Abstract
Introduction
Recent studies identified STAT4 (signal transducers and activators of transcription-4) as a susceptibility gene for systemic lupus erythematosus (SLE). STAT1 is encoded adjacently to STAT4 on 2q32.2-q32.3, upregulated in peripheral blood mononuclear cells from SLE patients, and functionally relevant to SLE. This study was conducted to test whether STAT4 is associated with SLE in a Japanese population also, to identify the risk haplotype, and to examine the potential genetic contribution of STAT1. To accomplish these aims, we carried out a comprehensive association analysis of 52 tag single nucleotide polymorphisms (SNPs) encompassing the STAT1-STAT4 region.
Methods
In the first screening, 52 tag SNPs were selected based on HapMap Phase II JPT (Japanese in Tokyo, Japan) data, and case-control association analysis was carried out on 105 Japanese female patients with SLE and 102 female controls. For associated SNPs, additional cases and controls were genotyped and association was analyzed using 308 SLE patients and 306 controls. Estimation of haplotype frequencies and an association study using the permutation test were performed with Haploview version 4.0 software. Population attributable risk percentage was estimated to compare the epidemiological significance of the risk genotype among populations.
Results
In the first screening, rs7574865, rs11889341, and rs10168266 in STAT4 were most significantly associated (P < 0.01). Significant association was not observed for STAT1. Subsequent association studies of the three SNPs using 308 SLE patients and 306 controls confirmed a strong association of the rs7574865T allele (SLE patients: 46.3%, controls: 33.5%, P = 4.9 × 10-6, odds ratio 1.71) as well as TTT haplotype (rs10168266/rs11889341/rs7574865) (P = 1.5 × 10-6). The association was stronger in subgroups of SLE with nephritis and anti-double-stranded DNA antibodies. Population attributable risk percentage was estimated to be higher in the Japanese population (40.2%) than in Americans of European descent (19.5%).
Conclusions
The same STAT4 risk allele is associated with SLE in Caucasian and Japanese populations. Evidence for a role of STAT1 in genetic susceptibility to SLE was not detected. The contribution of STAT4 for the genetic background of SLE may be greater in the Japanese population than in Americans of European descent.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is a complex disease characterized by autoantibody production and involvement of multiple organs, including kidneys. Both genetic and environmental factors contribute to the development of SLE [1]. Until now, several genes have been reported to be associated with SLE, of which interferon regulatory factor-5 (IRF5) has been identified as a susceptibility gene common to multiple populations [2–6]. Recently, association of STAT4 (signal transducers and activators of transcription-4) haplotype tagged by rs7574865T with SLE was demonstrated in Caucasians [7]. Subsequently, two genome-wide association studies [8, 9], a study focused on the STAT4 region in Caucasians [10], and replication studies in Colombians [11] and a Japanese population [12] have confirmed the association. In addition, an association of STAT4 with SLE phenotypes such as anti-double-stranded DNA (anti-dsDNA) autoantibodies, renal disorder, and age at diagnosis was reported [10, 13]. An association of rs7574865 with other autoimmune diseases such as rheumatoid arthritis and primary Sjögren syndrome has also been demonstrated [7, 11, 12, 14]. The STAT4 gene encodes a transcription factor belonging to the STAT family expressed in lymphocytes, macrophages, and dendritic cells. STAT4 is essential for interleukin (IL)-12 signaling and induces interferon-gamma (IFNγ) production and Th1 differentiation [15]. STAT4 is also activated by type I IFNs (IFNα/β) [16]. Moreover, the requirement of STAT4 in IL-23-induced IL-17 production has been suggested [17]. Two isoforms of STAT4, STAT4α and STAT4β, are known [18]. Expression of STAT4β, lacking the transactivation domain, did not appear to be affected by the STAT4 single nucleotide polymorphisms (SNPs) [13]. STAT1, another member of the STAT family, is activated by type I IFNs and IFNγ and plays an important role in immune responses [19]. STAT1 has been reported to be upregulated in peripheral blood mononuclear cells from SLE patients and in kidneys of lupus mice with nephritis [20, 21], suggesting that STAT1 may play a role in the pathogenesis of SLE. A possible role of SNPs in the STAT1-STAT4 region other than the haplotype tagged by rs7574865T has recently been excluded in Caucasians [10]. However, in view of substantial differences in disease-associated alleles among populations [2], such analysis should be performed in each population. In this study, we carried out a comprehensive association analysis of the STAT1-STAT4 region with SLE in a Japanese population by scanning 52 tag SNPs of the region encompassing STAT1 and STAT4.
