Abstract
Literature proposes numerous initiatives for optimization of the Operating Room (OR). Despite multiple suggested strategies for the optimization of workflow on the OR, its patients and (medical) staff, no uniform description of ‘optimization’ has been adopted. This makes it difficult to evaluate the proposed optimization strategies. In particular, the metrics used to quantify OR performance are diverse so that assessing the impact of suggested approaches is complex or even impossible. To secure a higher implementation success rate of optimisation strategies in practice we believe OR optimisation and its quantification should be further investigated. We aim to provide an inventory of the metrics and methods used to optimise the OR by the means of a structured literature study. We observe that several aspects of OR performance are unaddressed in literature, and no studies account for possible interactions between metrics of quality and efficiency. We conclude that a systems approach is needed to align metrics across different elements of OR performance, and that the wellbeing of healthcare professionals is underrepresented in current optimisation approaches.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Operating Room (OR) performance optimization is investigated from many angles and numerous different strategies are proposed. Think hereby of new systems based on data analysis that enable more efficient OR scheduling. However, many of these promising initiatives that are meant to improve the OR do not seem to land in practice [1]. Suggested changes do not always fit the overall workflow of the OR, or they solve the targeted problem ineffectively. Creating a support base amongst the people that implement or work with the innovation also tends to be problematic [2]. To enable improvement of OR performance with innovations that fit well in practice, it should be clear what is exactly meant with the term OR performance. Furthermore, to know if an innovation improves overall OR performance, one must know how to measure the overall performance. Below, we discuss what OR performance means according to literature and which elements it contains. Next, to investigate how to measure OR performance we make an inventory of the metrics used in literature to measure OR performance. Finally, to investigate how the field approaches OR performance optimization, we collected studies on this topic and addressed what methods were used and what aspect of OR performance the research focussed on. Besides perspectives on patients and healthcare professionals, we also consider economic perspectives on the OR on hospital budgets.
Pressures for change in the OR
The OR comprises a complex environment with multi-layered social interactions, unpredictability and a low tolerance for mistakes [3]. Irregularities in the workflow are often triggered by a combination of factors such as demanding caseloads, pressure to perform complex tasks and conflicting priorities. This can result in increased mental strain and stress amongst the healthcare professionals [4].
Irregularities in workflow on the OR also impact patients. Approximately 60% of the patients visit the OR at some point during their hospital stay [5]. Undergoing hospital admission and an operation makes many people experience emotions such as nervousness, agitation and uncertainty. Irregularities in the process can worsen this [6].
Accounting for about 35% to 40% of the costs, the OR is a large contributor to a hospital’s finances, also being one of the most costly units [7,8,9]. Over the past years, healthcare costs have increased and diminishing returns have prompted healthcare administrators to alleviate institutional costs through reductions in budget allocations [10].
Partly driven by the increasing demands for care on the one hand, and constrained resources on the other, a technological evolution has taken place over the last decades. This has played an important role in the development of surgery and resulted in dramatic changes in working conditions within the OR [11]. But healthcare professionals are not always prepared for this transformation of their work. Healthcare professionals are reported to lack preparation for radical (technical) changes in their work [12].
Despite the growing influx of new healthcare professionals, the sector experiences a major exodus of healthcare professionals. Causes are the heavy workload and a lack of autonomy. The limited autonomy of healthcare professionals in their daily work is appointed as a long-standing issue [12]. Research from the Dutch doctors organisation De Jonge Dokter has interviewed 622 young doctors about their work. About 50% of the interviewees has thought about quitting their job due to high work pressure, emotional pressure and working culture [13].
The impact of the workflow of the OR on patients, pressure on healthcare professionals that work on the OR, the vast changing work environment and economical constraints make that optimizing the OR is high on the academic agenda. However, the high expectations of patients, interactions between different professionals, unpredictability and complex surgical case scheduling make managing and changing the system difficult. Attempts to resort to commonly used industrial principles to increase factors such as efficiency have been demonstrated to easily fail due to these (and possibly other) particular characteristics of the OR [7]: human factors have too great of an impact to standardize and automate certain OR processes. Another complicating factor is the divergent perspectives on OR performance optimization.
