Abstract
Purpose
The role of transsphenoidal surgery in the recovery of preexisting hormone dysfunction from pituitary tumors remains controversial. This study aimed to investigate the incidence of hormone dysfunction among asymptomatic non-functioning pituitary adenomas and their recovery following endoscopic transsphenoidal surgery.
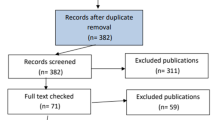
Methods
Eligibility criteria included age under 80 years, presence of a non-functioning pituitary adenoma compressing the normal gland resulting in deviation of the stalk, absence of visual symptoms, and availability for regular follow-up using MRI and pre- and post-operative endocrinological assessments. 182 patients with silent non-functioning pituitary adenomas were included in this study between March 2014 and December 2018. All patients underwent endoscopic transsphenoidal surgery and complete hormonal evaluation, with basal hormone assays and a combined pituitary function test before and after surgery until the end of last follow-up.
Results
Preoperative assessment of hormonal function revealed that 124 of 182 patients (68.1%) had at least a single hormone dysfunction preoperatively. Among these, 61 of 124 (49.2%) had a dysfunction in a single axis, and 63 (50.8%) had a hormone dysfunction in two or more axes. Overall, the median endocrinological follow-up duration was 15.0 months (6–57 months). At 1 month following surgery, 91 patients (73.4%) with hormone dysfunction experienced improvement in at least a single hormone axis. Prolactin was the most common hormone among those that recovered at the last follow up (92.8% improvement) followed by growth hormone (GH, 50.0%), thyroid stimulating hormone (TSH, 50.0%), gonadotropin (Gn, 46.9%), and adrenocorticotropic hormone (ACTH, 45.0%). Time to recovery varied from 1.1 months (for prolactin) to 2.2 months (for gonadotropin, and ACTH). In patients with preoperative deficiency in GH, and ACTH, postoperative transient diabetes insipidus was associated with poor recovery (GH: HR = 0.50, p = 0.048; ACTH: HR = 0.39, p = 0.023).
Conclusions
Non-functioning pituitary adenomas with silent hormone dysfunction are often overlooked by clinicians and patients. We suggest that even silent hormone dysfunction in patients with non-functioning pituitary adenomas can be improved with effective surgical decompression and these tumors may be potential indications of endoscopic transsphenoidal surgery.



Similar content being viewed by others
Data availability
The manuscript has no mandatory deposition data and will not be deposited.
References
Abdelmannan D, Aron DC (2010) Incidentally discovered pituitary masses: pituitary incidentalomas. Expert Rev Endocrinol Metab 5:253–264. https://doi.org/10.1586/eem.09.68
Iglesias P, Arcano K, Trivino V, Garcia-Sancho P, Diez JJ, Villabona C, Cordido F (2017) Prevalence, clinical features, and natural history of incidental clinically non-functioning pituitary adenomas. Horm Metab Res 49:654–659. https://doi.org/10.1055/s-0043-115645
Paschou SA, Vryonidou A, Goulis DG (2016) Pituitary incidentalomas: a guide to assessment, treatment and follow-up. Maturitas 92:143–149. https://doi.org/10.1016/j.maturitas.2016.08.006
Arafah BM (1986) Reversible hypopituitarism in patients with large nonfunctioning pituitary adenomas. J Clin Endocrinol Metab 62:1173–1179. https://doi.org/10.1210/jcem-62-6-1173
Berkmann S, Fandino J, Muller B, Remonda L, Landolt H (2012) Intraoperative MRI and endocrinological outcome of transsphenoidal surgery for non-functioning pituitary adenoma. Acta Neurochir 154:639–647. https://doi.org/10.1007/s00701-012-1285-5
Fatemi N, Dusick JR, Mattozo C, McArthur DL, Cohan P, Boscardin J, Wang C, Swerdloff RS, Kelly DF (2008) Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63:709–718. https://doi.org/10.1227/01.NEU.0000325725.77132.90
Nomikos P, Ladar C, Fahlbusch R, Buchfelder M (2004) Impact of primary surgery on pituitary function in patients with non-functioning pituitary adenomas—a study on 721 patients. Acta Neurochir 146:27–35. https://doi.org/10.1007/s00701-003-0174-3
Wichers-Rother M, Hoven S, Kristof RA, Bliesener N, Stoffel-Wagner B (2004) Non-functioning pituitary adenomas: endocrinological and clinical outcome after transsphenoidal and transcranial surgery. Exp Clin Endocrinol Diabetes 112:323–327. https://doi.org/10.1055/s-2004-820914
Webb SM, Rigla M, Wagner A, Oliver B, Bartumeus F (1999) Recovery of hypopituitarism after neurosurgical treatment of pituitary adenomas. J Clin Endocrinol Metab 84:3696–3700. https://doi.org/10.1210/jcem.84.10.6019
Jahangiri A, Wagner JR, Han SW, Tran MT, Miller LM, Chen R, Tom MW, Ostling LR, Kunwar S, Blevins L, Aghi MK (2016) Improved versus worsened endocrine function after transsphenoidal surgery for nonfunctional pituitary adenomas: rate, time course, and radiological analysis. J Neurosurg 124:589–595. https://doi.org/10.3171/2015.1.JNS141543
