Abstract
Until the recent spread of public-private partnerships, pharmaceutical firms had avoided research and development into neglected tropical diseases (NTDs). Because these are diseases that affect the poorest populations in developing regions, research and development initiatives have for the most part depended on the resources and expertise drawn from academia, international organizations, and intermittent state interventions in disease-endemic countries. Over the last few decades, however, public-private product development partnerships (PDPs) have been introducing new collaborative agreements in which the existing resources and expertise combine with the those traditionally withheld by the pharmaceutical industry and global health NGOs. This paper explores recent transformations in the representation of NTDs by examining the shifting logic and spaces of knowledge production which the advent of PDPs has enabled. An analysis of two case studies focused on Chagas disease-related initiatives addresses recurring preoccupations in Science, Technology and Society studies as well as in critical analyses of PDPs: that is, the back-and-forth movement of the disease from being an object of scientific inquiry to a public health concern, and the legitimacy risks and material asymmetries entailed in global health PDPs. Both cases show that it is major global health stakeholders and experts in non-endemic countries, rather than transnational pharmaceutical firms, that exert the greatest influence upon these changing representations: PDPs attempt to expand the preexisting biomedical focus on NTDs by means of incorporating “real world” drug development preoccupations (which I term epistemic shifts), but they also combine their stated global humanitarian aim with security concerns about the diseases spreading to non-endemic, industrialized countries (which I term geographical shifts).
Similar content being viewed by others
Introduction
Neglected tropical diseases (NTDs) are a heterogeneous group of infectious diseases that affect more than one billion individuals living in tropical and subtropical conditions (WHO 2022a). While most of these infections have relatively low mortality rates (GBD 2015), they still account for a greater burden measured in disability-adjusted life years than several major infectious diseases such as malaria or tuberculosis (Hotez 2011). However, because populations affected by NTDs live in poverty and have limited access to healthcare, the market incentives that drive pharmaceutical research and development are lacking in this field: for example, of all new pharmaceutical products approved between 2000 and 2011, only one percent targeted pathogens that cause neglected diseases (Pedrique et al. 2013).Footnote 1 These enduring pharmaceutical and healthcare deficits that characterize the NTD research and development landscape have led scholars and advocates to describe this situation in terms of both “market” and “public health failures” (e.g. Trouiller et al. 2002; Lezaun and Montgomery 2014).
These failures, however, contrast somewhat with an intricate history of research initiatives and advocacy efforts focused on NTDs and their causing pathogens (Hotez 2017; Molyneux et al. 2021). Since the 1970s, major stakeholders in the field of international health and philanthropy, such as the World Health Organization’s (WHO) Special Programme for Research and Training in Tropical Diseases (TDR), or the Rockefeller Foundation’s Great Neglected Diseases Network, have played a key role in convening development agencies, international organizations, and academic institutions to support research and development initiatives into NTDs (Keating 2014; Ridley, Ndumbe, and Korte 2008). After periods of sporadic support and dispersed initiatives, TDR and other global health stakeholders have led concerted efforts directed at raising the profile of these diseases in global public health agendas, but have lacked sufficient industry commitment to transform the neglected disease research and development landscape drastically (Liese, Rosemberg, and Schratz 2010; Savioli, Montresor, and Gabrielli 2011).
It was only in recent years that public-private product development partnerships (PDPs) emerged in response to this “fatal imbalance” between the dynamics of pharmaceutical research and development and the health needs of those affected by NTDs (MSF 2001). Through horizontal multi-sector collaborations – that is, without corporate hierarchies or state bureaucracies, but neither purely private, market-driven interests – PDPs are expected to mobilize the critical resources and expertise traditionally withheld by the pharmaceutical industry due to the absence of commercially viable markets in this field (Buse and Walt 2000a; Lezaun and Montgomery 2014). Instead, public-private partnerships rely on “trust and rather long-term commitments in which legitimacy and other noncommercial values play an important role for the private enterprises” (Mörth 2009: 103). PDP-based initiatives under the public-private model thus bring international health agencies and firms together, but also engage in novel collaborative ventures with civil organizations, academic and research institutes, health ministries, and philanthropic NGOs seeking to “contribute to a global public concern, even if only through spillover effects” (Kaul 2006: 224).
This paper explores recent transformations in the NTD research and development landscape by examining the role of public-private PDP-based initiatives. More specifically, I focus on two ongoing case studies – the TDR Targets resource for drug target prioritization and the Chagas Clinical Research Platform launched by the NGO Drugs for Neglected Disease initiative (DNDi) – to examine epistemic and geographical shifts that take place in scientific research, intervention strategies, and discourse as pharmaceutical firms and global health stakeholders take part more actively in partnerships promoting drug discovery and clinical trials to treat these diseases. A key question is: how do PDPs redefine or reinforce preexisting representation of NTDs, and how are the logic and spaces of knowledge production altered with the work of PDPs? The analysis builds on fieldwork conducted around Chagas disease-related initiatives and focuses mainly on the role of Argentinean experts and institutions, as well as international stakeholders and (their) counterparts in research and development initiatives operating under the public-private partnership model between 2015 and 2021.
These questions about the role of PDPs are guided by more fundamental concerns in Science, Technology, and Society studies (STS), as well as by political and sociological analyses of public-private partnerships in global health. First, STS has long addressed how expert knowledge and public concerns engage in processes of mutual definition and contestation (e.g., Gusfield 1981; Jasanoff 2004; Latour 2004). Such approaches, indeed, have been used to understand Chagas disease’s evolution from object of scientific inquiry to legitimate public health concern in both endemic (Kreimer 2015; Kropf 2009; Zabala 2010) and non-endemic countries (e.g. De Maio, Llovet, and Dinardi 2013) but not to address the specific role of public-private partnerships in altering or reinforcing such processes.
Second, critical analyses of partnerships have understood their emergence as a new policy interplay that challenges the assumed roles and boundaries of civil society and state (e.g. Börzel and Risse 2005; Mörth 2009; Schuppert 2011). This interplay poses certain legitimacy risks, such as shifting policy processes toward select private stakeholders and away from governmental organizations in addition to disproportionately favoring private companies in the capitalization of outcomes and resources (Martens 2003). Even though these underlying risks and asymmetrical relations embedded in partnerships have been dealt with in the global health literature (Buse and Walt 2000a; Moran 2005; Richter 2004), the perspective of beneficiaries and the unintended outcomes of public-private partnerships in the NTD landscape has remained largely unexamined (cf. Lezaun and Montgomery 2014; Mantilla 2011; Redfield 2012). In this paper I attempt to bridge these gaps in the literature by reflecting on the recent changes these initiatives have brought into the existing representation of Chagas and other NTDs.
The paper is divided into five sections. The first section develops Chagas disease’s evolution from an infection that affects the rural poor in Latin America to a proposed paradigm of NTDs in non-endemic countries. This section also examines the dominant logic of knowledge production and the historical uptake of the disease as a public health concern prior to the emergence of public-private PDPs. The second section describes the recent rise of global health public-private partnerships in NTD research and development, and presents the two PDP-based initiatives selected as case studies: the TDR Targets project and the DNDi Chagas Clinical Research Platform. The third section analyses epistemic shifts – or, changes in the logic of knowledge production – arising from the two PDPs under analysis. The fourth section analyses the geographical shifts – or, changes in spatial representations – associated with Chagas and other NTDs. Finally, the conclusions reflect on the influence of public-private PDPs as a whole, where global health stakeholders and experts – not the transnational pharmaceutical industry – raising concerns about NTDs spreading in non-endemic countries have brought about the greatest changes in the logic and spaces of knowledge production.
Chagas Disease as “A Paradigm” of NTDs
Chagas disease (or American trypanosomiasis) is an infectious disease caused by the protozoan parasite Trypanosoma cruzi. Even though the disease is endemic to 21 countries in the Americas – where it is estimated to affect approximately 6 million individuals (PAHO n.d.) – it is also seen as “a paradigm” of emerging infectious diseases in non-endemic countries (Angheben et al. 2015). Its main form of transmission involves triatomine insects commonly known as “kissing bugs,” which introduce the parasite into human hosts after feeding on blood and disposing of feces (WHO 2022b).Footnote 2 The resulting infection develops in two consecutive stages: an initial acute phase that causes flu-like symptoms, followed by a much longer chronic phase that produces cardiovascular and gastrointestinal damage in about 30 percent of patients, and which can ultimately lead to life-long disability and death. Treatment options are currently limited to two antiparasitic drugs developed in the 1960s and 1970s by the Roche and Bayer laboratories: benznidazole and nifurtimox. These drugs, however, show limited effectiveness in treating adults during the chronic phase and have toxic side effects after long-term use.