OR performance optimization metrics
The metrics used to quantify OR performance optimization reported in literature are diverse [14]. Many articles focus on the efficiency aspect of OR performance optimization, some focus more on the quality aspects. For example, the work of Bellini et al. [7] speaks of the optimization related factor efficiency in the sense of more precise scheduling and limiting waste of resources. Costa Jr. et al. (2015) speak of both efficiency and optimization, hereby focussing on resources and time management. Sandbaek et al. [16] refer to OR efficiency as maximizing throughput and OR utilization while minimizing overtime and waiting time, without additional resources. Tanaka et al. (2011) assesses OR performance using indicators such as the number of operations, the procedural fees per OR, the total utilization time per OR and total fees per OR. Rothstein & Raval [3] refer to the metrics of OR efficiency based on the Canadian Paediatric Wait Times Project: off-hours surgery, same-day cancellation rate, first case start-time accuracy, OR use, percentage of unplanned closures, case duration accuracy, turnover time and excess staffing costs. Alternatively, Arakelian, Gunningberg and Larsson (2008) emphasize that apart from cost-effectiveness, work in the OR should be organized to fulfil the demands on patient safety and high-quality care. From their perspective, OR departments must create efficient ways of planning and processing the work, while at the same time maintaining the quality of care. These authors also show that there are diverging perspectives among OR personnel on what efficiency and productivity entail.
The previous paragraphs illustrate that when speaking about OR performance optimization, different terminology is being used. Furthermore, although many studies focus on how to optimize or monitor certain aspects of the OR, studies on the impact of these changes on the quality and efficiency of the hospital as a whole appear to be lacking. This may lead to uncertain optimisation strategies that are difficult to substantiate with supporting evidence [15]. Table 1 summarizes both quality and efficiency aspects of OR workflow and strives to align the methods and metrics to assess OR performance in terms of 1. Patient safety 2. Quality of care 3. Cost-effectiveness and 4. Healthcare professional well-being.
Method
A systematic literature review was conducted to make an inventory of metrics for optimization of the OR in literature. We used the search engines Scopus, Web of Science and PubMed with the search terms: “Operation Room” AND Optimization and Workflow AND Optimization AND Hospital. We limited the search to articles that discuss ways to optimize the OR as a system, not the performed medical interventions themselves. Furthermore, articles that were not written in the English language or did not belong to the category healthcare or medicine were excluded.
Analysis
An inventory of the topics of the articles was made by filtering out 1. the focus/aim of the study, 2. the method used and 3. the conclusion. Optimization strategies in other hospital departments might be transferable to the OR as well. Therefore, to gain insight in the distribution of optimization strategies on the different departments of the hospital, the articles were analysed by labelling the operational department the research is focussed on, which topic was investigated, and which method was used. After creating this overview, only data about the OR was used. To obtain OR performance metrics a second analysis was conducted: OR performance characteristics from the articles were split into aspects with their corresponding metrics.
Coding nodes
Overall categories for departments, topics and methods were identified based on the first 50 articles, as the authors felt a saturation rate for new categories was reached. The remaining articles were then labelled within these categories. To illustrate, Table 2 shows two sections that were both labelled as the metric T_3 and two sections that were labelled as the method M_8.
Coding the articles
Some articles mention multiple topics or methods. If multiple topics were mentioned, the article was labelled for the topic which had the most emphasis. This is illustrated in Example 1, where both the topics patient throughput and costs are mentioned. However, the emphasis is on patient throughput. For topics the article was therefore labelled as T_3: Optimize patient flow.
When labelling the articles for their method, it occurred that an article investigates an optimization possibility and method by means of a literature study. The method of the article was then labelled as literature study. In Example 2, the article investigates how workflow can be improved by identifying the potential failures of the system by means of a management tool. However, the effects of the management system on workflow are investigated by a literature study. For methods the article was therefore labelled as M_1: Literature study. In the results the coded articles are displayed in 3 sunburst graphs: the first shows the distribution of methods and topics of all hospital departments, the second contains the distribution of methods and topics on the OR. To elucidate the OR data, the third graph shows a selection with the biggest categories of the second sunburst (categories with N ≥ 3). Some of the smaller categories are illustrated with examples in the text.