Materials and methods
Patients and healthy controls
Patients and controls were recruited at Juntendo University, the University of Tsukuba, and the University of Tokyo. All patients and healthy controls were unrelated Japanese persons living in the central part of Japan. Three hundred eight SLE patients (18 males and 290 females, average age 41.4 ± 13.5 years) and 306 healthy individuals (119 males and 187 females, average age 32.6 ± 9.8 years) were studied. Diagnosis of SLE and classification of the patients into clinical subsets were carried out according to the American College of Rheumatology criteria for SLE [22]. There was no overlap in cases or controls between this study and the recently reported study in a Japanese population [12]. These studies were reviewed and approved by the research ethics committees of the University of Tsukuba, the University of Tokyo, and Juntendo University. Informed consent was obtained from all study participants.
Association study
Fifty-two tag SNPs in the STAT1-STAT4 region were selected with an r2 threshold of 0.9 based on the HapMap Phase II JPT (Japanese in Tokyo, Japan) data. These tag SNPs captured 127 SNPs with a minor allele frequency of greater than or equal to 0.05. First screening was performed in 105 Japanese female SLE patients and 102 female healthy controls using the GoldenGate SNP genotyping assay (Illumina, Inc., San Diego, CA, USA). For the three SNPs that exhibited significant association (P < 0.01), additional samples were genotyped using the TaqMan SNP Genotyping Assay (Applied Biosystems, Foster City, CA, USA), and association was examined in 308 SLE patients and 306 healthy individuals.
Statistical analysis
Association of each SNP was analyzed by chi-square test. Because of the replicative nature of this study, correction for multiple testing was not performed, and unadjusted P values are shown. Haplotype frequency estimation and association analysis using the permutation test were performed with Haploview version 4.0 software (Broad Institute of MIT and Harvard, Cambridge, MA, USA). In the haplotype analysis, the genotype data for rs10168266, rs11889341, and rs7574865 were used and these SNPs were assumed to compose a single haplotype block. In the permutation test, only frequencies of haplotypes in this block were compared (that is, the 'Haplotypes in Blocks Only' option was used). Ten million permutations were performed. To test the significance of each SNP conditional on the genotypes of other SNPs, logistic regression analysis was performed under the additive model for the minor allele. Assuming a polymorphic site with two alleles A and a, genotypes were encoded as 0 = aa, 1 = Aa, and 2 = AA. Population attributable risk percentage (PAR%) for the risk genotype (rs7574865T/T and T/G) was estimated by the formula
PAR% = Pe (RR - 1)/(Pe [RR - 1] + 1),
where Pe represents the risk genotype frequency in the population and RR represents relative risk of the risk genotype [23]. Given the low prevalence of SLE, Pe can be estimated based on the genotype frequencies in healthy controls and RR can be approximated by odds ratio (OR) for the risk genotypes.
Results and Discussion
The STAT4 gene is located on 2q32.2-q32.3 adjacently to STAT1 gene, and the region encompassing STAT1 and STAT4 spans approximately 180 kilobase pairs. In the first screening, 52 tag SNPs in the STAT1-STAT4 region, selected with an r2 threshold of 0.9 based on the HapMap Phase II JPT data, were genotyped in 105 Japanese female SLE patients and 102 female healthy controls, and allele frequencies were compared between SLE patients and controls. A linkage disequilibrium (LD) plot and the results of the association study in the STAT1-STAT4 region are shown in Figure 1. Pairwise r2 values between 52 tag SNPs were calculated using genotyping data from 102 healthy individuals.
