Abstract
Increased CD44 antigen activity has been reported in recurrent cases of UBC. To date, no reliable biomarker is available with high significance and specificity for non-invasive detection of UBC. This study aimed to identify a CD44-linked microRNAs (miRNAs) (miR-9, miR-34a, miR-203) for non-invasive diagnosis of bladder cancer from other urinary tract malignancies. The expression of CD44-linked miRNAs was examined in serum, urine, and tissue specimens of Indian UBC patients (N = 25). For this purpose, healthy subjects (N = 25) and benign prostatic hyperplasia (BPH) (N = 10) patients were taken as controls. The relative expression of miRNAs was analyzed in serum, urine, and tissue samples using real-time quantitative reverse transcription PCR (qRT-PCR). The diagnostic potential of these miRNAs was accessed by plotting ROC curve. Increased miR-9 expression was observed in serum of UBC patients than healthy and BPH controls. In UBC patients, miR-34a expression was lower than healthy controls but non-significant as compared to BPH. miR-203 expression was considerably higher in serum of UBC patients but non-significant as compared to BPH controls. miR-203 was found to be considerably higher in urine samples from UBC patients as compared to BPH and healthy controls. The diagnostic potential of these miRNAs was evaluated using the ROC curve. Higher miR-203 levels in the urine of Indian UBC patients demonstrate its non-invasive diagnostic ability out of the three miRNAs studied. Our results characterize the non-invasive diagnostic potential of CD44-linked miR-203 in the urine of Indian UBC patients, which could be utilized in clinical settings in future after validation in larger patient cohort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary bladder cancer (UBC) is the tenth most prevalent type of urogenital malignancy worldwide. In 2020, there were an estimated 573,278 new cases and 212,536 deaths recorded globally [1]. Urothelial carcinoma, also called transitional cell carcinoma (TCC), is the predominant histological type of UBC. It is mainly classified into two types, viz non-muscle-invasive (NMIBC) and muscle-invasive bladder cancer (MIBC) [2]. The largest cases of UBC are diagnosed at the NMIBC stage. Patients with NMIBC have minimal risk of tumor-related death besides a very high recurrence rate (more than 75% of patients recur within five years) [3]. About 10–30% of NMIBC advances to MIBC with a reduced survival rate and frequent distant metastasis. The prevalence of UBC is four times greater in men than in women [4]. Environmental or occupational exposure to carcinogens, including tobacco and azo dyes in textile industries, are the critical risk factors for UBC. Most cases of UBC are detected in people over the age of 60 [5].
The most common symptom of UBC is either macroscopic or microscopic haematuria. Currently, UBC diagnosis involves cystoscopy and biopsy, which are obnoxious and expensive procedures [6]. The stage of bladder cancer diagnosis has not changed over the past ten years due to a lack of effective screening. Several FDA-approved urine-based tests (e.g., NMP22, NMP22 BladderChek, UroVysion, BTA-TRAK, and BTA-STAT ) for UBC diagnosis and monitoring are commercially available [7]. However, the sensitivity, specificity, and diagnostic efficacy of these urine-based assays are still sub-optimal; therefore, new molecular markers or assays must be translated into the clinics. Our lab has been working in the area of UBC for the past two decades, and the diagnostic potential of certain molecules has also been assessed in UBC [8, 9]. The use of minimally invasive “liquid biopsies” for the classification and characterization of urogenital malignancies is advancing rapidly [10]. Tumor cells release cell-free DNA, RNA (including mRNAs, miRNA and long non-coding RNA), peptides, and proteins, which confer potential as a promising biomarker [11].
