Abstract
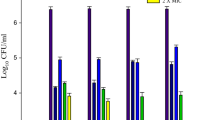
Candida glabrata is one of most prevalent yeast in fungal infections, especially in immunocompromised patients. Its azole resistance results in a low therapeutic response, particularly when associated with biofilms. The main goal of this work was to study the effectiveness of voriconazole (Vcz) against C. glabrata biofilms oral pathologies, as esophageal or oropharyngeal candidiasis. Antifungal susceptibilities were determined in pre-formed 24-h-biofilms and ERG genes expression was determined by qRT-PCR. Protein quantification was performed using BCA® Kit, carbohydrate was estimated according to the Dubois assay and β-1,3 glucans concentration were determined using Glucatell® kit. Finally, ergosterol, Vcz, and fluconazole (Flu) concentrations within the biofilm matrices were determined by RP-HPLC. Results showed that C. glabrata biofilms were more susceptible to Vcz than to Flu and that ERG genes expression evidenced an overexpression of the three ERG genes in the presence of both azoles. The matrix content presented a remarked decrease in proteins and an increase in carbohydrates, namely β-1,3 glucans. Ergosterol was successfully detected and quantified in the biofilm matrices, with no differences in all the considered conditions. Vcz demonstrated better diffusion through the biofilms and better cell penetration capacities, than Flu, indicating that the structure of the drug molecule fully influences its dissemination through the biofilm matrices. This work showed that Vcz is notably more effective than Flu for the treatment of resistant C. glabrata oral biofilms, which demonstrates a clinical relevance in its future use for the treatment of oropharyngeal/esophageal candidiasis caused by this species.


Similar content being viewed by others
References
Eggimann P, Garbino JPD. Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect Dis. 2003;3:685–702.
Shao P, Huang L, Hsueh P. Recent advances and challenges in the treatment of invasive fungal infections. Int J Antimicrob Agents. 2007;30:487–95.
Kaur R, Domergue R, Zupancic ML, Cormack BP. A yeast by any other name: Candida glabrata and its interaction with the host. Curr Opin Microbiol. 2005;8:378–84.
Pfaller M, Diekema D. Twelve years of fluconazole in clinical practice: global trends in species distribution and fluconazole susceptibility of bloodstream isolates of Candida. Clin Microbiol Infect. 2004;10:11–23.
Bethea EK, Carver BJ, Montedonico AE, Reynolds TB. The inositol regulon controls viability in Candida glabrata. Microbiology. 2010;156:452–62.
Hasosah MY, Showail M, Al-Sahafi A, Satti M, Jacobson K. Esophageal candidiasis in an immunocompetent girl. World J Pediatr. 2009;5:152–4.
Mimidis K, Papadopoulos V, Margaritis V, Thomopoulos K, Gatopoulou A, Nikolopoulou V, et al. Predisposing factors and clinical symptoms in HIV-negative patients with Candida oesophagitis: are they always present? Int J Clin Pract. 2005;59:210–3.
Marti CJ, Alvarez RM. Herpes simplex esophagitis associated to Candida albicans in an immunocompetent host. An Med Interna. 2004;21:312.
Sathyanarayanan V, Razak A, Prabhu MM, Saravu K, Ganesh PC, Rao AK. A case report of herpetic and candidal esophagitis in an immunocompetent adult. Asian Pac J Trop Biomed. 2011;1:251–2.
Xu S, Shen J. Newer antifungal agents micafungin and voriconazole for fungal infection prevention during hematopoietic cell transplantation: a meta-analysis. Eur Rev Med Pharmacol Sci. 2016;20:381–90.
Sanguinetti M, Posteraro B, Fiori B, Ranno S, Torelli R, Fadda G. Mechanisms of azole resistance in clinical isolates of Candida glabrata collected during a hospital survey of antifungal resistance. Antimicrob Agents Chemother. 2005;49:668–79.
Ma C, Li F, Shi L, Hu Y, Wang Y, Huang M, et al. Surveillance study of species distribution, antifungal susceptibility and mortality of nosocomial candidemia in a tertiary care hospital in China. BMC Complement Altern Med. 2013;13:337.
Neofytos D, Huprikar S, Reboli A, Schuster M, Azie N, Franks B, et al. Treatment and outcomes of Candida osteomyelitis: review of 53 cases from the PATH Alliance® registry. Eur J Clin Microbiol Infect Dis. 2014;33:135–41.
Pawar P, Kashyap H, Malhotra S, Sindhu R. Hp-β-CD voriconazole in situ gelling system for ocular drug delivery: in vitro, stability, and antifungal activities assessment. Biomed Res Int. 2013;2013:341218.
Chang T, Ho M, Yang Y, Lo P, Lin P, Wang A, et al. Distribution and drug susceptibilities of Candida species causing candidemia from a medical center in central Taiwan. J Infect Chemother. 2013;19:1065–71.
Sean M, Seenu M, William F, Gaurav K, Michael D, Gilbert M. Management of endogenous fungal endophthalmitis with voriconazole and caspofungin. Am J Ophthalmol. 2005;139:135–40.
