Abstract
Malnutrition and low dietary protein intake could be risk factors for developing peripheral and central hyperammonemia, especially in pediatrics. Both curcumin and resveratrol proved to be effective against several hepatic and cerebral injuries. They were reported to be beneficial in lowering circulating ammonia levels, yet both are known for their low bioavailability. The use of pharmaceutical nano-formulations as delivery systems for these two nutraceuticals could solve the aforementioned problem. Hence, the present study aimed to investigate the valuable outcome of using a combination of curcumin and resveratrol in a nanoemulsion formulation, to counteract protein-deficient diet (PDD)-induced hyperammonemia and the consequent complications in male albino rats. Results revealed that using a nanoemulsion containing both curcumin and resveratrol at a dose of (5 + 5 mg/kg) effectively reduced hepatic and brain ammonia levels, serum ALT and AST levels, hepatic and brain nitric oxide levels, oxidative DNA damage as well as disrupted cellular energy performance. In addition, there was a substantial increase in brain levels of monoamines, and a decrease in glutamate content. Therefore, it can be concluded that the use of combined curcumin and resveratrol nanoemulsion is an effective means of ameliorating the hepatic and cerebral adverse effects resulting from PDD-induced hyperammonemia in rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperammonemia is a metabolic condition characterized by elevated ammonia levels, which could lead to the development of acute and chronic liver diseases (Gutiérrez-de-Juan et al. 2017). It is also well established that hyperammonemia resulting from chronic liver disease is a key factor in the pathogenesis of brain dysfunction. Elevated brain ammonia can cause several complications, including impairment of energy utilization by brain cells, as well as disruption of monoaminergic neurotransmitter systems. Studies have demonstrated dopaminergic, noradrenergic and serotonergic neurotransmission alterations by experimentally-induced hyperammonemia (Ronan et al. 2007; Kawai et al. 2012; Higarza et al. 2019; Baraka et al. 2020). In addition, ammonia homeostasis is tightly regulated and linked to the recycling of the major excitatory neurotransmitter glutamate (Cabrera-Pastor et al. 2019), which is the main excitatory neurotransmitter in the central nervous system, and consequently, its alterations are associated with neurological problems (Singh et al. 2014). Particularly, when extracellular glutamate is elevated, glutamate acts as a toxic substance leading to neuronal dysfunction (Ochoa-Sanchez and Rose 2018). Besides, elevated concentrations of ammonia have been shown to generate excessive production of nitric oxide (NOx) (Dasarathy et al. 2017).
Previous investigators have highlighted the hazards of developing hyperammonemia in pediatrics especially in late infancy. Any imbalance in protein and/or energy demands is considered a risk for hyperammonemia (Häberle 2011). Malnutrition, low dietary protein and low amino acids intake can increase peripheral and consequently central ammonia levels (Holecek 2015; Hadjihambi et al. 2018).
Curcumin; a polyphenolic compound, is a component of Curcuma longa. It is a well-known anti-inflammatory and antioxidant molecule. Several studies have highlighted the role of curcumin in many different types of human pathologies, including neurocognitive disorders (Di Meo et al. 2019; Yavarpour-Bali et al. 2019). It was also reported to down-regulate the enzymatic activity of inducible nitric oxide synthase (iNOS) (Ghorbani et al. 2014; Boyanapalli and Kong 2015). Besides, curcumin was demonstrated to reduce brain edema after extrahepatic and intrahepatic damage (Frozandeh et al. 2021) as well as lower serum ammonia levels (Huang et al. 2015; Frozandeh et al. 2021).
On the other hand, resveratrol is a natural polyphenolic compound that exhibits beneficial pharmacological properties in a wide range of brain abnormalities; acting mainly as a neuroprotective with monoamines-preserving potential. It was reported to exhibit protective effects against many neurodegenerative diseases (Aguirre et al. 2014; Martínez-Abundis et al. 2016; Ahmed et al. 2020), and it was particularly shown to prevent ammonia toxicity by modulating oxidative stress (Malaguarnera et al. 2018; Kim and Song 2021). Moreover, it was reported that resveratrol exhibited neuroprotective effect against glutamate toxicity (Quincozes-Santos et al. 2014).
Nowadays, therapies based on nanotechnologies have emerged as an innovative and promising alternative to conventional therapy in the treatment of liver diseases (Al-Shakarchi et al. 2018). Therefore, the present study aimed to investigate the beneficial effects of using a combination of resveratrol and curcumin in a nanoemulsion formulation, to counteract protein-deficient diet (PDD)-induced hyperammonemia, and the consequent development of brain dysfunction in juvenile male albino rats.
Materials and methods
Solvents and drugs
Curcumin, resveratrol, phenobarbital, sodium hydrogen phosphate, potassium dihydrogen phosphate, methanol, acetonitrile, potassium hydroxide, ammonium acetate, potassium phosphate and sodium chloride were purchased from Sigma Aldrich, Germany. Labrafac Lipophile WL 1349 was kindly gifted by Gattefosse’, France. Cremophor RH was kindly gifted by BASF, Germany.
Preparation and characterization of nanoemulsions
Preparation of the nanoemulsions of curcumin, resveratrol and their combination was carried out using the spontaneous emulsification method as previously described (Nasr 2016). Briefly, 50 mg of each drug or both drugs were dissolved in Labrafac Lipophile oil (10% w/v) and Cremophor RH surfactant (10% w/v), followed by their gradual addition to a magnetically-stirred aqueous phase at room temperature (IKA C-MAG HS 7, Germany). The nanoemulsions were characterized for their particle size, polydispersity and surface charge using the Zetasizer device (Malvern, UK), after dilution 1:100 with deionized water at 25 °C, and equilibration time of two minutes. The detection angle was 173 °C, and the refractive index was set to 1.33 (Nasr 2016).
Animals
Male Wistar albino juvenile rats weighing 60–70 g were purchased from the National Research Centre (NRC) animal house. Animals were acclimatized for seven days before proceeding further with the experimental research. All experimental procedures followed the regulations of the Research Ethics Committee of the National Research Centre (approval number 2,415,062,022) in accordance with relevant national guidelines and regulations and compliance with the ARRIVE guidelines.