Extra-cellular matrix components play an important in cancer progression, and for the better understanding of cell-to-cell contact in tumor conditions, studies are now focusing culturing cancer cell on extracellular matrix (ECM)-coated plates [12]. Hyaluronic acid is one of the important ECM proteins where CD44 serves as a receptor for hyaluronic acid (HA, non-sulfated glycosaminoglycan). Our group had previously reported the importance of CD44 and its multiple variants along with HAS (hyaluronic acid synthase) in pathogenesis of UBC [13]. HA-activated CD44 favors tumor cell survival, metastasis, and chemoresistance via activation of diverse cellular pathways, including PI3K-Akt, RAS-MAP, JAK-STAT, etc. [14, 15]. miRNAs are small (18–22 nucleotide long), non-coding RNAs that regulate gene expression at the transcription and translation level. The sequence-specific pairing of miRNAs with the 3'-untranslated region (UTR) of the target mRNAs results in its degradation or translation suppression [16]. Deregulated miRNA expression has been spotted in many tumors and is associated with invasion, migration, and epithelial-mesenchymal transition (EMT) [17]–[19]. Our group has also reported the diagnostic significance of circulatory microRNAs in renal cell carcinoma (RCC) and multiple myeloma [20, 21].
CD44-associated miRNAs include miR-9, miR-21, miR-34a, miR-130, miR-143, miR-199, and miR-203 [22]–[24]. miRNAs are broadly classified into oncogenic (oncomiR) and tumor-suppressive (Anti-oncomiR) miRNAs. In bladder cancer, upregulated expression of miR-9 and downregulated expression of miR-34a and miR-203 have been reported [25]–[27]. Most of these studies were conducted in vitro using cell lines. Very limited reports are available on human specimens.
In this study, we investigated the differential expression of CD44-linked miRNAs comprising miR-9, miR-34a, and miR-203 in serum, urine, and tissue specimens of UBC patients in the Indian population. Moreover, the non-invasive diagnostic potential of these miRNAs was estimated by plotting the ROC curve. Out of all three miRNAs, miR-203 showed the non-invasive diagnostic potential in urine specimen of Indian UBC patient which requires further validation in larger cohorts.
Materials and methods
Study samples
The study was authorized by Institute's Ethics Committee (IEC No.: IEC-532/02.08.2019, RP-23/2019), and written consent was received from all patients and healthy subjects (N = 25). Histopathologically confirmed BPH (N = 10) and UBC (N = 25) patients were involved in the study. Patients and healthy subjects having urinary tract infections (UTIs) and other malignancy were excluded. Blood and urine specimens were collected from healthy subjects. Blood, urine, and tumor tissue specimens were collected from BPH controls. Blood, urine, tumor tissue, and adjacent healthy tissue specimens were collected from UBC patients. Total 3 mL of venous blood and 5 mL urine were collected from all the participants. Tumor and adjacent healthy tissues were collected from the same UBC patients during surgery.
Total RNA extraction and reverse transcription of microRNA
Blood was collected in serum separator tubes (SST) (BD Vacutainer®) to isolate serum. Total RNA was isolated as per manufacturer's protocol from serum and urine using miRNeasy Serum/Plasma kit (Qiagen; Catalog No. 217184) while miRNeasy minikit (Qiagen; Catalog No. 217004) was used for tissue specimens. cel-miR-39a was used as spike-in control for serum and urine samples (miRCURY LNA RT kit, Qiagen; Catalog No. 339340). RNA was quantified using Nanodrop™ spectrophotometer (ThermoFisher, USA). For reverse transcription, 1 μg of purified RNA was utilized to synthesize cDNA using miScript II RT kit (Qiagen; Catalog No. 218160) as per the manufacturer's protocol.
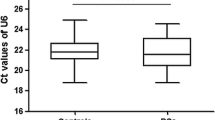
Quantitative microRNA expression by real-time PCR
The cDNA was diluted in 1:9 ratio using nuclease-free water (NFW) supplied in the miScript II RT Kit. The diluted cDNA was amplified using miRNA-specific primers (purchased from Qiagen) and miScript SYBR® Green PCR Kit (Qiagen; Catalog No. 218073) as per the manufacturer's protocol. Relative expression of miRNAs was analyzed using Bio-Rad CFX96 real-time PCR machine. Cel-miR-39a primer was used as an internal control in serum and urine, while SNORD48 was used to normalize relative expression in tissue samples.
