Abstract
One in 700 children is born with the down syndrome (DS). In DS, there is an extra copy of X chromosome 21 (trisomy). Interestingly, the chromosome 21 also contains an extra copy of the cystathionine beta synthase (CBS) gene. The CBS activity is known to contribute in mitochondrial sulfur metabolism via trans-sulfuration pathway. We hypothesize that due to an extra copy of the CBS gene there is hyper trans-sulfuration in DS. We believe that understanding the mechanism of hyper trans-sulfuration during DS will be important in improving the quality of DS patients and towards developing new treatment strategies. We know that folic acid “1-carbon” metabolism (FOCM) cycle transfers the “1-carbon” methyl group to DNA (H3K4) via conversion of s-adenosyl methionine (SAM) to s-adenosyl homocysteine (SAH) by DNMTs (the gene writers). The demethylation reaction is carried out by ten-eleven translocation methylcytosine dioxygenases (TETs; the gene erasers) through epigenetics thus turning the genes off/on and opening the chromatin by altering the acetylation/HDAC ratio. The S-adenosyl homocysteine hydrolase (SAHH) hydrolyzes SAH to homocysteine (Hcy) and adenosine. The Hcy is converted to cystathionine, cysteine and hydrogen sulfide (H2S) via CBS/cystathioneγ lyase (CSE)/3-mercaptopyruvate sulfurtransferase (3MST) pathways. Adenosine by deaminase is converted to inosine and then to uric acid. All these molecules remain high in DS patients. H2S is a potent inhibitor of mitochondrial complexes I-IV, and regulated by UCP1. Therefore, decreased UCP1 levels and ATP production can ensue in DS subjects. Interestingly, children born with DS show elevated levels of CBS/CSE/3MST/Superoxide dismutase (SOD)/cystathionine/cysteine/H2S. We opine that increased levels of epigenetic gene writers (DNMTs) and decreased in gene erasers (TETs) activity cause folic acid exhaustion, leading to an increase in trans-sulphuration by CBS/CSE/3MST/SOD pathways. Thus, it is important to determine whether SIRT3 (inhibitor of HDAC3) can decrease the trans-sulfuration activity in DS patients. Since there is an increase in H3K4 and HDAC3 via epigenetics in DS, we propose that sirtuin-3 (Sirt3) may decrease H3K4 and HDAC3 and hence may be able to decrease the trans-sulfuration in DS. It would be worth to determine whether the lactobacillus, a folic acid producing probiotic, mitigates hyper-trans-sulphuration pathway in DS subjects. Further, as we know that in DS patients the folic acid is exhausted due to increase in CBS, Hcy and re-methylation. In this context, we suggest that folic acid producing probiotics such as lactobacillus might be able to improve re-methylation process and hence may help decrease the trans-sulfuration pathway in the DS patients.

Similar content being viewed by others
Data availability
Enquiries about data availability should be directed to the authors.
