Abstract
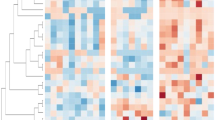
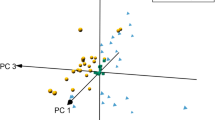
Heart failure is a syndrome with symptoms or signs caused by cardiac dysfunction. In clinic, four stages (A, B, C, and D) were used to describe heart failure progression. This study was aimed to explore plasma metabolomic and lipidomic profiles in different HF stages to identify potential biomarkers. Metabolomics and lipidomics were performed using plasma of heart failure patients at stages A (n = 49), B (n = 61), and C+D (n = 26). Analysis of Variance (ANOVA) was used for screening dysregulated molecules. Bioinformatics was used to retrieve perturbed metabolic pathways. Univariate and multivariate receiver operating characteristic curve (ROC) analyses were used for potential biomarker screening. Stage A showed significant difference to other stages, and 142 dysregulated lipids and 134 dysregulated metabolites were found belonging to several metabolic pathways. Several marker panels were proposed for the diagnosis of heart failure stage A versus stage B-D. Several molecules, including lysophosphatidylcholine 18:2, cholesteryl ester 18:1, alanine, choline, and Fructose, were found correlated with B-type natriuretic peptide or left ventricular ejection fractions. In summary, using untargeted metabolomic and lipidomic profiling, several dysregulated small molecules were successfully identified between HF stages A and B-D. These molecules would provide valuable information for further pathological researches and biomarker development.





Similar content being viewed by others
References
Mosterd A, Hoes AW (2007) Clinical epidemiology of heart failure. Heart 93:1137–1146. https://doi.org/10.1136/hrt.2003.025270
Mendez GF, Cowie MR (2001) The epidemiological features of heart failure in developing countries: a review of the literature. Int J Cardiol 80:213–219. https://doi.org/10.1016/s0167-5273(01)00497-1
McMurray JJ, Stewart S (2000) Epidemiology, aetiology, and prognosis of heart failure. Heart 83:596–602. https://doi.org/10.1136/heart.83.5.596
Redfield MM (2002) Heart failure–an epidemic of uncertain proportions. N Engl J Med 347:1442–1444. https://doi.org/10.1056/NEJMe020115
Aurigemma GP, Gottdiener JS, Shemanski L, Gardin J, Kitzman D (2001) Predictive value of systolic and diastolic function for incident congestive heart failure in the elderly: the cardiovascular health study. J Am Coll Cardiol 37:1042–1048. https://doi.org/10.1016/s0735-1097(01)01110-x
Aurigemma GP, Gaasch WH (2004) Clinical practice. Diastolic heart failure. N Engl J Med 351:1097–1105. https://doi.org/10.1056/NEJMcp022709
Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS, Ganiats TG, Goldstein S, Gregoratos G, Jessup ML, Noble RJ, Packer M, Silver MA, Stevenson LW, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Jacobs AK, Hiratzka LF, Russell RO, Smith SC Jr (2001) ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the 1995 guidelines for the evaluation and management of heart failure). J Am Coll Cardiol 38:2101–2113. https://doi.org/10.1016/s0735-1097(01)01683-7
Remes J, Miettinen H, Reunanen A, Pyörälä K (1991) Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J 12:315–321. https://doi.org/10.1093/oxfordjournals.eurheartj.a059896
Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Omland T, Wolf PA, Vasan RS (2004) Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med 350:655–663. https://doi.org/10.1056/NEJMoa031994
Dunn WB, Bailey NJ, Johnson HE (2005) Measuring the metabolome: current analytical technologies. Analyst 130:606–625. https://doi.org/10.1039/b418288j
Ortmayr K, Dubuis S, Zampieri M (2019) Metabolic profiling of cancer cells reveals genome-wide crosstalk between transcriptional regulators and metabolism. Nat Commun 10:1841. https://doi.org/10.1038/s41467-019-09695-9
Luo P, Yin P, Hua R, Tan Y, Li Z, Qiu G, Yin Z, Xie X, Wang X, Chen WJH (2018) A Large-scale, multicenter serum metabolite biomarker identification study for the early detection of hepatocellular carcinoma. Hepatology 67:662–675
