Abstract
The STAT4 has been found to be a susceptible gene in the development of systemic lupus erythematosus (SLE) in various populations. There are evident population differences in the context of clinical manifestations of SLE, therefore we investigated the prevalence of the STAT4 G > C (rs7582694) polymorphism in patients with SLE (n = 253) and controls (n = 521) in a sample of the Polish population. We found that patients with the STAT4 C/G and CC genotypes exhibited a 1.583-fold increased risk of SLE incidence (95 % CI = 1.168–2.145, p = 0.003), with OR for the C/C versus C/G and G/G genotypes was 1.967 (95 % CI = 1.152–3.358, p = 0.0119). The OR for the STAT4 C allele frequency showed a 1.539-fold increased risk of SLE (95 % CI = 1.209–1.959, p = 0.0004). We also observed an increased frequency of STAT4 C/C and C/G genotypes in SLE patients with renal symptoms OR = 2.259 (1.365–3.738, p = 0.0014), (p corr = 0.0238) and in SLE patients with neurologic manifestations OR = 2.867 (1.467–5.604, p = 0.0016), (p corr = 0.0272). Moreover, we found a contribution of STAT4 C/C and C/G genotypes to the presence of the anti-snRNP Ab OR = 3.237 (1.667–6.288, p = 0.0003), (p corr = 0.0051) and the presence of the anti-Scl-70 Ab OR = 2.665 (1.380–5.147, p = 0.0028), (p corr = 0.0476). Our studies confirmed an association of the STAT4 C (rs7582694) variant with the development of SLE and occurrence of some clinical manifestations of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a chronic autoimmune disorder characterized by the development of an immune response directed against any parts of the host body [1]. The course of SLE is unpredictable, with periods of remission and flare-ups [1]. Moreover, this autoimmune disorder is vastly heterogeneous, with various clinical manifestations including malar and discoid rash, photosensitivity, arthritis, serositis, as well as renal, neurologic, hematologic, immunologic and mucocutaneous manifestations, and biosynthesis of a broad array of autoantibodies [1]. The occurrence of SLE is nine times frequent in pre-menopausal women than in men [1].
It is accepted that environmental factors together with genetic components are involved in the abnormal immune responses and pathogenesis of SLE [2–6]. Flare-ups of SLE can be triggered by various environmental components, such as exposure to ultraviolet light, drugs, chemicals, and viral infections [6]. Candidate gene and genome wide association studies revealed numerous susceptibility genes of SLE, and the association of some of these genes have been confirmed among distinct populations [3].
The immune cells from patients with SLE display many abnormalities, including reduced T cell cytotoxicity, abnormal function of CD4+ T cells, abnormal activation of B cells, and alterations in cytokine biosynthesis [7–9]. The STAT (signal transducer and activator of transcription) 4 gene is expressed in T and B cells, monocytes, macrophages, natural killer cells, and dendritic cells [10]. STAT4 is a transcription factor and a member of the STAT family [10]. Its expression may support the differentiation of immune cells to inflammatory subsets, production of inflammatory cytokines and autoantibodies, prevention of apoptosis, and presentation of autoantigens, which may promote the development of autoimmune diseases [10].
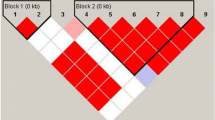
Several genome-wide association studies have identified STAT4 as an SLE susceptible gene in Caucasian and Asian populations [4, 5]. Recently, many studies have demonstrated the contribution of intronic single nucleotide polymorphisms (SNPs) of STAT4 G > C (rs7582694) and G > T (rs7574865) to the incidence of SLE and its clinical manifestations [11–19]. Both of these polymorphisms display complete linkage disequilibrium (LD) in Asian and Caucasian populations presented in HapMap CHB data (http://hapmap.ncbi.nlm.nih.gov/).
We studied the STAT4 G > C (rs7582694) polymorphism distribution in SLE patients in a sample from a Polish cohort. As SLE is a heterogeneous disorder, we also assessed the association of these polymorphisms with various clinical symptoms of SLE and the production of autoantibodies.
