Abstract
The TP53 signal transduction pathway is an attractive target for cancer treatments. In this study, we conducted a comprehensive molecular evaluation of 907 patients with cancer in Japan to identify genomic alterations in the TP53 pathway. TP53 mutations were frequently detected in many cancers, except melanoma, thymic tumors, gastrointestinal stromal tumors, and renal cancers. The frequencies of non-synonymous single nucleotide variants (SNVs) in the TP53 family members TP63 and TP73 were relatively low, although genes with increased frequencies of SNVs were as follows: PTEN (11.7%) in breast cancer, CDKN2A (11.1 and 9.6%) in pancreas and head and neck cancers, and ATM (18.0 and 11.1%) in liver and esophageal cancers. MDM2 expression was decreased or increased in patients with mutant or wild-type TP53, respectively. CDKN1A expression was increased with mutant TP53 in head and neck cancers. Moreover, TP63 overexpression was characteristically observed in squamous cell carcinomas of the lung, esophagus, and head and neck region. Additionally, overexpression of TP63 and TP73 was frequently observed in thymomas. Our results reveal a spectrum of genomic alterations in the TP53 pathway that is characteristic of many tumor types, and these data may be useful in the trials of targeted therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Genome sequencing is an essential tool for cancer research that leads to important biological discoveries and allows for the systematic classification of mutations based on cellular signal transduction pathways [1, 2]. Furthermore, data accumulated from studies using tumor tissues of patients with cancer has led to the identification of somatic alterations in many cancer-related genes [3, 4]. The TP53 gene encodes a tumor suppressor and frequently undergoes somatic mutation in tumor cells [5]. A database of TP53 mutations is available [6, 7], and there are detailed data regarding the functional activities of TP53 mutants.
TP53 mediates diverse cellular functions, including the response to DNA damage and induction of cell cycle arrest, cellular senescence, autophagy, and apoptosis [8–10]. Additionally, TP53 can regulate the cellular metabolism [11], inhibit stem cell self-renewal, and control the reprograming of differentiated cells into stem cells [8]. TP53 has also been shown to mediate tumor metastasis and invasion [12]. The disruption of signaling pathways that activate TP53 play an important role in tumor progression. Although TP53 knockout mice develop normally, their susceptibility to cancers is higher than wild-type TP53 animals [13]. TP53 germline mutations in humans are associated with increased susceptibility to cancer and an earlier age of onset compared to TP53 wild-type controls [14]. Li-Fraumeni syndrome is a rare, inherited, and highly penetrant disorder that predisposes individuals to cancer. This syndrome is characterized by autosomal dominant TP53 germline mutation [15]. Thus, exploiting the tumor suppressor function of TP53 and the high frequencies of TP53 mutations in cancer tissues represents an appealing therapeutic strategy for developing cancer treatments. However, despite numerous attempts to target the TP53 pathway [16, 17], there are currently no treatments available in the clinic [5].
TP53 activity is regulated by the E3 ubiquitin protein ligase and proto-oncoprotein murine double minute 2 (MDM2) and by post-translational modifications, such as phosphorylation and acetylation. MDM2 inhibits TP53 transcriptional activity by binding to the N-terminal domain of TP53, which leads to downregulation of the TP53 pathway [18]. Overexpression of MDM2 in mice revealed a TP53-independent role in tumorigenesis [19], and MDM2 overexpression or amplification occurs in many human cancers and contributes to oncogenesis [20, 21]. Previous studies have demonstrated that inhibiting MDM2-TP53 binding in xenograft models restores TP53 function and can inhibit tumor cell proliferation and induce apoptosis [22]. However, the data indicate that the mechanisms underlying these effects are associated with the more complex regulation of MDM2 expression. Although many TP53-associated molecules play important roles in regulating TP53 transcription [8, 23], the regulatory mechanisms underlying its activation in vivo have not been fully elucidated. In this study, we present a comprehensive analysis of genomic alterations that are associated with the TP53 pathway in various tumors in a Japanese population. We analyzed tumor tissues and adjacent normal tissues and blood samples to identify tumor-specific somatic mutations. We anticipate that this comprehensive analysis will lead to the development of individualized treatment strategies.