Receiver operating characteristic (ROC) curve
ROC curve was plotted to access the diagnostic potential of these circulatory miRNAs between the true-positive rate against the false-positive rate for the different possible cut-points of quantitative miRNA expression results to define the optimal cut-off values with maximum sensitivity and specificity. All the data analysis was done using GraphPad Prism 9.
Statistical analysis
Data were presented as Median (Range) for circulatory levels of miRNA. Comparison between patients and different control groups were performed using the Wilcoxon rank-sum test and one-way ANOVA test (Kruskal Wallis test). Statistical significance was defined at a p value less than 0.05 (p < 0.05).
Results
Study subjects
Newly diagnosed 25 UBC patients, and 10 BPH patients, along with 25 healthy controls, were introduced in the study. The demographic details of the participants are given in Table 1.
Relative microRNA expression in serum
The relative expression of CD44-associated miRNAs (miR-9, miR-34a, and miR-203) has been examined in serum of UBC, BPH, and healthy subjects using qRT-PCR. The relative expression of miR-9 in serum of UBC patients was significantly upregulated in contrast to healthy (p < 0.001) and BPH controls (p < 0.01) (Fig. 1A, Table 2). The relative expression of miR-34a in serum of UBC patients was significantly downregulated in UBC patients in opposition to healthy controls (p < 0.05) but was non-significant in BPH controls (Fig. 1B, Table 2). The relative expression of miR-203 was significantly upregulated in UBC patients in contrast to healthy controls (p < 0.05) but was non-significant in BPH controls (Fig. 1C, Table 2).
Circulatory levels of microRNAs of UBC patients. A Relative miR-9 expression in serum B Relative miR-34a expression in serum and C Relative miR-203 expression in serum. (n = 25 healthy controls; n = 10 BPH controls; n = 25 UBC patients). The levels were represented as arbitrary units (AU). The data were represented as median (range). The bars of significance not mentioned between some groups depict non-significance. [Healthy controls (control); BPH controls (BPH); UBC patients (UBC); *p < 0.05; **p < 0.01; ***p < 0.001; ns: non-significant]
Relative microRNA expression in urine
The relative expression of CD44-associated miRNAs (miR-9, miR-34a and miR-203) has been studied in the urine of UBC patients along with healthy and BPH controls using qRT-PCR. The relative expression of miR-9 in the urine of UBC patients was significantly upregulated in relation to healthy control (p < 0.05) but was non-significant in BPH controls (Fig. 2A, Table 2). The relative expression of miR-34a in the urine of UBC patients was non-significant as opposed to BPH and healthy controls (Fig. 2B, Table 2). The relative expression of miR-203 was significantly upregulated in UBC patients in relation to healthy (p < 0.01) and BPH controls (p < 0.05) (Fig. 2C, Table 2) which indicates its non-invasive diagnostic ability.
Relative microRNAs expression in urine. A Relative miR-9 expression in urine. B Relative miR-34a expression in urine and C Relative miR-203 expression in urine. (n = 15 healthy controls; n = 10 BPH controls; n = 15 UBC patients). The levels were represented as arbitrary units (AU). The data were represented as median (range). The bars of significance not mentioned between some groups depict non-significance. [Healthy controls (control); BPH controls (BPH); UBC patients (UBC); *p < 0.05; **p < 0.01; ***p < 0.001; ns: non-significant]
Relative microRNA expression in tissue
The relative expression of CD44-associated miRNAs (miR-9, miR-34a, and miR-203) has been studied in the tissue specimens of UBC patients along with BPH controls using qRT-PCR. The relative expression of miR-9 in tumor tissue of UBC patients was significantly upregulated as opposed to adjacent non-tumor tissue of UBC patients (p < 0.05) but was non-significant in relation to BPH controls (Fig. 3A, Table 2). The relative expression of miR-34a in tumor tissue of UBC was downregulated in comparison to BPH (p < 0.05) but non-significant as opposed to the adjacent non-tumor tissue of same UBC patients (Fig. 3B, Table 2). The relative expression of miR-203 in tumor tissue of UBC patients was non-significant in comparison to adjacent non-tumor tissue of UBC patients and BPH controls (Fig. 3C, Table 2).