Patients and methods
Patients and controls
Data for two hundred and fifty-three women fulfilling the American College of Rheumatology Classification criteria for SLE [20, 21] were collected in a random manner for the study at the Institute of Rheumatology in Warsaw, Poland (Table 1). Controls included five hundred and twenty-one unrelated healthy volunteers and healthy women selected during medical examination at the Institute of Mother and Child, Warsaw. Women with SLE and controls were of Polish and Caucasian origin and of a similar age. The mean age of SLE patients at diagnosis was 34 ± 8 years, and of controls 33 ± 7 years. All participating subjects provided written consent. The study procedures were approved by the Local Ethical Committee of Poznań University of Medical Sciences.
Genotyping
DNA was isolated from peripheral leucocytes using a standard salting out procedure. Identification of the STAT4 C > G (rs7582694) polymorphic variant was performed by polymerase chain reaction-restriction fragment length polymorphism (PCR–RFLP). PCR was conducted employing primer pair 5′ ATCCAACTCTTCTCAGCCCTT 3′ and 5′ TCATAATCAGGAGAGAGGAGT 3′. The PCR-amplified fragments of STAT4 that were 338 bp in length were isolated and digested with the endonuclease HpyCH4III (ACN/GT) NewEngland BioLabs, (Ipswich, USA). The STAT4 C allele was cleaved into 258 and 80 bp fragments, whereas the STAT4 G allele remained uncut. DNA fragments were separated by electrophoresis on 3 % agarose gel and visualized by ethidium bromide staining. The STAT4 C > G polymorphism was confirmed by repeated PCR–RFLP. The genotyping quality was examined by direct sequencing of approximately 10 % of the all samples.
Statistical analysis
The distribution of genotypes in patients and controls was examined for deviation from Hardy–Weinberg equilibrium using exact and log likelihood ratio χ2 tests (http://ihg.gsf.de/cgi-bin/hw/hwa1.pl). The polymorphism was tested for association with SLE incidence using the χ2 test for trend (p trend). The χ2 test was employed to examine differences in genotypic and allelic distribution between patients and controls, and a p value <0.05 was considered statistically significant. The Odds Ratio (OR) and 95 % Confidence Intervals (95 % CI) were calculated. Contribution of the STAT4 C > G polymorphism to clinical manifestations and the production of autoantibodies (Ab) was determined by χ2 test. The Bonferroni correction for multiple comparisons was used and both p values, before (p) and after correction (p corr), were determined. Power analysis was performed using uncorrected χ2 test using Power and Sample Size Calculation program version 2.1.30.
Results
Prevalence of STAT4 G > C polymorphism in SLE patients and healthy individuals
Distribution of STAT4 G > C genotypes did not display significant deviation from Hardy–Weinberg equilibrium between patients and healthy individuals. The prevalence of the STAT4 C/C genotype was 1.8-fold times higher in patients with SLE than in healthy individuals (Table 2). The STAT4 C/G heterozygous frequency in patients was higher than in controls and amounted to 37 and 31 %, respectively (Table 2). The OR for SLE patients with the C/C genotype as compared to the C/G and G/G genotypes was 1.967 (95 % CI = 1.152–3.358, p = 0.0119) and OR for the C/C and C/G genotypes as compared to the G/G genotype was 1.583 (95 % CI = 1.168–2.145, p = 0.0030) (Table 2; Figure 1S, online supplementary data).
To evaluate the effect of the minor allele as a risk factor in SLE incidence, we also assessed the minor allele’s distribution in patients and healthy individuals. The frequency of the STAT4 C allele was higher in patients with SLE compared to healthy individuals, with frequencies of 30 and 22 %, respectively (Table 2). The OR for the STAT4 C allele frequency showed a 1.539-fold increased risk of SLE (95 % CI = 1.209–1.959, p = 0.0004) (Table 2; Figure 1S, online supplementary data). The p value of the χ2 test for the trend observed for the STAT4 G > C polymorphism was also statistically significant (p trend = 0.0008). The statistical power of this study amounted to 84 % for the C/C or C/G genotypes and 69 % for the C/C genotype (Table 2).
