Abstract
Introduction
Almost 50% of children with intracranial ependymoma experience disease relapse, and their outcomes are extremely poor. The aim of this study was to investigate optimal salvage treatment for pediatric intracranial ependymoma after the first relapse and to identify prognostic factors affecting survival.
Methods
We conducted a retrospective analysis of 159 children who underwent initial treatment for intracranial ependymoma at Beijing Tiantan Hospital from 2013 to 2017.
Results
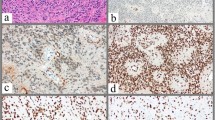
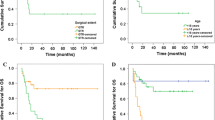
Relapse was observed in 73 patients (73/159; 45.9%), with a median age of 7.2 ± 3.5 years old. Molecular subgrouping analysis identified H3K27me3-negative PF-EPNs in 74% of patients, ST-RELA EPNs in 21% of patients, and H3K27me3-positive PF-EPNs in 5% of patients. The 5-year event-free survival (EFS) and overall survival (OS) rates after first relapse were 21.1% (95% CI 16.0–26.2) and 30.5% (95% CI 19.8–30.8), respectively. Patients with GTR at first relapse had higher 5-year EFS and 5-year OS than those with STR (P = 0.031 and P = 0.003) or no surgery (P = 0.007 and P = 0.001). Radiotherapy or re-radiotherapy at first relapse significantly prolonged 5-year EFS and OS (both P < 0.001). Patients with H3K27me3-negative PF-EPN had worse 5-year EFS and OS than those with ST-RELA EPN (P = 0.001 and P = 0.002). Multivariate analysis showed that both tumor resection and radiotherapy at first relapse had independent prognostic significance for survival (all P < 0.05).
Conclusion
Children with recurrent intracranial EPN have poor outcomes, and surgery and radiotherapy at first relapse should be encouraged to improve their prognosis.




Similar content being viewed by others
Data availability
The dataset and material are available from the corresponding authors on reasonable request.
Code availability
Not applicable.
References
Ostrom QT, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS (2021) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2014–2018. Neuro Oncol 23:iii1-iii105. https://doi.org/10.1093/neuonc/noab200
McGuire CS, Sainani KL, Fisher PG (2009) Incidence patterns for ependymoma: a surveillance, epidemiology, and end results study. J Neurosurg 110:725–729. https://doi.org/10.3171/2008.9.JNS08117
Pajtler KW, Witt H, Sill M et al (2015) Molecular classification of ependymal tumors across all CNS compartments, histopathological grades, and age groups. Cancer Cell 27:728–743. https://doi.org/10.1016/j.ccell.2015.04.002
Witt H, Mack SC, Ryzhova M et al (2011) Delineation of two clinically and molecularly distinct subgroups of posterior fossa ependymoma. Cancer Cell 20:143–157. https://doi.org/10.1016/j.ccr.2011.07.007
Merchant TE, Li C, Xiong X, Kun LE, Boop FA, Sanford RA (2009) Conformal radiotherapy after surgery for paediatric ependymoma: a prospective study. Lancet Oncol 10:258–266. https://doi.org/10.1016/s1470-2045(08)70342-5
Ruda R, Reifenberger G, Frappaz D, Pfister SM, Laprie A, Santarius T, Roth P, Tonn JC, Soffietti R, Weller M, Moyal EC (2018) EANO guidelines for the diagnosis and treatment of ependymal tumors. Neuro Oncol 20:445–456. https://doi.org/10.1093/neuonc/nox166
Pejavar S, Polley MY, Rosenberg-Wohl S, Chennupati S, Prados MD, Berger MS, Banerjee A, Gupta N, Haas-Kogan D (2012) Pediatric intracranial ependymoma: the roles of surgery, radiation and chemotherapy. J Neurooncol 106:367–375. https://doi.org/10.1007/s11060-011-0671-9
Grundy RG, Wilne SA, Weston CL et al (2007) Primary postoperative chemotherapy without radiotherapy for intracranial ependymoma in children: the UKCCSG/SIOP prospective study. Lancet Oncol 8:696–705. https://doi.org/10.1016/S1470-2045(07)70208-5
Massimino M, Miceli R, Giangaspero F et al (2016) Final results of the second prospective AIEOP protocol for pediatric intracranial ependymoma. Neuro Oncol 18:1451–1460. https://doi.org/10.1093/neuonc/now108