Relative microRNAs expression in bladder tissue specimen. Box whisker plot depicting the relative microRNA expression of A miR-9 expression in tissue, B miR-34a expression in tissue and C miR-203 expression in tissue. (n = 10 BPH controls; n = 12 UBC NT; n = 25 UBC T). The levels were represented as arbitrary units (AU). The data were represented as median (range). The bars of significance not mentioned between some groups depict non-significance. [BPH controls (BPH); UBC adjacent normal tissue (UBC NT); UBC tumor tissue (UBC T); *p < 0.05; **p < 0.01; ***p < 0.001; ns non-significant]
Diagnostic potential of microRNAs in serum, urine, and tissue of UBC
The diagnostic potential of CD44-associated miRNAs (miR-9, miR-34a, and miR-203) was evaluated by plotting the ROC curve, which provides sensitivity, specificity, area under the curve (AUC) and cut-off values of these biomolecules. miR-203 showed optimum sensitivity and specificity in the serum (Fig. 4. A-F), urine (Fig. 5 A-F), and tissue specimen (Fig. 6 A-F) of UBC patients in contrast to miR-9 and miR-34a.
The ROC curve for diagnostic potential of microRNAs in serum. miR-9 serum (A, B); miR-34a serum (C, D); miR-203 serum (E, F). Graph A, C, and E depict the comparison between the serum samples of healthy controls and UBC patients. Graph B, D, and F depict the comparison between serum samples of BPH control and UBC patients. The graphs showcase the optimum sensitivity and specificity, area under curve along with cut-off values for serum levels [Healthy controls (control); BPH controls (BPH); UBC patients (UBC); AUC – area under the curve]
The ROC curve for diagnostic potential of microRNAs in urine. miR-9 urine (A, B); miR-34a urine (C, D); miR-203 urine (E, F). Graph A, C, and E showcase the comparison between the urine samples of healthy controls and UBC patients. Graph B, D, and F showcase the comparison between urine samples of BPH control and UBC patients. The graphs showcase the optimum sensitivity and specificity, area under curve along with cut-off values for serum levels [Healthy controls (control); BPH controls (BPH); UBC patients (UBC); AUC area under the curve]
The ROC curve for diagnostic potential of microRNAs in tissue. miR-9 tissue (A, B); miR-34a tissue (C, D); miR-203 tissue (E, F). Graph A, C, and E depict the comparison between the tissue of BPH and UBC patients. Graph B, D, and F depict the comparison between adjacent normal tissue and tumor tissue of UBC patients. BPH controls (BPH); UBC adjacent normal tissue (UBC NT); UBC tumor tissue (UBC T). The graphs showcase the optimum sensitivity and specificity, area under curve along with cut-off values for serum levels [BPH controls (BPH); UBC adjacent normal tissue (UBC NT); UBC tumor tissue (UBC T); AUC area under the curve]
Correlation
The expression of microRNAs (miR-9, miR-34a, and miR-203) in serum, urine, and tissue specimen of UBC patients was correlated by the Spearman correlation analysis. It has been observed that expression of miR-203 in urine showed significant positive correlation with expression in tumor tissue of UBC patients (r = 0.5832, p = 0.0393). This finding, thus, suggests that urinary miR-203 could be exploited further for diagnosis of UBC in future.