Linkage disequilibrium plot of the STAT1-STAT4 region in a Japanese population and first screening of 52 tag single nucleotide polymorphisms (SNPs). In the upper panel, P values for differences in allele frequencies were calculated by chi-square test using two-by-two contingency tables. The -log P value for each SNP is shown. In the lower panel, r2 values calculated using Haploview version 4.0 software based on data from 102 healthy individuals are shown. The location and direction of transcription of STAT1 and STAT4 are indicated by arrows. SNPs rs10168266, rs11889341, and rs7574865 belong to the same haplotype block.
Among the tag SNPs, rs10168266C>T, rs11889341C>T, and rs7574865G>T were most significantly associated with SLE in the first screening (P < 0.01). Allele frequencies of rs10168266T, rs11889341T, and rs7574865T were significantly increased in SLE compared with healthy controls (Table 1 and Figure 1). These SNPs were located in the introns of STAT4 and in LD with each other. In contrast, significant association was not detected for SNPs in the STAT1 region (P > 0.05).
To confirm the association detected in the first screening, additional patients and controls were genotyped for the three SNPs using the TaqMan SNP Genotyping Assay, and association was examined in 308 SLE patients and 306 healthy controls in total (Table 2). Significant deviation from Hardy-Weinberg equilibrium was not detected in healthy controls (P > 0.05). The rs7574865T allele, previously shown to be associated with SLE in Caucasians, was significantly increased in SLE patients (46.3%) compared with controls (33.5%, P = 4.9 × 10-6, OR 1.71). The association was compatible with the dominant model, under which the OR was 2.19 (T/T + G/T versus G/G).
The SNPs rs11889341 and rs10168266 were in LD with rs7574865 (r2: 0.57 to 0.78, D': 0.91 to 0.97) and were also significantly associated with SLE (allele frequency: P = 6.6 × 10-6 and P = 6.3 × 10-6, respectively). Haplotype analysis revealed that the haplotype carrying rs10168266T, rs11889341T, and rs7574865T was significantly increased (SLE: 36.8%, control: 24.3%, P = 1.5 × 10-6) whereas the haplotype carrying 10168266C, rs11889341C, and rs7574865G was significantly decreased in SLE (SLE: 52.7%, control: 65.0%, P = 1.0 × 10-5). Logistic regression analysis demonstrated that the association of each SNP lost statistical significance when adjusted for genotype of the other SNPs (Table 3). Thus, due to the strong LD, it was impossible to identify a single causative SNP among the three.
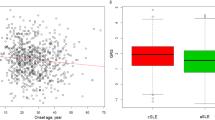
We next tested whether STAT4 rs7574865 was associated with phenotypes of SLE such as presence of nephritis, anti-dsDNA antibodies, and early age of onset (less than 20 years) as STAT4 genotype has been shown to be more strongly associated with subgroups of SLE with these phenotypes [10] (Table 4). Association of rs7574865 was observed both in SLE patients with nephritis (P = 1.0 × 10-5, OR = 1.85) and in those without nephritis (P = 0.0031, OR = 1.55). The association was stronger in SLE patients with nephritis, although the difference between SLE with and without nephritis (case-only analysis) did not reach statistical significance. Similarly, rs7574865T was significantly increased in SLE patients with anti-dsDNA antibodies compared with healthy controls, whereas association was not detected in SLE patients without anti-dsDNA antibodies. The frequency of rs7574865T was slightly higher in the patients with an age of onset of less than 20 years as compared with greater than or equal to 20 years, although the difference was not statistically significant. These tendencies are consistent with those reported in Caucasians [10]. These interpretations were not affected when the significance level was corrected for the number of comparisons (three phenotypes).
To evaluate the epidemiological significance of STAT4 polymorphism in the genetic background of SLE in the Japanese population, we estimated the PAR% in Japanese persons and Caucasians using our present data and previously reported data [8, 11, 12] (Table 5). Because the frequency and OR of the risk genotype of rs7574865 were greater in the Japanese population than those of North Americans of European descent [8], PAR% in the Japanese population (40.2%) was much higher than that of the latter (19.5%). A similarly high PAR% was observed in two of the three Japanese case-control series reported by Kobayashi and colleagues [12] and in Colombians [11]. Because PAR% may be affected by the difference in the method of ascertainment of each study, this comparison may not be completely valid. Nevertheless, these observations suggested that the contribution of STAT4 for SLE is greater in the Japanese population as compared with the Americans of European descent.