Merchant TE, Bendel AE, Sabin ND et al (2019) Conformal radiation therapy for pediatric ependymoma, chemotherapy for incompletely resected ependymoma, and observation for completely resected, supratentorial ependymoma. J Clin Oncol 37:974–983. https://doi.org/10.1200/JCO.18.01765
Ritzmann TA, Rogers HA, Paine SML, Storer LCD, Jacques TS, Chapman RJ, Ellison D, Donson AM, Foreman NK, Grundy RG (2020) A retrospective analysis of recurrent pediatric ependymoma reveals extremely poor survival and ineffectiveness of current treatments across central nervous system locations and molecular subgroups. Pediatr Blood Cancer 67:e28426. https://doi.org/10.1002/pbc.28426
Zacharoulis S, Ashley S, Moreno L, Gentet JC, Massimino M, Frappaz D (2010) Treatment and outcome of children with relapsed ependymoma: a multi-institutional retrospective analysis. Childs Nerv Syst 26:905–911. https://doi.org/10.1007/s00381-009-1067-4
Byer L, Kline CN, Coleman C, Allen IE, Whitaker E, Mueller S (2019) A systematic review and meta-analysis of outcomes in pediatric, recurrent ependymoma. J Neurooncol 144:445–452. https://doi.org/10.1007/s11060-019-03255-3
Massimino M, Barretta F, Modena P et al (2021) Second series by the Italian Association of Pediatric Hematology and Oncology of children and adolescents with intracranial ependymoma: an integrated molecular and clinical characterization with a long-term follow-up. Neuro Oncol 23:848–857. https://doi.org/10.1093/neuonc/noaa257
Tsai JW, Manoharan N, Alexandrescu S et al (2021) Outcomes after first relapse of childhood intracranial ependymoma. Pediatr Blood Cancer e28930. https://doi.org/10.1002/pbc.28930
Adolph JE, Fleischhack G, Mikasch R et al (2021) Local and systemic therapy of recurrent ependymoma in children and adolescents: short- and long-term results of the E-HIT-REZ 2005 study. Neuro Oncol 23:1012–1023. https://doi.org/10.1093/neuonc/noaa276
Tsang DS, Burghen E, Klimo P Jr, Boop FA, Ellison DW, Merchant TE (2018) Outcomes after reirradiation for recurrent pediatric intracranial ependymoma. Int J Radiat Oncol Biol Phys 100:507–515. https://doi.org/10.1016/j.ijrobp.2017.10.002
Merchant TE, Boop FA, Kun LE, Sanford RA (2008) A retrospective study of surgery and reirradiation for recurrent ependymoma. Int J Radiat Oncol Biol Phys 71:87–97. https://doi.org/10.1016/j.ijrobp.2007.09.037
Bouffet E, Hawkins CE, Ballourah W, Taylor MD, Bartels UK, Schoenhoff N, Tsangaris E, Huang A, Kulkarni A, Mabbot DJ, Laperriere N, Tabori U (2012) Survival benefit for pediatric patients with recurrent ependymoma treated with reirradiation. Int J Radiat Oncol Biol Phys 83:1541–1548. https://doi.org/10.1016/j.ijrobp.2011.10.039
Bouffet E, Capra M, Bartels U (2009) Salvage chemotherapy for metastatic and recurrent ependymoma of childhood. Childs Nerv Syst 25:1293–1301. https://doi.org/10.1007/s00381-009-0883-x
DeWire M, Fouladi M, Turner DC et al (2015) An open-label, two-stage, phase II study of bevacizumab and lapatinib in children with recurrent or refractory ependymoma: a collaborative ependymoma research network study (CERN). J Neurooncol 123:85–91. https://doi.org/10.1007/s11060-015-1764-7
Komori K, Yanagisawa R, Miyairi Y et al (2016) Temozolomide treatment for pediatric refractory anaplastic ependymoma with low MGMT protein expression. Pediatr Blood Cancer 63:152–155. https://doi.org/10.1002/pbc.25696
Antony R, Wong KE, Patel M, Olch AJ, McComb G, Krieger M, Gilles F, Sposto R, Erdreich-Epstein A, Dhall G, Gardner S, Finlay JL (2014) A retrospective analysis of recurrent intracranial ependymoma. Pediatr Blood Cancer 61:1195–1201. https://doi.org/10.1002/pbc.24996
Lobon MJ, Bautista F, Riet F et al (2016) Re-irradiation of recurrent pediatric ependymoma: modalities and outcomes: a twenty-year survey. Springerplus 5:879. https://doi.org/10.1186/s40064-016-2562-1