Materials and methods
Subjects
The Shizuoka Cancer Center (Shizuoka, Japan) launched Project HOPE in late January 2014. The project objective is to improve cancer medicine [24]. As a component of this project, we performed whole exome sequencing (WES) using blood samples and fresh surgical specimens. We then conducted comprehensive analyses of gene expression using matched tumor and adjacent normal tissues from each patient. Tumor-specific single nucleotide variants (SNVs) were determined by comparing tumor tissue with blood cell data from the same patient. The characteristics of the subjects are summarized in Table 1, and the detailed histpathological characteristics are presented in Supplementary Table 1. The research plan was designed according to the revised Ethical Guidelines for Human Genome/Gene Analysis Research in Japan (http://www.lifescience.mext.go.jp/files/pdf/n1115_01.pdf) and was approved by the Institutional Review Board of the Shizuoka Cancer Center. All patients provided written informed consent.
DNA preparation
We obtained blood and tumor samples from 907 patients with cancer at the time of surgery. Surgeries were performed at the Shizuoka Cancer Center Hospital between January 2014 and March 2015. Sample genomic DNA was extracted from whole blood and tumor tissues using a QIAamp DNA Mini kit (Qiagen, Hilden, Germany). DNA was quantified using a Nanodrop spectrophotometer (Thermo Fisher Scientific, Wilmington, DE, USA) and a Qubit 2.0 fluorometer (Thermo Fisher Scientific). AcroMetrix Oncology Hotspot Control DNA (Thermo Fisher Scientific) was used as the standard.
RNA preparation
Fresh tumor and adjacent normal tissue were soaked in RNAlater reagent (Qiagen). The total RNA was then isolated and purified using an RNeasy Mini kit (Qiagen) according to the manufacturer’s protocol. Total RNA was analyzed using a Nanodrop 2000 spectrophotometer (Thermo Fisher Scientific) and gel electrophoresis. The RNA quality was evaluated using gel electrophoresis and the A260/A280 value. The RNA integrity number (RIN) [25] was determined using an Agilent 2100 Bioanalyzer (Agilent Technologies, Santa Clara, CA, USA). We used RNA samples with an A260/A280 > 1.8 and a RIN > 6.0 for gene expression analysis.
Whole exome sequencing (WES)
We performed WES using an Ion Proton System equipped with a PI chip V2 together with an AmpliSeq Exome kit (Thermo Fisher Scientific) [26]. Briefly, 100 ng each of tumor and matched blood cell DNA was used for target amplification with the following protocol: 99 °C for 2 min, followed by 10 cycles at 95 °C for 15 s and 60 °C for 16 min, and a final hold at 10 °C. The incorporated primer sequences were partially digested using FuPa Reagent (Thermo Fisher Scientific). Ion Torrent Proton adapters were ligated to the amplicons at 22 °C for 30 min and then at 72 °C for 10 min. The amplicon library was purified using Agencourt AMPure XP Beads (Thermo Fisher Scientific). The library DNA was quantified by qRT-PCR, and 7 pM library DNA was used for sequencing. The sequencing data were aligned to the human reference genome (assembly GRCh37/hg19) and were quality trimmed using Ion Torrent Suite version 4.2 (Thermo Fisher Scientific). The mutations were visualized using the Integrative Genomics Viewer [27] and were validated using Sanger sequencing or pyrosequencing.