Chen K, Wu W, Sun M, Lai C, Chao A. Endogenous fungal endophthalmitis: causative organisms, management strategies, and visual acuity outcomes. Am J Ophthalmol. 2012;154:213–4.
Chang Y, Yang C, Lee F, Lee S. Voriconazole for Candida endophthalmitis. Ophthalmology. 2012;119:2414–5.
Pfaller MA, Messer SA, Rhomberg PR, Jones RN, Castanheira M. In vitro activities of isavuconazole and comparator antifungal agents tested against a global collection of opportunistic yeasts and molds. J Clin Microbiol. 2013;51:2608–16.
Chander J, Singla N, Sidhu S, Gombar S. Epidemiology of Candida blood stream infections: experience of a tertiary care centre in North India. J Infect Dev Ctries. 2013;7:670–5.
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2015;62:e1–50.
Williams DW, Wilson MJ, Lewis MAO, Potts AJC. Identification of Candida species by PCR and restriction fragment length polymorphism analysis of intergenic spacer regions of ribosomal DNA. J Clin Microbiol. 1995;33:2476–9.
Silva S, Negri M, Henriques M, Oliveira R, Williams D, Azeredo J. Silicone colonization by non-Candida albicans Candida species in the presence of urine. J Med Microbiol. 2010;59:747–54.
DuBois M, Gilles K, Hamilton J, Rebers P, Smith F. Colorimetric method for determination of sugars and related substances. Anal Chem. 1956;28:350–6.
Marin S, Morales H, Ramos AJ, Sanchis V. Evaluation of growth quantification methods for modelling the growth of Penicillium expansum in an apple-based medium. J Sci Food Agric. 2006;86:1468–74.
Pfaffl MW, Tichopad A, Prgomet C, Neuvians TP. Determination of stable housekeeping genes, differentially regulated target genes and sample integrity: BestKeeper–Excel-based tool using pair-wise correlations. Biotechnol Lett. 2004;26:509–15.
Rodrigues CF, Silva S, Azeredo J, Henrique M. Detection and quantification of fluconazole within Candida glabrata biofilms. Mycopathologia. 2015;179:391–5.
Ibrahim A, Eldin B, Ibrahim A, Eldin B, Shalaby A. Determination of voriconazole and its degradation products in pharmaceutical formulations using high performance liquid chromatography with ultra–violet detection. Eurasian J Anal Chem. 2010;5:254–64.
Sadasivudu P, Shastri N, Sadanandam M. Development and validation of RP-HPLC and UV methods of analysis for fluconazole in pharmaceutical solid dosage forms. Int J ChemTech Res. 2009;1:1131–6.
Fukuoka T, Johnson DA, Winslow CA, de Groot MJ, Burt C, Hitchcock CA, Filler SG. Genetic basis for differential activities of fluconazole and voriconazole against Candida krusei. Antimicrob Agents Chemother. 2003;47:1213–9.
Gallagher J, Dodds Ashley E, Drew R, Perfect J. Antifungal pharmacotherapy for invasive mould infections. Expert Opin Pharmacother. 2003;4:147.
de Groot PWJ, Kraneveld Ea, Yin QY, Dekker HL, Gross U, Crielaard W, et al. The cell wall of the human pathogen Candida glabrata: differential incorporation of novel adhesin-like wall proteins. Eukaryot Cell. 2008;7:1951–64.
Fidel P, Vazquez J, Sobel J. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev. 1999;12:80–96.
Arnold T, Dotson E, Sarosi G, Hage C. Traditional and emerging antifungal therapies. Proc Am Thorac Soc. 2010;7:222–8.
Alcazar-Fuoli L, Mellado E. Current status of antifungal resistance and its impact on clinical practice. Br J Haematol. 2014;166:471–84.
West L, Lowman D, Mora-Montes H, Grubb S, Murdoch C, Thornhill M, et al. Differential virulence of Candida glabrata glycosylation mutants. Biol Chem. 2013;288:22006–18.
Aghdam MRF, Sund S. Invasive esophageal Candidiasis with chronic mediastinal abscess and fatal pneumomediastinum. Am J Case Rep. 2016;17:466–71.
Wilheim AB, Miranda-Filho DDB, Nogueira RA, Rêgo RS, Lima KDM, Pereira LM (2009) The resistance to fluconazole in patients with esophageal candidiasis. Arq Gastroenterol. 2009;46:32–7.
European Committee on Antimicrobial Susceptibility Testing – Antifungal agents, Breakpoint tables for interpretation of MICs, Version 8.0, valid from 2015-11-16. http://www.eucast.org/clinical_breakpoints/
Kowalsdy S, Dixon D. Fluconazole: a new antifungal agent. Clin Pharm. 1990;10:179–90.
Janssen P, Vanden J, Bossche H. Mode of action cytochrome P450 monooxygenase inhibitors. Focus on azole derivates. Arch Pharm Chem Sci. 1987;15:23–40.