Experimental design
Rats were divided into eight groups (n = 16). The first group was designated as the normal control and was fed a normal standard recommended rats’ pellet diet for seventy-five days, kept in the same room and under the same conditions as all the other groups, and ingested 5 ml/kg distilled water daily during the last fifteen days. The seven other groups were fed a protein-deficient diet (PDD) consisting of pellets of shelled corn grains for 75 days (Ahmed-Farid et al. 2017). Drug treatments started from day 61 and for 15 days; in which two groups (RL and RH) ingested the resveratrol nanoemulsion at two dose levels (2.5 and 5 mg/kg, p.o), two groups (CL and CH) ingested the curcumin nanoemulsion at two dose levels (2.5 and 5 mg/ kg, p.o), two groups (MRCL and MRCH) ingested the combination nanoemulsion at two dose levels (2.5 + 2.5 and 5 + 5 mg/ kg, p.o). The final group assigned as PDD control was given daily oral ingestion of distilled water (5 ml/ kg, p.o).
On day 76, after the last treatments ingestions by 24 h, rats in each group were divided randomly into two subsets of 8 rats; the first subset was subjected to phenobarbital anesthesia for blood samples collection, and the other subset was sacrificed by decapitation for brain and liver tissues’ collection. Tissues were kept at -80 °C for further studies.
Quantification of serum ALT and AST levels (IU/L) in serum
Serum total aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels were measured spectrophotometrically with JASCO V-630 spectrophotometer (Serial No. C322461148 Japan) using a kit provided by a local supplier (Bio-diagnostic Co.) (Reitman and Frankel 1957). For more information, the kit’s manual is provided as supplementary material.
Quantification of hepatic and brain ammonia (µmol/g), NOx (µmol/g), 8-OHdG content (pg/g), ATP, ADP and AMP (µg/g), brain 5-HT, NE, DA and glutamate (µg/g) in brain or liver tissues
Brain or liver tissues were homogenized in phosphate buffer. The supernatant was separated. Ammonia was assessed spectrophotometrically with JASCO V-630 spectrophotometer (Serial No. C322461148 Japan), in which 1 ml of liver or brain supernatant was added to 1.5 ml of phenol–nitroprusside reagent and 2 ml of sodium hypochlorite reagent and the mixture was left for 20 min at room temperature. The color intensity was then measured at 630 nm against distilled water blank, and ammonium chloride (0.1–1.0 mmol) was used as standard (Oyovwi et al. 2021).
For all other brain and liver parameters, HPLC system (Agilent HP 1200 series, USA) consisting of quaternary pump, column oven, Rheodine injector and 20 µl loop, and UV variable wavelength detector was used. The report and chromatograms were taken from Chemstation program (Agilent, USA). For the assessment of brain glutamate level, C18 reversed phase column was used. The mobile phase was a seven-step gradient of increasing concentrations of solvent B from 5 to 70%. Solvent A was composed of 50 mM ammonium acetate (pH 6.5) and solvent B was 100 mM ammonium acetate (pH 6.5): acetonitrile (1:1). The flow rate was 2 ml/min, and detection was performed at wavelength 254 nm. (Ahmed-Farid et al. 2017). For serotonin (5-HT), norepinephrine (NE) and dopamine (DA) levels, an AQUA column C18 was used. The mobile phase was 20mM potassium phosphate, pH 2.5: methanol (99:1), the flow rate 1.5ml/min, and detection was done at wavelength 210 nm (Pagel et al. 2000). For the brain and hepatic nitric oxide (nitrates + nitrites) (NOx) levels, the analytical column was anion exchange PRP-X100 Hamilton. The mobile phase was a mixture of 0.1 M sodium chloride:methanol, at a volume ratio of 45:55, the flow rate was 2 ml/min, and the detection wavelength was 230 nm (Papadoyannis et al. 1999). For the brain and hepatic 8-hydroxy-2-deoxyguanosine (8-OHdG) levels, the analytical column was C18 reverse phase column. The eluting solution was water:methanol at a ratio of 85:15 with 50 mM potassium dihydrogen phosphate pH 5.5, at a flow rate of 0.68 ml/min; detected at wavelength 245 nm (Lodovici et al. 1997). For the brain and hepatic adenosine tri, di and monophosphate (ATP, ADP and AMP) levels, the analytical column was Ultrasphere ODS EC column. The mobile phase A consisted of potassium dihydrogen phosphate solution adjusted to pH 7.0 using 0.1 mol/L potassium hydroxide, while mobile phase B consisted of 100% acetonitrile. Flow rate of the mobile phase was 1.2 ml/min, and the detection wavelength was 254 nm. The resulting data was also used for computation of AMP/ATP ratio as well as the total adenylate energy charge (AEC) according to the equation: (ATP + 1/2ADP)/(ATP + ADP + AMP) (Atkinson and Walton 1967; Teerlink et al. 1993; Saleh et al. 2017b).
Statistical analyses
Statistical analyses were carried out using one-way ANOVA followed by Tukey’s multiple comparisons test. P < 0.05 was accepted as significant in all types of statistical tests. Graph prism software, version 9 was used to carry out all statistical tests. Values were expressed as means ± S.E. Pearson’s correlation study was conducted using the same software program where the difference was considered significant at P < 0.0001.
Results
Characterization of the nanoemulsions
The properties of the prepared nanoemulsions are displayed in Table 1.
Impact on serum hepatic enzymes ALT and AST
Both ALT and AST levels were significantly elevated by 92.61% and 23.82% respectively, after chronic ingestion of the PDD diet for seventy-five days as compared to the normal group. Generally, most treatment groups normalized ALT levels and significantly reduced AST levels compared to the PDD control group. It is worth mentioning that ingesting the nanoemulsion formulation containing both curcumin and resveratrol at a dose level of 5 + 5 mg/kg normalized both ALT and AST levels (Fig. 1).
Impact on hepatic and brain ammonia levels
Chronic ingestion of the PDD diet resulted in a significant elevation in the hepatic ammonia level, and consequently the brain ammonia level by 77.19% and 81.17% respectively, compared to the normal group. All nanoformulations significantly reduced the hepatic ammonia levels, whereas; only curcumin and resveratrol ingested at the higher dose level (5 mg/kg) as well as both dose levels of the combined formulations significantly reduced the brain ammonia level (Fig. 2).