Contribution of STAT4 G > C polymorphism to clinical manifestations and production of autoantibodies in patients with SLE
We found an association between STAT4 C/C and C/G genotypes with renal OR = 2.259 (1.365–3.738, p = 0.0014), (p corr = 0.0238) and neurologic manifestations OR = 2.867 (1.467–5.604, p = 0.0016), (p corr = 0.0272) of the disease (Table 1; Figure 2S, online supplementary data). Moreover, we observed a significant association between the STAT4 C/C and C/G genotypes and the presence of anti-snRNP Ab OR = 3.237 (1.667–6.288, p = 0.0003), (p corr = 0.0051). There was also significant association between the C/C and C/G genotypes and the anti-Scl-70 Ab OR = 2.665 (1.380–5.147, p = 0.0028), (p corr = 0.0476) (Table 3; Figure 3S, online supplementary data).
Discussion
STATs include DNA-interacting transcription factors that trigger the expression of the DNA’s target genes by recognizing specific DNA regulatory sequences [10]. The expression of STATs has been observed in a vast range of cell types, however the expression of STAT4 mainly takes place in immune cells and the testis [22]. STAT4 is essential for signal transduction by interleukin-12 (IL-12), interleukin-23 (IL-23), and type 1 interferon (IFN) in T cells and monocytes [10]. IL-12 induces the STAT4-dependent NK cell activation and differentiation of naive CD4+ lymphocytes into Th1 effector cells and IFNγ production [23–25]. STAT4 also mediates the IL-23-dependent expansion of Th17 cells, contributing to autoimmune diseases [26]. It has been demonstrated that STAT4-deficient mice display reduced manifestation of T cell-linked experimental autoimmune diseases including encephalomyelitis, arthritis, myocarditis, colitis, and autoimmune diabetes [10]. Moreover, STAT4 deficiency results in a reduction of IFNγ biosynthesis in immune cells [10]. Accordingly, an association between disease activity in SLE patients and activation of the type 1 IFN system has been observed [27].
We observed that STAT4 G > C (rs7582694) intronic substitution may significantly increase the risk of SLE occurrence in a sample of the Polish population. Recent studies carried out by Luan et al. [28] demonstrated a statistically significant contribution of STAT4 G > C (rs7582694) to SLE incidence in the Mainland Chinese female population. The association of the STAT4 G > T (rs7574865) polymorphism with SLE development was also previously observed in other Asian ethnic groups residing in Hong Kong, Northern Han of China, and Japan [14–19]. The contribution of the STAT4 G > C (rs7582694) or STAT4 G > T (rs7574865) polymorphisms to SLE incidence was also observed in large groups of patients of European origin, among them a Finnish family cohort as well as Spanish, Swedish and other populations [11–13, 29, 30]. The SNP rs7574865 has also been confirmed as a genetic risk factor in the incidence of SLE in Colombian, Mexican, and Argentinian cohorts [30, 31]. However, the rs7574865 polymorphism has not been found to be a risk factor for SLE in the Turkish population [32].
In our study, patients with the STAT4 C/C or G/C genotypes exhibited a significantly increased risk of developing either renal or neurologic manifestations of SLE.
An association between the STAT4 G > T (rs7574865) polymorphism and nepthritis has also been demonstrated in Americans of European descent [11]. Moreover, the contribution of STAT4 G > C (rs7582694) or STAT4 G > T (rs7574865) SNPs to the production of double-stranded DNA autoantibodies has been found in Swedish and American Europeans [11, 12, 33]. The STAT4 G > T (rs7574865) SNP has also been associated with antiphospholipid syndrome in Italian cohorts [34], as has the production of anti-Sm antibodies in a Northern Han Chinese population [15]. Additionally, other STAT4 SNPs were correlated with lupus nephritis, arthritis, and the production of anti-SSA/B autoantibodies in a Northern Han Chinese population [15]. The different effects of the STAT4 G > C (rs7582694) or STAT4 G > T (rs7574865) SNPs on clinical manifestations in various ethnicities may result from different sizes of the studied groups, genetic heterogeneity or patient interaction with disparate environmental factors [6].
