. Frailty, or decreased baseline physiologic reserve, is a demonstrated independent risk factor for adverse outcomes following MBTR. The present study sought to assess the impact of frailty, measured by the Risk Analysis Index (RAI), on MBTR outcomes.
Methods
All MBTR were queried from the National Inpatient Sample (NIS) from 2019 to 2020 using diagnosis and procedural codes. The relationship between preoperative RAI frailty score and our primary outcome – non-home discharge (NHD) – and secondary outcomes – complication rates, extended length of stay (eLOS), and mortality – were analyzed via univariate and multivariable analyses. Discriminatory accuracy was tested by computation of concordance statistics in area under the receiver operating characteristic (AUROC) curve analysis.
Results
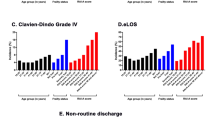
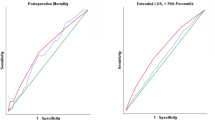
There were 20,185 MBTR patients from the NIS database from 2019 to 2020. Each patient’s frailty status was stratified by RAI score: 0–20 (robust): 34%, 21–30 (normal): 35.1%, 31–40 (very frail): 13.9%, 41+ (severely frail): 16.8%. Compared to robust patients, severely frail patients demonstrated increased complication rates (12.2% vs. 6.8%, p < 0.001), eLOS (37.6% vs. 13.2%, p < 0.001), NHD (52.0% vs. 20.6%, p < 0.001), and mortality (9.9% vs. 4.1%, p < 0.001). AUROC curve analysis demonstrated good discriminatory accuracy of RAI-measured frailty in predicting NHD after MBTR (C-statistic = 0.67).
Conclusion
Increasing RAI-measured frailty status is significantly associated with increased complication rates, eLOS, NHD, and mortality following MBTR. Preoperative frailty assessment using the RAI may aid in preoperative surgical planning and risk stratification for patient selection.

Similar content being viewed by others
References
Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS (2020) CBTRUS Statistical Report: primary brain and other Central Nervous System Tumors diagnosed in the United States in 2013–2017. Neurooncology 22(Supplement1):iv1–iv96. https://doi.org/10.1093/neuonc/noaa200
Amsbaugh MJ, Kim CS (2023) Brain Metastasis. In: StatPearls. StatPearls Publishing; Accessed July 17, 2023. http://www.ncbi.nlm.nih.gov/books/NBK470246/
Hatiboglu MA, Wildrick DM, Sawaya R (2013) The role of surgical resection in patients with brain metastases. Ecancermedicalscience 7:308. https://doi.org/10.3332/ecancer.2013.308
Huff WX, Agrawal N, Shapiro S et al (2018) Efficacy of pre-operative stereotactic radiosurgery followed by surgical resection and correlative radiobiological analysis for patients with 1–4 brain metastases: study protocol for a phase II trial. Radiat Oncol 13(1):252. https://doi.org/10.1186/s13014-018-1178-8
Prabhu RS, Akinyelu T, Vaslow ZK et al (2023) Risk factors for progression and toxic Effects after preoperative stereotactic radiosurgery for patients with resected brain metastases. JAMA Oncol Published Online June 8:e231629. https://doi.org/10.1001/jamaoncol.2023.1629
D’Andrea G, Palombi L, Minniti G, Pesce A, Marchetti P (2017) Brain metastases: Surgical Treatment and overall survival. World Neurosurg 97:169–177. https://doi.org/10.1016/j.wneu.2016.09.054
Proescholdt MA, Schödel P, Doenitz C et al (2021) The management of Brain Metastases—Systematic review of neurosurgical aspects. Cancers (Basel) 13(7):1616. https://doi.org/10.3390/cancers13071616
Ene CI, Ferguson SD (2022) Surgical Management of Brain Metastasis: Challenges and Nuances. Front Oncol 12:847110. https://doi.org/10.3389/fonc.2022.847110
Zaslavsky O, Cochrane BB, Thompson HJ, Woods NF, Herting JR, LaCroix A (2013) Frailty: a review of the first decade of research. Biol Res Nurs 15(4):422–432. https://doi.org/10.1177/1099800412462866
Kerschbaumer J, Krigers A, Demetz M et al (2022) The clinical Frailty Scale as useful tool in patients with brain metastases. J Neurooncol 158(1):51–57. https://doi.org/10.1007/s11060-022-04008-5
Sastry RA, Pertsch NJ, Tang O, Shao B, Toms SA, Weil RJ (2020) Frailty and outcomes after craniotomy for brain tumor. J Clin Neurosci 81:95–100. https://doi.org/10.1016/j.jocn.2020.09.002