Abbreviations
- ADA:
-
Adenosine deaminase
- CBS:
-
Cystathionine beta synthase
- CSE:
-
Cystathionine gamma lyase
- DNMT:
-
DNA methyl transferase
- DS:
-
Down syndrome
- H3K4:
-
Histone 3 lysine 4
- Hcy:
-
Homocysteine
- H2S:
-
Hydrogen sulfide
- HDAC:
-
Histone de-acetylase
- SAM:
-
S-adenosyl methionine
- MTHFRS:
-
Methyl tetrahydro folate reductase synthase
- SAH:
-
S-adenosyl homocysteine
- SAHH:
-
S-adenosyl homocysteine hydrolase
- 3MST:
-
3-Mercaptosulphurtranferase
- SOD:
-
Super oxide dismutase
- TET:
-
Ten eleven translocators
- UCP1:
-
Mitochondrial uncoupling protein1
References
Zuhra K, Augsburger F, Majtan T, Szabo C (2020) Cystathionine-β-Synthase: molecular regulation and pharmacological inhibition. Biomolecules. https://doi.org/10.3390/biom10050697
George AK, Majumder A, Ice H, Homme RP, Eyob W, Tyagi SC, Singh M (2020) Genes and genetics in hyperhomocysteinemia and the “1-carbon metabolism”: implications for retinal structure and eye functions. Can J Physiol Pharmacol 98:51–60. https://doi.org/10.1139/cjpp-2019-0236
George AK, Master K, Majumder A, Homme RP, Laha A, Sandhu HS, Tyagi SC, Singh M (2019) Circular RNAs constitute an inherent gene regulatory axis in the mammalian eye and brain (1). Can J Physiol Pharmacol 97:463–472. https://doi.org/10.1139/cjpp-2018-0505
Singh M, George AK, Homme RP, Majumder A, Laha A, Sandhu HS, Tyagi SC (2019) Expression analysis of the circular RNA molecules in the human retinal cells treated with homocysteine. Curr Eye Res 44:287–293. https://doi.org/10.1080/02713683.2018.1542005
Singh M, Tyagi SC (2017) Homocysteine mediates transcriptional changes of the inflammatory pathway signature genes in human retinal pigment epithelial cells. Int J Ophthalmol 10:696–704. https://doi.org/10.18240/ijo.2017.05.06
Singh M, George AK, Homme RP, Majumder A, Laha A, Sandhu HS, Tyagi SC (2018) Circular RNAs profiling in the cystathionine-β-synthase mutant mouse reveals novel gene targets for hyperhomocysteinemia induced ocular disorders. Exp Eye Res 174:80–92. https://doi.org/10.1016/j.exer.2018.05.026
Tran SK, Ngo TH, Nguyen PH, Truong AB, Truong GK, Tran KDD, Vo PM, Nguyen PT, Nguyen TT, Nguyen PNT, Nguyen KT, Tran HD (2023) Hyperhomocysteinemia in patients with newly diagnosed primary hypertension in can tho city vietnam. Healthcare (Basel). https://doi.org/10.3390/healthcare11020234
Yuan D, Chu J, Lin H, Zhu G, Qian J, Yu Y, Yao T, Ping F, Chen F, Liu X (2022) Mechanism of homocysteine-mediated endothelial injury and its consequences for atherosclerosis. Front Cardiovasc Med 9:1109445. https://doi.org/10.3389/fcvm.2022.1109445
Zhang L, Xu R, Ma X, Zhang X, Gong J, Li Z (2023) Mechanism of arterial injury exacerbated by hyperhomocysteinemia in spontaneously hypertensive rats. Sci Rep 13:2482. https://doi.org/10.1038/s41598-023-28731-9
Choi JH, Seo JW, Lee MY, Lee YT, Yoon KJ, Park CH (2022) Association between elevated plasma homocysteine and low skeletal muscle mass in asymptomatic adults. Endocrinol Metab (Seoul) 37:333–343. https://doi.org/10.3803/EnM.2021.1202
Griñán R, Escolà-Gil JC, Julve J, Benítez S, Rotllan N (2022) Epigenetic regulation by microRNAs in hyperhomocysteinemia-accelerated atherosclerosis. Int J Mol Sci. https://doi.org/10.3390/ijms232012452