At this point, molecular mechanisms that account for the association of STAT4 intron SNPs with SLE remain unclear. Studies with lupus model mice lacking Stat4 showed conflicting results. Stat4 deficiency reduced nephritis and autoantibody production in B6.NZM.Sle1.Sle2.Sle3 mice [24]. In contrast, Stat4-deficient NZM (New Zealand mixed) mice developed accelerated nephritis and increased mortality in the absence of high levels of autoantibodies [25]. STAT4 has been shown to be involved in the induction of IFNγ, differentiation of Th1 and Th17 cells, and signal transduction from type I IFN receptors [15]. Th1 cytokines, especially IFNγ, have been shown to play a role in the pathogenesis of lupus nephritis [26]. Recently, T cells from SLE patients were shown to produce excessive amounts of IFNγ upon stimulation [27]. These observations may implicate the role of STAT4 SNPs in IFNγ production.
The role of type I IFNs in SLE has been established [1]. Elevated serum type I IFN levels and expression of IFN-inducible genes in peripheral mononuclear cells were reported in SLE [28, 29]. The association of IRF5, which induces type I IFNs, with SLE has been established [2–6]. STAT4 is activated by type I IFN as well as IL-12 signals and produces IFNγ [15]. Thus, STAT4 may also contribute to SLE as a component of the type I IFN signal pathway. Furthermore, STAT4 has been reported to transduce IL-12 signals to induce IFNγ production in B cells [30].
It is interesting to note that significant association of STAT4 was not observed in SLE patients without anti-dsDNA antibodies (Table 4). It would have been interesting to examine the effect of the genotype on the levels, rather than presence or absence, of anti-dsDNA antibody However, because the antibody levels fluctuate in association with disease activity and treatment, association with the genotype should be examined using the lifetime highest anti-dsDNA antibody level of each patient. Such data were not available for this study, and we hope that we can address this issue in the future.
Most of these observations imply that STAT4 risk genotype may be associated with an elevated expression level and/or function of STAT4 protein. A recent study reported that the STAT4 risk allele was associated with overexpression of STAT4 in osteoblasts but not in B cells [13]. To address the significance of such findings, it will be necessary to examine the effect of this genotype on the expression levels and splicing isoforms in T and B cells.
Conclusion
Through comprehensive association analysis of the STAT1-STAT4 region with SLE in the Japanese population, we demonstrated that the same STAT4 risk allele in Caucasians was strongly associated with susceptibility to SLE in the Japanese population. In contrast, evidence for an association of STAT1 SNPs was not observed. The contribution of STAT4 SNPs to the genetic background of SLE may be greater in the Japanese population than in Americans of European descent.
Abbreviations
- anti-dsDNA:
-
anti-double-stranded DNA
- CI:
-
confidence interval
- IFN:
-
interferon
- IL:
-
interleukin
- IRF5:
-
interferon regulatory factor-5
- JPT:
-
Japanese in Tokyo, Japan
- LD:
-
linkage disequilibrium
- OR:
-
odds ratio
- PAR%:
-
population attributable risk percentage
- RR:
-
relative risk
- SLE:
-
systemic lupus erythematosus
- SNP:
-
single nucleotide polymorphism
- STAT:
-
signal transducers and activators of transcription.
References
Kyogoku C, Tsuchiya N: A compass that points to lupus: genetic studies on type I interferon pathway. Genes Immun. 2007, 8: 445-455. 10.1038/sj.gene.6364409.
Kawasaki A, Kyogoku C, Ohashi J, Miyashita R, Hikami K, Kusaoi M, Tokunaga K, Takasaki Y, Hashimoto H, Behrens TW, Tsuchiya N: Association of IRF5 polymorphisms with systemic lupus erythematosus in a Japanese population: support for a crucial role of intron 1 polymorphisms. Arthritis Rheum. 2008, 58: 826-834. 10.1002/art.23216.