STAT4 gene variants have also been found to be risk factors for other autoimmune diseases including rheumatoid arthritis, Crohn’s disease, asthma, systemic sclerosis, and Sjogren’s syndrome [35–39].
The role of STAT4 G > C (rs7582694) or STAT4 G > T (rs7574865) SNPs in the expression of STAT4 have been studied [12, 30]. Abelson et al. (2009) used quantitative PCR to demonstrate significantly higher levels of STAT4 mRNA in mononuclear cells bearing the SLE risk TT genotypes as compared to cells having the GG or GT genotypes of the rs7574865 SNP [30]. Moreover, Sigurdsson et al. [12] indicated that gene variants having the rs8179673 SNP in almost perfect pair-wise LD with rs7582694 led to over-expression of STAT4 in pooled primary human osteoblasts.
Our genetic studies are consistent with other studies that have demonstrated the STAT4 G > C (rs7582694) intronic substitution as a significant risk factor of SLE incidence. Moreover, we found that this SNP can be associated with renal and neurological symptoms of SLE. Since this autoimmune disease is vastly heterogeneous, further studies of this polymorphism’s effects on clinical manifestations of SLE in other populations would be valuable.
References
Sekigawa I, Naito T, Hira K, Mitsuishi K, Ogasawara H, Hashimoto H, Ogawa H (2004) Possible mechanisms of gender bias in SLE: a new hypothesis involving a comparison of SLE with atopy. Lupus 13:217–222
Warchoł T, Lianeri M, Łacki JK, Jagodziński PP (2010) SDF1-3’ G801A polymorphisms in Polish patients with systemic lupus erythematosus. Mol Biol Rep 37:3121–3125
Harley IT, Kaufman KM, Langefeld CD, Harley JB, Kelly JA (2009) Genetic susceptibility to SLE: new insights from fine mapping and genome-wide association studies. Nat Rev Genet 10:285–290
International Consortium for Systemic Lupus Erythematosus Genetics (SLEGEN), Harley JB, Alarcón-Riquelme ME, Criswell LA, Jacob CO, Kimberly RP, Moser KL, Tsao BP, Vyse TJ, Langefeld CD, Nath SK, Guthridge JM, Cobb BL, Mirel DB, Marion MC, Williams AH, Divers J, Wang W, Frank SG, Namjou B, Gabriel SB, Lee AT, Gregersen PK, Behrens TW, Taylor KE, Fernando M, Zidovetzki R, Gaffney PM, Edberg JC, Rioux JD, Ojwang JO, James JA, Merrill JT, Gilkeson GS, Seldin MF, Yin H, Baechler EC, Li QZ, Wakeland EK, Bruner GR, Kaufman KM, Kelly JA (2008) Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat Genet 40:204–210
Han JW, Zheng HF, Cui Y, Sun LD, Ye DQ, Hu Z, Xu JH, Cai ZM, Huang W, Zhao GP, Xie HF, Fang H, Lu QJ, Xu JH, Li XP, Pan YF, Deng DQ, Zeng FQ, Ye ZZ, Zhang XY, Wang QW, Hao F, Ma L, Zuo XB, Zhou FS, Du WH, Cheng YL, Yang JQ, Shen SK, Li J, Sheng YJ, Zuo XX, Zhu WF, Gao F, Zhang PL, Guo Q, Li B, Gao M, Xiao FL, Quan C, Zhang C, Zhang Z, Zhu KJ, Li Y, Hu DY, Lu WS, Huang JL, Liu SX, Li H, Ren YQ, Wang ZX, Yang CJ, Wang PG, Zhou WM, Lv YM, Zhang AP, Zhang SQ, Lin D, Li Y, Low HQ, Shen M, Zhai ZF, Wang Y, Zhang FY, Yang S, Liu JJ, Zhang XJ (2009) Genome-wide association study in a Chinese Han population identifies nine new susceptibility loci for systemic lupus erythematosus. Nat Genet 41:1234–1237