Because of these epidemiological features and deficient pharmaceutical situation, Chagas disease has been classified as one of the “most neglected diseases” (MSF 2001; Yamey 2002). For example, it is estimated that over 90 percent of actual cases lack proper access to diagnostic or treatment (Plataforma de Investigación Clínica en Enfermedad de Chagas 2019). Moreover, kissing bugs dwell in precariously built huts and animal sheds, so the disease is often associated with the rural poor and marginalized locations. Yet, due to ongoing migratory movements – both domestic and international – a different epidemiological landscape with higher prevalence of Chagas disease in traditionally non-endemic areas has been forming over the last decades. In these previously uncontaminated zones where this “tropical” disease is now spreading, T. cruzi transmission can still occur congenitally (from mother to child) or serologically (via blood transfusion or organ transplantation) (Schmunis 2007).
This shifting epidemiological landscape has also led a number of experts and authorities in non-endemic countries to identify a public health concern in Chagas disease. This is most notably the situation of countries hosting large Latin American communities, such as the United States, Canada, Italy, and Spain, although cases have also been reported throughout Europe, or even as far as Australia, New Zealand, and Japan (e.g. Imai et al. 2019; Jackson, Pinto, and Pett 2014). Indeed, one of the first scholarly articles warning about possible public health risks associated with imported Chagas disease in Europe dates back to the 1980s (Pehrson, Wahlgren, and Bengtsson 1981), but it was not until the 2010s that European medical and public health experts reached a certain level of consensus about its epidemiological status (De Maio, Llovet, and Dinardi 2013; Eurosurveillance editorial team 2011). Reviews in the fields of cardiology (Strasen et al. 2014) and transfusion medicine (Angheben et al. 2015) determined that the disease already constituted a “new threat” in non-endemic countries due to its implications for the provision of healthcare and safety of blood transfusions.
In the United States, isolated cases of autochthonous T. cruzi infection are known to exist but are still considered epidemiologically insignificant in relation to the risk posed by imported Chagas disease (Bern et al. 2019).Footnote 3 Research articles and editorials published in specialized journals like PLOS Neglected Tropical Diseases feature titles along the lines of “An Unfolding Tragedy of Chagas Disease in North America” (Hotez et al. 2013) or “Chagas Disease: The New HIV/AIDS of the Americas” (Hotez et al. 2012). As early as the 1980s papers addressing Chagas disease in the United States were already admonishing the “lack of knowledge in industrialized nations” with “several signs warning that [these countries] would have to face the problem” (Schmunis 2007: 80; see also Kirchhoff, Gam, and Gillian 1987).
Trypansoma Cruzi: Model or Menace?
Interest in the Chagas-causing pathogen has a more complicated history than that of the disease itself. This history, however, has not always translated into positive public health outcomes against the disease. The causing pathogen and its vectors, along with its clinical manifestations, were first identified between 1908 and 1909 by Carlos Ribeiro Justiniano das Chagas, a Brazilian clinician and researcher based in Rio de Janeiro who enjoyed high academic prestige but failed in his attempts to draw the attention of Brazilian public health authorities and political circles in his discovery (Kropf 2009; Sanmartino 2009). In a letter written in 1928, he warned about the “nefarious sign” that stemmed from this new trypanosomiasis: “every study points a finger at a malnourished population living in poor conditions […] Talk about this disease and you will have governments against you” (Quoted in Jörg and Storino 2002: 10, with emphasis in the original).Footnote 4
Nevertheless, Chagas’s findings managed to spark interest among emerging scientific and medical circles in Latin America. And in the 1950s this interest eventually drew attention from political circles in a few Latin American countries as public health and sanitation offered a space for convergence between preexisting scientific interest in the disease and new political ambitions. In Argentina, for instance, each individual diagnosis of Chagas disease began to be extrapolated to entire populations living in similar sociodemographic conditions (Zabala 2010). This “epidemiological shift” soon raised estimated infection rates from the magnitude of the hundreds to around one million individuals, which in turn helped establish Chagas disease as a legitimate public health concern rather than a mere object of scientific and medical interest (Kreimer 2015). Nation-wide intervention strategies targeting housing conditions, vector control, health care access, and blood screening began to move the focus away from T. cruzi and place it on the affected populations.
However, toward the 1970s, a new research space devoted to T. cruzi would once again reshape the significance of Chagas disease as a public health concern. During this stage, novel techniques in molecular biology (and earlier fields such as biochemistry and immunology) were also justified under a rhetoric of social and political import: for example, basic research into the biochemistry of the pathogenic organism, or the mechanisms involved in host immune response, would supposedly provide the basis for “leaving the pre-scientific stage in the application of medicine behind” and, at the same time, serve “the health of the people” (quoted in Zabala 2010: 214–215). The means for translating this new wealth of knowledge about T. cruzi into applicable biomedical technologies were still uncertain but, in principle, this promising research space (including its expected outcomes) was not intended to compete against the preexisting intervention strategies focused on living conditions and access to healthcare.
This new scientific promise endowed with a social consideration helped core loci representatives in Argentina and Brazil secure local funds for basic research into T. cruzi. One crucial source of stable financial resources and decisive symbolic capital was provided by TDR, which in 1977 provided material research support for Chagas disease working groups in Latin America. Throughout the following decades, these support structures would progressively displace knowledge production in fields of “lower scientific hierarchy” (Kreimer and Zabala 2007; WHO et al. 2007; Zabala 2010) – such as cardiology or clinical practice – in favor of biology, biochemistry, and immunology. Progressively, these transformations would also shift interest in Chagas disease back to the realm of T. cruzi.
This strengthening of international scientific ties around T. cruzi research underpinned subsequent biomedical approaches to Chagas disease. However, these approaches did not necessarily translate into a heightened consideration of the disease – or even patients – as a public health concern in endemic countries. Even if TDR originally emphasized the economic and social determinants of health, its research support programs ultimately favored scientific and technological capacity-building that offered solutions – or, “promises” – in the form of potential biomedical advancements (Parker, Pollman, and Allen 2016; Reidpath, Allotey, and Pokhrel 2011; Ferpozzi 2020). Incidentally, during the same period, public health initiatives in different Latin American countries such as vector control, epidemiological surveillance, and early access to diagnostics or treatment suffered increasingly from defunding, institutional overlapping, and even a paucity of interest among decision-makers (Plataforma de Investigación Clínica en Enfermedad de Chagas 2019; Zabala 2010).Footnote 5 In any case, commercially driven research and development initiatives were virtually absent throughout this whole period.
Subsequently, during the 1990s and early 2000s, genome sequencing projects dedicated to pathogens causing NTDs drove scientific interest in T. cruzi even further. Justification provided for the Trypanosoma cruzi Genome Project (TcGP) in particular was somewhat ambiguous in this regard. While its proposal envisioned the possibility of developing new, more effective drugs against the disease by fully sequencing the parasite’s genome, its participants also suggested that T. cruzi became “a key model organism for laboratories in the region” and an “attraction” for local researchers and laboratories abroad (Ferrari et al. 1997: 843–844). As Levin et al. (2021) point out, this was “a happy story from the point of view of scientific research, but a sad story regarding the social issues” that come with the disease (14). An unintended outcome of the TcGP, however, was the launch of the TDR Targets project, a WHO/TDR-coordinated PDP-based initiative targeting T. cruzi plus several other pathogens that cause neglected and high-priority infectious diseases.
Public-Private PDPs in the Neglected Disease Landscape
PDPs in the neglected disease landscape emerged almost in parallel with the spread of public-private global health partnerships during the 1990s and 2000s. Public-private partnerships are collaborative agreements between government agencies and private companies and often also involve collaborations with non-governmental, international, or non-profit organizations (Börzel and Risse 2005). Global health public-private partnerships, in particular, include at least one company and an intergovernmental organization but normally involve bilateral or civil organizations such as research and development institutes, government agencies, and philanthropic or grassroots NGOs (Richter 2004). These engagements can either make up specific partnership agreements or provide an underlying framework that enables horizontal and voluntary collaboration among partners (Richter 2005). In this way, global health public-private partnerships encompass a variety of goals, organizational forms, or constituent membership, while PDPs are initiatives more specifically aimed at producing or delivering otherwise unavailable healthcare technologies such as drugs or vaccines (cf. Buse and Walt 2000b).