Goshtasbi K, Abiri A, Sahyouni R, Mahboubi H, Raefsky S, Kuan EC, Hsu FPK, Cadena G (2019) Visual and endocrine recovery following conservative and surgical treatment of pituitary apoplexy: a meta-analysis. World Neurosurg 132:33–40. https://doi.org/10.1016/j.wneu.2019.08.115
Sam S, Molitch ME (2005) The pituitary mass: diagnosis and management. Rev Endocr Metab Disord 6:55–62. https://doi.org/10.1007/s11154-005-5225-z
Ajlan AM, Abdulqader SB, Achrol AS, Aljamaan Y, Feroze AH, Katznelson L, Harsh GR (2018) Diabetes insipidus following endoscopic transsphenoidal surgery for pituitary adenoma. J Neurol Surg B Skull Base 79:117–122. https://doi.org/10.1055/s-0037-1604363
Yildirim AE, Sahinoglu M, Ekici I, Cagil E, Karaoglu D, Celik H, Nacar OA, Belen AD (2016) Nonfunctioning pituitary adenomas are really clinically nonfunctioning? Clinical and endocrinological symptoms and outcomes with endoscopic endonasal treatment. World Neurosurg 85:185–192. https://doi.org/10.1016/j.wneu.2015.08.073
Cho KR, Hong SD, Hur KY, Kim ST, Seol HJ, Lee JI, Kong DS, Nam DH (2016) Serial re-expansion of pituitary gland is associated with endocrinologic recovery. World Neurosurg 90:496–503. https://doi.org/10.1016/j.wneu.2016.03.050
Castinetti F, Dufour H, Gaillard S, Jouanneau E, Vasiljevic A, Villa C, Trouillas J (2015) Non-functioning pituitary adenoma: when and how to operate? What pathologic criteria for typing? Ann Endocrinol 76:220–227. https://doi.org/10.1016/j.ando.2015.04.007
Molitch ME (2017) Diagnosis and treatment of pituitary adenomas: a review. JAMA 317:516–524. https://doi.org/10.1001/jama.2016.19699
Ogiwara T, Nagm A, Nakamura T, Mbadugha T, Horiuchi T, Hongo K (2019) Significance and indications of surgery for asymptomatic nonfunctioning pituitary adenomas. World Neurosurg 128:e752–e759. https://doi.org/10.1016/j.wneu.2019.04.250
Huang W, Molitch ME (2018) Management of nonfunctioning pituitary adenomas (NFAs): observation. Pituitary 21:162–167. https://doi.org/10.1007/s11102-017-0856-0
Hong SD, Nam DH, Kong DS, Kim HY, Chung SK, Dhong HJ (2016) Endoscopic modified transseptal transsphenoidal approach for maximal preservation of sinonasal quality of life and olfaction. World Neurosurg 87:162–169. https://doi.org/10.1016/j.wneu.2015.12.050
Hong SD, Nam DH, Seol HJ, Choi NY, Kim HY, Chung SK, Dhong HJ (2015) Endoscopic binostril versus transnasal transseptal microscopic pituitary surgery: sinonasal quality of life and olfactory function. Am J Rhinol Allergy 29:221–225. https://doi.org/10.2500/ajra.2015.29.4165
Taylor DG, Jane JA, Oldfield EH (2018) Resection of pituitary macroadenomas via the pseudocapsule along the posterior tumor margin: a cohort study and technical note. J Neurosurg 128:422–428. https://doi.org/10.3171/2017.7.JNS171658
Lee EJ, Ahn JY, Noh T, Kim SH, Kim TS, Kim SH (2009) Tumor tissue identification in the pseudocapsule of pituitary adenoma: should the pseudocapsule be removed for total resection of pituitary adenoma? Neurosurgery 64:ONS62–ONS69. https://doi.org/10.1227/01.NEU.0000330406.73157.49
Laws ER Jr, Iuliano SL, Cote DJ, Woodmansee W, Hsu L, Cho CH (2016) A benchmark for preservation of normal pituitary function after endoscopic transsphenoidal surgery for pituitary macroadenomas. World Neurosurg 91:371–375. https://doi.org/10.1016/j.wneu.2016.04.059
Harary M, DiRisio AC, Dawood HY, Kim J, Lamba N, Cho CH, Smith TR, Zaidi HA, Laws ER (2018) Endocrine function and gland volume after endoscopic transsphenoidal surgery for nonfunctional pituitary macroadenomas. J Neurosurg 131(4):1–10. https://doi.org/10.3171/2018.5.JNS181054
Freda P, Katznelson L, Molitch M (2011) The hormone foundation’s patient guide to pituitary incidentaloma assessment and treatment. J Clin Endocrinol Metab 96:35a–36a. https://doi.org/10.1210/jcem.96.4.zeg35a
Freda PU, Beckers AM, Katznelson L, Molitch ME, Montori VM, Post KD, Vance ML (2011) Pituitary incidentaloma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96:894–904. https://doi.org/10.1210/jc.2010-1048
Acknowledgements
We would like to thank Editage (www.editage.co.kr) for English language editing.
Author information
Authors and Affiliations
Contributions
DSK conceived and designed the study. MHL, and KYH analyzed the data and wrote the manuscript. SDH, HJS, JWC, JIL, and DHN provided and collected data.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. No funds, grants, or other support was received.
Ethical approval
The study was approved by the appropriate institutional research ethics committee (Samsung Medical Center) and certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. As the study is retrospective study, the informed consent was waived by ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, M.H., Hur, K.Y., Hong, S.D. et al. Early hormonal recovery following endoscopic transsphenoidal surgery for silent non-functioning pituitary adenomas with hormone dysfunction. J Neurooncol 153, 343–350 (2021). https://doi.org/10.1007/s11060-021-03774-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03774-y