Validation of somatic mutations using deep sequencing of the Custom Cancer Panel (CCP)
The candidate mutations identified by WES were validated using the Ion Torrent PGM AmpliSeq Custom Panel (Themo Fisher Scientific) for 409 target genes (the target genes are available at https://www.thermofisher.com). We used a 200-bp standard DNA option to design the AmpliSeq primers. Sample DNA was diluted to 10 ng/µL, and 1 µL was used to prepare the amplicon library according to the manufacturer’s protocol (Themo Fisher Scientific). The target sequences were amplified using the customized primers and were then partially digested. The adapters and barcodes were ligated to the amplicons, which were then purified using the Agencourt AMPure XP reagent (Thermo Fisher Scientific). The libraries were sequenced using the same method described above for WES.
Comprehensive gene expression analysis using a DNA microarray
Cyanin-3 (Cy3)-labeled cRNA was prepared from 100 ng of RNA using a One-color Low Input Quick Amp Labeling kit (Agilent Technologies) according to the manufacturer’s instructions, and the RNA was purified using an RNeasy Mini kit (Qiagen). Dye incorporation and the cRNA yield were evaluated using the Nanodrop 2000 spectrophotometer. Cy3-labeled cRNA was hybridized to SurePrint G3 Human GE version 2.0 containing 50,599 probes (Agilent Technologies) for 17 h at 65 °C while rotating in an Agilent hybridization oven. After hybridization, the microarrays were washed for 1 min at room temperature with GE Wash Buffer 1 (Agilent Technologies) and for 1 min at 37 °C with GE Wash Buffer 2 (Agilent Technologies). The microarrays were then dried using the Agilent stabilization and drying solution. The slides were scanned using an Agilent DNA microarray scanner immediately after washing [28]. The scanned images were quantitated using GeneSpring version 13.1.1 software (Agilent Technologies) to generate raw signal intensity data. The raw signals were log-transformed and normalized (GeneSpring software). The difference in the normalized microarray signal intensities (fold change) between the tumor and adjacent normal tissue were then calculated [29].
Results
We used WES to analyze 18,835 genes in paired tumor tissue and blood samples to detect genetic changes in 19 different tumors. Simultaneously, we used the CCP comprising 409 target genes to conduct deep sequencing of tumor tissue samples. The mean depth of coverage of the target regions was 118-fold for WES and 1,101-fold for the CCP. We detected the following 9,439 non-synonymous single nucleotide variants (SNVs) by WES and CCP using 409 target genes in 907 patient tumors: 6,889 missense, 858 nonsense, 229 splice site, 1309 frameshift, and 154 other mutations. The genes listed in Supplementary Table 2 are classified as oncogenes or tumor suppressor genes according to Vogelstein et al. [30]. If there were multiple mutations found in a gene, then all of the mutations were counted. There are 30 genes, including BRCA1 and BRCA2, that are not involved in the CCP (the genes are marked by an asterisk in Supplementary Table 2). The non-synonymous SNVs of well-annotated cancer genes, such as PIK3CA, APC, KRAS, CTNNB1, FBXW7, GATA3 and VHL, and TP53, were consistent with those of previous studies [3, 4, 31].
Somatic mutations in TP53 were the most frequently detected (52.7%) in the set of cancer-related genes. The frequencies of missense, nonsense, frameshift, and splice site somatic mutations in TP53 were 72.0, 14.2, 8.2, and 5.6%, respectively. The tumor frequencies were the following: colorectum (72.0%), esophagus (61.1%), stomach (59.5%), head and neck (57.5%), lung (48.9%), and pancreas (38.9%) (Table 2). There were no TP53 mutations detected in renal cancer, melanoma, thymic tumor, or gastrointestinal stromal tumor (GIST). The data indicate that 92.5% of the somatic mutations were identified in the DNA-binding domain of TP53.
The frequencies of somatic mutations in members of the TP53 family and its related genes were low (Table 2). However, we detected increased frequencies of somatic mutations among genes encoding components of the TP53 signaling pathway (Table 3). These genes are important and well-established genes for p53-associated responses [8, 9]. The mutation data include the following: PTEN (11.7 and 8.7%) in breast and colorectal cancer; ATM (18.0 and 11.1%) in liver and esophagus cancer; CDKN2A (11.1 and 9.6%) in pancreas and head and neck cancer; and ATM (50.0%), ATR (41.7%), PTEN (83.3%), RB1 (41.7%), and EP300 (33.3%), which is an acetyltransferase (HAT) associated with TP53 acetylation [32], in uterine cancer. We detected the wild-type pleckstrin homology-like domain family member 3 (PHLDA3), which is a TP53-regulated repressor of AKT [33], and the TP53-upregulated modulator of apoptosis (PUMA) in all samples.