In many ways, the spread of PDPs in the neglected disease landscape reflects several perceptions that marked the passage from international to global public health in the 1990s. Those perceptions included increasing disillusionment with international agencies as well as a heightened consideration for the individuals and organizations beyond the realm of nation states (Buse and Walt 2000a; Brown, Cueto, and Fee 2006). At the same time, a shared recognition of an “emerging diseases worldview” concerned with “an infectious diseases burden of globalization” began to put infectious diseases high on the agendas of global public health politics (Füller 2014: 176). In such a worldview, the focus on infectious diseases was no longer confined to poverty, development, or tropical conditions but rather on its interactions with the “global north” (cf. Weir and Mykhaloskiy 2010; Shahvisi 2019).
In terms of their advantages and risks, PDPs have been characterized rather uniformly in the existing literature on partnerships (cf. Richter 2004) although they have received less attention in STS. In terms of their advantages, private actors that join PDPs can respond to increasing demands for corporate responsibility, enhance their public image, and contribute funds and critical expertise to relegated health issues; partnerships also allow private actors to exert greater influence on the global and international regulatory scene and, because of this, gain privileged access to unconquered markets and untapped scientific resources in developing countries (Buse and Walt 2000a; Kaul 2006; Lezaun and Montgomery 2014; Moran 2005). On the other hand, international agencies depend less on contributions from donor countries and obtain increased legitimacy by means of incorporating “civil society” into the policy-making process (cf. Börzel and Risse 2005; Mörth 2009).
The risks of PDPs, by contrast, have been identified in their dissolution of limits and responsibilities, and in the fundamental inequalities that exist among partners (Richter 2004). For instance, according to Martens (2003), the term “partnership” is eminently political and not just stylistic: it “implicitly downgrades the role of governments and intergovernmental organizations and upgrades the (political) status of private actors” such as transnational corporations (26), so the priorities of funding agents can displace policies in the receiving countries, duplicate existing efforts, or compete against government agencies for scarce local attention and resources (Mantilla 2011). In a similar sense, Buse and Walt (2000b) note that “the costs for the private sector seem to be relatively small in relation to overall gains: a potential small loss of resources if programmes do not work but huge benefits in public relations when they succeed” (706). Indeed, private partners need not give up entirely on other competitive or speculative intentions in spite of the noncommercial, humanitarian rhetoric that pervades global health PDPs (Kaul 2006; Lezaun and Montgomery 2014; Moran 2005; Nwaka and Ridley 2003).
Last and perhaps most important is the issue of legitimacy. Public-private partnerships emerged partly as a response to the democratic deficit entailed in the policy processes of international health organizations (Buse and Walt 2000a). Inclusion of non-state actors, including firms and the non-for-profit sector is expected to enhance their alleged participatory and democratic nature (Börzel and Risse 2005, p. 16). But if such inclusion is selective or lacks transparency, it may also render those policy processes less rather than more democratic (Mörth 2009). This is notably the case in the NTD landscape, where structural conditions result in patients being “largely people who, in Karl Marx’s infamous phrase (1975 [1852]) ‘must be represented’” (Redfield 2012: 180). In this scenario, patient representation depends on the role exercised by states, intergovernmental organizations, global health NGOs, and experts – even if the latter have been concerned chiefly with the disease-causing pathogens rather than health systems and access structures. In this sense, the novelty of PDPs is that they add pharmaceutical companies and philanthropic NGOs to this list of legitimate “spokespersons” (Rabeharisoa, Moreira, and Akrich 2014) entitled to problematize neglected diseases.
TDR Targets
TDR Targets is a drug target prioritization resource focused on several pathogens that cause neglected diseases and other higher-priority infections (Urán Landaburu et al. 2019). This open-access chemogenomic resource emerged between 2005 and 2006, partly as a continuation of the TcGP. Just as many other contemporary genome sequencing projects, the TcGP was heavily influenced by the Human Genome Project (HGP) but devoted exclusively to the pathogenic organism responsible for Chagas disease. The project was executed in parallel with other genome sequencing efforts centered on the trypanosomes that cause sleeping sickness and leishmania, and was completed in 2005 with the publishing of the first sequences in Science (El-Sayed et al. 2005).Footnote 6 According to its proponents, completion of the TcGP would be likely to result “in the final eradication of Chagas disease” (Trypanosoma cruzi Genome Consortium 1997: 20).
Less than a decade later, however, WHO had already deemed the TcGP outcomes insufficient: in 2005, after recognizing that genome sequences would not necessarily produce the required pharmaceutical technologies, WHO launched a call for the TDR Targets project. This new resource was not only meant to take advantage of the experience gained with the genome sequencing projects but also convene those stakeholders who – like the pharmaceutical industry – had avoided research and development efforts in the field of NTDs. Building on the wealth of expertise acquired with the TcGP, the TDR Targets project was granted to the Laboratory of Genomics and Bioinformatics at the National University of San Martin in Argentina (UNSaM) in collaboration with the Wellcome Sanger Institute in the United Kingdom, the University of Melbourne in Australia, and the Universities of Washington and Pennsylvania in the United States.
While TDR Targets was envisaged with an initial aim of engaging pharmaceutical firms and universities in joint research and development efforts, WHO eventually abandoned its coordinating role with the expectation that the project would be taken up and supported by “other” stakeholders (Rodríguez-Medina et al. 2019). Much of TDR Targets’ interactions with the pharmaceutical industry then took place under a de facto public-private partnership model in which firms were meant to contribute critical know-how as well as financial, legal, or technical resources. However, after WHO discontinued its initial financing, the project execution depended on funds from the public science system and formal cooperation agreements with foreign government ministries and pharmaceutical firms.Footnote 7 The remaining engagement of the pharmaceutical industry in TDR Targets has since occurred through somewhat ad hoc instances, and WHO’s coordinating role is still lacking. At an earlier stage of the TDR Targets project, its principal investigator had already hinted at the social and scientific configuration of NTD pharmaceutical research and development:
no one has a very clear idea of what a good drug target is…. It wasn’t easy getting everyone on the same page…. There were people from Glaxo… from Pfizer […] because WHO has lots of contacts with lots of laboratories […] [Laboratories] don’t have a very clear idea of how to go out and find those targets, but they know how the processes are likely to work in each company […] So, while we talked about many different things, they knew that translating or implementing this would be impossible […] [the criteria] was a certain one in one company; in another company something else was more important […] even if firms were interested in academia doing all the work for them to reap the fruits later… they’d realize that they’re developing a product that … they have to sell to populations that have no money (TDR Targets principal investigator at UNSaM, interview, June 24 2015).
In setting up the TDR Targets project, WHO had acknowledged the limitations that complicate drug development in the neglected diseases landscape. In particular, WHO’s shift in focus during the 2010s sought to redress the dominance of “flat world” perspectives – or promises of the “ultimate cure” – according to which the results of basic research would translate into the pharmaceutical technologies needed to treat NTDs (cf. Reidpath, Allotey, and Pokhrel 2011). But if WHO’s initial mediating role in organizing TDR Targets was clearly necessary for enabling interactions between academia and industry, it was also insufficient. As the TDR strategy abandoned intermediation and moved toward field intervention:
The WHO made something of a deep turn in its scientific program since the 1980s and 1990s […] actually, all the pathogen genome projects started there – and now they’re doing more field intervention: epidemiological studies, epidemiological surveillance.... in fact, there’s no more funding to apply for... I understand it was part of this shift in the subject areas they fund […] they don’t do much research in molecular stuff like this.... From a regulatory perspective, it might be that, as a political arm, it can be useful to make contact with them […] from an outsider’s perspective, I see it as a symptom of having other actors investing strongly in research… and TDR disengaged from this and started doing other things […] Today [WHO’s core] role is no longer there (TDR Targets principal investigator at UNSaM, interview, August 30 2019).
But it was not just TDR who revised the research fields and expert knowledge relied on during previous decades to intervene into NTDs. For DNDi in particular, advancing treatment options against neglected diseases did not necessarily involve drug discovery efforts, or even drugs per se. Instead, facing a context marked by the lack of effective medical and pharmacological treatments directly, DNDi began to reassess preexisting assumptions through the Chagas Clinical Research Platform, moving its research focus back toward benznidazole – an existing, yet not so widely used drug – as an accessible treatment option against Chagas disease (Sosa-Estani 2011; Plataforma de Investigación Clínica en Enfermedad de Chagas 2019).
