Abstract
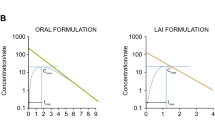
Half-life (t 1/2) is the oldest but least well understood pharmacokinetic parameter, because most definitions are related to hypothetical 1-compartment body models that don’t describe most drugs in humans. Alternatively, terminal half-life (t 1/2,z) is utilized as the single defining t 1/2 for most drugs. However, accumulation at steady state may be markedly over predicted utilizing t 1/2, z. An apparent multiple dosing half-life (t 1/2, app) was determined from peak and trough steady-state ratios and found to be significantly less than reported terminal t 1/2s for eight orally dosed drugs with t 1/2,z values longer than one day. We define a new parameter, “operational multiple dosing half-life” (t 1/2, op), as equal to the dosing interval at steady-state where the maximum concentration at steady-state is twice the maximum concentration found for the first dose. We demonstrate for diazepam that the well-accepted concept that t 1/2,z representing the great majority of the AUC will govern accumulation can be incorrect. Using oral diazepam, we demonstrate that t 1/2, op is remarkably sensitive to the absorption t 1/2, even when this absorption t 1/2 is much less than t 1/2,z, and describe the relevance of this in designing extended release dosage forms. The t 1/2, op is compared with previously proposed half-lives for predicting accumulation.

Similar content being viewed by others
Abbreviations
- AUC:
-
area under the curve
- AUMC:
-
area under the moment curve
- EHL:
-
effective half-life
- MRT:
-
mean residence time in the body
- MRTc :
-
mean residence time in the central compartment
- Rc :
-
Wagner’s drug accumulation index
- sd:
-
single dose
- ss:
-
steady-state
References
L. L. Brunton, J. S. Lozo, and K. L. Parker. Goodman and Gilman’s The Pharmacological Basis of Therapeutics, 11th edn. McGraw-Hill Medical, New York, NY, 2006.
C. F. Lacy, L. L. Armstrong, M. P. Goldman, and L. L. Lance. Drug Information Handbook. A Comprehensive Resource for all Clinicians and Healthcare Professionals, 17th edn. Lexi-Comp, Hudson, OH, 2008–2009.
L. Z. Benet. Multiple dosing half-life. A composite term useful in designing therapeutic regimens. Presented at The Third Japanese–American Conference on Pharmacokinetics and Biopharmaceutics, Kyoto, Japan (1985), as available through reference 4.
J. G. Wagner. Dosage intervals based on mean residence times. J. Pharm. Sci. 76:35–38 (1987). doi:10.1002/jps.2600760111.
P. Veng-Pedersen, and N. B. Modi. Optimal extravascular dosing intervals. J. Pharmacokinet. Biopharm. 19:405–412 (1991). doi:10.1007/BF01061664.
K. C. Kwan, N. R. Bohidar, and S. S. Hwang. Estimation of an effective half-life. In L. Z. Benet, G. Levy, and B. Ferraiolo (eds.), Pharmacokinetics: A Modern View, Plenum, New York, NY, 1984, pp. 147–162.
H. G. Boxenbaum, and M. Battle. Effective half-life in clinical pharmacology. J. Clin. Pharmacol. 35:763–766 (1995).
J. G. Wagner. Drug accumulation. J. Clin. Pharmacol. 7:84–88 (1967).
W. A. Colburn. Pharmacokinetic analysis of concentration time data obtained following administration of drugs that are recycled in the bile. J. Pharm. Sci. 73:313–317 (1984). doi:10.1002/jps.2600730308.
A. Hsu, G. R. Granneman, G. Witt, C. Locke, J. Denissen, A. Molla, J. Valdes, J. Smith, K. Erdman, N. Lyons, P. Niu, J.-P. Decourt, J.-B. Fourtillan, J. Girault, and J. M. Leonard. Multiple-dose pharmacokinetics of ritonavir in human immunodeficiency virus-infected subjects. Antimicrob. Agents Chemother. 41:898–905 (1997).
L. Z. Benet. Pharmacokinetics and metabolism of bepridil. Am. J. Cardiol. 55:8C–13C (1985). doi:10.1016/0002-9149(85)90799-4.
P. Augustijns, P. Geusens, and N. Verbeke. Chloroquine levels in blood during chronic treatment of patients with rheumatoid arthritis. Eur. J. Clin. Pharmacol. 42:429–433 (1992).