Sigurdsson S, Nordmark G, Göring HH, Lindroos K, Wiman AC, Sturfelt G, Jönsen A, Rantapää-Dahlqvist S, Möller B, Kere J, Koskenmies S, Widén E, Eloranta ML, Julkunen H, Kristjansdottir H, Steinsson K, Alm G, Rönnblom L, Syvänen AC: Polymorphisms in the tyrosine kinase 2 and interferon regulatory factor 5 genes are associated with systemic lupus erythematosus. Am J Hum Genet. 2005, 76: 528-537. 10.1086/428480.
Graham RR, Kyogoku C, Sigurdsson S, Vlasova IA, Davies LR, Baechler EC, Plenge RM, Koeuth T, Ortmann WA, Hom G, Bauer JW, Gillett C, Burtt N, Cunninghame Graham DS, Onofrio R, Petri M, Gunnarsson I, Svenungsson E, Rönnblom L, Nordmark G, Gregersen PK, Moser K, Gaffney PM, Criswell LA, Vyse TJ, Syvänen AC, Bohjanen PR, Daly MJ, Behrens TW, Altshuler D: Three functional variants of IFN regulatory factor 5 (IRF5) define risk and protective haplotypes for human lupus. Proc Natl Acad Sci USA. 2007, 104: 6758-6763. 10.1073/pnas.0701266104.
Ferreiro-Neira I, Calaza M, Alonso-Perez E, Marchini M, Scorza R, Sebastiani GD, Blanco FJ, Rego I, Pullmann R, Pullmann R, Kallenberg CG, Bijl M, Skopouli FN, Mavromati M, Migliaresi S, Barizzone N, Ruzickova S, Dostal C, Schmidt RE, Witte T, Papasteriades C, Kappou-Rigatou I, Endreffy E, Kovacs A, Ordi-Ros J, Balada E, Carreira P, Gomez-Reino JJ, Gonzalez A: Opposed independent effects and epistasis in the complex association of IRF5 to SLE. Genes Immun. 2007, 8: 429-438. 10.1038/sj.gene.6364407.
Kelly JA, Kelley JM, Kaufman KM, Kilpatrick J, Bruner GR, Merrill JT, James JA, Frank SG, Reams E, Brown EE, Gibson AW, Marion MC, Langefeld CD, Li QZ, Karp DR, Wakeland EK, Petri M, Ramsey-Goldman R, Reveille JD, Vilá LM, Alarcón GS, Kimberly RP, Harley JB, Edberg JC: Interferon regulatory factor-5 is genetically associated with systemic lupus erythematosus in African Americans. Genes Immun. 2008, 9: 187-194. 10.1038/gene.2008.4.
Remmers EF, Plenge RM, Lee AT, Graham RR, Hom G, Behrens TW, de Bakker PI, Le JM, Lee HS, Batliwalla F, Li W, Masters SL, Booty MG, Carulli JP, Padyukov L, Alfredsson L, Klareskog L, Chen WV, Amos CI, Criswell LA, Seldin MF, Kastner DL, Gregersen PK: STAT4 and the risk of rheumatoid arthritis and systemic lupus erythematosus. N Engl J Med. 2007, 357: 977-986. 10.1056/NEJMoa073003.
Hom G, Graham RR, Modrek B, Taylor KE, Ortmann W, Garnier S, Lee AT, Chung SA, Ferreira RC, Pant PV, Ballinger DG, Kosoy R, Demirci FY, Kamboh MI, Kao AH, Tian C, Gunnarsson I, Bengtsson AA, Rantapää-Dahlqvist S, Petri M, Manzi S, Seldin MF, Rönnblom L, Syvänen AC, Criswell LA, Gregersen PK, Behrens TW: Association of systemic lupus erythematosus with C8orf13-BLK and ITGAM-ITGAX. N Engl J Med. 2008, 358: 900-909. 10.1056/NEJMoa0707865.
International Consortium for Systemic Lupus Erythematosus Genetics (SLEGEN), Harley JB, Alarcón-Riquelme ME, Criswell LA, Jacob CO, Kimberly RP, Moser KL, Tsao BP, Vyse TJ, Langefeld CD: Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat Genet. 2008, 40: 204-210. 10.1038/ng.81.