Jönsen A, Bengtsson AA, Nived O, Truedsson L, Sturfelt G (2007) Gene-environment interactions in the aetiology of systemic lupus erythematosus. Autoimmunity 40:613–617
Crispín JC, Tsokos GC (2008) Novel molecular targets in the treatment of systemic lupus erythematosus. Autoimmun Rev 7:256–261
Stohl W, Metyas S, Tan SM, Cheema GS, Xu D, Oamar B, Roschke V, Wu Y, Baker KP, Hilbert DM (2003) B lymphocyte stimulator overexpression in patients with systemic lupus erythematosus: longitudinal observations. Arthritis Rheum 48:3475–3486
Al-Janadi M, Al-Balla S, Al-Dalaan A, Raziuddin S (1993) Cytokine profile in systemic lupus erythematosus, rheumatoid arthritis, and other rheumatic diseases. J Clin Immunol 13:58–67
Kaplan MH (2005) STAT4: a critical regulator of inflammation in vivo. Immunol Res 31:231–242
Taylor KE, Remmers EF, Lee AT, Ortmann WA, Plenge RM, Tian C, Chung SA, Nititham J, Hom G, Kao AH, Demirci FY, Kamboh MI, Petri M, Manzi S, Kastner DL, Seldin MF, Gregersen PK, Behrens TW, Criswell LA (2008) Specificity of the STAT4 genetic association for severe disease manifestations of systemic lupus erythematosus. PLoS Genet 4:e1000084
Sigurdsson S, Nordmark G, Garnier S, Grundberg E, Kwan T, Nilsson O, Eloranta ML, Gunnarsson I, Svenungsson E, Sturfelt G, Bengtsson AA, Jönsen A, Truedsson L, Rantapää-Dahlqvist S, Eriksson C, Alm G, Göring HH, Pastinen T, Syvänen AC, Rönnblom L (2008) A risk haplotype of STAT4 for systemic lupus erythematosus is overexpressed, correlates with anti-dsDNA and shows additive effects with two risk alleles of IRF5. Hum Mol Genet 17:2868–2876
Hellquist A, Sandling JK, Zucchelli M, Koskenmies S, Julkunen H, D’Amato M, Garnier S, Syvänen AC, Kere J (2009) Variation in STAT4 is associated with systemic lupus erythematosus in a finnish family cohort. Ann Rheum Dis 69:883–886
Yang W, Ng P, Zhao M, Hirankarn N, Lau CS, Mok CC, Chan TM, Wong RW, Lee KW, Mok MY, Wong SN, Avihingsanon Y, Lee TL, Ho MH, Lee PP, Wong WH, Lau YL (2009) Population differences in SLE susceptibility genes: STAT4 and BLK, but not PXK, are associated with systemic lupus erythematosus in Hong Kong Chinese. Genes Immun 10:219–226
Li P, Cao C, Luan H, Li C, Hu C, Zhang S, Zeng X, Zhang F, Zeng C, Li Y (2011) Association of genetic variations in the STAT4 and IRF7/KIAA1542 regions with systemic lupus erythematosus in a Northern Han Chinese population. Hum Immunol 72:249–255
Su Y, Zhao Y, Liu X, Guo JP, Jiang Q, Liu XY, Zhang FC, Zheng Y, Li XX, Song H, Huang CB, Huang YH, Wang T, Pan SS, Li C, Liu X, Zhu L, Zhang CF, Li ZG (2010) Variation in STAT4 is associated with systemic lupus erythematosus in Chinese Northern Han population. Chin Med J (Engl) 123:3173–3177
Kiyohara C, Washio M, Horiuchi T, Tada Y, Asami T, Ide S, Atsumi T, Kobashi G, Takahashi H, Kyushu Sapporo SLE (KYSS) Study Group (2009) Cigarette smoking, STAT4 and TNFRSF1B polymorphisms, and systemic lupus erythematosus in a Japanese population. J Rheumatol 36:2195–2203