Ferrari S, Sanguinetti M, De Bernardis F, Torelli R, Posteraro B, Vandeputte P, et al. Loss of mitochondrial functions associated with azole resistance in Candida glabrata results in enhanced virulence in mice. Antimicrob Agents Chemother. 2011;55:1852–60.
Al-fattani Ma, Douglas LJ. Penetration of Candida biofilms by antifungal agents. Antimicrob Agents Chemother. 2004;48:3291–7.
De Luca C, Guglielminetti M, Ferrario A, Calabrò M, Casari E. Candidemia: species involved, virulence factors and antimycotic susceptibility. New Microbiol. 2012;35:459–68.
Grandesso S, Sapino B, Mazzuccato S, Solinas M, Bedin M, D’Angelo M, et al. Study on in vitro susceptibility of Candida spp. isolated from blood culture. Infect Med. 2012;20:25–30.
Lewis R, Kontoyiannis D, Darouiche R, Raad I, Prince R. Antifungal activity of amphotericin B, fluconazole, and voriconazole in an in vitro model of Candida catheter-related bloodstream infection. Antimicrob Agents Chemother. 2002;46:3499–505.
Donlan R, Costerton J. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15:167–93.
Osawa K, Shigemura K, Yoshida H, Fujisawa M, Arakawa S. Candida urinary tract infection and Candida species susceptibilities to antifungal agents. J Antibiot (Tokyo). 2013;66:651–4.
Narita A, Muramatsu H, Sakaguchi H, Doisaki S, et al. Correlation of CYP2C19 phenotype with voriconazole plasma concentration in children. J Pediatr Hematol Oncol. 2013;35(5):e21.
Caira M, Alkhamis K, Obaidat R. Preparation and crystal characterization of a polymorph, a monohydrate, and an ethyl acetate solvate of the antifungal fluconazole. J Pharm Sci. 2004;93:601–61.
Henry K, Nickels J, Edlind T. Upregulation of ERG genes in Candida species by azoles and other sterol biosynthesis inhibitors. Antimicrob Agents Chemother. 2000;44:2693–700.
Berila N, Hyroššová P, Subík J. Oxidative stress response and virulence factors in Candida glabrata clinical isolates. Folia Microbiol (Praha). 2011;56:116–21.
Tzu Shan N, Desa MNM, Sandai D, Chong PP, Than LTL. Growth, biofilm formation, antifungal susceptibility and oxidative stress resistance of Candida glabrata are affected by different glucose concentrations. Infect Genet Evol Elsevier B.V. 2015;40:331–8.
Cuéllar-Cruz M, López-Romero E, Ruiz-Baca E, Zazueta-Sandoval R. Differential response of Candida albicans and Candida glabrata to oxidative and nitrosative stresses. Curr Microbiol. 2014;69:733–9.
Jandric Z, Gregori C, Klopf E, Radolf M, Schüller C. Sorbic acid stress activates the Candida glabrata high osmolarity glycerol MAP kinase pathway. Front Microbiol. 2013;4:350.
Miyazaki T, Kohno S. ER stress response mechanisms in the pathogenic yeast Candida glabrata and their roles in virulence. Virulence. 2014;5:365–70.
Taff HT, Nett JE, Zarnowski R, Ross KM, Sanchez H, Cain MT, et al. A Candida biofilm-induced pathway for matrix glucan delivery: implications for drug resistance. PLoS Pathog. 2012;8:e1002848.
Zarnowski R, Westler WM, Lacmbouh GA, Marita JM, Bothe JR, Bernhardt J, et al. Novel entries in a fungal biofilm matrix encyclopedia. MBio. 2014;5:1–13.
Lewis RE, Viale P, Kontoyiannis DP. The potential impact of antifungal drug resistance mechanisms on the host immune response to Candida. Virulence. 2012;3:368–76.
Acknowledgements
This work was supported by the Programa Operacional, Fatores de competitividade—COMPETE and by national funds through FCT—Fundação para a Ciência e a Tecnologia on the scope of the projects FCT [PTDC/SAU-MIC/119069/2010], [RECI/EBB-EBI/0179/2012], [PEst-OE/EQB/LA0023/2013] and Célia F. Rodrigues’ [SFRH/BD/93078/2013] PhD Grant. The authors thank the Project “BioHealth—Biotechnology and Bioengineering approaches to improve health quality”, Ref. NORTE-07-0124-FEDER-000027, co-funded by the Programa Operacional Regional do Norte (ON.2—O Novo Norte), QREN, FEDER. The authors would like to acknowledge Pfizer®, S.A. for the kindly donation of Voriconazole and Fluconazole.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that there is no financial/personal interest or belief that could affect their objectivity.
Rights and permissions
About this article
Cite this article
Rodrigues, C.F., Gonçalves, B., Rodrigues, M.E. et al. The Effectiveness of Voriconazole in Therapy of Candida glabrata’s Biofilms Oral Infections and Its Influence on the Matrix Composition and Gene Expression. Mycopathologia 182, 653–664 (2017). https://doi.org/10.1007/s11046-017-0135-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-017-0135-7