Taylor KE, Remmers EF, Lee AT, Ortmann WA, Plenge RM, Tian C, Chung SA, Nititham J, Hom G, Kao AH, Demirci FY, Kamboh MI, Petri M, Manzi S, Kastner DL, Seldin MF, Gregersen PK, Behrens TW, Criswell LA: Specificity of the STAT4 genetic association for severe disease manifestations of systemic lupus erythematosus. PLoS Genet. 2008, 4: e1000084-10.1371/journal.pgen.1000084.
Palomino-Morales RJ, Rojas-Villarraga A, González CI, Ramírez G, Anaya JM, Martín J: STAT4 but not TRAF1/C5 variants influence the risk of developing rheumatoid arthritis and systemic lupus erythematosus in Colombians. Genes Immun. 2008, 9: 379-382. 10.1038/gene.2008.30.
Kobayashi S, Ikari K, Kaneko H, Kochi Y, Yamamoto K, Shimane K, Nakamura Y, Toyama Y, Mochizuki T, Tsukahara S, Kawaguchi Y, Terai C, Hara M, Tomatsu T, Yamanaka H, Horiuchi T, Tao K, Yasutomo K, Hamada D, Yasui N, Inoue H, Itakura M, Okamoto H, Kamatani N, Momohara S: Association of STAT4 with susceptibility to rheumatoid arthritis and systemic lupus erythematosus in the Japanese population. Arthritis Rheum. 2008, 58: 1940-1946. 10.1002/art.23494.
Sigurdsson S, Nordmark G, Garnier S, Grundberg E, Kwan T, Nilsson O, Eloranta M-L, Gunnarsson I, Svenungsson E, Sturfelt G, Bengtsson AA, Jönsen A, Truedsson L, Rantapää-Dahlqvist S, Eriksson C, Alm G, Göring HHH, Pastinen T, Syvänen A-C, Rönnblom L: A common STAT4 risk haplotype for systemic lupus erythematosus is over-expressed, correlates with anti-dsDNA production and shows additive effects with two IRF5 risk alleles. Hum Mol Genet. 2008, 17: 2868-2876. 10.1093/hmg/ddn184.
Korman BD, Alba MI, Le JM, Alevizos I, Smith JA, Nikolov NP, Kastner DL, Remmers EF, Illei GG: Variant form of STAT4 is associated with primary Sjögren's syndrome. Genes Immun. 2008, 9: 267-270. 10.1038/gene.2008.1.
Watford WT, Hissong BD, Bream JH, Kanno Y, Muul L, O'Shea JJ: Signaling by IL-12 and IL-23 and the immunoregulatory roles of STAT4. Immunol Rev. 2004, 202: 139-156. 10.1111/j.0105-2896.2004.00211.x.
Nguyen KB, Watford WT, Salomon R, Hofmann SR, Pien GC, Morinobu A, Gadina M, O'Shea JJ, Biron CA: Critical role for STAT4 activation by type 1 interferons in the interferon-gamma response to viral infection. Science. 2002, 297: 2063-2066. 10.1126/science.1074900.
Mathur AN, Chang HC, Zisoulis DG, Stritesky GL, Yu Q, O'Malley JT, Kapur R, Levy DE, Kansas GS, Kaplan MH: Stat3 and Stat4 direct development of IL-17-secreting Th cells. J Immunol. 2007, 178: 4901-4907.
Hoey T, Zhang S, Schmidt N, Yu Q, Ramchandani S, Xu X, Naeger LK, Sun YL, Kaplan MH: Distinct requirements for the naturally occurring splice forms Stat4α and Stat4β in IL-12 responses. EMBO J. 2003, 22: 4237-4248. 10.1093/emboj/cdg393.
Takeda K, Akira S: STAT family of transcription factors in cytokine-mediated biological responses. Cytokine Growth Factor Rev. 2000, 11: 199-207. 10.1016/S1359-6101(00)00005-8.
Baechler EC, Gregersen PK, Behrens TW: The emerging role of interferon in human systemic lupus erythematosus. Curr Opin Immunol. 2004, 16: 801-807. 10.1016/j.coi.2004.09.014.