Mi J, Chen X, Yiran Y, Tang Y, Liu Q, Xiao J, Ling W (2022) S-adenosylhomocysteine induces cellular senescence in rat aorta vascular smooth muscle cells via NF-κB-SASP pathway. J Nutr Biochem 107:109063. https://doi.org/10.1016/j.jnutbio.2022.109063
Singh M, Pushpakumar S, Zheng Y, Homme RP, Smolenkova I, Mokshagundam SPL, Tyagi SC (2022) Hydrogen sulfide mitigates skeletal muscle mitophagy-led tissue remodeling via epigenetic regulation of the gene writer and eraser function. Physiol Rep 10:e15422. https://doi.org/10.14814/phy2.15422
Yoo TK, Rhim HC, Lee YT, Yoon KJ, Park CH (2022) Relationship between hyperhomocysteinemia and coexisting obesity with low skeletal muscle mass in asymptomatic adult population. Sci Rep 12:12439. https://doi.org/10.1038/s41598-022-16401-1
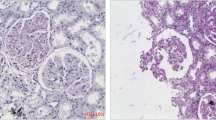
Niamien-Attai C, Bacchetta J, Ranchin B, Sanlaville D, Cochat P (2017) Renal abnormalities in down syndrome: a review. Arch Pediatr 24:1013–1018. https://doi.org/10.1016/j.arcped.2017.07.014
Málaga S, Pardo R, Málaga I, Orejas G, Fernández-Toral J (2005) Renal involvement in down syndrome. Pediatr Nephrol 20:614–617. https://doi.org/10.1007/s00467-005-1825-9
Nishida Y, Akaoka I, Kobayashi M, Maruki K, Oshima Y (1979) Renal impairment in urate excretion in patients with Down’s syndrome. J Rheumatol 6:103–107
Tanaka Y, Shibata R, Sakamoto K (1993) A case of Down syndrome with chronic renal failure caused by long-term asymptomatic hyperuricemia. No To Hattatsu 25:364–368
Teng H, Wu B, Zhao K, Yang G, Wu L, Wang R (2013) Oxygen-sensitive mitochondrial accumulation of cystathionine β-synthase mediated by Lon protease. Proc Natl Acad Sci U S A 110:12679–12684. https://doi.org/10.1073/pnas.1308487110
Szabo C, Ransy C, Módis K, Andriamihaja M, Murghes B, Coletta C, Olah G, Yanagi K, Bouillaud F (2014) Regulation of mitochondrial bioenergetic function by hydrogen sulfide. Part I. Biochemical and physiological mechanisms. Br J Pharmacol 171:2099–2122. https://doi.org/10.1111/bph.12369
Panagaki T, Randi EB, Augsburger F, Szabo C (2019) Overproduction of H(2)S, generated by CBS, inhibits mitochondrial Complex IV and suppresses oxidative phosphorylation in Down syndrome. Proc Natl Acad Sci U S A 116:18769–18771. https://doi.org/10.1073/pnas.1911895116
Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, Lupo PJ, Riehle-Colarusso T, Cho SJ, Aggarwal D, Kirby RS (2019) National population-based estimates for major birth defects, 2010–2014. Birth Defects Res 111:1420–1435. https://doi.org/10.1002/bdr2.1589
Liehr T (2019) From human cytogenetics to human chromosomics. Int J Mol Sci. https://doi.org/10.3390/ijms20040826
Kamalakar A, Harris JR, McKelvey KD, Suva LJ (2014) Aneuploidy and skeletal health. Curr Osteoporos Rep 12:376–382. https://doi.org/10.1007/s11914-014-0221-4
Sotonica M, Mackic-Djurovic M, Hasic S, Kiseljakovic E, Jadric R, Ibrulj S (2016) Association of parental age and the type of down syndrome on the territory of bosnia and herzegovina. Med Arch 70:88–91. https://doi.org/10.5455/medarh.2016.70.88-91
Pogribna M, Melnyk S, Pogribny I, Chango A, Yi P, James SJ (2001) Homocysteine metabolism in children with down syndrome: in vitro modulation. Am J Hum Genet 69:88–95. https://doi.org/10.1086/321262
Panagaki T, Randi EB, Szabo C (2020) Role of 3-mercaptopyruvate sulfurtransferase in the regulation of proliferation and cellular bioenergetics in human down syndrome fibroblasts. Biomolecules. https://doi.org/10.3390/biom10040653