Impact on hepatic and brain NOx levels and 8-OHdG levels
The protein-deficient diet resulted in an extensive elevation in both hepatic and brain NOx levels by 80.79% and 107.16% respectively, as well as a substantial increase in the 8-OHdG levels by 82.4% and 96.97% respectively, as compared to the normal group. Ingesting the combined formulation at the higher dose level normalized both parameters in both organs. In addition, all other treatment groups significantly reduced both parameters compared to the PDD group (Fig. 3).
Impact on hepatic and brain cellular energy parameters
Ingestion of PDD significantly disrupted the hepatic and brain cellular energy parameters, represented by a substantial decrease in the ATP levels by 56.3% and 49.8% respectively, as well as a significant decrease in the AEC ratios (0.52, 0.54 vs. 0.72, 0.71) respectively, in addition to extensive increase in the AMP/ATP ratios (0.87, 0.81 vs. 0.16, 0.22) respectively, as compared to the normal group. All treatment groups managed to ameliorate this disruption in cellular energy parameters compared to the PDD group, where the most promising results were obtained when ingesting the combination formulation of the higher dose levels of MRCH (Fig. 4).
Impact on brain monoaminergic neurotransmitters and glutamate levels
Ingestion of PDD chronically resulted in a significant reduction in serotonin, dopamine, and norepinephrine levels by 31.86%, 57.32% and 40.8% respectively, compared to the normal group. Meanwhile, it substantially elevated the glutamate level by 58.6%. Treatment with the formulations under investigation significantly ameliorated the disruption in the monoaminergic neurotransmitters and glutamate levels (Fig. 5).
Correlation studies
Correlation studies revealed a positive correlation between the elevated hepatic ammonia level and hepatic levels of NOx, 8-OHdG, and AMP/ATP ratio, as well as serum ALT and AST. There was also a negative correlation between elevated hepatic ammonia level and hepatic ATP level as well as hepatic AEC ratio, indicating that elevated hepatic ammonia level is a direct cause of liver injury represented by the pronounced nitrosative stress, oxidative DNA damage, disrupted cellular energy and elevated serum hepatic enzymes levels. Moreover, there was a positive correlation between elevated hepatic ammonia and elevated brain ammonia levels. Besides, elevated brain ammonia level was directly correlated to elevated brain contents of glutamate, NOx, 8-OHdG, AMP/ATP ratio, and inversely correlated to brain levels of monoamines, ATP, and AEC ratio; designating that brain hyperammonemia could be a leading cause of development of cerebral dysfunction. (Figs. 6 and 7)
Discussion
The present study aimed to investigate the beneficial effects of using resveratrol and curcumin in nanoemulsions either alone or in combination to counteract the adverse effects of ingesting a PDD in juvenile rats chronically for seventy-five days, represented by the development of hepatic and brain hyperammonemia and the accompanying consequences on brain monoaminergic and glutamatergic systems.
Hyperammonemia resulting from liver damage is considered a major risk factor for the development of brain abnormalities due to alteration of monoaminergic and glutamatergic neurotransmitter systems, overproduction of nitric oxide (NOx), oxidative DNA damage, impaired ATP generation, accompanied by a disruption in cellular energy (Albrecht and Zielińska 2019; Yan et al. 2021; Hadjihambi et al. 2022). Ammonia is a weak base in the body consisting of two molecular forms, NH3 and NH4+, that can readily cross the Blood-brain barrier (BBB) (Vairappan et al. 2019). In hyperammonemia, the over influx of ammonia from the blood to the brain occurs, where it accumulates and acts as a neurotoxin due to prompting a series of neurological abnormalities including bioenergetic failure, oxidative/nitrosative stress, glutamate-mediated neurological death, and cerebral edema (Dasarathy et al. 2017; Oyovwi et al. 2021). In addition, elevated ammonia levels have long been proven to be associated with depletion in serotonin, norepinephrine and dopamine (Albrecht and Wegrzynowicz 2005; Higarza et al. 2019; Baraka et al. 2020).
Dietary protein deficiency and decreased body intake of essential amino acids, especially the branched-chain amino acids (BCAAs), were previously reported to be associated with severe liver damage associated with a disrupted capacity to detoxify ammonia through the urea cycle and consequent elevation in ammonia levels (Katayama 2020). Besides, it was formerly stated that ingestion of a choline-deficient diet resulted in a significant increase in ammonia levels with a high degree of hepatic steatosis and inflammation (Gutiérrez-de-Juan et al. 2017). Similarly, several investigations highlighted that chronic ingestion of methionine-choline deficient diet resulted in a significant elevation in serum ALT and AST along with pronounced hepatic oxidative stress and DNA fragmentation as well as elevation in brain ammonia and NOx levels (Tahan et al. 2009; Amin et al. 2017; Saleh et al. 2017a). In particular, this condition can be very hazardous in pediatrics suffering from malnutrition, hence inadequate protein and amino acids supplementation could eventually lead to the development of hyperammonemia (Häberle 2011; Holecek 2015; Hadjihambi et al. 2018).
Our results revealed that PDD ingestion by juvenile rats led to pronounced status of hyperammonemia both in the liver and brain, along with elevation in the nitrosative stress and oxidative DNA damage, in addition to definite disturbance in the maintenance of cellular energy balance. Serum liver enzymes ALT and AST were increased, indicating hepatic malfunctioning. In addition, serotonin, norepinephrine and dopamine levels were reduced, while the glutamate level was elevated, indicating the possibility of the development of central neuronal excitotoxicity. Correlation studies revealed the existence of a positive correlation between elevated hepatic ammonia levels and brain ammonia levels. Besides, there was a direct correlation between elevated hepatic ammonia levels as well as brain ammonia levels and the elevation in NOx levels, the existence of oxidative DNA damage, and disruption in cellular energy parameters in the corresponding organ. Hepatic ammonia level was also found to correlate with the elevated serum ALT and AST. Furthermore, elevated brain ammonia level was inversely correlated to the brain levels of monoamines. In addition, it could be estimated that PDD-induced hyperammonemia would lead to brain excitotoxicity, as a positive correlation between brain ammonia level and brain glutamate level was detected. Thus, hyperammonemia resulting from PDD would be considered a hazardous risk factor for hepatic as well as cerebral damages.