P. Colleste, M. Garle, M. D. Rawlins, and F. Sjoqvist. Interindividual differences in chlorthalidone concentration in plasma and red cells of man after single and multiple doses. Eur. J. Clin. Pharmacol. 9:319–325 (1976). doi:10.1007/BF00561667.
S. A. Kaplan, M. L. Jack, K. Alexander, and R. E. Weinfeld. Pharmacokinetic profile of diazepam in man following single intravenous and oral and chronic oral administrations. J. Pharm. Sci. 16:1789–1796 (1973). doi:10.1002/jps.2600621111.
K. Budde, H. H. Neumayer, G. Lehne, M. Winkler, I. A. Hauser, A. Lison, L. Fritsche, J. P. Soulillou, P. Fauchald, J. Dantal, and RADW 102 Renal Transplant Study Group. Tolerability and steady-state pharmacokinetics of everolimus in maintenance renal transplant patients. Nephrol. Dial. Transplant. 19:2606–2614 (2004). doi:10.1093/ndt/gfh322.
D. A. L. Newcombe, F. Bochner, J. M. White, and A. A. Somogyi. Evaluation of levo-alpha-acetylmethdol (LAAM) as an alternative treatment for methadone maintenance patients who regularly experience withdrawal: a pharmacokinetic and pharmacodynamic analysis. Drug Alcohol Depend. 76:63–72 (2004). doi:10.1016/j.drugalcdep.2004.04.004.
R. C. Li, P. K. Narang, I. Poggesi, and M. Strolin-Benedetti. A model based assessment of redistribution dependent elimination and bioavailability of rifabutin. Biopharm. Drug Dispos. 17:223–236 (1996). doi:10.1002/(SICI)1099-081X(199604)17:3<223::AID-BDD954>3.0.CO;2-S.
J. J Zimmerman, and B. D. Kahan. Pharmacokinetics of sirolimus in stable renal transplant patients after multiple oral dose administration. J. Clin. Pharmacol. 37:405–415 (1997).
S. Dhillon, and A. Richens. Pharmacokinetics of diazepam in epileptic patients and normal volunteers following intravenous administration. Br. J. Clin. Pharmacol. 12:841–844 (1981).
M. Iwamoto, L. A. Wenning, A. S. Petery, M. Laethem, M. De Smet, J. T. Kost, S. A. Merschman, K. M. Strohmaier, S. Ramael, K. C. Lasseter, J. A. Stone, K. M. Gottesdiener, and J. A. Wagner. Safety, tolerability, and pharmacokinetics of raltegravir after single and multiple doses in healthy subjects. Clin. Pharmacol. Ther. 83:293–299 (2008). doi:10.1038/sj.clpt.6100281.
J. Boni, J. M. Korth-Bradley, L. S. Richards, S. T. Chiang, D. R. Hicks, and L. Z. Benet. Chiral bioequivalence: effect of absorption rate on racemic etodolac. Clin. Pharmacokinet. 39:459–469 (2000). doi:10.2165/00003088-200039060-00006.
P. Macheras, M. Symillides, and C. Repos. An improved intercept method for the assessment of absorption rate in bioequivalence studies. Pharm. Res. 13:1755–1758 (1996). doi:10.1023/A:1016421630290.
F. H. Dost. Der Blutspiegel. Thieme, Leipzig, 1953, pp. 252–255.
L. Z. Benet. General treatment of linear mammillary models with elimination from any compartment as used in pharmacokinetics. J. Pharm. Sci. 61:536–541 (1972). doi:10.1002/jps.2600610408.
J. M. Bailey. Context-sensitive half-times. What are they and how valuable are they in anaesthesiology. Clin. Pharmacokinet. 41:793–799 (2002). doi:10.2165/00003088-200241110-00001.
Acknowledgements
Drs. Sahin and Benet were supported in part during the course of this work by NIH Grant R21 GM75900. The authors appreciate the critical reviews of this work as it progressed and the suggestions of Drs. Malcolm Rowland, Nicholas Holford, Harold Boxenbaum, Svein Øie and Stephen Hwang. Thanks also to Ms. Anita Grover for sharing her preliminary evaluations of everolimus and bepridil simulations with changing absorption rate.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sahin, S., Benet, L.Z. The Operational Multiple Dosing Half-life: A Key to Defining Drug Accumulation in Patients and to Designing Extended Release Dosage Forms. Pharm Res 25, 2869–2877 (2008). https://doi.org/10.1007/s11095-008-9787-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-008-9787-9