Discussion
Urothelial carcinoma of bladder is characterized by excessive growth in the inner lining of the bladder, i.e., urothelium. Since the rise in the COVID-19 pandemic, it has been seen that SARS-CoV-2 infection in patients with UBC has led to increase in fatalities. One of the reasons being immunological impairment seen in patients and targeting complement system has emerged as one of the effective ways to curb such conditions [28]–[30]. The cases of UBC are steadily rising due to changing lifestyle (smoking) and environmental (and occupational) conditions. Epigenetic modifications including DNA methylation, histone modifications, and post-transcriptional alterations mediated by non-coding RNA transcripts such as miRNAs play a crucial role in tumor development and progression.
microRNAs are short, non-coding RNAs that affect gene expression at the post-transcriptional level. A variety of miRNAs differentially expressed in bladder cancer have been reported [31]. Catto et al. found altered miRNA expression in the urothelium of bladder cancer patients as opposed to healthy controls. They also observed a pattern of decreased miRNA expression in low-grade tumors, including loss of miRNAs which normally suppresses FGFR3 expression. In high-grade tumors, they found upregulation of a number of miRNAs, including one that affects p53 [32].
ECM plays an important role in pathogenesis of various cancers including UBC. ECM components mediate their downstream effects via interaction with a cell surface glycoprotein, CD44. It serves as hyaluronic acid receptor and involved in cell–cell interactions, cell adhesion, and migration. Higher CD44 expression in cells provides stem-cell-like properties to the cancer cells. Previously our group reported that CD44 splice variants support the progression of urothelial carcinoma of bladder through ERK, Akt, p53, and STAT pathways [13].
The prognosis of the disease is still debatable. Currently, there is no diagnostic tool with optimum sensitivity and specificity for the non-invasive detection of bladder cancer. Biopsy, which is an invasive method, is the only confirmatory test for bladder cancer. Hence, in this maiden attempt, we studied the relative expression of CD44-associated miRNAs (miR-9, miR-34a, and miR-203) in biological fluids and tissue specimens of Indian UBC patients along with BPH and healthy controls and assessed their diagnostic potential as non-invasive biomarker for detection of bladder cancer.
In the present study, relative miR-9 expression was significantly upregulated in serum samples of UBC patients in relation to their BPH and healthy controls. Urine samples of UBC patients showed significant expression of miR-9 in contrast to healthy controls but not BPH controls. However, significant expression of miR-9 was reported in tumor tissue specimens of UBC patients in comparison to adjacent non-tumor tissues but not BPH tissues. This is the first study showcasing the circulatory levels of miR-9 in serum of UBC patients, and the results are in harmony with the reports of its higher levels in serum and tissue samples in other cancers like ovarian cancer and lung cancer [33, 34]. ROC curve analysis of miR-9 in serum samples of UBC patients and healthy controls showed optimum sensitivity and specificity proving its less invasive diagnostic potential to differentiate UBC patients from healthy controls through serum samples.
Relative miR-34a expression in serum and tissue samples was lower in UBC patients as compared to healthy controls but non-significant in contrast to BPH controls. Expression of miR-34a was non-significant in urine of UBC patients as compared to healthy and BPH controls. It may be due to the small sample size of the study subjects. In concordance with this observation, we previously observed downregulation of miR-34a in circulation and tumor site of RCC [20]. Similar reports of downregulation of miR-34s were also observed in breast cancer, prostate cancer, and mice models of bladder cancer [26, 35, 36]. ROC curve analysis of miR-34a in all biological samples showed ≤ 80% specificity and sensitivity which is very less to use it as a biomarker.
We found significantly increased relative miR-203 expression in urine samples of Indian UBC patients as compared to healthy and BPH controls. Similar reports of higher miR-203 expression are also available for tissue specimens of pancreatic adenocarcinoma and breast cancer [37, 38]. miR-203 expression is downregulated in cell lines of several cancers like cutaneous squamous cell carcinoma and prostate cancer including urinary bladder cancer showing its dual role in cancer progression [27, 39, 40]. The ROC curve analysis of miR-203 in urine showed maximum sensitivity and specificity as compared to other miRNAs which indicate its non-invasive diagnostic potential for diagnosis of bladder cancer using urine specimens. Further, urinary expression of miR-203 correlated significantly with tissue levels in UBC affirming the utilization of urine specimen as an in-situ representation of tumor milieu, hence, could be exploited for diagnosis of UBC in clinical settings.