Dimopoulos K, Constantine A, Clift P, Condliffe R, Moledina S, Jansen K, Inuzuka R, Veldtman GR, Cua CL, Tay ELW, Opotowsky AR, Giannakoulas G, Alonso-Gonzalez R, Cordina R, Capone G, Namuyonga J, Scott CH, D’Alto M, Gamero FJ, Chicoine B, Gu H, Limsuwan A, Majekodunmi T, Budts W, Coghlan G, Broberg CS (2023) Cardiovascular complications of down syndrome: scoping review and expert consensus. Circulation 147:425–441. https://doi.org/10.1161/circulationaha.122.059706
Postolache L, Parsa A, Simoni P, Boitsios G, Ismaili K, Schurmans T, Monier A, Casimir G, Albert A, Parsa CF (2022) Widespread kidney anomalies in children with Down syndrome. Pediatr Nephrol 37:2361–2368. https://doi.org/10.1007/s00467-022-05455-y
George AK, Homme RP, Majumder A, Laha A, Metreveli N, Sandhu HS, Tyagi SC, Singh M (2019) Hydrogen sulfide intervention in cystathionine-β-synthase mutant mouse helps restore ocular homeostasis. Int J Ophthalmol 12:754–764. https://doi.org/10.18240/ijo.2019.05.09
George AK, Homme RP, Stanisic D, Tyagi SC, Singh M (2021) Protecting the aging eye with hydrogen sulfide. Can J Physiol Pharmacol 99:161–170. https://doi.org/10.1139/cjpp-2020-0216
Singh M, Hardin SJ, George AK, Eyob W, Stanisic D, Pushpakumar S, Tyagi SC (2020) Epigenetics, 1-Carbon metabolism, and homocysteine during dysbiosis. Front Physiol 11:617953. https://doi.org/10.3389/fphys.2020.617953
Stoll C, Dott B, Alembik Y, Roth MP (2015) Associated congenital anomalies among cases with down syndrome. Eur J Med Genet 58:674–680. https://doi.org/10.1016/j.ejmg.2015.11.003
Tsiouplis NJ, Bailey DW, Chiou LF, Wissink FJ, Tsagaratou A (2020) TET-mediated Epigenetic regulation in immune cell development and disease. Front Cell Dev Biol 8:623948. https://doi.org/10.3389/fcell.2020.623948
Bogdanović O, Lister R (2017) DNA methylation and the preservation of cell identity. Curr Opin Genet Dev 46:9–14. https://doi.org/10.1016/j.gde.2017.06.007
Duchon A, Moreno DMM, M Chevalier C Nalesso V Andre P Fructuoso-Castellar M Mondino M Po C Noblet V Birling MC Potier MC and Herault Y (2022) Ts66Yah, a mouse model of Down syndrome with improved construct and face validity. Dis Model Mech. https://doi.org/10.1242/dmm.049721
Antonarakis SE, Epstein CJ (2006) The challenge of down syndrome. Trends Mol Med 12:473–479. https://doi.org/10.1016/j.molmed.2006.08.005
Roper RJ, Goodlett CR (2022) A new down syndrome rat model races forward. Trends Genet 38:1101–1102. https://doi.org/10.1016/j.tig.2022.05.001
Acknowledgements
The authors would like to thank all members of the laboratory for their continued help, and excellent support. Part of this study was supported by NIH grants AR-71789, HL139047, and DK116591.
Funding
The study was partly supported by NIH grants (HL-139047, DK116591 and AR-71789).
Author information
Authors and Affiliations
Contributions
S.P. collected relevant literature, M.S. conceived, wrote and finalized the manuscript, U.S, N.T, and S.C.T helped in reviewing the contents.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pushpakumar, S., Singh, M., Sen, U. et al. The role of the mitochondrial trans-sulfuration in cerebro-cardio renal dysfunction during trisomy down syndrome. Mol Cell Biochem 479, 825–829 (2024). https://doi.org/10.1007/s11010-023-04761-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-023-04761-9