Current strategies in the management of hyperammonemia aim to decrease ammonia levels and thus target the modulation of the metabolic processes and organs involved in ammonia detoxification, in addition to the down-regulation of oxidative stress (Germoush et al. 2018). Curcumin and resveratrol are two polyphenols that have been extensively studied in the medicinal field as nutraceuticals with documented antioxidant and anti-inflammatory effects, resulting in well-established hepato- and neuro-protective potentials (Malaguarnera et al. 2018; Moore et al. 2018; Khan et al. 2019; Galiniak et al. 2019; Ahmed et al. 2020; Benameur et al. 2021; Miguel et al. 2021; Jabczyk et al. 2021; Chupradit et al. 2022). Unfortunately, both resveratrol and curcumin exhibit low bioavailability and solubility (Liu et al. 2016; Galiniak et al. 2019; Ma et al. 2019; Jabczyk et al. 2021). Pharmaceutical nanotechnology has proven to provide superior drug delivery systems using several techniques, to encapsulate both nutraceuticals in nanoformulations that showed promising results in the management of several hepatic complications as well as neurodegenerative disorders due to enhanced bioavailability (Ganesan et al. 2015; Vasconcelos et al. 2019; Moradi et al. 2020; Grilc et al. 2021; Elbaset et al. 2022).
In the present study, curcumin and resveratrol nanoemulsions significantly ameliorated the adverse effects of PDD-induced hepatic and brain hyperammonemia in juvenile rats, indicating antioxidant potential as well as pronounced hepatoprotective and neuroprotective effects. The high dose level combination of MRCH (5 + 5 mg/kg) exhibited the most promising results regarding the reduction in serum ALT and AST levels, declination in hepatic and brain ammonia levels, reversal of hepatic nitrosative stress as well as oxidative DNA damage, elevation in brain monoamines levels, along with the decrease in glutamate level, and improvement of hepatic and brain cellular energy indices.
Our study is in agreement with previous investigations in which the hepato- and neuroprotective effects of curcumin, either when used in conventional form or nanoformulations, have been extensively investigated, and were generally attributed to antioxidant, anti-inflammatory and DNA preservation potentials (Farzaei et al. 2018; Kheiripour et al. 2021; Nebrisi 2021; Moghaddam et al. 2021). Curcumin consumption in several models of drug-induced hepatotoxicity in rats resulted in decreased serum levels of hepatic enzymes including ALT and AST, declined serum ammonia levels, and hindrance of hepatic oxidative stress (Khan et al. 2019; Frozandeh et al. 2021). Moreover, it was reported that curcumin consumption could ameliorate nicotine-induced oxidative stress in the liver, kidney, spleen and lungs in female rats under protein-restricted diet (Maiti et al. 2015). Similarly, curcumin was found effective in counteracting methionine-choline deficient diet-induced elevation in serum ALT as well as increased hepatic oxidative stress and 8-OHdG, which is a well-known marker of oxidative DNA damage (Leclercq et al. 2004; Vizzutti et al. 2010). In addition, the previous investigation in our laboratory highlighted the beneficial effects of curcumin nanoemulsion in counteracting high-fat, high-fructose (HFHF)-induced hepatic damage represented by the reduction of the elevated serum ALT, AST levels and hepatic MDA, NOx, 8-OHdG levels along with elevation of the declined hepatic GSH level and AEC ratio (Elbaset et al. 2022). Meanwhile, curcumin was also reported to be effective in counteracting cerebral ischemia-induced oxidative stress and glutamate excitotoxicity (Subedi and Gaire 2021) and proved to be effective in inhibiting the expression of monoamine oxidase (MAO-A and MAO-B) enzymes leading to increased levels of norepinephrine, serotonin, and dopamine (Bhat et al. 2019; Matias et al. 2021). In addition, curcumin iron oxide nanoparticles were reported to reduce brain NOx levels and elevate serotonin and dopamine levels in rats’ reserpine model of depression (Khadrawy et al. 2021).
On the other hand, resveratrol exhibited pronounced antioxidant potential in several models, principally via the control of major antioxidant enzymes, and block of DNA damage by free radicals (Pal and Sarkar 2014; Szkudelski and Szkudelska 2018; Meng et al. 2021). Former investigations demonstrated that it could also decrease the level of 8-OHdG, suppress NOx production, and reverse the disruption of energy homeostasis by elevating the production of ATP in cellular mitochondria (Saleh et al. 2017b; Ahmed et al. 2020; Meng et al. 2021; Kim and Song 2021). Furthermore, in-vitro and in-vivo studies delineated the ability of resveratrol to improve liver functions represented by declination in ALT and AST levels, reduction of ammonia levels, maintenance of the blood-brain barrier (BBB) integrity, amelioration of hyperammonemia-induced mitochondrial dysfunction, and disruption in the glutamatergic system and cellular redox imbalance (Bobermin et al. 2015, 2018; Vairappan et al. 2019). Besides, resveratrol was previously reported to partially prevent low protein diet-induced maternal as well as offspring oxidative stress and metabolic dysfunction (Vega et al. 2016). Similarly, it was demonstrated to reduce serum ALT, AST as well as hepatic MDA, and ameliorate methionine-choline deficient diet-induced hepatic steatosis in mice (Ji et al. 2015; Kong et al. 2022). The neuroprotective effect of resveratrol could be attributed to improved liver function and, thus, ammonia metabolism, as well as direct antioxidant and anti-inflammatory potentials both on the liver and brain tissues (Vairappan et al. 2019). In addition, resveratrol was previously reported as a neurotransmitter enhancer (Sarubbo et al. 2015; Gu et al. 2019; Ahmed et al. 2020).