This study is a maiden attempt that provides a brief insight into the potential role of CD44-linked miRNAs (miR-9, miR-34a, and miR-203) as a non-invasive biomarker for the diagnosis of urothelial carcinoma of bladder. Dysregulated expression of these microRNAs might contribute to disease pathogenesis which needs to be validated in future. Out of three miRNAs, miR-203 showed potential of non-invasive biomarker for urine-based detection of UBC from other urinary tract malignancies. Furthermore, study of these microRNAs in larger cohort might validate the clinical utility as non-invasive diagnostic biomarker in detection of urinary bladder cancer.
Conclusion
Urothelial carcinoma of the bladder becomes a significant concern these days. Most of the cases are detected at advanced stages. Confirmation of UBC patients is done mainly by invasive methods such as TURBT due to the lack of effective non-invasive biomarkers. Identification of new potential biomarkers in biological fluids can help diagnose bladder cancer at stage. We found that miR-203 showed high sensitivity and specificity in urine that can serve as a non-invasive biomarker for UBC detection, which needs to be validated in a larger cohort.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Sung H et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin 71(3):209–249. https://doi.org/10.3322/CAAC.21660
Tran L, Xiao JF, Agarwal N, Duex JE, Theodorescu D (2020) Advances in bladder cancer biology and therapy. Nat Rev Cancer 21(2):104–121. https://doi.org/10.1038/s41568-020-00313-1
Sanli O et al (2017) Bladder cancer. Nat Rev Dis Primers 3:17022. https://doi.org/10.1038/nrdp.2017.22
Mahdavifar N, Ghoncheh M, Pakzad R, Momenimovahed Z, Salehiniya H (2016) Epidemiology, incidence and mortality of bladder cancer and their relationship with the development index in the world. Asian Pac J Cancer Prev 17(1):381–386. https://doi.org/10.7314/APJCP.2016.17.1.381
Burger M et al (2013) Epidemiology and risk factors of urothelial bladder cancer. Eur Urol 63(2):234–241. https://doi.org/10.1016/j.eururo.2012.07.033
Alfred Witjes J et al (2017) Updated 2016 EAU guidelines on muscle-invasive and metastatic bladder cancer. Eur Urol 71(3):462–475. https://doi.org/10.1016/j.eururo.2016.06.020
Smith Z, Guzzo T (2013) Urinary markers for bladder cancer. F1000Prime Rep 5:1–6
Singh A et al (2021) Autophagy-associated HMGB-1 as a novel potential circulating non-invasive diagnostic marker for detection of urothelial carcinoma of bladder. Mol Cell Biochem. https://doi.org/10.1007/s11010-021-04299-8
Appunni S, Anand V, Khandelwal M, Seth A, Mathur S, Sharma A (2017) Altered expression of small leucine-rich proteoglycans (Decorin, Biglycan and Lumican): plausible diagnostic marker in urothelial carcinoma of bladder. Tumour Biol 39(5):1010428317699112. https://doi.org/10.1177/1010428317699112
Satyal U, Srivastava A, Abbosh PH (2019) Urine biopsy—liquid gold for molecular detection and surveillance of bladder cancer. Frontiers Oncol. https://doi.org/10.3389/fonc.2019.01266
Soria F et al (2019) Molecular markers in bladder cancer. World J Urol 37(1):31–40. https://doi.org/10.1007/s00345-018-2503-4
Satyam A, Tsokos MG, Tresback JS, Zeugolis DI, Tsokos GC (2020) Cell-derived extracellular matrix-rich biomimetic substrate supports podocyte proliferation, differentiation, and maintenance of native phenotype. Adv Funct Mater 30(44):1908752. https://doi.org/10.1002/adfm.201908752