The DNDi Chagas Clinical Research Platform
DNDi is an initiative born out of TDR and the international NGO Doctors without Borders (Médecins Sans Frontières, MSF).Footnote 8 It emerged in 2003 following a “new wave” of humanitarian and philanthropic enterprises focused on improving access to pharmaceutical products for the poor (Redfield 2012: 161). Under the motto "Best science for the most neglected,” the initiative aims to alter the fatal imbalance that affects pharmaceutical research and development for neglected diseases such as pediatric HIV, malaria, hepatitis C, and Chagas, plus five other infections classified in the WHO list of NTDs.Footnote 9 Rather than conducting in-house research, DNDi outsources its clinical and pharmaceutical research programs to public and private entities with scientific and technological infrastructures (Croft 2005). In this sense, DNDi operates under a paradigm of multisectoral association that mobilizes donor and partner resources or interacts directly with their representatives. The scope of DNDi activities, however, is not restricted to coordinating research and development for accessible medicines but also involves cross-sector advocacy, communication campaigns, intellectual property leverage, and public health strategies, with the ultimate goal of circumventing the free market situation that surrounds pharmaceutical access for neglected diseases. From DNDi’s perspective, this means treating drugs as public goods (Redfield 2012: 164; cf. Kaul 2006).
The DNDi Latin American office, based in Rio de Janeiro, opened in 2004 with the aim of supporting regional research and development activities for Chagas disease, leishmaniasis, and malaria. Since 2009, it has coordinated the Chagas Clinical Research Platform, which operates with approximately 150 institutions in 23 donor and partner countries. This partnership presents itself as a “flexible network” that contributes to research and development into the disease by means of promoting expert meetings and training, protocol standardization and regulation, and integration of ethical principles (Plataforma de Investigación Clínica en Enfermedad de Chagas 2019). As a forum for technical discussion and information exchange, the Platform aims to “generate a critical mass of specialized knowledge and strengthen local research capacities” required to face the present challenges posed by Chagas disease (DNDi Latin America 2021). Partners are represented by public hospitals, biopharmaceutical firms, and NGOs (including DNDi), as well as diverse organizations in the public science and technology sector in endemic and non-endemic countries; donors, on the other hand, include foreign development assistance offices, as well as a number of international and non-profit stakeholders such as TDR and MSF.
In 2015, Chagas disease research represented the vast majority of DNDi Latin America’s (2015) expenditures. Yet the Chagas Clinical Research Platform has directed its efforts beyond drug discovery – and also beyond T. cruzi – itself. Instead, the platform has focused on different phases of clinical research, diagnostics, and criteria for assessing cure rates. Such efforts relied mostly on the two existing antiparasitic drugs and helped determine benznidazole’s dosing regimens and efficacy during the disease’s chronic phase. Much of this move away from flat world perspectives was a result of MSF’s early focus on “access”: understanding that research and development alone did not guarantee access to medicines, the Platform prioritized funding proposals only “if they respond to a specific medical need, and if they facilitate or enable sustainable access to the resulting innovation” (Childs 2011: 9).
For DNDi, then, access to treatment and diagnostics constitute goals equivalent to those of drug development. However, according to a former platform coordinator, this was not a particularly widespread notion in disease-endemic countries until the last decade:
an interesting movement began to take place in which many actors become involved… especially at the global level… not so much in endemic countries, who were stuck in a series of preconceived notions and theories that made any advancements in research impossible […] an awareness about the problem of Chagas being not just a biomedical problem […] many times, the human component is missing […] it is yet to be seen whether this is sustainable… how to keep that interest in the social area… what DNDi always attempts to do is to keep the patient at the center… because otherwise research can be oriented toward results or other objectives that are not mainly [the patients’] needs… (former Chagas Clinical Research Platform coordinator, interview, 26 May 2016).
Again, somewhat paradoxically, the Platform’s objective of “eliminating Chagas disease as a public health concern” (Plataforma de Investigación Clínica en Enfermedad de Chagas 2019, p. 2) has drawn heavily on the experience of non-endemic countries. As one of its partners highlighted during a scientific session held in Madrid by DNDi and the Spanish Royal Academy of Medicine:
when we thought about patients and thought we had to diagnose, we realized that the medicines weren’t there, that it was impossible to promote diagnostics when we couldn’t offer treatment for patients, so our first concern was that the medicines became available. […] Even in the United States, in collaboration with DNDi […] we got approval from the FDA [Food and Drug Administration]… where they told us that Chagas disease was a public health problem…. I don’t think that there is any other neglected disease that is also a public health problem in the United States. We also made a commitment with DNDi… since we were going to obtain an economic benefit from this approval, then [we would] assign it to better access for patients.… But what did we find? When the medicines were there, the number of treated patients did not increase…. Medicines are indispensable but not sufficient. So we have been working a lot in the area of communication, which is not the area we know the most about. We do know about scientific matters, biological matters, medical matters… (Silvia Gold, Leader of Mundo Sano Foundation and member of DNDi’s Board of Directors, extraordinary session at the Spanish Royal Academy of Medicine, June 30 2021).
This emphasis on “patients’ needs” clearly exceeds that of otherwise “flat” biomedical perspectives. Yet, these broader and seemingly favorable epistemic shifst in research and development efforts might also be informed by new concerns for the well-being and safety of individuals other than patients – that is, the citizens of non-endemic geographies threatened by the potential spread of NTDs.
Epistemic Shifts
The history of Chagas disease research is, as most NTDs, marked by a shifting back-and-forth focus between its causing pathogen and the human hosts it infects. The initial clinical and parasitological focus was aimed at the affected populations – namely the rural poor – as medical and political elites in Latin America framed the disease as a public health concern. During the 1970s, new laboratory-based approaches rolled the research and development focus back to its causing pathogen. These approaches were ultimately meant to contribute to the resolution of a public health concern in endemic countries; however, over the following decades, they favored international research programs that almost exclusively translated into renewed flows of scientific funding and prestige, but not necessarily into the promised pharmaceutical solutions (Ferpozzi 2020).
PDPs surfaced in the NTD landscape with a dual approach to these shifts in research and development. Throughout the 2000s and 2010s, select global health stakeholders began to promote public-private partnerships with a rhetoric that stressed the needs of the populations affected by NTDs (Lezaun and Montgomery 2014; MSF 2001). Such rhetoric found those needs unmet as a consequence of both market and public health failures. Market failures could clearly be ascribed to the absence of commercial incentives that drove the pharmaceutical industry interest away from research and development into NTDs. Public health failures, on the other hand, could be ascribed not just to the lack of capacity or interest shown in public and international health but also to the limitations that stemmed from biomedically centered and laboratory-based approaches in NTD research and development.
Both TDR Targets and DNDi’s Chagas Clinical Research Platform emerged at least partly in response to such limitations. TDR Targets was conceived as a space for convergence between institutions experienced in NTD-related genomic resources and central players in the transnational pharmaceutical sector. Its collaborative dynamics did not move knowledge production too drastically away from the established research fields, but did require revising preexisting assumptions – or, “promises” – made over decades of basic biomedical research focused on the pathogenic organisms causing NTDs. However, it was the same strategic move toward field intervention that caused WHO’s strategy to veer away from capacity building and support for basic research in endemic countries, leaving TDR Targets without sustained financial support and a centralized coordination role.
The Chagas Clinical Research Platform, on the other hand, managed to integrate a wider range of epidemiological and clinical concerns into its scope of action. Such an integrated approach to Chagas disease aligned with MSF and DNDi’s focus on access and patients – rather than on biomedical research and drug development per se – which generated a renewed interest in the already existing drug benznidazole as well as more accurate knowledge about possible dosing regimens and criteria for diagnosing and assessing cure rates.
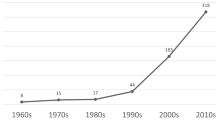
This approach, however, may also be a contingent result of the influence of public health experts, researchers, and advocates becoming increasingly concerned with the public health dimension of the disease in non-endemic countries. Levin et al.’s (2021) recent examination of “bibliographic clusters” in Chagas disease-related publications, for instance, has identified a dominant cluster representing research subfields concerned with clinical and drug studies during the chronic phase. While this is followed by another cluster concerned with in vitro studies of T. cruzi and immune response with an almost identical publication share, the volume of the former has shown a steady growth since the mid-2000s, whereas the latter has stagnated during the last decade.Footnote 10 These changes have been interpreted partly as a result of recent migratory processes which “drove research on diagnosis and promoted the publication of studies on chronic treatment of Chagas in other countries like Spain or Switzerland” (6).Footnote 11
While in scientific terms this epistemic shift still lacks sufficient knowledge production in the social sciences and humanities (cf. Levin, Kreimer and Jensen 2021) – including public health and epidemiology – it arguably stands closer to the “real social issues” that had been absent from NTD research and development agendas. Real social issues – as defined by Reidpath et al. (2011) in opposition to a “flat world science” – acknowledge at least some of “the many marginalizing factors in the social, cultural, economic, political and physical environments in which affected populations live” (Mantilla 2011: 121). Drug resistance, compliance, lack of access, and structures of existing health systems thus became more central preoccupations among public and global health experts and research networks that are no longer confined to pharmaceutical development exclusively, even if they are still heavily reliant on clinical and biomedical forms of expertise.