Possible interactions between the TP53-related mutations and smoking status were examined in the stratified analyses (Supplementary Table 3). Among them, the TP53 mutation in smoking status was found to be associated with lung cancers in a statistically significant manner (P = .0169). One limitation of the present study is that we had insufficient information on the drinking status of the enrolled subjects. Possible interactions with smoking status, and other environmental/lifestyle-related factors need to be evaluated in further studies.
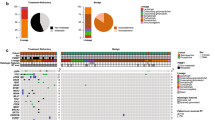
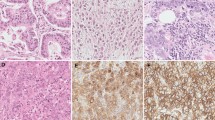
We next used microarrays to conduct gene expression profiling analysis on pairs of tumors and adjacent normal tissue (Fig. 1). The following genes were overexpressed in various tumors: CCND1 in colorectal and renal cancers, and sarcoma; CCNE1 in colorectal, lung, stomach, esophagus, head and neck, uterine and ovarian cancers, and sarcoma; and CDKN2A in lung, uterine, and ovarian cancers. PHLDA3 expression was decreased in breast and rectal cancer. However, PHLDA3 was increased in renal cancer and GIST. The expression level of AKT1 was decreased in renal cancer and GIST. The expressions BAX and PUMA were increased in the majority of samples. TP53 overexpression was detected in colorectal cancer and TP63 overexpression was characteristically detected in squamous cell carcinoma of the lung, esophagus, and tumors in the head and neck region. Moreover, the expression levels of TP53, TP63, and TP73 were increased at high frequency in thymomas.
Analysis of gene expression profiles of 19 tumor types. Heat map showing 14 of the TP53 pathway-associated genes that were differentially expressed in tumor tissues relative to adjacent normal tissues. The expression levels (log2) were normalized for each gene and are shown by the graded color scale, with red and blue representing high and low expressions, respectively. White squares indicate the expression levels (absent call) for which the fold change (FC) could not be calculated, as described in Methods. TP53 status (bottom) is indicated by dark green and white squares that indicate the presence and absence of mutations, respectively. Yellow bars with numbers beneath the graphs indicate squamous cell carcinomas of the lung, esophagus, and head and neck region. Bright green bars with numbers (bottommost) indicate thymoma cases in thymus. a Colon (n = 163), rectum (n = 148); b lung (n = 176); c stomach (n = 116); d esophagus (n = 18); e liver (n = 61); f breast (n = 60); g head & neck (n = 73); h sarcoma (n = 16); i pancreas (n = 18); j kidney (n = 13); k GIST (n = 9); l uterus (n = 12); m thymus (n = 6); n melanoma (n = 5); o ovary (n = 4); p brain (n = 3); q skin (n = 3); r bile duct (n = 2); s gallbladder (n = 1). The bottommost number shows an individual tumor
We compared the expression levels of the most important TP53-responsive genes MDM2 and CDKN1A (encoding p21) based on TP53 status (Fig. 2). This analysis indicated that MDM2 was consistently expressed at a high level in the surgical specimens of renal cancer, thymic tumor, and GIST. However, somatic mutations in TP53 were not detected. In patients with other cancer types, the absence of a somatic mutation in TP53 was commonly associated with increased MDM2 expression, except colorectal cancers. In contrast, the presence of somatic mutations in TP53 was associated with decreased MDM2 expression. While the expression levels of CDKN1A were increased in surgical specimens from the esophagus and head and neck cancers with a mutated TP53 gene, the expression levels were unrelated to the TP53 status in patients with other cancer types.