Heimann M, Schäfer N, Bode C et al (2021) Outcome of Elderly Patients With Surgically Treated Brain Metastases. Frontiers in Oncology. 11. Accessed July 17, 2023. https://www.frontiersin.org/articles/https://doi.org/10.3389/fonc.2021.713965
Thommen R, Kazim SF, Rumalla K et al (2022) Preoperative frailty measured by risk analysis index predicts complications and poor discharge outcomes after Brain Tumor Resection in a large multi-center analysis. J Neurooncol Published Online October 31. https://doi.org/10.1007/s11060-022-04135-z
Estes EM, Rumalla K, Kazim SF et al (2023) Frailty Measured by the Risk Analysis Index Predicts Nonhome Discharge and Mortality After Resection in Refractory Epilepsy: Analysis of 1236 Patients From a Prospective Surgical Registry, 2012 to 2020. Neurosurgery. Published online February 28, https://doi.org/10.1227/neu.0000000000002439
Link RL, Rumalla K, Courville EN et al (2023) Prospective application of the risk analysis index to measure preoperative frailty in spinal tumor surgery: a single center outcomes analysis. World Neurosurg X 19:100203. https://doi.org/10.1016/j.wnsx.2023.100203
Kassicieh AJ, Rumalla K, Kazim SF, Asserson DB, Schmidt MH, Bowers CA (2022) Preoperative risk model for perioperative stroke after intracranial tumor resection: ACS NSQIP analysis of 30,951 cases. NeuroSurg Focus 53(6):E9. https://doi.org/10.3171/2022.9.FOCUS22402
Bowers CA, Varela S, Conlon M et al (2023) Comparison of the risk analysis index and the modified 5-factor frailty index in predicting 30-day morbidity and mortality after spine surgery. J Neurosurg Spine 39(1):136–145. https://doi.org/10.3171/2023.2.SPINE221019
Skandalakis GP, Medani K, Rumalla K et al (2023) Preoperative frailty and 30-day mortality after resection of brain metastases: a multicenter surgical registry analysis of 11,038 patients. NeuroSurg Focus 55(2):E8. https://doi.org/10.3171/2023.5.FOCUS23198
Lakomkin N, Hadjipanayis CG (2018) Non-routine discharge disposition is associated with post-discharge complications and 30-day readmissions following craniotomy for brain tumor resection. J Neurooncol 136(3):595–604. https://doi.org/10.1007/s11060-017-2689-0
Tang OY, Pugacheva A, Bajaj AI, Rivera Perla KM, Weil RJ, Toms SA (2022) The National Inpatient Sample: a primer for neurosurgical Big Data Research and systematic review. World Neurosurg 162:e198–e217. https://doi.org/10.1016/j.wneu.2022.02.113
Huan-Tze L, Yun-Ru L, Kuan-Der L, Huey-En T (2023) Frailty in chronic myeloid leukemia: evidence from 2016–2018 Nationwide Inpatient Sample of the US. BMC Geriatr 23(1):334. https://doi.org/10.1186/s12877-023-03962-7
Guo Y, Wu H, Sun W, Hu X, Dai J (2022) Effects of frailty on postoperative clinical outcomes of aneurysmal subarachnoid hemorrhage: results from the National Inpatient Sample database. BMC Geriatr 22(1):460. https://doi.org/10.1186/s12877-022-03141-0
Siddiqui E, Banco D, Berger JS, Smilowitz NR (2023) Frailty Assessment and Perioperative Major adverse Cardiovascular events after noncardiac surgery. Am J Med 136(4):372–379e5. https://doi.org/10.1016/j.amjmed.2022.12.033
Covell MM, Rumalla K, Kassicieh AJ et al (2022) Frailty measured by risk analysis index and adverse discharge outcomes after adult spine deformity surgery: analysis of 3104 patients from a prospective surgical registry (2011–2020). Spine J Published Online December 24:S1529. 9430(22)01078-6
Kassicieh AJ, Rumalla K, Segura AC et al (2023) Endoscopic and nonendoscopic approaches to single-level lumbar spine decompression: Propensity score-matched comparative analysis and Frailty-Driven Predictive Model. Neurospine 20(1):119–128. https://doi.org/10.14245/ns.2346110.055
Rumalla K, Kazim SF, Jain P, McKee RG, Schmidt MH, Bowers CA (2023) Preoperative frailty and 30-day mortality after surgery for type II odontoid fracture: a retrospective observational analysis of a large multicenter surgical registry. Spine J 23(6):885–887. https://doi.org/10.1016/j.spinee.2023.02.004
Chowdhury MZI, Turin TC (2020) Variable selection strategies and its importance in clinical prediction modelling. Fam Med Community Health 8(1):e000262. https://doi.org/10.1136/fmch-2019-000262