Regarding nanoformulations of resveratrol, it was formerly reported that resveratrol selenium nanoparticles exhibited ameliorative effects against aluminium chloride-induced cerebral dysfunction and cognitive defects and the action was attributed to the antioxidant and anti-inflammatory potentials (Abozaid et al. 2022). Besides, nanostructured lipid carriers containing resveratrol ameliorated oxidative stress and cerebral inflammation following ischemic stroke in rats (Ashafaq et al. 2021). Moreover, resveratrol nanoemulsion prepared by spontaneous emulsification method, followed by high-pressure homogenization using vitamin E:sefsol (1:1) as the oil phase was reported to counteract haloperidol-induced neuronal damage and oxidative stress in brain tissue (Pangeni et al. 2014).
Conclusion
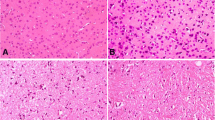
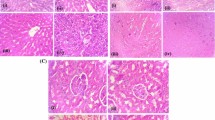
To our knowledge, this is the first report of using a combined resveratrol and curcumin nanoemulsion to counteract PDD-induced hyperammonemia in juvenile rats, and according to the results, it can be delineated that the nanoemulsion was effective in ameliorating both the hepatic and cerebral adverse effects. A limitation of the current study is the absence of tissue histological examinations, which would have provided more insights on the nanoemulsion’s therapeutic effect. Futuristic work will also include the quantification of brain cell death using annexin V assay. Moreover, further investigations are necessary to estimate the effectiveness of this strategy in managing such complications in pediatrics suffering from malnutrition-induced hyperammonemia.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ATP:
-
Adenosine triphosphate
- ADP:
-
Adenosine diphosphate
- AMP:
-
Adenosine monophosphate
- AEC:
-
Adenylate energy charge
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BBB:
-
Blood-brain barrier
- DA:
-
Dopamine levels
- GSH:
-
Glutathione
- MDA:
-
Malondialdehyde
- NOx:
-
Nitric oxide
- iNOS:
-
Nitric oxide synthase
- NE:
-
Norepinephrine
- PDD:
-
Protein-deficient diet
- 5-HT:
-
Serotonin
- 8-OHdG:
-
8-hydroxy-2-deoxyguanosine
References
Abozaid OAR, Sallam MW, El-Sonbaty S et al (2022) Resveratrol-Selenium Nanoparticles alleviate neuroinflammation and neurotoxicity in a rat model of Alzheimer’s disease by regulating Sirt1/miRNA-134/GSK3β expression. https://doi.org/10.1007/s12011-021-03073-7. Biol Trace Elem Res
Aguirre L, Fernández-Quintela A, Arias N, Portillo M (2014) Resveratrol: anti-obesity mechanisms of action. Molecules 19:18632–18655. https://doi.org/10.3390/molecules191118632
Ahmed-Farid OAH, Nasr M, Ahmed RF, Bakeer RM (2017) Beneficial effects of curcumin nano-emulsion on spermatogenesis and reproductive performance in male rats under protein deficient diet model: enhancement of sperm motility, conservancy of testicular tissue integrity, cell energy and seminal plasma amino a. J Biomed Sci 24:66. https://doi.org/10.1186/s12929-017-0373-5
Ahmed RF, El Awdan SA, Abdel Jaleel GA et al (2020) Correlation between brain neurotransmitters and insulin sensitivity: Neuro-preservative role of resveratrol against high fat, high fructose-induced insulin resistance. J Appl Pharm Sci 10:26–36. https://doi.org/10.7324/japs.2020.102005
Al-Shakarchi W, Alsuraifi A, Curtis A, Hoskins C (2018) Dual acting Polymeric Nano-Aggregates for Liver Cancer Therapy. Pharmaceutics 10:63–76. https://doi.org/10.3390/pharmaceutics10020063
Albrecht J, Wegrzynowicz M (2005) Endogenous Neuroprotectants in Ammonia Toxicity in the Central Nervous System: facts and hypotheses. Metab Brain Dis 20:253–263. https://doi.org/10.1007/s11011-005-7904-6
Albrecht J, Zielińska M (2019) Exchange-mode glutamine transport across CNS cell membranes. Neuropharmacology 161:107560. https://doi.org/10.1016/j.neuropharm.2019.03.003
Amin MM, Ahmed RF, Saleh DO (2017) Methionine and Choline Deficient Diet-induced non-alcoholic steatohepatitis in rats: role of Melatonin. J Appl Pharm Sci 7:12–19. https://doi.org/10.7324/JAPS.2017.70902
Ashafaq M, Intakhab Alam M, Khan A et al (2021) Nanoparticles of resveratrol attenuates oxidative stress and inflammation after ischemic stroke in rats. Int Immunopharmacol 94:107494. https://doi.org/10.1016/j.intimp.2021.107494
Atkinson DE, Walton GM (1967) Adenosine triphosphate conservation in metabolic regulation. Rat liver citrate cleavage enzyme. J Biol Chem 242:3239–3241
Baraka SM, Saleh DO, Ghaly NS et al (2020) Flavonoids from Barnebydendron riedelii leaf extract mitigate thioacetamide-induced hepatic encephalopathy in rats: the interplay of NF-κB/IL-6 and Nrf2/HO-1 signaling pathways. Bioorg Chem 105:104444. https://doi.org/10.1016/j.bioorg.2020.104444
Benameur T, Soleti R, Panaro MA et al (2021) Curcumin as prospective anti-aging natural compound: Focus on Brain. Molecules 26:4794. https://doi.org/10.3390/molecules26164794
Bhat A, Mahalakshmi AM, Ray B et al (2019) Benefits of curcumin in brain disorders. BioFactors 45:666–689. https://doi.org/10.1002/biof.1533
Bobermin LD, Hansel G, Scherer EBS et al (2015) Ammonia impairs glutamatergic communication in astroglial cells: protective role of resveratrol. Toxicol Vitr 29:2022–2029. https://doi.org/10.1016/j.tiv.2015.08.008