Validation
The labelling was performed independently by two of the authors. Discrepancies were discussed and adjusted by obtaining consensus.
Example 1: “In most hospitals, patients move through their operative day in a linear fashion, starting at registration and finishing in the recovery room. Given this pattern, only 1 patient may occupy the efforts of the operating room team at a time. By processing patients in a parallel fashion, operating room efficiency and patient throughput are increased while costs remain stable” [18].
Example 2: “Failure mode and effects analysis (FMEA) is a valuable reliability management tool that can pre-emptively identify the potential failures of a system and assess their causes and effects, thereby preventing them from occurring. The use of FMEA in the healthcare setting has become increasingly popular over the last decade, being applied to a multitude of different areas. The objective of this study is to review comprehensively the literature regarding the application of FMEA for healthcare risk analysis” [21].
Results
In this section, the results of the inventory of OR performance metrics and the addressed OR performance topics in literature are shown.
Review statistics
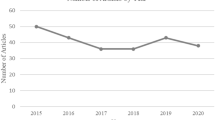
Figure 1 shows the search engines, search terms and number of papers found.
OR performance metrics
Based on Table 1, the characteristics of OR performance (efficiency and quality) have been split up into aspects and were then further specified into metrics (Table 3).
Addressed OR performance topics in literature
Table 4 shows the categories used to analyse the articles, the corresponding labels and their names. In Appendix 1, Supp. Tab. 1, the topic category and their corresponding sources are presented.
Distribution of the labels
Appendix 2, Supp. Figure 1, shows a sunburst graph that illustrates the distribution of the labels per department (D_x). To give an overview that represents the distribution of departments in a hospital, only the data from the second search criteria (Workflow AND Optimization AND Hospital) was included in this graph. The inner circle contains the different departments, namely the OR, ER (emergency room), outpatient clinic, patient clinic and the hospital in general. The middle circle shows the corresponding methods, the outer circle shows the topics. Most articles focus on the OR (D_1, N = 16). The ER receives less attention (D_2, N = 2). There were no articles that were labelled for outpatient clinic (D_3).
In Appendix 2, Supp. Figure 2 zooms in on methods and corresponding topics of just the OR. This graph includes all OR data from both search criteria and shows the methods, topics and number of articles in each category. In Fig. 2, a selection of the OR sunburst graph is displayed. This selection contains the most frequent combination of period, method and topic (N ≥ 3). Most articles have the aim to optimize scheduling (N = 7), workflow tracking (N = 5) and patient flow (N = 4) by computational means such as machine learning.
All data was then stratified by the means of a bar chart. Figure 3 shows the data while looking at different methods per topic. Computational methods (M_8) are used most frequently (N = 41).
The methods that were used the least are experiments with the medical staff (M_7, N = 2) and system engineering (M_10, N = 2). The most investigated topics are patient flow (T_10, N = 18), OR scheduling (T_3, N = 17) and workflow tracking systems (T_5, N = 15).
Discussion
In this study we addressed what methods were used in other studies, what aspect of OR performance they focussed on, and for which department the effects were to be relevant. We aimed to investigate how the field approaches OR performance optimization and to create an overview of OR performance metrics for the categories of patient safety, quality of care, cost-effectiveness, and the well-being of healthcare professionals.
Most studies focused on patient safety, quality of care and cost-effectiveness. This might be explained by the fact that healthcare has a central focus on patient wellbeing and clinical outcome measures. One striking result from this study is that the well-being of healthcare professionals is largely ignored in OR optimization studies. Ill-performing in these areas may contribute to staff shortages. Therefore, we deliberately added the well-being of healthcare professionals as a crucial aspect of OR performance as we feel that this is a subject that must be taken in account in OR optimisation.
By taking all four categories within OR performance as a starting point for the delineation of the ways to measure OR performance, we strive to create an all-encompassing overview of relevant metrics in literature. More metrics were found for efficiency than for quality aspects. This was as expected because efficiency tends to be easier to measure than quality aspects. Furthermore, quality metrics are often subjective. For instance, well-being of healthcare professionals, is linked to the metric autonomy (freedom to make your own choices, plan your workday etc.). This is a capacity that is difficult to quantify in a valid and reliable way.