Anand V et al (2019) CD44 splice variant (CD44v3) promotes progression of urothelial carcinoma of bladder through Akt/ERK/STAT3 pathways: novel therapeutic approach. J Cancer Res Clin Oncol 145(11):2649–2661. https://doi.org/10.1007/s00432-019-03024-9
Khan K et al (2020) Resveratrol, curcumin, paclitaxel and miRNAs mediated regulation of PI3K/Akt/mTOR pathway: go four better to treat bladder cancer. Cancer Cell Int 20(1):1–19. https://doi.org/10.1186/s12935-020-01660-7
Marei HE et al (2021) p53 signaling in cancer progression and therapy. Cancer Cell Int 21(1):703. https://doi.org/10.1186/S12935-021-02396-8
He L, Hannon GJ (2004) MicroRNAs: small RNAs with a big role in gene regulation. Nat Rev Genet 5(7):522–531. https://doi.org/10.1038/nrg1379
Rupaimoole R, Slack FJ (2017) MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat Rev Drug Discov 16(3):203–221. https://doi.org/10.1038/nrd.2016.246
Amir S, Mabjeesh NJ (2017) microRNA expression profiles as decision-making biomarkers in the management of bladder cancer. Histol Histopathol 32(2):107–119
Goulet CR et al (2019) Cancer-associated fibroblasts induce epithelial-mesenchymal transition of bladder cancer cells through paracrine IL-6 signalling. BMC Cancer. https://doi.org/10.1186/s12885-019-5353-6
Yadav S, Khandelwal M, Seth A, Saini AK, Dogra PN, Sharma A (2017) Serum microRNA expression profiling: potential diagnostic implications of a panel of serum microRNAs for clear cell renal cell cancer. Urology 104:64–69. https://doi.org/10.1016/j.urology.2017.03.013
Gupta N, Kumar R, Seth T, Garg B, Sati HC, Sharma A (2019) Clinical significance of circulatory microRNA-203 in serum as novel potential diagnostic marker for multiple myeloma. J Cancer Res Clin Oncol 145(6):1601–1611. https://doi.org/10.1007/s00432-019-02896-1
Karousou E et al (2017) Roles and targeting of the HAS/hyaluronan/CD44 molecular system in cancer. Matrix Biol 59:3–22. https://doi.org/10.1016/j.matbio.2016.10.001
Bourguignon LYW (2012) Hyaluronan-CD44 interaction promotes microRNA signaling and RhoGTPase activation leading to tumor progression. Small GTPases 3(1):53–59. https://doi.org/10.4161/sgtp.19110
Monoe Y et al (2021) Pharmacological inhibition of miR-130 family suppresses bladder tumor growth by targeting various oncogenic pathways via PTPN1. Int J Mol Sci. https://doi.org/10.3390/ijms22094751
Wang H et al (2015) miR-9 promotes cell proliferation and inhibits apoptosis by targeting LASS2 in bladder cancer. Tumor Biol 36(12):9631–9640. https://doi.org/10.1007/s13277-015-3713-7
Yu G, Yao W, Xiao W, Li H, Xu H, Lang B (2014) MicroRNA-34a functions as an anti-metastatic microRNA and suppresses angiogenesis in bladder cancer by directly targeting CD44. J Exp Clin Cancer Res 33(1):1–13. https://doi.org/10.1186/s13046-014-0115-4
Shen J, Zhang J, Xiao M, Yang J, Zhang N (2017) miR-203 suppresses bladder cancer cell growth and targets Twist1. Oncol Res Featur Preclin Clin Cancer Therap 26(8):1155–1165. https://doi.org/10.3727/096504017x15041934685237
Satyam A, Tsokos GC (2020) Curb complement to cure COVID-19. Clin Immunol 221:108603. https://doi.org/10.1016/j.clim.2020.108603
Satyam A, Tsokos MG, Brook OR, Hecht JL, Moulton VR, Tsokos GC (2021) Activation of classical and alternative complement pathways in the pathogenesis of lung injury in COVID-19. Clin Immunol 226:108716. https://doi.org/10.1016/j.clim.2021.108716