Bobermin LD, Souza DO, Gonçalves C-A, Quincozes-Santos A (2018) Resveratrol prevents ammonia-induced mitochondrial dysfunction and cellular redox imbalance in C6 astroglial cells. Nutr Neurosci 21:276–285. https://doi.org/10.1080/1028415X.2017.1284375
Boyanapalli SSS, Kong A-NT (2015) “Curcumin, the King of Spices”: Epigenetic Regulatory Mechanisms in the Prevention of Cancer, neurological, and Inflammatory Diseases. Curr Pharmacol reports 1:129–139. https://doi.org/10.1007/s40495-015-0018-x
Cabrera-Pastor A, Arenas YM, Taoro-Gonzalez L et al (2019) Chronic hyperammonemia alters extracellular glutamate, glutamine and GABA and membrane expression of their transporters in rat cerebellum. Modulation by extracellular cGMP. Neuropharmacology 161:107496. https://doi.org/10.1016/j.neuropharm.2019.01.011
Chupradit S, Bokov D, Zamanian MY et al (2022) Hepatoprotective and therapeutic effects of resveratrol: a focus on anti-inflammatory and antioxidative activities. Fundam Clin Pharmacol 36:468–485. https://doi.org/10.1111/fcp.12746
Dasarathy S, Mookerjee RP, Rackayova V et al (2017) Ammonia toxicity: from head to toe? Metab Brain Dis 32:529–538. https://doi.org/10.1007/s11011-016-9938-3
Di Meo F, Margarucci S, Galderisi U et al (2019) Curcumin, Gut Microbiota, and Neuroprotection. https://doi.org/10.3390/nu11102426. Nutrients 11:
Elbaset MA, Nasr M, Ibrahim BMM et al (2022) Curcumin nanoemulsion counteracts hepatic and cardiac complications associated with high-fat/high‐fructose diet in rats. J Food Biochem. https://doi.org/10.1111/jfbc.14442
Farzaei M, Zobeiri M, Parvizi F et al (2018) Curcumin in Liver Diseases: a systematic review of the Cellular Mechanisms of oxidative stress and clinical perspective. Nutrients 10:855. https://doi.org/10.3390/nu10070855
Frozandeh F, Shahrokhi N, Khaksari M et al (2021) Evaluation of the protective effect of curcumin on encephalopathy caused by intrahepatic and extrahepatic damage in male rats. Iran J Basic Med Sci 24:760–766. https://doi.org/10.22038/ijbms.2021.53171.11976
Galiniak S, Aebisher D, Bartusik-Aebisher D (2019) Health benefits of resveratrol administration. Acta Biochim Pol. https://doi.org/10.18388/abp.2018_2749
Ganesan P, Ko H-M, Kim I-S, Choi D-K (2015) Recent trends in the development of nanophytobioactive compounds and delivery systems for their possible role in reducing oxidative stress in Parkinson’s disease models. Int J Nanomedicine 6757. https://doi.org/10.2147/IJN.S93918
Germoush MO, Othman SI, Al-Qaraawi MA et al (2018) Umbelliferone prevents oxidative stress, inflammation and hematological alterations, and modulates glutamate-nitric oxide-cGMP signaling in hyperammonemic rats. Biomed Pharmacother 102:392–402. https://doi.org/10.1016/j.biopha.2018.03.104
Ghorbani Z, Hekmatdoost A, Mirmiran P (2014) Anti-hyperglycemic and insulin Sensitizer Effects of Turmeric and its Principle Constituent Curcumin. Int J Endocrinol Metab 12. https://doi.org/10.5812/ijem.18081
Grilc NK, Sova M, Kristl J (2021) Drug delivery strategies for Curcumin and other Natural Nrf2 modulators of oxidative stress-related Diseases. Pharmaceutics 13:2137. https://doi.org/10.3390/pharmaceutics13122137
Gu Z, Chu L, Han Y (2019) Therapeutic effect of resveratrol on mice with depression. Exp Ther Med. https://doi.org/10.3892/etm.2019.7311
Gutiérrez-de-Juan V, De Davalillo SL, Fernández-Ramos D et al (2017) A morphological method for ammonia detection in liver. PLoS ONE 12:e0173914. https://doi.org/10.1371/journal.pone.0173914
Häberle J (2011) Clinical practice: the management of hyperammonemia. Eur J Pediatr 170:21–34. https://doi.org/10.1007/s00431-010-1369-2
Hadjihambi A, Arias N, Sheikh M, Jalan R (2018) Hepatic encephalopathy: a critical current review. Hepatol Int 12:135–147. https://doi.org/10.1007/s12072-017-9812-3
Hadjihambi A, Cudalbu C, Pierzchala K et al (2022) Abnormal brain oxygen homeostasis in an animal model of liver disease. JHEP Rep 4:100509. https://doi.org/10.1016/j.jhepr.2022.100509
Higarza SG, Arboleya S, Gueimonde M et al (2019) Neurobehavioral dysfunction in non-alcoholic steatohepatitis is associated with hyperammonemia, gut dysbiosis, and metabolic and functional brain regional deficits. PLoS ONE 14:e0223019. https://doi.org/10.1371/journal.pone.0223019
Holecek M (2015) Ammonia and amino acid profiles in liver cirrhosis: Effects of variables leading to hepatic encephalopathy. Nutrition 31:14–20. https://doi.org/10.1016/j.nut.2014.03.016
Huang WC, Chiu WC, Chuang HL et al (2015) Effect of curcumin supplementation on physiological fatigue and physical performance in mice. Nutrients 7:905–921. https://doi.org/10.3390/nu7020905
Jabczyk M, Nowak J, Hudzik B, Zubelewicz-Szkodzińska B (2021) Curcumin in Metabolic Health and Disease. Nutrients 13:4440. https://doi.org/10.3390/nu13124440
Ji G, Wang Y, Deng Y et al (2015) Resveratrol ameliorates hepatic steatosis and inflammation in methionine/choline-deficient diet-induced steatohepatitis through regulating autophagy. Lipids Health Dis 14:134. https://doi.org/10.1186/s12944-015-0139-6
Katayama K (2020) Zinc and protein metabolism in chronic liver diseases. Nutr Res 74:1–9. https://doi.org/10.1016/j.nutres.2019.11.009
Kawai H, Ishibashi T, Kudo N et al (2012) Behavioral and biochemical characterization of rats treated chronically with thioacetamide: proposal of an animal model for hepatic encephalopathy associated with cirrhosis. J Toxicol Sci 37:1165–1175. https://doi.org/10.2131/jts.37.1165