In terms of their social and political configuration, TDR Targets and the DNDi Chagas Clinical Research Platform have received a more or less direct influence from experts and authorities in non-endemic countries attempting to raise the disease status to that of a public health concern. This influence resulted in an increased awareness about the insufficiency of the dominant laboratory-driven research focused on the biology of disease-causing pathogens, but it still requires intermediation from “partners” such as global health stakeholders and international research centers in order to materialize. This dependence, however, can also have paradoxical effects on the environments where individuals and collectives affected by NTDs live.
Global health PDPs and their focus on “patients,” may not necessarily have emerged from security concerns, but, as I shall discuss in the following section, they alter how the “tropical” nature of neglected diseases and their interaction with “non-endemic” geographies is being represented.
Geographical Shifts
The history of Chagas disease is also marked by a back-and-forth movement between the spaces of knowledge production and the sites where it emerges as a public health concern. Like most NTDs, the disease is conceived of as an affliction of the rural, marginalized poor, which means that knowledge production and intervention strategies have depended on representation and resources mobilized from metropolitan sites (Kreimer 2019). However, this initial “diffusionist” movement (cf. Basalla 1967) changed in recent decades as the disease became a matter of concern for new sets of global and public health stakeholders, including experts in industrialized countries where non-endemic T. cruzi infection is known to exist.
The implications of these shifts have been partly analyzed by De Maio et al. (2013) along the “statist” versus “globalist” divide in international health policy (cf. Davies 2010; Lakoff 2010). Concerned with securitization, the statist perspective directs national health policies and discourse toward defense against foreign threats (Weir and Mikhalovskiy 2010). The globalist perspective, by contrast, is concerned with the health rights and well-being of individuals beyond the enclosures of nation-states (cf. Brown, Cueto, and Fee 2006). In this way, contemporary approaches to non-endemic Chagas disease align in this way with either perspective: that is, those “overwhelmingly focused on the alarmist threat that the disease was something that would spread to the USA”, and those “evidenced by the work of non-government organizations such as Partners in Health and Médecines Sans Frontières” which could eventually overcome the “reactionary and defensive characteristics of statist thinking in global health” (De Maio, Llovet, and Dinardi 2013: 5–6).
These opposed perspectives, however, do not necessarily exclude one another. Indeed, De Maio et al. (2013) acknowledge that the heightened recognition of Chagas disease and its new epidemiological pattern could result in improved resources for affected groups, although it may at the same time “lead to a further stigmatization… and a backlash reminiscent of the ‘sick immigrant’ paradigm” (4).
But what happens with PDPs and their humanitarian framing of Chagas and other NTDs? De Maio et al. (2013) examined the disease uptake in academia, states, and NGOs, but did not consider the specific dynamics involved in public-private partnerships. While not strictly directed at private stakeholders or PDPs in particular, critical approaches to the NTD concept and discourse may suggest a response to these questions. Shahvisi (2019), for instance, suggests that the term “tropical” is both physical and conceptual: it describes a geography as well as a historical project that stems from colonial domination and marginalization. Yet the term also erases such historical traces by placing health inequalities at the level of physical determinants, an erasure that results not just in exoneration from moral responsibilities but also in a framing of existing interventions in the NTDs landscape as “supererogatory acts of kindness rather than as justice in the form of reparation or distribution” (12). The term “neglected,” on the other hand, conveys a sense of “passive” failure and omission of duties, disguising those same historical processes whereby health needs emerged in these regions and remain unmet among these populations.
Public health concerns about Chagas disease in non-endemic countries are clearly not the main reason for PDP-based initiatives such as TDR Targets or the Chagas Clinical Research Platform to exist. However, dominant representations of “neglect” and “tropicality” – that is, the essentializing discourses about the environmental prevalence of disease – align partially with the work of public-private PDPs. First, the discourses of PDP-based initiatives have been frequently accompanied by moral and political justifications that include calls for intervention into the inequalities that account for the prevalence of NTDs among the poorest. While those calls necessarily acknowledge a wider range of determinants other than mere research and development gaps, PDPs still require intermediation of major global health stakeholders and research centers in non-endemic countries to achieve and sustain their objectives. However, and even if this approach and strategy itself constitutes a laudable advancement, it is still disputable whether global health stakeholders in general and pharma in particular are fully willing or able to make the sort of impacts that, in the last instance, would be in the interest of neglected populations in developing regions instead of their own.
Second, PDP-based initiatives such as TDR Targets and the DNDI Chagas Clinical Research Platform were born out of preoccupations that differed considerably from those of biosecurity. Yet, their approach was also informed by the recent uptake of Chagas and other NTDs in non-endemic countries. Indeed, experts and public health authorities in non-endemic countries are making knowledge contributions that increasingly deviate from previous laboratory-driven approaches to neglected diseases. But again, their recent shift toward the acknowledgment of broader determinants and patient-centered rather than pathogen-centered research is not necessarily driven by a recognition of the health rights of affected individuals and collectives. Rather, it appears as a response that stems from those who feel threatened by them. Shahvisi (2019) describes this paradoxical outcome that stems from the spread of NTDs to the Global North:
“tropical” disease research was historically driven by the needs of colonial powers. More recently, its modern equivalent has been motivated by the need to contain infectious diseases which could spread to Global North regions. Neither of these incentives applies to the diseases under the NTD umbrella at this moment, since most of the diseases therein do not spread easily, and are easily treated where they affect those who have access to medical resources. Lakoff [2010] describes a major fault-line in global health between a “global health security” framing, in which infectious diseases which might threaten the Global North are prioritised, and “humanitarian biomedicine,” in which diseases of poverty which actually affect the Global South are the focus. (21).
In this way, PDPs do not necessarily contribute to securitization but respond to concerns that clearly exceed the conditions for and prevalence of NTDs and their causing pathogens in traditionally endemic regions.
Conclusion
In this paper I explored the role of public-private PDPs in transforming existing forms of representing NTDs. Doing away with state dependence and purely commercially-driven incentives, public-private partnerships are expected to overcome the market and public health failures that characterize the neglected disease research and development landscape. PDPs, in particular, take advantage of existing research capacities and infrastructures but also convene a variety of global health stakeholders – the usual and the new, such as philanthropic NGOs and transnational pharmaceutical companies – for concerted drug development efforts against NTDs. Yet, because of their reliance on highly selective stakeholders, PDPs can also enable unilateral appropriation of benefits and deviate attention and resources from critical problem areas in disease-endemic countries. In spite of the humanitarian framing of issues that fall under their scope, PDPs may also restrict participation and at the same time overemphasize the importance of pharmaceutical technologies as the ultimate cure for the poor (Mantilla 2011; Reidpath, Allotey, and Phokrell 2011). After all, such risks and unintended outcomes entailed with public-private PDPs have been defining features throughout the history of NTDs, where experts in dominant research fields and intervening organizations exercised the role of “spokesperson” for those unable to represent themselves (cf. Molyneux et al. 2021; Rabeharisoa, Moreira, and Akrich 2014; Redfield 2012). With the advent of PDPs, these asymmetries could deepen in favor of private transnational stakeholders whose interests, ultimately, hardly coincide with those of populations affected by NTDs (Lezaun and Montgomery 2014).
However, in the PDP-based initiatives analyzed in this paper – TDR Targets and DNDi Chagas Clinical Research Platform – it was not pharmaceutical firms that exerted the greatest influence upon the changing representation of NTDs. Their focus on Chagas disease, in particular, has shown how PDPs affect the disease’s back-and-forth movement from an object of scientific interest embedded in its causing pathogen to a legitimate public health concern in endemic countries. But these transformations arise from international organizations and global health NGOs changing strategies – most notably, WHO and DNDi – as well as from the influence of traditionally non-endemic countries acknowledging the disease as an incoming public health problem that stems from immigration, rather than from private pharmaceutical firms. TDR Targets, for instance, emerged from the preexisting biomedical focus on T. cruzi in endemic countries – the pathogenic organism causing Chagas disease – but also acknowledged the “real world complexity” (Reidpath, Allotey, and Phokrell 2011) (i.e., access and compliance) that held drug development back in spite of pharmaceutical promises. Yet, as WHO abandoned its funding and coordinating role to move toward field intervention, collaborations between academia and industry continue through rather ad hoc, dispersed interactions.