Considering the research topics addressed in literature it was found that most articles have the aim to optimize OR scheduling, Workflow tracking or Patient flow by computational means, such as machine learning. Thanks to greater computing power, as well as the growing availability of large amounts of data, machine learning holds the promise to make sense of complex modelling tasks [24]. Topics such as OR scheduling, Workflow tracking and Patient flow fit this picture. They are suitable for computational simulations and optimizations of complex systems such as the OR that are characterised by high variability in the timing and alignment of processes.
Categories that involve experiments with healthcare professionals (such as interventions in practice) were only limitedly represented in the literature. With AI on the rise, it seems a logical choice to use simulations to test optimizations instead of occupying the (often overworked) healthcare professionals. However, although simulated efficacy trials have generated many possible interventions to improve healthcare, their impact on practice and policy is limited so far [25]. Establishing and conveying the credibility of computational modelling and simulation outcomes is a delicate task [26] and the step from simulation to implementation in practice turns out to be a difficult one.
Kessler & Glasgow point out that healthcare research must deal with “wicked” problems that are multilevel, multiply determined, complex and interacting. Research tends to isolate, decontextualize and simplify issues in order to be able to investigate them. Consequently, the small number of studies with representative populations, staff and settings that substantiate optimisation approaches is in sheer contrast with the large number of papers that promote the potential of computational methods.
Overall, similar to what Fong et al. (2016) report, timepoints, cost, methodology and outcome measures were inconsistent across the studies in this review, and it appears that multiple metrics can fit a topic. Nevertheless, the topics of the articles cited in this review give insightful handles of how to structure OR performance metrics. Increasing awareness about these topics and metrics amongst the people who work with them is therefore of value.
Awareness should also be increased about the definitions of the concepts of OR performance [17]. It is important to realize that the term “OR performance” only describes a snapshot in time but extents across all topics. Some studies talk about performance, but do not always specify if there is change in this performance. Change can only be measured over time. When doing so, clear criteria are required to determine if the change is also an improvement. In one context something might be an improvement, in another it might worsen the situation [27].
The ideal scenario would be to optimize an OR performance topic for all the metrics from Table 3. However, this may not always be attainable. A sensible approach is to apply relevant metrics both at the beginning of your project and after your intervention in the system, and to evaluate the impact on all four categories of OR performance. By prioritizing and assigning weights to metrics acceptable ranges for the optimisation outcomes could be defined. When looking at optimization in this way, it should comprise two elements: improvement on a (set of) metric(s) and an improvement of the total system after your intervention.
This approach is illustrated in Fig. 4, where on the left the hypothetical optimization of one metric is shown, and on the right the same change of the metric is shown, together with another metric of the system. When, for example, one chooses to optimize OR performance by increasing the metric Number of operations per OR per month, you aim for point A in Fig. 4. However, Fig. 4 also illustrates that an increase along one metric could mean a (unintended) decrease on another. When taking other metrics into account you can see it is actually point B you are aiming for. Therefore, measuring every metric before and after your intervention to monitor the impact on the total system is essential for a thorough validation of its appropriateness.
Modelling the metrics
Optimizing the system for a certain metric while also considering the other metrics should be part of the optimization strategy. Practical execution of this strategy is a roadmap with design steps in which the metrics are incorporated. In the following paragraphs this idea will be illustrated with Fig. 5 and an example scenario for an optimization goal.
Figure 5 shows an example of the main steps of a research approach (aim, method, data collection, results, conclusion) with an emphasis on the phase between method and data collection. The approach is based on the Plan-Do-Check-Act method of Deming [28]. In a fictitious scenario the aim of the project is to improve the well-being of healthcare professionals on the OR. This is the first step of the model in Fig. 5. In second step it is determined that the method used to achieve the aim will be increasing the metric autonomy of the healthcare professionals. A questionnaire amongst the staff involved shows that the healthcare professionals would like to have more autonomy over when they work. A more open work schedule is therefore suggested.
In the third step of the model the most important metrics that could be affected by this change are listed by the researchers:
-
Excess staffing costs (often caused by over- or under-utilization of the OR).