Correlations between the TP53 status and MDM2 or CDKN1A expression levels in various tumor types. The TP53 status is indicated as mutated (+) or non-mutated (−). In each case, the MDM2 or CDKN1A expression level is denoted as the number of tumor tissues with increased (red) or decreased (blue) expression relative to adjacent normal tissues, as described in Methods. a Colorectum (n = 311); b lung (n = 176); c stomach (n = 116); d esophagus (n = 18); e liver (n = 61); f breast (n = 60); g head & neck (n = 73); h sarcoma (n = 16); i pancreas (n = 18); j kidney (n = 13); k GIST (n = 9); l uterus (n = 12); m thymus (n = 6); n melanoma (n = 5); o others (n = 13). Others were as follows: ovary (n = 4), brain (n = 3), bile duct (n = 2), skin (n = 3), and gallbladder (n = 1). Somatic TP53 mutations were not detected in kidney, GIST, thymus, and melanoma
Discussion
Genes encoding downstream components of the TP53 signaling pathway were identified in studies using various inducible promoters in cancer cell lines, gene silencing, and transgenic knock-in models [34]. Additionally, recent extensive cancer genome analyses have revealed that numerous genes encoding components of the TP53 pathway are altered in human cancers. These findings suggest that the TP53 pathway plays a critical role in a range of malignancies [9]. These are currently a limited number of studies examining gene expression simultaneously in fresh tissues from multiple tumor types in a Japanese population to determine TP53 status or mutations in genes encoding components of the pathway.
In the present study, we detected TP53 mutations and other genetic abnormalities in the TP53 pathway in many tumors. We were intrigued that our microarray analysis revealed that MDM2 was frequently expressed at high levels in patients with wild-type TP53. We assume in these patients that MDM2 formed a complex with wild-type TP53 and inhibited the ability of TP53 to activate transcription of its target gene(s). The overexpression of MDM2 promotes cell proliferation and tumorigenesis and is correlated with poor clinical outcomes [35]. The inactivation of MDM2 is essential for the activation of TP53. Thus, MDM2 may represent an independent target for drug development. For example, Tovar et al. [36] reported that the small molecule RG7112 acts as an MDM2 antagonist and showed potent antitumor activity in tumors expressing wild-type TP53 in xenograft mouse models. In addition, we detected CDKN1A overexpression in tumors of the colorectum, head and neck, esophagus, and stomach with mutated TP53. CDKN1A is a key regulator of the cell cycles, cell death, DNA repair, and cell motility [37]. Several studies have indicated that the CDKN1A overexpression is correlated with poor prognosis in different cancers, including esophageal carcinoma [38, 39]. Thus, identifying target molecules based on TP53 status may facilitate the stratification of patients and development of more effective targeted therapies. TP63 is frequently expressed in squamous cell carcinomas of the lung, head and neck region, and esophagus [40–42]. In this study, we detected high levels of TP63 expression in patients with these carcinomas. Moreover, we demonstrate that TP53, T63, and TP73 were frequently expressed in thymomas. There are a limited number of reports describing the gene expressions in thymoma patients [43]. TP63 and TP73 encode a C-terminal sterile-alpha-motif domain that is not present in TP53. This domain is important for protein–protein interactions and is associated with regulating development [44]. The transcription factors TP63 and TP73 are phosphorylated and play important roles in the activation of transcription genes controlling apoptosis [45]. TP63 also has essential roles in embryogenesis and in the maintenance and differentiation of epithelial stem cells [46, 47]. TP63 and TP73 are overexpressed in human cancers, and their loss affects tumor progression and metastasis [45]. Moreover, abnormal splicing caused by TP63/TP73 overexpression is frequently observed in human malignancies and is associated with poor clinical outcomes [44]. Thus TP63/TP73 may be promising new targets for treating thymomas.