The DNDi Chagas Clinical Research Platform, on the other hand, emerged out of similar critiques of the existing biomedical focus in NTD research and development in general and T. cruzi research in particular. Its search for new drugs to treat Chagas disease was shaped by DNDi’s emphasis on “access,” rather than pharmaceutical technologies or causing pathogens per se, which revalued the already available drug – benznidazole – by means of establishing cure rates, efficacy, and dosing regimens instead of continuing the long and costly quest for a new drug. However, this shift in focus was not just the result of DNDi’s humanitarian framing of NTDs, but also an increasing preoccupation with Chagas disease as an emerging public health concern in non-endemic countries.
In closing, the focus on Chagas disease and its causing pathogen might be relevant not just to the field of NTDs – where the disease is considered a “paradigm” in non-endemic countries – but also more generally to STS and critical analyses of PDPs. The two initiatives analyzed in this paper have shown how knowledge production on the disease and its uptake as a public health concern affect each other – what Jasanoff (2004) terms “co-production” in STS. But these processes are not just restricted to the disciplinary fields within which the disease is understood, or to the bodies of expert knowledge utilized to devise intervention strategies. They are, at the same time, shaped by changes in the logic and spaces of knowledge production – or, what I have referred to as epistemic and geographical shifts. Epistemic shifts are reflected in the changes that affect the research and development focus as well as the new social configuration embedded in PDPs: their previous biomedical focus was not abandoned, but the intervening stakeholders attempted to complement the dominant views and emphasis on the disease-causing pathogen by recognizing the structural and contextual limitations embedded in such perspective. These shifts, however, were complemented by one that is geographical in nature, which moved the focus away from the causing pathogen and back to “patients” in a way that combines a global humanitarian medical aim with securitization against the perceived threat posed by immigrant populations in non-endemic countries.
Notes
The criteria used to define NTDs vary and sometimes overlap with those used in more encompassing terms such as “neglected diseases,” which frequently include malaria, tuberculosis, and HIV/AIDS (e.g. Policy Cures Research 2021). In this paper I use the term NTDs to refer to the nearly 20 infectious diseases listed by WHO (2022a) – which excludes the aforementioned “big three” (malaria, tuberculosis, and HIV/AIDS) – but also acknowledge that such terminologies call for critical scrutiny (see Shahvisi 2019).
Country-specific data on transmission remains elusive. Transmission types and rates may vary greatly depending on environmental and epidemiological factors such as success of vector control programs, extension of extractive farming, and broader demographic processes (Chagas Coalition 2023; Plataforma de Investigación Clínica en Enfermedad de Chagas 2019; WHO 2022c).
This and all following translations into English are my own.
Vector control initiatives were arguably more successful in Brazil, Chile, Colombia, Guatemala, and Uruguay, although their success depended critically on support provided by international agencies and global health NGOs (IS Global 2012; Plataforma de Investigación Clínica en Enfermedad de Chagas 2019).
The whole project execution involved more than 20 laboratories throughout the Americas and Europe. Argentinean core loci representatives played a crucial role in exerting influence upon its funders and coordinating institutions: for example, Mariano J. Levin (1999), one of the principal project associates, envisaged the practical outlines of the project with Daniel Cohen, a French geneticist and central figure in the HGP who endorsed the TcGP shortly before it was launched; A. Carlos Frasch, another principal associate, relied on his position as an advisor on parasitic diseases for several WHO committees to secure funds from the United States National Institutes of Health among other sources (Ferpozzi 2020).
Recent sources included joint funding from GlaxoSmithKline Argentina and the National Agency for the Promotion of Science and Technology as well as the Indo-Argentina Bilateral Cooperation Project, a joint funding from the Indian Department of Science and Technology and the Argentinian Ministry of Science and Technology. Among its current collaborators are the Indian National Chemical Laboratory and the Argentinian non-profit research foundation Leloir Institute. Collaborators’ expertise lies chiefly in molecular and computational biology, genetics, biochemistry, and parasitology.
Among the founding members of DNDi were also public research organizations and health ministries in Brazil, Kenia, Malaysia, and France.
Other NTDs under the DNDi scope include visceral and cutaneous leishmaniases, sleeping sickness, mycetoma, and river blindness. In 2020 the initiative launched the COVID-19 Clinical Research Coalition.
Bibliographic clusters represent articles grouped according to the similarity or “coupling” of references. The underlying assumption is that “texts sharing more references are closer in epistemic space” (Levin, Kreimer and Jensen 2021: 4). The top two clusters reviewed above make up roughly 30 percent of almost 20,000 articles published between 1921 and 2019 registered in the Web of Science.
Another cluster pertaining to drug discovery with around 8 percent publication share is associated with clinical trials driven by DNDi (Levin, Kreimer, and Jensen 2021: 9).
References
Angheben, Andrea, Lucia Boix, Dora Buonfrate, Federico Gobbi, Zeno Bisoffi, Simonetta Pupella, and Giorgio Gandini, and Giuseppe Aprili. 2015. Chagas Disease and Transfusion Medicine: A Perspective from Non-Endemic Countries. Blood Transfusion 3(4): 540–550. https://doi.org/10.2450/2015.0040-15.
Basalla, George. 1967. The Spread of Western Science. A Three-Stage Model Describes the Introduction of Modern Science into Any Non-European Nation. Science 156(3775): 611–622. https://doi.org/10.1126/science.156.3775.611.
Bern, Caryn, Louisa A. Messenger, Jeffrey D. Whitman, and James H. Maguire. 2019. Chagas Disease in the United States: A Public Health Approach. Clinical Microbiology Reviews 33(1). https://doi.org/10.1128/CMR.00023-19.
Brown, Theodore M., Marcos Cueto, and Elizabeth Fee. 2006. The World Health Organization and the Transition From ‘International’ to ‘Global’ Public Health. American Journal of Public Health 96(1): 62–72. https://doi.org/10.2105/ajph.2004.050831.
Börzel, Tanja, and Thomas Risse. 2005. Public–Private Partnership. Effective and Legitimate Tools of Transnational Governance? In Complex Sovereignty: Reconstituting Political Authority in the Twenty-First Century, eds. E. Grande and L. W. Pauly, 195–216. Toronto: University of Toronto Press.
Buse, Kent, and Gill Walt. 2000a. Global Public–Private Partnerships for Health: Part I – a new development in health? Bulletin of the World Health Organization – The International Journal of Public Health 78 (4): 549–561.
———. (2000b). Global Public–Private Partnerships for Health: Part II – what are the health issues for global governance?. Bulletin of the World Health Organization – The International Journal of Public Health 78(5): 699–709.
Chagas Coalition. 2023. How is it transmitted? https://www.infochagas.org/en/como-se-transmite. Accessed January 9 2023.
Childs, Michelle. 2011. Innovación, acceso y desafíos relacionados con la enfermedad de Chagas. Plataforma de Investigación Clínica En Enfermedad de Chagas 1: 9.
Croft, Simon L. 2005. Public-Private Partnership: From There to Here. Transactions of the Royal Society of Tropical Medicine and Hygiene 99 (January): 9–14. https://doi.org/10.1016/j.trstmh.2005.06.008.
Davies, Sara E. 2010. Global Politics of Health. Cambridge: Polity Press.
De Maio, Fernando G., Ignacio Llovet, and Graciela Dinardi. 2013. Chagas Disease in Non-Endemic Countries: ‘Sick Immigrant’ Phobia or a Public Health Concern? Critical Public Health 24(3): 372–380. https://doi.org/10.1080/09581596.2013.836589.
DNDi, Latin America. 2015. Medicamentos para Poblaciones Olvidadas. Informe Anual. Rio de Janeiro: DNDi América Latina. https://www.dndial.org/es/communicacion/informe-anual-2/. Accessed April 18 2022.
DNDi Latin America. 2021. Plataforma de Chagas. https://www.dndial.org/es/enfermedades/enfermedad-chagas/plataformadechagas/. Accessed April 18 2022.
El-Sayed, N. M., P. J. Myler, D. C. Bartholomeu, D. Nilsson, et al. 2005. The Genome Sequence of Trypanosoma cruzi, Etiologic Agent of Chagas Disease. Science 309(5733): 409–415. https://doi.org/10.1126/science.1112631.