Saito R, Kumabe T, Kanamori M, Sonoda Y, Tominaga T (2010) Dissemination limits the survival of patients with anaplastic ependymoma after extensive surgical resection, meticulous follow up, and intensive treatment for recurrence. Neurosurg Rev 33:185–191; discussion 191–182. https://doi.org/10.1007/s10143-010-0243-z
De B, Khakoo Y, Souweidane MM, Dunkel IJ, Patel SH, Gilheeney SW, De Braganca KC, Karajannis MA, Wolden SL (2018) Patterns of relapse for children with localized intracranial ependymoma. J Neurooncol 138:435–445. https://doi.org/10.1007/s11060-018-2815-7
Zhao F, Wu T, Wang LM, Zhang J, Zhang H, Li SW, Zhang S, Li P, Wang B, Luo L, Liu PN (2021) Survival and prognostic factors of adult intracranial ependymoma: a single-institutional analysis of 236 patients. Am J Surg Pathol. https://doi.org/10.1097/pas.0000000000001669
Massimino M, Barretta F, Modena P et al (2021) Treatment and outcome of intracranial ependymoma after first relapse in AIEOP 2nd protocol. Neuro Oncol. https://doi.org/10.1093/neuonc/noab230
Messahel B, Ashley S, Saran F et al (2009) Relapsed intracranial ependymoma in children in the UK: patterns of relapse, survival and therapeutic outcome. Eur J Cancer 45:1815–1823. https://doi.org/10.1016/j.ejca.2009.03.018
Gupta T, Maitre M, Gupta P et al (2020) Extent of re-excision, sequence/timing of salvage re-irradiation, and disease-free interval impact upon clinical outcomes in recurrent/progressive ependymoma. J Neurooncol 147:405–415. https://doi.org/10.1007/s11060-020-03434-7
Panwalkar P, Clark J, Ramaswamy V et al (2017) Immunohistochemical analysis of H3K27me3 demonstrates global reduction in group—a childhood posterior fossa ependymoma and is a powerful predictor of outcome. Acta Neuropathol 134:705–714. https://doi.org/10.1007/s00401-017-1752-4
Kilday JP, Mitra B, Domerg C et al (2012) Copy number gain of 1q25 predicts poor progression-free survival for pediatric intracranial ependymomas and enables patient risk stratification: a prospective European clinical trial cohort analysis on behalf of the Children’s Cancer Leukaemia Group (CCLG), Societe Francaise d’Oncologie Pediatrique (SFOP), and International Society for Pediatric Oncology (SIOP). Clin Cancer Res 18:2001–2011. https://doi.org/10.1158/1078-0432.CCR-11-2489
Junger ST, Andreiuolo F, Mynarek M et al (2020) CDKN2A deletion in supratentorial ependymoma with RELA alteration indicates a dismal prognosis: a retrospective analysis of the HIT ependymoma trial cohort. Acta Neuropathol 140:405–407. https://doi.org/10.1007/s00401-020-02169-z
Pajtler KW, Mack SC, Ramaswamy V et al (2017) The current consensus on the clinical management of intracranial ependymoma and its distinct molecular variants. Acta Neuropathol 133:5–12. https://doi.org/10.1007/s00401-016-1643-0
Author information
Authors and Affiliations
Contributions
Conception and design: FZ, YT; Development of methodology: FZ, YT; Acquisition of data: CL, ZL., TS, WL, ZH; Analysis and interpretation of data: ZL., BL, JW, ZH, FZ; Writing, review, and/or revision of the manuscript: FZ, YT; Administrative, technical, or material support: ZL., CL, JG; Study supervision: FZ, YT, JG.
Corresponding authors
Ethics declarations
Conflict of interest
The authors indicated no potential conflicts of interest.
Consent to participate
All patients or legal guardians provided written informed consent to participate in this study.
Consent for publication
All patients or legal guardians provided written informed consent to publish their data.
Ethical approval
This study was approved by the ethics committee of Beijing Tiantan Hospital, Capital Medical University. The use of the clinical data was conducted in conformity with the institutional review boards (KY 2020-090-02).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Zm., Han, Z., Wang, Jm. et al. Treatment and outcome of pediatric intracranial ependymoma after first relapse. J Neurooncol 157, 385–396 (2022). https://doi.org/10.1007/s11060-022-03975-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-03975-z