In this study, we used WES and global gene expression profiling to reveal the types of genetic abnormalities that occur in Japanese patients with cancer. Several types of cancer-acquired mechanisms result in the inactivation of the TP53 or components of its signal transduction pathway. Thus, restoration of the TP53-mediated tumor suppression system could serve as a key strategy for preventing tumor development and progression. Understanding how target genes are involved in the TP53 pathway in many tumor types is essential for selecting patients who will respond to cancer therapy. We expect that our study will lead to further functional characterization of genes in the context of TP53-based individualized therapy.
References
Kilpivaara O, Aaltonen LA (2013) Diagnostic cancer genome sequencing and the contribution of germline variants. Science 339:1559–1562
Garraway LA, Lander ES (2013) Lessons from the cancer genome. Cell 153:17–37
Lawrence MS, Stojanov P, Mermel CH, Garraway LA, Golub TR, Meyerson M, Gabriel SB, Lander ES, Getz G (2014) Discovery and saturation analysis of cancer genes across 21 tumor types. Nature 505:495–501
Kandoth C, McLellan MD, Vandin F, Ye K, Niu B, Lu C, Xie M, Zhang Q, McMichael JF, Wyczalkowski MA, Leiserson MDM, Miller CA, Welch JS, Walter MJ, Wendl MC, Ley TJ, Wilson RK, Raphael BJ, Ding L (2013) Mutational landscape and significance across 12 major cancer types. Nature 502:333–339
Soussi T, Wiman KG (2015) TP53: an oncogene in disguise. Cell Death Differ 22:1239–1249
Petitjean A, Mathe E, Kato S, Ishioka C, Tavtigian SV, Hainaut P, Olivier M (2007) Impact of mutant p53 functional properties on TP53 mutation patterns and tumor phenotype: lessons from recent developments in the IARC TP53 database. Hum Mutat 28:622–629
Leroy B, Fournier JL, Ishioka C, Monti P, Inga A, Fronza G, Soussi T (2013) The TP53 website: an integrative resource centre for the TP53 mutation database and TP53 mutant analysis. Nucleic Acids Res 41:D962–D969
Bieging KT, Mello SS, Attardi LD (2014) Unravelling mechanisms of p53-mediated tumor suppression. Nat Rev Cancer 14:359–370
Stracquadanio G, Wang X, Wallace MD, Grawenda AM, Zhang P, Hewitt J, Zeron-Medina J, Castro-Giner F, Tomlinson IP, Goding CR, Cygan KJ, Fairbrother WG, Thomas LF, Soetrom P, Gemignani F, Landi S, Schuster-Bockler B, Bell DA, Bond GL (2016) The importance of p53 pathway genetics in inherited and somatic cancer genomes. Nat Rev Cancer 16:251–265
White E (2015) The role for autophagy in cancer. J Clin Invest 125:42–46
Haupt S, Raghu D, Haupt Y (2016) Mutant p53 drives cancer by subverting multiple tumor suppression pathways. Front. Oncol 6:12. doi:10.3389/fonc.2016.00012
Cordani M, Pacchiana R, Butera G, D’Orazi G, Scarpa A, Donadelli M (2016) Mutant p53 proteins alter cancer cell secretome and tumour microenvironment: involvement in cancer invasion and metastasis. Cancer Lett 376:303–309
Donehower LA, Harvey M, Slagle BL, McArthur MJ, Montgomery CA Jr, Butel JS, Bradley A (1992) Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature 356:215–221
Merino D, Malkin D (2014) p53 and hereditary cancer. Subcell Biochem. 85: 1–16
Malkin D (2011) Li-Fraumeni syndrome. Gene Cancer 2:475–484
Hoe KK, Verma CS, Lane DP (2014) Drugging the p53 pathway: understanding the route to clinical efficacy. Nat Rev Drug Discov 13:217–236