Eurosurveillance editorial team. 2011. A Note from the Editors: Chagas Disease: Neglected in Europe? Euro Surveillance : European Communicable Disease Bulletin 16 (37): 19970.
Ferpozzi, Hugo. 2020. Straight Outta the Tropics: Pathological Features of Techno-Scientific Promises in Neglected Tropical Disease Research, Tapuya: Latin American Science. Technology and Society 3(1): 205–226. https://doi.org/10.1080/25729861.2020.1819078
Ferrari, I., H. Lorenzi, M. R. Santos, S. Brandariz, et al. 1997. Towards the Physical Map of the Trypanosoma Cruzi Nuclear Genome: Construction of YAC and BAC Libraries of the Reference Clone T. Cruzi CL-Brener. Memorias Do Instituto Oswaldo Cruz 92(6): 843–852. https://doi.org/10.1590/S0074-02761997000600021.
Füller, Henning. 2014. Global health security? Questioning an ‘emerging diseases worldview’. In World Disasters Report. Focus on Culture and Risk, eds. T. Cannon and L. Schipper, 176–77. International Federation of Red Cross and Red Crescent Societies.
GBD. 2016. Global, Regional, and Expectancy, National Life, All-Cause Mortality, and Cause-Specific Mortality for 249 Causes of Death, 1980–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. The Lancet 388(10053): 1459–1544. https://doi.org/10.1016/s0140-6736(16)31012-1.
Gusfield, Joseph. 1981. The Culture of Public Problems. Drinking-Driving and the Symbolic Order. Chicago, IL: University of Chicago Press.
Hotez, Peter J. 2011. The development impact of the neglected tropical diseases (NTDs). Expert paper. New York: United Nations. https://www.un.org/development/desa/pd/fr/node/2517. Accessed April 18 2022.
Hotez, Peter J. 2017. The Poverty-Related Neglected Diseases: Why Basic Research Matters. PLOS Biology 15(11): e2004186. https://doi.org/10.1371/journal.pbio.2004186.
Hotez, Peter J., Eric Dumonteil, Laila Woc-Colburn, Jose A. Serpa, et al. 2012. Chagas Disease: ‘The New HIV/AIDS of the Americas.’ PLoS Neglected Tropical Diseases 6(5): e1498. https://doi.org/10.1371/journal.pntd.0001498.
Hotez, Peter J., Eric Dumonteil, Miguel Betancourt Cravioto, Maria Elena Bottazzi, et al. 2013. An Unfolding Tragedy of Chagas Disease in North America. PLoS Neglected Tropical Diseases 7(10): e2300. https://doi.org/10.1371/journal.pntd.0002300.
Imai, Kazuo, Kazuhisa Misawa, Morichika Osa, Norihito Tarumoto, et al. 2019. Chagas Disease: A Report of 17 Suspected Cases in Japan, 2012–2017. Tropical Medicine and Health 47(1): 38. https://doi.org/10.1186/s41182-019-0168-3.
IS Global. 2012. Chagas: A Disease That Can No Longer Be Neglected. Barcelona: Barcelona Institute for Health. https://www.isglobal.org/en/-/chagas-a-disease-that-can-no-longer-be-neglected. Accessed April 18 2022.
Jackson, Yves, Angie Pinto, and Sarah Pett. 2014. Chagas Disease in Australia and New Zealand: Risks and Needs for Public Health Interventions. Tropical Medicine & International Health 19(2): 212–218. https://doi.org/10.1111/tmi.12235.
Jasanoff, Sheila. 2004. Ordering knowledge, ordering society. In States of Knowledge: The Co-Production of Science and the Social Order, edited by S. Jasanoff, 13–45. New York: Routledge.
Jörg, Miguel, and Rubén Storino. 2002. La enfermedad de Chagas en el siglo XXI: Consenso para una asignatura pendiente”. Revista Argentina de Cardiología 70(1): 10–11.
Kaul, Inge. 2006. Exploring the Policy Space Between Market and States: Global Public–Private Partnerships. In The New Public Finance: Responding to Global Challenges, edited by I. Kaul and P. Conceição, 219–268. Oxford: Oxford University Press.
Keating, Conrad. 2014. Ken Warren and the Rockefeller Foundation’s Great Neglected Diseases Network, 1978–1988: The Transformation of Tropical and Global Medicine. Molecular Medicine 20(S1): S24–S30. https://doi.org/10.2119/molmed.2014.00221.
Kirchhoff, L. V., A. A. Gam, and F. C. Gilliam. 1987. American Trypanosomiasis (Chagas’ Disease) in Central American Immigrants. The American Journal of Medicine 82(5): 915–920. https://doi.org/10.1016/0002-9343(87)90152-5.
Kreimer, Pablo. 2015. Co-producing Social Problems and Scientific Knowledge: Chagas Disease and the Dynamics of Research Fields in Latin America. In Sociology of Science Yearbook, edited by M. Merz and P. Sormani, 173–90. Dordrecht: Springer.
Kreimer, Pablo. 2019. Science and Society in Latin America: Peripheral Modernities. New York: Routledge.
Kreimer, Pablo, and Juan P. Zabala. 2007. Chagas Disease in Argentina: Reciprocal Construction of Social and Scientific Problems. Science, Technology & Society 12(1): 49–72. https://doi.org/10.1177/097172180601200104.
Kropf, Simone Petraglia. 2009. Doença de Chagas, Doença do Brasil: ciência, saúde e nação, 1909–1962. Rio de Janeiro: Editora Fiocruz.
Lakoff, Andrew. 2010. Two Regimes of Global Health. Humanity: An International Journal of Human Rights, Humanitarianism, and Development 1(1): 59–79. https://doi.org/10.1353/hum.2010.0001.
Latour, Bruno. 2004. Why Has Critique Run out of Steam? From Matters of Fact to Matters of Concern. Critical Inquiry 30(2): 225–248. https://doi.org/10.1086/421123.
Levin, Luciano G., Pablo Kreimer, and Pablo Jensen. 2021. Chagas Disease across Contexts: Scientific Knowledge in a Globalized World. Medical Anthropology 40(6): 572–589. https://doi.org/10.1080/01459740.2021.1946805.
Levin, Mariano J. 1999. Contribución del proyecto genoma de Trypanosoma cruzi a la comprensión de la patogénesis de la cardiomiopatía chagásica crónica. Medicina 59 (II): 18–24.
Lezaun, Javier, and Catherine M. Montgomery. 2014. The Pharmaceutical Commons. Science, Technology, & Human Values 40(1): 3–29. https://doi.org/10.1177/0162243914542349.
Liese, Bernhard, Mark Rosenberg, and Alexander Schratz. 2010. Programmes, Partnerships, and Governance for Elimination and Control of Neglected Tropical Diseases. The Lancet 375(9708): 67–76. https://doi.org/10.1016/s0140-6736(09)61749-9.
Mantilla, Bryanna. 2011.Invisible Plagues, Invisible Voices: A Critical Discourse Analysis of Neglected Tropical Diseases. Social Medicine 6(3): 118–127.
Martens, Jens. 2003. The Future of Multilateralism after Monterrey and Johannesburg, Dialogue on Globalization. Occasional Papers (10). Berlin: Friedrich Ebert Stiftung.
Marx, Karl. 1975. [1852]. In The eighteenth Brumaire of Louis Bonaparte. New York: International Publishers.
Molyneux, David H, Alan Fenwick, Anarfi Asamoa-Bah, Lorenzo Savioli, and Peter Hotez. 2021. The History of the Neglected Tropical Disease Movement. Transactions of The Royal Society of Tropical Medicine and Hygiene 115(2): 169–175. https://doi.org/10.1093/trstmh/trab015.
Moran, Mary. 2005. A Breakthrough in R&D for Neglected Diseases: New Ways to Get the Drugs We Need. PLoS Medicine 2(9): e302. https://doi.org/10.1371/journal.pmed.0020302.
Mörth, Ulrika. 2009. The Market Turn in EU Governance–The Emergence of Public–Private Collaboration. Governance 22(1): 99–120. https://doi.org/10.1111/j.1468-0491.2008.01423.x.
MSF. 2001. Fatal Imbalance. The Crisis in Research and Development for Drugs for Neglected Diseases. Geneva: Médecins Sans Frontières Access to Essential Medicines Campaign and the Drugs for Neglected Diseases Working Group. https://msfaccess.org/fatal-imbalance-crisis-research-and-development-drugs-neglected-diseases. Accessed April 18 2021.