Calzada E, Avery E, Sam PN, Modak A, Wang C, McCaffery JM, Han X (2019) Phosphatidylethanolamine made in the inner mitochondrial membrane is essential for yeast cytochrome bc(1) complex function. Nat Commun 10:1432. https://doi.org/10.1038/s41467-019-09425-1
Chen W, Zeng J, Wang W, Yang B, Zhong L, Zhou J (2020) Comprehensive metabolomic and lipidomic analysis reveals metabolic changes after mindfulness training. Mindfulness 11:1390–1400. https://doi.org/10.1007/s12671-020-01359-w
Zhou J, Sun L, Chen L, Liu S, Zhong L (2019) Comprehensive metabolomic and proteomic analyses reveal candidate biomarkers and related metabolic networks in atrial fibrillation. Metabolomics 15:96. https://doi.org/10.1007/s11306-019-1557-7
Zhou J, Li Q (2020) Plasma metabolomics and lipidomics reveal perturbed metabolites in different disease stages of chronic obstructive pulmonary disease. Int J Chron Obstr Pulm Dis 15:553–565. https://doi.org/10.2147/copd.s229505
Xia J, Sinelnikov IV, Han B, Wishart DS (2015) Metaboanalyst 3.0–making metabolomics more meaningful. Nucleic Acids Res 43:W251–W257. https://doi.org/10.1093/nar/gkv380
de Giuli F, Khaw KT, Cowie MR, Sutton GC, Ferrari R, Poole-Wilson PA (2005) Incidence and outcome of persons with a clinical diagnosis of heart failure in a general practice population of 696,884 in the United Kingdom. Eur J Heart Fail 7:295–302. https://doi.org/10.1016/j.ejheart.2004.10.017
Cowie MR, Wood DA, Coats AJ, Thompson SG, Suresh V, Poole-Wilson PA, Sutton GC (2000) Survival of patients with a new diagnosis of heart failure: a population based study. Heart 83:505–510. https://doi.org/10.1136/heart.83.5.505
Hunter WG, Kelly JP, McGarrah RW 3rd, Kraus WE, Shah SH (2016) Metabolic dysfunction in heart failure: diagnostic, prognostic, and pathophysiologic insights from metabolomic profiling. Curr Heart Fail Rep 13:119–131. https://doi.org/10.1007/s11897-016-0289-5
Cheng ML, Wang CH, Shiao MS, Liu MH, Huang YY, Huang CY, Mao CT, Lin JF, Ho HY, Yang NI (2015) Metabolic disturbances identified in plasma are associated with outcomes in patients with heart failure: diagnostic and prognostic value of metabolomics. J Am Coll Cardiol 65:1509–1520. https://doi.org/10.1016/j.jacc.2015.02.018
Wang J, Li Z, Chen J, Zhao H, Luo L, Chen C, Xu X, Zhang W, Gao K, Li B, Zhang J, Wang W (2013) Metabolomic identification of diagnostic plasma biomarkers in humans with chronic heart failure. Mol Biosyst 9:2618–2626. https://doi.org/10.1039/c3mb70227h
Deidda M, Piras C, Dessalvi CC, Locci E, Barberini L, Torri F, Ascedu F, Atzori L, Mercuro G (2015) Metabolomic approach to profile functional and metabolic changes in heart failure. J Transl Med 13:297. https://doi.org/10.1186/s12967-015-0661-3
Dunn WB, Broadhurst DI, Deepak SM, Buch MH, McDowell G, Spasic I, Ellis DI, Brooks N, Kell DB, Neyses L (2007) Serum metabolomics reveals many novel metabolic markers of heart failure, including pseudouridine and 2-oxoglutarate. Metabolomics 3:413–426. https://doi.org/10.1007/s11306-007-0063-5
Hunter WG, Kelly JP, McGarrah RW, Khouri MG, Craig D, Haynes C, Ilkayeva O, Stevens RD, Bain JR, Muehlbauer MJ, Newgard CB, Felker GM, Hernandez AF, Velazquez EJ, Kraus WE, Shah SH (2016) Metabolomic profiling identifies novel circulating biomarkers of mitochondrial dysfunction differentially elevated in heart failure with preserved versus reduced ejection fraction: evidence for shared metabolic impairments in clinical heart failure. J Am Heart Assoc. https://doi.org/10.1161/jaha.115.003190
Zordoky BN, Sung MM, Ezekowitz J, Mandal R, Han B, Bjorndahl TC, Bouatra S, Anderson T, Oudit GY, Wishart DS, Dyck JR (2015) Metabolomic fingerprint of heart failure with preserved ejection fraction. PLoS ONE 10:e0124844. https://doi.org/10.1371/journal.pone.0124844