Kawasaki A, Ito I, Hikami K, Ohashi J, Hayashi T, Goto D, Matsumoto I, Ito S, Tsutsumi A, Koga M, Arinami T, Graham RR, Hom G, Takasaki Y, Hashimoto H, Behrens TW, Sumida T, Tsuchiya N (2008) Role of STAT4 polymorphisms in systemic lupus erythematosus in a Japanese population: a case-control association study of the STAT1-STAT4 region. Arthritis Res Ther 10:R113
Kobayashi S, Ikari K, Kaneko H, Kochi Y, Yamamoto K, Shimane K, Nakamura Y, Toyama Y, Mochizuki T, Tsukahara S, Kawaguchi Y, Terai C, Hara M, Tomatsu T, Yamanaka H, Horiuchi T, Tao K, Yasutomo K, Hamada D, Yasui N, Inoue H, Itakura M, Okamoto H, Kamatani N, Momohara S (2008) Association of STAT4 with susceptibility to rheumatoid arthritis and systemic lupus erythematosus in the Japanese population. Arthritis Rheum 58:1940–1946
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Yamamoto K, Kobayashi H, Arai A, Miura O, Hirosawa S, Miyasaka N (1997) cDNA cloning, expression and chromosome mapping of the human STAT4 gene: both STAT4 and STAT1 genes are mapped to 2q32.2–>q32.3. Cytogenet Cell Genet 77:207–210
Kisseleva T, Bhattacharya S, Braunstein J, Schindler CW (2002) Signaling through the JAK/STAT pathway, recent advances and future challenges. Gene 285:1–24
Levy DE, Darnell JE Jr (2002) Nat Rev Mol Cell Biol 3:651–662
O’Shea JJ, Gadina M, Schreiber RD (2002) Cell 109(suppl.):S121–S131
Hunter CA (2005) New IL-12-family members: IL-23 and IL-27, cytokines with divergent functions. Nat Rev Immunol 5:521–531
Bengtsson AA, Sturfelt G, Truedsson L, Blomberg J, Alm G, Vallin H, Rönnblom L (2000) Activation of type I interferon system in systemic lupus erythematosus correlates with disease activity but not with antiretroviral antibodies. Lupus 9:664–671
Luan H, Li P, Cao C, Li C, Hu C, Zhang S, Zeng X, Zhang F, Zeng C, Li Y (2011) A single-nucleotide polymorphism of the STAT4 gene is associated with systemic lupus erythematosus (SLE) in female Chinese population. Rheumatol Int. doi:10.1007/s00296-010-1767-9
Suarez-Gestal M, Calaza M, Endreffy E, Pullmann R, Ordi-Ros J, Sebastiani GD, Ruzickova S, Jose Santos M, Papasteriades C, Marchini M, Skopouli FN, Suarez A, Blanco FJ, D’Alfonso S, Bijl M, Carreira P, Witte T, Migliaresi S, Gomez-Reino JJ, Gonzalez A, European Consortium of SLE DNA Collections (2009) Replication of recently identified systemic lupus erythematosus genetic associations: a case-control study. Arthritis Res Ther 11:R69
Abelson AK, Delgado-Vega AM, Kozyrev SV, Sánchez E, Velázquez-Cruz R, Eriksson N, Wojcik J, Linga Reddy MV, Lima G, D’Alfonso S, Migliaresi S, Baca V, Orozco L, Witte T, Ortego-Centeno N, AADEA Group, Abderrahim H, Pons-Estel BA, Gutiérrez C, Suárez A, González-Escribano MF, Martin J, Alarcón-Riquelme ME (2009) STAT4 associates with systemic lupus erythematosus through two independent effects that correlate with gene expression and act additively with IRF5 to increase risk. Ann Rheum Dis 68:1746–1753