Khadrawy YA, Hosny EN, Magdy M, Mohammed HS (2021) Antidepressant effects of curcumin-coated iron oxide nanoparticles in a rat model of depression. Eur J Pharmacol 908:174384. https://doi.org/10.1016/j.ejphar.2021.174384
Khan H, Ullah H, Nabavi SM (2019) Mechanistic insights of hepatoprotective effects of curcumin: therapeutic updates and future prospects. Food Chem Toxicol 124:182–191. https://doi.org/10.1016/j.fct.2018.12.002
Kheiripour N, Plarak A, Heshmati A et al (2021) Evaluation of the hepatoprotective effects of curcumin and nanocurcumin against paraquat-induced liver injury in rats: modulation of oxidative stress and Nrf2 pathway. J Biochem Mol Toxicol 35. https://doi.org/10.1002/jbt.22739
Kim Y-K, Song J (2021) Therapeutic applications of resveratrol in hepatic encephalopathy through its regulation of the Microbiota, Brain Edema, and inflammation. J Clin Med 10:3819. https://doi.org/10.3390/jcm10173819
Kong L, An X, Hu L et al (2022) Resveratrol ameliorates nutritional steatohepatitis through the mmu–miR–599/PXR pathway. Int J Mol Med 49:47. https://doi.org/10.3892/ijmm.2022.5102
Leclercq IA, Farrell GC, Sempoux C et al (2004) Curcumin inhibits NF-κB activation and reduces the severity of experimental steatohepatitis in mice. J Hepatol 41:926–934. https://doi.org/10.1016/j.jhep.2004.08.010
Liu W, Zhai Y, Heng X et al (2016) Oral bioavailability of curcumin: problems and advancements. J Drug Target 24:694–702. https://doi.org/10.3109/1061186X.2016.1157883
Lodovici M, Casalini C, Briani C, Dolara P (1997) Oxidative liver DNA damage in rats treated with pesticide mixtures. Toxicology 117:55–60
Ma Z, Wang N, He H, Tang X (2019) Pharmaceutical strategies of improving oral systemic bioavailability of curcumin for clinical application. J Control Release 316:359–380. https://doi.org/10.1016/j.jconrel.2019.10.053
Maiti M, Chattopadhyay K, Verma M, Chattopadhyay B (2015) Curcumin protects against nicotine-induced stress during protein malnutrition in female rat through immunomodulation with cellular amelioration. Mol Biol Rep 42:1623–1637. https://doi.org/10.1007/s11033-015-3929-z
Malaguarnera G, Pennisi M, Bertino G et al (2018) Resveratrol in patients with minimal hepatic encephalopathy. Nutrients 10:329. https://doi.org/10.3390/nu10030329
Martínez-Abundis E, Mendez-del Villar M, Pérez-Rubio KG et al (2016) Novel nutraceutic therapies for the treatment of metabolic syndrome. World J Diabetes 7:142. https://doi.org/10.4239/wjd.v7.i7.142
Matias JN, Achete G, Campanari GS dos S, et al (2021) A systematic review of the antidepressant effects of curcumin: beyond monoamines theory. Aust New Zeal J Psychiatry 55:451–462. https://doi.org/10.1177/0004867421998795
Meng T, Xiao D, Muhammed A et al (2021) Anti-inflammatory action and mechanisms of Resveratrol. Molecules 26:229. https://doi.org/10.3390/molecules26010229
Miguel CA, Noya-Riobó MV, Mazzone GL et al (2021) Antioxidant, anti-inflammatory and neuroprotective actions of resveratrol after experimental nervous system insults. Special focus on the molecular mechanisms involved. Neurochem Int 150:105188. https://doi.org/10.1016/j.neuint.2021.105188
Moghaddam AH, Maboudi K, Bavaghar B et al (2021) Neuroprotective effects of curcumin-loaded nanophytosome on ketamine-induced schizophrenia-like behaviors and oxidative damage in male mice. Neurosci Lett 765:136249. https://doi.org/10.1016/j.neulet.2021.136249
Moore A, Beidler J, Hong M (2018) Resveratrol and Depression in Animal Models: a systematic review of the Biological Mechanisms. Molecules 23:2197. https://doi.org/10.3390/molecules23092197
Moradi SZ, Momtaz S, Bayrami Z et al (2020) Nanoformulations of herbal extracts in treatment of neurodegenerative Disorders. Front Bioeng Biotechnol 8. https://doi.org/10.3389/fbioe.2020.00238
Nasr M (2016) Development of an optimized hyaluronic acid-based lipidic nanoemulsion co-encapsulating two polyphenols for nose to brain delivery. Drug Deliv 23:1444–1452. https://doi.org/10.3109/10717544.2015.1092619
Nebrisi EE (2021) Neuroprotective activities of Curcumin in Parkinson’s disease: a review of the literature. Int J Mol Sci 22:11248. https://doi.org/10.3390/ijms222011248
Ochoa-Sanchez R, Rose CF (2018) Pathogenesis of hepatic Encephalopathy in Chronic Liver Disease. J Clin Exp Hepatol 8:262–271. https://doi.org/10.1016/j.jceh.2018.08.001
Oyovwi MO, Ben-Azu B, Tesi EP et al (2021) Repeated endosulfan exposure induces changes in neurochemicals, decreases ATPase transmembrane ionic-pumps, and increased oxidative/nitrosative stress in the brains of rats: reversal by quercetin. Pestic Biochem Physiol 175:104833. https://doi.org/10.1016/j.pestbp.2021.104833
Pagel P, Blome J, Wolf HU (2000) High-performance liquid chromatographic separation and measurement of various biogenic compounds possibly involved in the pathomechanism of Parkinson’s disease. J Chromatogr B Biomed Sci Appl 746:297–304
Pal S, Sarkar C (2014) Protective effect of resveratrol on fluoride induced alteration in protein and nucleic acid metabolism, DNA damage and biogenic amines in rat brain. Environ Toxicol Pharmacol 38:684–699. https://doi.org/10.1016/j.etap.2014.07.009