Theriault BC, Pazniokas J, Adkoli AS et al (2020) Frailty predicts worse outcomes after intracranial meningioma surgery irrespective of existing prognostic factors. NeuroSurg Focus 49(4):E16. https://doi.org/10.3171/2020.7.FOCUS20324
Cole KL, Varela S, Rumalla K et al (2022) Advanced frailty assessment tool predicts successful awake craniotomy in a 92-year-old patient: a case report. Surg Neurol Int 13:404. https://doi.org/10.25259/SNI_542_2022
Patel AJ, Suki D, Hatiboglu MA, Rao VY, Fox BD, Sawaya R (2015) Impact of surgical methodology on the complication rate and functional outcome of patients with a single brain metastasis. J Neurosurg 122(5):1132–1143. https://doi.org/10.3171/2014.9.JNS13939
Khalafallah AM, Jimenez AE, Patel P, Huq S, Azmeh O, Mukherjee D (2020) A novel online calculator predicting short-term postoperative outcomes in patients with metastatic brain tumors. J Neurooncol 149(3):429–436. https://doi.org/10.1007/s11060-020-03626-1
Werner RM, Coe NB, Qi M, Konetzka RT (2019) Patient outcomes after Hospital Discharge to Home with Home Health Care vs to a skilled nursing facility. JAMA Intern Med 179(5):617–623. https://doi.org/10.1001/jamainternmed.2018.7998
Colasacco CJ, Abouezzi J, Arbuiso S et al (2022) Association of baseline frailty and age with postoperative outcomes in metastatic brain tumor patients. J Neurosurg Sci Published Online November 7. https://doi.org/10.23736/S0390-5616.22.05865-9
Huq S, Khalafallah AM, Patel P et al (2021) Predictive model and online calculator for Discharge Disposition in Brain Tumor Patients. World Neurosurg 146:e786–e798. https://doi.org/10.1016/j.wneu.2020.11.018
Picot J, Cooper K, Bryant J, Clegg AJ (2011) Karnofsky performance status and WHO performance status scores. In: The Clinical Effectiveness and Cost-Effectiveness of Bortezomib and Thalidomide in Combination Regimens with an Alkylating Agent and a Corticosteroid for the First-Line Treatment of Multiple Myeloma: A Systematic Review and Economic Evaluation. NIHR Journals Library; Accessed July 17, 2023. https://www.ncbi.nlm.nih.gov/books/NBK97482/
Schmidt AQ, von Euw S, Roy JM et al (2023) Frailty predicts hospital acquired infections after brain tumor resection: analysis of 27,947 patients’ data from a prospective multicenter surgical registry. Clin Neurol Neurosurg 229:107724. https://doi.org/10.1016/j.clineuro.2023.107724
Rumalla K, Thommen R, Kazim SF et al (2023) Risk analysis index and 30-Day mortality after Brain Tumor Resection: a multicenter Frailty Analysis of 31,776 patients from 2012 to 2020. J Neurol Surg B Skull Base. Published Online February 13. https://doi.org/10.1055/a-2015-1162
Berthelsen CL (2000) Evaluation of coding data quality of the HCUP National Inpatient Sample. Top Health Inf Manage 21(2):10–23
Donoho DA, Wen T, Babadjouni RM et al (2018) Predictors of 30- and 90-day readmission following craniotomy for malignant brain tumors: analysis of nationwide data. J Neurooncol 136(1):87–94. https://doi.org/10.1007/s11060-017-2625-3
Jimenez AE, Cicalese KV, Chakravarti S et al (2022) Social determinants of health and the prediction of 90-day mortality among brain tumor patients. J Neurosurg 137(5):1338–1346. https://doi.org/10.3171/2022.1.JNS212829
Carli F, Baldini G (2021) From preoperative assessment to preoperative optimization of frail older patiens. Eur J Surg Oncol 47(3 Pt A):519–523. https://doi.org/10.1016/j.ejso.2020.06.011
Acknowledgements
None.
Funding
The authors did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
M.C. wrote the manuscript draft, revised the manuscript draft, and managed the project. A.W. wrote the manuscript draft. K.R. performed the statistical analyses, prepared Fig. 1, and prepared Tables 1, 2 and 3. C.D. wrote the manuscript draft. C.B. wrote the manuscript draft, revised the manuscript draft, and provided study supervision. All authors reviewed the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Covell, M.M., Warrier, A., Rumalla, K.C. et al. RAI-measured frailty predicts non-home discharge following metastatic brain tumor resection: national inpatient sample analysis of 20,185 patients. J Neurooncol 164, 663–670 (2023). https://doi.org/10.1007/s11060-023-04461-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04461-w