Abstract
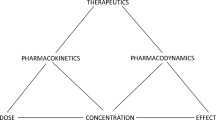
Here we characterize and summarize the pharmacokinetic changes for metabolized drugs when drug–drug interactions and pharmacogenomic variance are observed. Following multiple dosing to steady-state, oral systemic concentration–time curves appear to follow a one-compartment body model, with a shorter rate limiting half-life, often significantly shorter than the single dose terminal half-life. This simplified disposition model at steady-state allows comparisons of measurable parameters (i.e., area under the curve, half-life, maximum concentration and time to maximum concentration) following drug interaction or pharmacogenomic variant studies to be utilized to characterize whether a drug is low versus high hepatic extraction ratio, even without intravenous dosing. The characteristics of drugs based on the ratios of area under the curve, maximum concentration and half-life are identified with recognition that volume of distribution is essentially unchanged for drug interaction and pharmacogenomic variant studies where only metabolic outcomes are changed and transporters are not significantly involved. Comparison of maximum concentration changes following single dose interaction and pharmacogenomic variance studies may also identify the significance of intestinal first pass changes. The irrelevance of protein binding changes on pharmacodynamic outcomes following oral and intravenous dosing of low hepatic extraction ratio drugs, versus its relevance for high hepatic extraction ratio drugs is re-emphasized.
Similar content being viewed by others
References
Benet LZ, Bowman CM, Liu S, Sodhi JK (2018) The extended clearance concept following oral and intravenous dosing: theory and critical analyses. Pharm Res 35:242
Grover A, Benet LZ (2009) Effects of drug transporters on volume of distribution. AAPS J 11:250–261
Benet LZ, Galeazzi RJ (1979) Noncompartmental determination of the steady-state volume of distribution. J Pharm Sci 68:1071–1074
Sahin S, Benet LZ (2008) The operational multiple dosing half-life: a key to defining drug accumulation in patients and to designing extended release dosage forms. Pharm Res 25:2869–2877
Benet LZ, Liu S, Wolfe AR (2018) The universally unrecognized assumption in predicting drug clearance and organ extraction ratio. Clin Pharmacol Ther 103:521–525
Benet LZ, B-a Hoener (2002) Changes in plasma protein binding have little clinical relevance. Clin Pharmacol Ther 71:115–121
Alván G, Piafsky K, Lind M, von Bahr C (1977) Effect of pentobarbital on the disposition of alprenolol. Clin Pharmacol Ther 22:316–321
Blake CM, Kharasch ED, Schwab M, Nagele P (2013) Meta-analysis of CYP2D6 metabolizer phenotype and metoprolol pharmacokinetics. Clin Pharmacol Ther 94:394–399
Kharasch ED, Regina KJ, Blood J, Friedel C (2015) Methadone pharmacogenomics: CYP2B6 polymorphisms determine plasma concentrations, clearance and metabolism. Anesthesiology 123:1142–1153
Hsu YC, Chen BG, Yang YS, Huang SP, Huang MH, Chen TJ, Liu HC, Lin DL, Jones AW (2013) Methadone concentrations in blood, plasma and oral fluid determined by isotope-dilution gas chromatography-mass spectrometry. Anal Bioanal Chem 405:3921–3928
Rogge MC, Solomon WR, Sedman AJ, Welling PG, Toothaker RD, Wagner JG (1988) The theophylline-enoxacin interaction: I. Effect of enoxacin dose size on theophylline disposition. Clin Pharmacol Ther 44:579–587
Kharasch ED, Walker A, Hoffer C, Sheffels P (2005) Sensitivity of intravenous and oral alfentanil and pupillary miosis as minimally invasive and noninvasive probes for hepatic and first-pass CYP3A activity. J Clin Pharmacol 45:1187–1197
Backman JT, Kivistö KT, Olkkola KT, Neuvonen PJ (1998) The area under the plasma concentration-time curve for oral midazolam is 400-fold larger during treatment with itraconazole than with rifampin. Eur J Clin Pharmacol 54:53–58
Wood AJJ, Kornhauser DM, Wilkinson GR, Shand DG, Branch RA (1978) The influence of cirrhosis on steady-state blood concentrations of unbound propranolol after oral administration. Clin Pharmacokinet 3:478–487
Acknowledgements
The authors thank the UCSF PharmD Class of 2021 for their understanding, questions and patience in the presentation of the material presented here. This work was supported in part by a Mary Ann Koda-Kimble Seed Award for Innovation. Dr. Benet is a member of the UCSF Liver Center supported by NIH grant P30 DK026743. Ms. Bowman was supported by the National Science Foundation Graduate Research Fellowship Program (Grant 1144247) and a Pharmaceutical Research and Manufacturers of America Foundation Pre-doctoral Fellowship in Pharmaceutics. Ms. Koleske was supported in part by NIGMS grant R25 GM56847. Ms. Rinaldi was supported by the National Science Foundation Graduate Research Fellowship Program (Grant 1650113). Ms. Sodhi was supported in part by an American Foundation for Pharmaceutical Education Predoctoral Fellowship and NIGMS grant R25 GM56847.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Benet, L.Z., Bowman, C.M., Koleske, M.L. et al. Understanding drug–drug interaction and pharmacogenomic changes in pharmacokinetics for metabolized drugs. J Pharmacokinet Pharmacodyn 46, 155–163 (2019). https://doi.org/10.1007/s10928-019-09626-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-019-09626-7