Cheok CF, Verma CS, Baselga J, Lane DP (2011) Translating p53 into the clinic. Nat Rev Clin Oncol 8:25–37
Nag S, Qin J, Srivenugopal KS, Wang M, Zhang R (2013) The MDM2-p53 pathway revisited. J Biomed Res 27:254–271
Jones SN, Hancock AR, Vogel H, Donehower LA, Bradley A (1998) Overexpression of Mdm2 in mice reveals a p53-independent role for Mdm2 in tumorigenesis. Proc Natl Acad Sci USA 95:15608–15612
Deb SP, Singh S, Deb S (2014) MDM2 overexpression, activation of signaling networks, and cell proliferation. Subcell Biochem 85: 215–234
Wade M, Li YC, Wahl GM (2013) MDM2, MDMX and p53 in oncogenesis and cancer therapy. Nat Rev Cancer 13:83–96
Wang S, Sun W, Zhao Y, McEachern D, Meaux I, Barriere C, Stuckey J, Meagher J, Bai L, Liu L, Hoffman-Luca CG, Lu J, Shangary S, Yu S, Bernard D, Aguilar A, Dos-Santos O, Besret L, Guerif S, Pannier P, Gorge-Bernat D, Debussche L (2014) SAR405838: An optimized inhibitor of MDM2-p53 interaction that induces complete and durable tumor regression. Cancer Res 74:5855–5865
Nakamura Y (2004) Isolation of p53-target genes and their functional analysis. Cancer Sci 95:7–11
Yamaguchi K, Urakami K, Ohshima K, Mochizuki T, Akiyama Y, Uesaka K, Nakajima T, Takahashi M, Tamai S, Kusuhara M (2014) Implementation of individualized medicine for cancer patients by multiomics-based analyses-the Project HOPE-. Biomed Res (Tokyo) 35: 407–412
Stan AD, Ghose S, Gao XM, Roberts RC, Lewis-Amezcua K, Hatanpaa KJ, Tamminga CA (2006) Human postmortem tissue: what quality markers matter? Brain Res 1123:1–11
Urakami K, Shimada Y, Ohshima K, Nagashima T, Serizawa M, Tanabe T, Saito J, Usui T, Watanabe Y, Naruoka A, Ohnami SU, Ohnami S, Mochizuki T, Kusuhara M, Yamaguchi K (2016) Next generation sequencing approach for detecting 491 fusion genes from human cancer. Biomed Res 37: 51–62 (Tokyo)
Robinson JT, Thorvaldsdottir H, Winckler W, Guttman M, Lander ES, Getz G, Mesirov JP (2011) Integrative genomics viewer. Nat Biotechnol 29:24–26
Fu J, Khaybullin R, Zhang Y, Xia A, Qi X (2015) Gene expression profiling leads to discovery of correlation of matrix metalloproteinase 11 and heparanase 2 in breast cancer progression. BMC Cancer 15:473–482
Furuhata S, Ando k, Oki M, Aoki K, Ohnishi S, Aoyagi K, Sasaki H, Sakamoto H, Yoshida T, Ohnami S (2007) Gene expression profiles of endothelial progenitor cells by oligonucleotide microarray analysis. Mol Cell Biochem 298:125–138
Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA Jr, Kinzler KW (2013) Cancer genome landscapes. Science 339:1546–1558
Tamborero D, Gonzalez-Perez A, Perez-Llamas C, Deu-Pons J, Kandoth C, Reimand J, Lawrence MS, Getz G, Bader GD, Ding L, Lopez-Bigas N (2013) Comprehensive identification of mutational cancer driver genes across 12 tumor types. Sci Rep 3: 2650. doi:10.1038/srep02650
Zhang E, Guo Q, Gao H, Xu R, Teng S, Wu Y (2015) Metformin and resveratrol inhibited high glucose-induced metabolic memory of endothelial senescence through SIRT1/p300/p53/p21 pathway. PLoS One 10:e0143814. doi:10.1371/journal.pone.0143814
Kawase T, Ohki R, Shibata T, Tsutsumi S, Kamimura N, Inazawa J, Ohta T, Ichikawa H, Aburatani H, Tashiro F, Taya Y (2009) PH domain-only protein PHLDA3 is a p53-regulated repressor of Akt. Cell 136:535–550