Mahmod M, Pal N, Rayner J, Holloway C, Raman B, Dass S, Levelt E, Ariga R, Ferreira V, Banerjee R, Schneider JE, Rodgers C, Francis JM, Karamitsos TD, Frenneaux M, Ashrafian H, Neubauer S, Rider O (2018) The interplay between metabolic alterations, diastolic strain rate and exercise capacity in mild heart failure with preserved ejection fraction: a cardiovascular magnetic resonance study. J Cardiovasc Magn Reson 20:88. https://doi.org/10.1186/s12968-018-0511-6
Shelp BJ, Bown AW, McLean MD (1999) Metabolism and functions of gamma-aminobutyric acid. Trends Plant Sci 4:446–452. https://doi.org/10.1016/s1360-1385(99)01486-7
Carillo BA, Oliveira-Sales EB, Andersen M, Tufik S, Hipolide D, Santos AA, Tucci PJ, Bergamaschi CT, Campos RR (2012) Changes in GABAergic inputs in the paraventricular nucleus maintain sympathetic vasomotor tone in chronic heart failure. Auton Neurosci 171:41–48. https://doi.org/10.1016/j.autneu.2012.10.005
Williams RB, Marchuk DA, Gadde KM, Barefoot JC, Grichnik K, Helms MJ, Kuhn CM, Lewis JG, Schanberg SM, Stafford-Smith M, Suarez EC, Clary GL, Svenson IK, Siegler IC (2001) Central nervous system serotonin function and cardiovascular responses to stress. Psychosom Med 63:300–305. https://doi.org/10.1097/00006842-200103000-00016
Saxena PR, Villalón CM (1990) Cardiovascular effects of serotonin agonists and antagonists. J Cardiovasc Pharmacol 15(Suppl 7):S17-34
Turski WA, Nakamura M, Todd WP, Carpenter BK, Whetsell WO Jr, Schwarcz R (1988) Identification and quantification of kynurenic acid in human brain tissue. Brain Res 454:164–169. https://doi.org/10.1016/0006-8993(88)90815-3
Swartz KJ, During MJ, Freese A, Beal MF (1990) Cerebral synthesis and release of kynurenic acid: an endogenous antagonist of excitatory amino acid receptors. J Neurosci 10:2965–2973. https://doi.org/10.1523/jneurosci.10-09-02965.1990
Boldyrev AA, Severin SE (1990) The histidine-containing dipeptides, carnosine and anserine: distribution, properties and biological significance. Adv Enzyme Regul 30:175–194. https://doi.org/10.1016/0065-2571(90)90017-v
Troughton RW, Frampton CM, Yandle TG, Espiner EA, Nicholls MG, Richards AM (2000) Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (N-BNP) concentrations. Lancet 355:1126–1130. https://doi.org/10.1016/s0140-6736(00)02060-2
Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, Olofsson B, Ostergren J (2003) Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet 362:777–781. https://doi.org/10.1016/s0140-6736(03)14285-7
Schymanski EL, Jeon J, Gulde R, Fenner K, Ruff M, Singer HP, Hollender J (2014) Identifying small molecules via high resolution mass spectrometry: communicating confidence. Environ Sci Technol 48:2097–2098. https://doi.org/10.1021/es5002105
Funding
This study was funded by the Fund for Fostering Young Scholars of Peking University Health Science Center (Grant No. BMU2018PY006), the National Natural Science Foundation of China (82070272) and Beijing Municipal Natural Science Foundation (7202225).
Author information
Authors and Affiliations
Contributions
JZ, XC, LZ, and MC designed this study. XC and WC collected the clinical samples. JZ and LZ performed the metabolomic and lipidomic experiments. JZ analyzed the omics data. XC and MC reviewed the statistical results. JZ and MC wrote the manuscript. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures performed in these studies involving human participants were in accordance with the ethical standards of the institutional and national research committee of Peking University Third Hospital (ethical approval number M2017293), and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Written informed consent was provided for all participants before enrollment.
Consent for publication
Written informed consent for publication was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, J., Chen, X., Chen, W. et al. Comprehensive plasma metabolomic and lipidomic analyses reveal potential biomarkers for heart failure. Mol Cell Biochem 476, 3449–3460 (2021). https://doi.org/10.1007/s11010-021-04159-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-021-04159-5