Jamaly S et al (2021) Complement activation and increased expression of Syk, mucin-1 and CaMK4 in kidneys of patients with COVID-19. Clin Immunol 229:108795. https://doi.org/10.1016/j.clim.2021.108795
Battista Di Pierro G et al (2012) Bladder cancer: a simple model becomes complex. Curr Genomics 13(5):395–415. https://doi.org/10.2174/138920212801619232
Catto JWF et al (2009) Distinct MicroRNA alterations characterize high- and low-grade bladder cancer. Can Res 69(21):8472–8481. https://doi.org/10.1158/0008-5472.CAN-09-0744
Wang H, Wu Q, Zhang Y, Zhang H-N, Wang Y-B, Wang W (2017) TGF-β1-induced epithelial–mesenchymal transition in lung cancer cells involves upregulation of miR-9 and downregulation of its target, E-cadherin. Cell Mol Biol Lett 22(1):22. https://doi.org/10.1186/s11658-017-0053-1
Zhou B et al (2017) Overexpressed miR-9 promotes tumor metastasis via targeting E-cadherin in serous ovarian cancer. Frontiers Med 11(2):214–222. https://doi.org/10.1007/s11684-017-0518-7
Li L, Yuan L, Luo J, Gao J, Guo J, Xie X (2013) MiR-34a inhibits proliferation and migration of breast cancer through down-regulation of Bcl-2 and SIRT1. Clin Exp Med 13(2):109–117. https://doi.org/10.1007/s10238-012-0186-5
Gaur S et al (2015) Chitosan nanoparticle-mediated delivery of miRNA-34a decreases prostate tumor growth in the bone and its expression induces non-canonical autophagy. Oncotarget 6(30):29161–29177
Ikenaga N et al (2010) MicroRNA-203 expression as a new prognostic marker of pancreatic adenocarcinoma. Ann Surg Oncol 17(12):3120–3128. https://doi.org/10.1245/s10434-010-1188-8
He S, Zhang G, Dong H, Ma M, Sun Q (2016) miR-203 facilitates tumor growth and metastasis by targeting fibroblast growth factor 2 in breast cancer. Onco Targets Ther 9:6203–6210. https://doi.org/10.2147/OTT.S108712
García-Sancha N, Corchado-Cobos R, Pérez-Losada J, Cañueto J (2019) MicroRNA dysregulation in cutaneous squamous cell carcinoma. Int J Mol Sci. https://doi.org/10.3390/ijms20092181
Saini S et al (2011) Regulatory role of mir-203 in prostate cancer progression and metastasis. Clin Cancer Res 17(16):5287–5298. https://doi.org/10.1158/1078-0432.CCR-10-2619
Funding
This research did not receive any specific grant from funding agency.
Author information
Authors and Affiliations
Contributions
AS1 conceived and designed the study. PS1 provided patient sample; PS2 AS2 KDR performed experiments, acquired, and analyzed data; AS1 and NG drafted the manuscript; NG helped in analyzing data; AS1, SA, PS2, AS2, and NG edited the final manuscript. [AS1: Alpana Sharma; AS2: Aishwarya Singh; PS1: Prabhjot Singh; PS2: Pradeep Singh].
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This research involving human patients and healthy individuals had provided written-informed consent. This study has been approved by Institutional Human Ethics Committee of All India Institute of Medical Sciences, New Delhi, India (IEC No.: IEC-532/02.08.2019, RP-23/2019) prior to its commencement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, P., Singh, A., Gupta, N. et al. Non-invasive diagnostic potential of microRNA-203 in liquid biopsy of urothelial carcinoma of bladder. Mol Cell Biochem 477, 2173–2182 (2022). https://doi.org/10.1007/s11010-022-04431-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-022-04431-2