Pangeni R, Sharma S, Mustafa G et al (2014) Vitamin E loaded resveratrol nanoemulsion for brain targeting for the treatment of Parkinson’s disease by reducing oxidative stress. Nanotechnology 25:485102. https://doi.org/10.1088/0957-4484/25/48/485102
Papadoyannis IN, Samanidou VF, Nitsos CC (1999) Simultaneous determination of nitrite and nitrate in drinking water and human serum by high performance anion-exchange chromatography and uv detection. J Liq Chromatogr Relat Technol 22:2023–2041. https://doi.org/10.1081/JLC-100101783
Quincozes-Santos A, Bobermin LD, Tramontina AC et al (2014) Oxidative stress mediated by NMDA, AMPA/KA channels in acute hippocampal slices: neuroprotective effect of resveratrol. Toxicol Vitr 28:544–551. https://doi.org/10.1016/j.tiv.2013.12.021
Reitman S, Frankel S (1957) A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am J Clin Pathol 28:56–63
Ronan PJ, Gaikowski MP, Hamilton SJ et al (2007) Ammonia causes decreased brain monoamines in fathead minnows (Pimephales promelas). Brain Res 1147:184–191. https://doi.org/10.1016/j.brainres.2007.02.015
Saleh DO, Ahmed RF, Amin MM (2017a) Modulatory role of co-enzyme Q10 on methionine and choline deficient diet-induced non-alcoholic steatohepatitis (NASH) in albino rats. Appl Physiol Nutr Metab 42:243–249. https://doi.org/10.1139/apnm-2016-0320
Saleh DO, El Awdan SA, Jaleel GAA, Ahmed RF (2017b) Resveratrol attenuates hepatic complications associated with insulin resistance: implications on hepatic HAIR, LAIR, cell energy and DNA fragmentation. J Appl Pharm Sci 7:020–027. https://doi.org/10.7324/JAPS.2017.70804
Sarubbo F, Ramis MR, Aparicio S et al (2015) Improving effect of chronic resveratrol treatment on central monoamine synthesis and cognition in aged rats. Age (Omaha) 37:37. https://doi.org/10.1007/s11357-015-9777-x
Singh S, Mondal P, Trigun SK (2014) Acute liver failure in rats activates glutamine-glutamate cycle but declines antioxidant enzymes to induce oxidative stress in cerebral cortex and cerebellum. PLoS ONE 9. https://doi.org/10.1371/journal.pone.0095855
Subedi L, Gaire BP (2021) Neuroprotective Effects of Curcumin in Cerebral Ischemia: Cellular and Molecular Mechanisms. ACS Chem Neurosci 12:2562–2572. https://doi.org/10.1021/acschemneuro.1c00153
Szkudelski T, Szkudelska K (2018) Potential of resveratrol in mitigating metabolic disturbances induced by ethanol. Biomed Pharmacother 101:579–584. https://doi.org/10.1016/j.biopha.2018.02.063
Tahan V, Atug O, Akin H et al (2009) Melatonin ameliorates methionine- and choline-deficient diet-induced nonalcoholic steatohepatitis in rats. J Pineal Res 46:401–407. https://doi.org/10.1111/j.1600-079X.2009.00676.x
Teerlink T, Hennekes M, Bussemaker J, Groeneveld J (1993) Simultaneous determination of creatine compounds and adenine nucleotides in myocardial tissue by high-performance liquid chromatography. Anal Biochem 214:278–283. https://doi.org/10.1006/abio.1993.1488
Vairappan B, Sundhar M, Srinivas BH (2019) Resveratrol restores neuronal tight Junction Proteins through correction of Ammonia and inflammation in CCl4-Induced Cirrhotic mice. Mol Neurobiol 56:4718–4729. https://doi.org/10.1007/s12035-018-1389-x
Vasconcelos T, Araújo F, Lopes C et al (2019) Multicomponent self nano emulsifying delivery systems of resveratrol with enhanced pharmacokinetics profile. Eur J Pharm Sci 137:105011. https://doi.org/10.1016/j.ejps.2019.105011
Vega CC, Reyes-Castro LA, Rodríguez-González GL et al (2016) Resveratrol partially prevents oxidative stress and metabolic dysfunction in pregnant rats fed a low protein diet and their offspring. J Physiol 594:1483–1499. https://doi.org/10.1113/JP271543
Vizzutti F, Provenzano A, Galastri S et al (2010) Curcumin limits the fibrogenic evolution of experimental steatohepatitis. Lab Investig 90:104–115. https://doi.org/10.1038/labinvest.2009.112
Yan T, Li F, Xiong W et al (2021) Nootkatone improves anxiety- and depression‐like behavior by targeting hyperammonemia‐induced oxidative stress in D‐galactosamine model of liver injury. Environ Toxicol 36:694–706. https://doi.org/10.1002/tox.23073
Yavarpour-Bali H, Ghasemi-Kasman M, Pirzadeh M (2019) Curcumin-loaded nanoparticles: a novel therapeutic strategy in treatment of central nervous system disorders. Int J Nanomedicine 14:4449–4460. https://doi.org/10.2147/ijn.s208332
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Nanoemulsions preparations were performed by Prof. Dr. Maha Nasr. Pharmacological study was performed by Ass. Prof. Dr. Rania F. Ahmed, biological analyses were performed by Ass. Prof. Dr. Rania F. Ahmed and Ass. Prof. Dr. Omar A.H. Ahmed-Farid. The first draft of the manuscript was written by Prof. Dr. Maha Nasr, Ass. Prof. Dr. Rania F. Ahmed and Ass. Prof. Dr. Omar A.H. Ahmed-Farid. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
All experimental procedures followed the regulations of the Research Ethics Committee of the National Research Centre (approval number 2415062022) in accordance with relevant national guidelines and regulations and compliance with the ARRIVE guidelines.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nasr, M., Ahmed-farid, O.A. & Ahmed, R.F. Curcumin-resveratrol nano-formulation counteracting hyperammonemia in rats. Metab Brain Dis 38, 1365–1377 (2023). https://doi.org/10.1007/s11011-023-01162-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-023-01162-1