Dong J, Wang QX, Zhou CY, Ma XF, Zhang YC: Activation of the STAT1 signalling pathway in lupus nephritis in MRL/lpr mice. Lupus. 2007, 16: 101-109. 10.1177/0961203306075383.
Hochberg MC: Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997, 40: 1725-10.1002/art.1780400928.
Schildkraut JM: Examining complex genetic interactions. Approach to Gene Mapping in Complex Human Diseases. Edited by: Haines JL, Pericak-Vance MA. 1998, New York, NY: Wiley-Liss, 379-410.
Xu Z, Duan B, Croker BP, Morel L: STAT4 deficiency reduces autoantibody production and glomerulonephritis in a mouse model of lupus. Clin Immunol. 2006, 120: 189-198. 10.1016/j.clim.2006.03.009.
Jacob CO, Zang S, Li L, Ciobanu V, Quismorio F, Mizutani A, Satoh M, Koss M: Pivotal role of Stat4 and Stat6 in the pathogenesis of the lupus-like disease in the New Zealand mixed 2328 mice. J Immunol. 2003, 171: 1564-1571.
Akahoshi M, Nakashima H, Tanaka Y, Kohsaka T, Nagano S, Ohgami E, Arinobu Y, Yamaoka K, Niiro H, Shinozaki M, Hirakata H, Horiuchi T, Otsuka T, Niho Y: Th1/Th2 balance of peripheral T helper cells in systemic lupus erythematosus. Arthritis Rheum. 1999, 42: 1644-1648. 10.1002/1529-0131(199908)42:8<1644::AID-ANR12>3.0.CO;2-L.
Harigai M, Kawamoto M, Hara M, Kubota T, Kamatani N, Miyasaka N: Excessive production of IFN-γ in patients with systemic lupus erythematosus and its contribution to induction of B lymphocyte stimulator/B cell-activating factor/TNF ligand superfamily-13B. J Immunol. 2008, 181: 2211-2219.
Crow MK: Interferon-α: a new target for therapy in systemic lupus erythematosus?. Arthritis Rheum. 2003, 48: 2396-2401. 10.1002/art.11226.
Baechler EC, Batliwalla FM, Karypis G, Gaffney PM, Ortmann WA, Espe KJ, Shark KB, Grande WJ, Hughes KM, Kapur V, Gregersen PK, Behrens TW: Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc Natl Acad Sci USA. 2003, 100: 2610-2615. 10.1073/pnas.0337679100.
Durali D, de Goër de Herve M-G, Giron-Michel J, Azzarone B, Delfraissy J-F, Taoufik Y: In human B cells, IL-12 triggers a cascade of molecular events similar to Th1 commitment. Blood. 2003, 102: 4084-4089. 10.1182/blood-2003-02-0518.
Acknowledgements
This work was supported by KAKENHI (Grant-in-Aid for Scientific Research) (B) from the Japan Society for the Promotion of Science; KAKENHI on the Priority Area 'Applied Genomics' from the Ministry of Education, Culture, Sports, Science and Technology of Japan; and grants from the Ministry of Health, Labour and Welfare of Japan; the Japan Rheumatism Foundation; and the Naito Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
RRG, GH, and TWB are employees of and hold stocks or shares in Genentech, Inc. (South San Francisco, CA, USA). The other authors declare that they have no competing interests.
Authors' contributions
AK participated in the study design, carried out all genotyping and statistical analyses, and wrote the manuscript. II, KH, MK, and TA participated in the first screening using Illumina GoldenGate assay (with AK), including tag SNP selection, genotyping, and statistical analysis. JO carried out statistical analysis with AK and helped in the manuscript preparation. TH, DG, IM, SI, AT, YT, HH, and TS recruited Japanese patients with SLE and collected clinical information. RRG and GH provided Caucasian data. NT conceived of the study, together with TWB, and participated in its design and coordination, recruited patients and controls, and helped in the manuscript preparation. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kawasaki, A., Ito, I., Hikami, K. et al. Role of STAT4 polymorphisms in systemic lupus erythematosus in a Japanese population: a case-control association study of the STAT1-STAT4region. Arthritis Res Ther 10, R113 (2008). https://doi.org/10.1186/ar2516
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar2516