Brady CA, Jiang D, Mello SS, Johnson TM, Jarvis LA, Kozak MM, Broz DK, Basak S, Park EJ, McLaughlin ME, Karnezis AN, Attardi LD (2011) Distinct p53 transcriptional programs dictate acute DNA damage responses and tumor suppression. Cell 145:571–583
Onel K, Cordon-Cardo C (2004) MDM2 and prognosis. Mol Cancer Res 2:1–8
Tovar C, Graves B, Packman K, Filipovic Z, Xia BHM, Tardell C, Garrido R, Lee E, Kolinsky K, To KH, Linn M, Podlaski F, Wovkulich P, Vu B, Vassilev LT (2013) MDM2 small-molecule antagonist RG7112 activates p53 signaling and regresses human tumors in preclinical cancer models. Cancer Res 73:2587–2597
Jung YS, Qian Y, Chen X (2010) Examination of the expanding pathways for the regulation of p21 expression and activity. Cell Signal 22:1003–1012
Taghavi N, Biramijamal F, Sotoudeh M, Moaven O, Khademi H, Abbaszadegan MR, Malekzadeh R (2010) Association of p53/p21 expression with cigarette smoking and prognosis in esophageal squamous cell carcinoma patients. World J Gastroenterol 16:4958–4967
Gomyo Y, Ikeda M, Osaki M, Tatebe S, Tsujitani S, Ikeguchi M, Kaibara N, Ito H (1997) Expression of p21 (waf1/cip1/sdi1), but not p53 protein, is a factor in the survival of patients with advanced gastric carcinoma. Cancer 79:2067–2072
Weber A, Bellmann U, Bootz F, Wittekind C, Tannapfel A (2002) Expression of p53 and its homologues in primary and recurrent squamous cell carcinomas of the head and neck. Int J Cancer 99:22–28
Massion PP, Taflan PM, Rahman SMJ, Yildiz P, Shyr Y, Edgerton ME, Westfall MD, Roberts JR, Pietenpol JA, Carbone DP, Gonzalez AL (2003) Significance of p63 amplification and overexpression in lung cancer development and prognosis. Cancer Res 63:7113–7121
Hu H, Xia SH, Li AD, Xu X, Cai Y, Han YL, Wei F, Chen BS, Huang XP, Han YS, Zhang JW, Zhang X, Wu M, Wang MR (2002) Elevated expression of p63 protein in human esophageal squamous cell carcinomas. Int J Cancer 102:580–583
Liang CC, Lu TL, Yu YR, You LR, Chen CM (2015) β-catenin activation drives thymoma initiation and progression in mice. Oncotarget 6:13978–13993
Inoue K, Fry EA (2014) Alterations of p63 and p73 in human cancers. Subcell Biochem 85: 17–40
Candi E, Agostini M, Melino G, Bernassola F (2014) How the TP53 family proteins TP63 and TP73 contribute to tumorigenesis: regulators and effectors. Hum Mutat 35:702–714
Mills AA, Zheng B, Wang XJ, Vogel H, Roop DR, Bradley A (1999) P63 is a p53 homologue required for limb and epidermal morphogenesis. Nature 398:708–713
Yang A, Schweitzer R, Sun D, Kaghad M, Walker N, Bronson RT, Tabin C, Sharpe A, Caput D, Crum C, McKeon F (1999) p63 is essential for regenerative proliferation in limb, craniofacial and epithelial development. Nature 398:714–718
Acknowledgements
We thank Mami Mizuguchi and Fukumi Kamada for their excellent contributions and the staff at the Shizuoka Cancer Center Hospital for clinical support and sample preparation.
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ohnami, S., Ohshima, K., Nagashima, T. et al. Comprehensive characterization of genes associated with the TP53 signal transduction pathway in various tumors. Mol Cell Biochem 431, 75–85 (2017). https://doi.org/10.1007/s11010-017-2977-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-017-2977-1