Nwaka, Solomon, and Robert G. Ridley. 2003. Virtual Drug Discovery and Development for Neglected Diseases through Public–Private Partnerships. Nature Reviews Drug Discovery 2(11): 919–928. https://doi.org/10.1038/nrd1230.
PAHO. n.d. Chagas Disease. https://www.paho.org/en/topics/chagas-disease. Accessed January 10 2023.
Parker, Melissa, Katja Polman, and Tim Allen. 2016. Neglected Tropical Diseases in Biosocial Perspective. Journal of Biosocial Science 48(S1): S1–S15. https://doi.org/10.1017/s0021932016000274.
Pedrique, Belen, Nathalie Strub-Wourgaft, Claudette Some, Piero Olliaro, Patrice Trouiller, Nathan Ford, Bernard Pécoul, and Bradol Jean-Hervé. 2013. The Drug and Vaccine Landscape for Neglected Diseases (2000–11): A Systematic Assessment. The Lancet Global Health 1(6): e371–e379. https://doi.org/10.1016/s2214-109x(13)70078-0.
Pehrson Pehr-Olov, Mats Wahlgren, and Elias Bengtsson. 1981. Asymptomatic Congenital Chagas’ Disease in a 5-Year-Old Child. Scandinavian Journal of Infectious Diseases 13(4): 307–308. https://doi.org/10.3109/inf.1981.13.issue-4.14.
Plataforma de Investigación Clínica en Enfermedad de Chagas. 2019. Informativo no. 9. Rio de Janeiro: DNDi América Latina.
Policy Cures Research. 2021. Neglected Disease Research and Development: Where to now?. Surry Hills, Australia: Policy Cures Research. https://policy-cures-website-assets.s3.ap-southeast-2.amazonaws.com/wp-content/uploads/2021/04/15055816/G-FINDER-2020_Final-Report.pdf. Accessed April 18 2022.
Rabeharisoa, Vololona, Tiago Moreira, and Madeleine Akrich. 2014. Evidence-Based Activism: Patients’, Users’ and Activists’ Groups in Knowledge Society. BioSocieties 9(2): 111–128. https://doi.org/10.1057/biosoc.2014.2.
Redfield, Peter. 2012. Bioexpectations: Life Technologies as Humanitarian Goods. Public Culture 24(1): 157–184. https://doi.org/10.1215/08992363-1443592.
Reidpath, Daniel D., Pascale Allotey, and Subhash Pokhrel. 2011. Social Sciences Research in Neglected Tropical Diseases 2: A Bibliographic Analysis. Health Research Policy and Systems 9(1). https://doi.org/10.1186/1478-4505-9-1.
Richter, Judith. 2004. Public–Private Partnerships for Health: A Trend with No Alternatives? Development 47(2): 43–48. https://doi.org/10.1057/palgrave.development.1100043.
Richter, Judith. 2005. Global partnerships and Health for All: Towards an institutional strategy. A discussion paper prepared for WHO’s Department of Government, Civil Society and Private Sector Relations (GPR). Geneva: World Health Organization.
Ridley, Robert G., Peter Ndumbe, and Rolf Korte. 2008. Two Years after the Fourth External Review: TDR Moves Forward with a New Vision and Strategy. PLoS Neglected Tropical Diseases 2(11): e307. https://doi.org/10.1371/journal.pntd.0000307.
Rodriguez-Medina L, Ferpozzi H, Layna J, Martin Valdez E and Kreimer P (2019) International Ties at Peripheral Sites: Coproducing Social Processes and Scientific Knowledge in Latin America. Science as Culture 28(4): 562–88. https://doi.org/10.1080/09505431.2019.1629409
Sanmartino, Mariana. 2009. 100 años de Chagas (1909–2009): Revisión, Balance y Perspectiva. Revista de la Sociedad Entomológica Argentina 68(3–4): 243–52.
Savioli, L., A. Montresor, and A. Gabrielli. 2011. Neglected Tropical Diseases: The Development of a Brand with No Copyright. A Shift from a Disease-Centered to a Tool-Centered Strategic Approach. In The Causes and Impacts of Neglected Tropical and Zoonotic Diseases: Opportunities for Integrated Intervention Strategies, edited by E. R. Choffnes, D. A. Relman, and Forum on Microbial Threats Board on Global Health, 481–489. Washington, DC: The National Academies Press.
Schmunis, Gabriel A. 2007. Epidemiology of Chagas Disease in Non Endemic Countries: The Role of International Migration. Memórias Do Instituto Oswaldo Cruz 102 (S1): 75–86. https://doi.org/10.1590/s0074-02762007005000093.
Schuppert, Gunnar Folke. 2011. Partnerships. In The SAGE Handbook of Governance, ed. M. Bevir, 286–99. London: SAGE. https://doi.org/10.4135/9781446200964.n18.
Shahvisi, Arianne. 2019. Tropicality and Abjection: What Do We Really Mean by ‘Neglected Tropical Diseases’? Developing World Bioethics 19(4): 224–234. https://doi.org/10.1111/dewb.12223.
Sosa-Estani, Sergio. 2011. Nuevo Escenario de Estudios Clínicos y Perspectivas Para los Próximos Años. Plataforma de Investigación Clínica En Enfermedad de Chagas 1: 11.
Strasen, Jörn, Tatjana Williams, Georg Ertl, Thomas Zoller, August Stich, and Oliver Ritter. 2014. Epidemiology of Chagas Disease in Europe: Many Calculations, Little Knowledge. Clinical Research in Cardiology: Official Journal of the German Cardiac Society 103(1): 1–10. https://doi.org/10.1007/s00392-013-0613-y.
Trouiller, Patrice, Piero Olliaro, Els Torreele, James Orbinski, and Richard Laing, and Nathan Ford. 2002. Drug Development for Neglected Diseases: A Deficient Market and a Public-Health Policy Failure. The Lancet 359 (9324): 2188–2194. https://doi.org/10.1016/s0140-6736(02)09096-7.
Trypanosoma cruzi Genome Consortium. 1997. The Trypanosoma Cruzi Genome Initiative. Parasitology Today 13(1): 247–292. https://doi.org/10.1016/s0169-4758(96)10074-0.
Urán Landaburu, Lionel, Ariel J, Santiago Berenstein, Parag Videla, Dhanasekaran Maru, Ariel Shanmugam, and Chernomoretz, and Fernán Agüero. 2019. TDR Targets 6: Driving Drug Discovery for Human Pathogens through Intensive Chemogenomic Data Integration. Nucleic Acids Research 48. https://doi.org/10.1093/nar/gkz999.
Weir, Lorna, and Eric. Mykhalovskiy. 2010. Global Public Health Vigilance. Creating a World on Alert. New York: Routledge.
WHO. 2022a. Neglected Tropical Diseases. https://www.who.int/news-room/questions-and-answers/item/neglected-tropical-diseases. Accessed April 18 2022.
WHO. 2022b. Chagas disease (also known as American Trypanosomiasis). https://www.who.int/news-room/fact-sheets/detail/chagas-disease-(american-trypanosomiasis). Accessed January 9 2023.
WHO 2022c. World Chagas Disease Day: finding and reporting every case. https://www.who.int/news/item/14-04-2022-world-chagas-disease-day-bringing-a-forgotten-disease-to-the-fore-of-global-attention. Accessed January 9 2023.
WHO, UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases, and Pan American Health Organization. 2007. Reporte del grupo de trabajo científico sobre la enfermedad de Chagas: 17–20 de abril de 2005, actualizado en julio de 2007, edited by F. Guhl and J. K. Lazdins-Helds. Buenos Aires, Argentina: World Health Organization. https://apps.who.int/iris/handle/10665/69724/. Accessed April 18 2022.
Yamey, Gavin. 2002. Public Sector Must Develop Drugs for Neglected Diseases. Bmj 324 (7339): 698. https://doi.org/10.1136/bmj.324.7339.698/b.
Zabala, Juan P. 2010. La enfermedad de Chagas en la Argentina. Investigación científica, problemas sociales y políticas sanitarias [Chagas disease in Argentina. Scientific reserach, social problems, and sanitation policies.]. Bernal: Universidad Nacional de Quilmes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ferpozzi, H. Public-Private Partnerships and the Landscape of Neglected Tropical Disease Research: The Shifting Logic and Spaces of Knowledge Production. Minerva 61, 607–629 (2023). https://doi.org/10.1007/s11024-023-09496-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11024-023-09496-x