Palomino-Morales RJ, Rojas-Villarraga A, González CI, Ramírez G, Anaya JM, Martín J (2008) STAT4 but not TRAF1/C5 variants influence the risk of developing rheumatoid arthritis and systemic lupus erythematosus in Colombians. Genes Immun 9:379–382
Zervou MI, Vazgiourakis VM, Yilmaz N, Kontaki E, Trouw LA, Toes RE, Bicakcigil M, Boumpas DT, Yavuz S, Goulielmos GN (2011) TRAF1/C5, eNOS, C1q, but not STAT4 and PTPN22 gene polymorphisms are associated with genetic susceptibility to systemic lupus erythematosus in Turkey. Hum Immunol 72:1210–1213
Chung SA, Taylor KE, Graham RR, Nititham J, Lee AT, Ortmann WA, Jacob CO, Alarcón-Riquelme ME, Tsao BP, Harley JB, Gaffney PM, Moser KL, SLEGEN, Petri M, Demirci FY, Kamboh MI, Manzi S, Gregersen PK, Langefeld CD, Behrens TW, Criswell LA (2011) Differential genetic associations for systemic lupus erythematosus based on anti-dsDNA autoantibody production. PLoS Genet 7:e1001323
Yin H, Borghi MO, Delgado-Vega AM, Tincani A, Meroni PL, Alarcón-Riquelme ME (2009) Association of STAT4 and BLK, but not BANK1 or IRF5, with primary antiphospholipid syndrome. Arthritis Rheum 60:2468–2471
Lee YH, Woo JH, Choi SJ, Ji JD, Song GG (2009) Association between the rs7574865 polymorphism of STAT4 and rheumatoid arthritis: a meta-analysis. Rheumatol Int 30:661–666
Glas J, Seiderer J, Nagy M, Fries C, Beigel F, Weidinger M, Pfennig S, Klein W, Epplen JT, Lohse P, Folwaczny M, Göke B, Ochsenkühn T, Diegelmann J, Müller-Myhsok B, Roeske D, Brand S (2010) Evidence for STAT4 as a common autoimmune gene: Rs7574865 is associated with colonic Crohn’s disease and early disease onset. PLoS One 5:e10373
Pykäläinen M, Kinos R, Valkonen S, Rydman P, Kilpeläinen M, Laitinen LA, Karjalainen J, Nieminen M, Hurme M, Kere J, Laitinen T, Lahesmaa R (2005) Association analysis of common variants of STAT6, GATA3, and STAT4 to asthma and high serum IgE phenotypes. J Allergy Clin Immunol 115:80–87
Rueda B, Broen J, Simeon C, Hesselstrand R, Diaz B, Suárez H, Ortego-Centeno N, Riemekasten G, Fonollosa V, Vonk MC, van den Hoogen FH, Sanchez-Román J, Aguirre-Zamorano MA, García-Portales R, Pros A, Camps MT, Gonzalez-Gay MA, Coenen MJ, Airo P, Beretta L, Scorza R, van Laar J, Gonzalez-Escribano MF, Nelson JL, Radstake TR, Martin J (2009) The STAT4 gene influences the genetic predisposition to systemic sclerosis phenotype. Hum Mol Genet 18:2071–2207
Korman BD, Alba MI, Le JM, Alevizos I, Smith JA, Nikolov NP, Kastner DL, Remmers EF, Illei GG (2008) Variant form of STAT4 is associated with primary Sjogren’s syndrome. Genes Immun 9:267–270
Acknowledgments
Supported by grant No 502-01-01124182-07474, Poznan University of Medical Sciences. The technical assistance of Ms. Monika Świerczewska is gratefully acknowledged.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Piotrowski, P., Lianeri, M., Wudarski, M. et al. Contribution of STAT4 gene single-nucleotide polymorphism to systemic lupus erythematosus in the Polish population. Mol Biol Rep 39, 8861–8866 (2012). https://doi.org/10.1007/s11033-012-1752-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-012-1752-3