-
OR utilization
-
Quality of care and patient safety
-
Autonomy
In the fourth step the selected metrics are combined in logical sets as system optimisation metrics with assigned weights and acceptance ranges. As an example, we could look at optimizing OR utilization. In this case the constant consists of the metric off time per OR per month and the utility time per OR per month (see Eq. 1).
Ranges of the constant are then given scores and weights to calculate the optimal value (Table 5). For example, if T* were to be greater than 1, there would be more off time per OR than utility time. That is an undesirable scenario. This range is therefore given a score of -1 and a weight of 2.
When T* is low there is a high utility rate of the OR’s. When T* is high there is a low utility rate. A more complete overview would be created when also plotting financial metrics and metrics concerning the well-being of the medical staff.
After data has been collected in step 5 of the model, the results of step 6 can be compared in step 7. One can then evaluate whether the intended innovation will improve the system in such a way that it is worth the investment. And if not, consider carefully based on the metric overviews where adjustments to the intervention are required.
Limitations
This study has limitations. A major focus of this paper is the importance of seeing the whole picture when doing research. We have given examples of possibilities to bring this way of doing research into practice. However, despite the broad view of this study, we did not cover all aspects of healthcare. We looked at just the OR. Following our own philosophy, we want to stress that an even broader scope is relevant for successful optimization in healthcare. There is an intricate interplay between the different departments of a hospital. Increasing the efficiency of the OR might, for example, cause trouble in the timetable of the PACU (Post Anaesthesia Care Unit).
Concluding remarks
In this study it was found that there are many different perspectives and approaches used to optimize OR performance. The metrics used to optimize OR performance are diverse. Based on our inventory of the metrics and methods used in literature we conclude that part of the crucial aspects of OR performance, such as the wellbeing of healthcare professionals, are underrepresented in the research field. The lack of studies that account for possible interactions between metrics of quality and efficiency have limited the impact of optimisation approaches. Too much focus on one metric potentially deteriorates other elements of the system you try to optimize. To obtain profitable OR optimization, a systems approach that aligns metrics across functions and better representation of the wellbeing of healthcare professionals are needed.
Future research
An informative topic to investigate further is to test the effect of awareness of metrics when optimizing OR metrics in practice. The hypothesis here is that more awareness of OR performance metrics and their correlations amongst researchers could lead to better optimizing strategies. In this context, the model in Fig. 5 might also be tested. Does it increase awareness? Do researchers use different approaches with the model than without? Does this lead to better outcomes?
Another direction is the continuous measuring of OR performance metrics to be able to monitor unintended interactions, in ways that not put a burden on healthcare professionals (i.e., increasing administrative tasks). Furthermore, technology can speed up and smoothen processes within the OR, but the impact on perioperative processes might not have been considered. An interesting way to put these thoughts to practice is investigating how the increase of technology on the OR has influenced the work of healthcare professionals such as OR nurses and supporting department.
Abbreviations
- OR:
-
Operating Room
- FMEA:
-
Failure mode and effects analysis
- VSM:
-
Value Stream Mapping
- ER:
-
Emergency Room
- OSH:
-
Occupational Safety and Health
- PACU:
-
Post Anaesthesia Care Unit
References
Cassidy CE, Harrison MB, Godfrey C, Nincic V, Khan PA, Oakley P, et al. Use and effects of implementation strategies for practice guidelines in nursing: a systematic review. Implementation Science. 2021;16(1):1–29.
Hellström A, Lifvergren S, Quist J. Applying Process Management in Healthcare – Investigating Implementation Difficulties. J Quist - International Annual EurOMA . 2009;(June 2014):1–10.
Rothstein DH, Raval M V. Operating room efficiency. Seminars in Pediatric Surgery. 2018;27(2):79–85.
Wheelock A, Suliman A, Wharton R, Babu ED, Hull L, Vincent C, et al. The impact of operating room distractions on stress, workload, and teamwork. Annals of Surgery. 2015;261(6):1079–84.
Clavel D, Mahulea C, Albareda J, Silva M. A decision support system for elective surgery scheduling under uncertain durations. Applied Sciences (Switzerland). 2020;10(6):1–21.
Landon PM, Lazar J, Heylighen A, Dong H. Inclusive Designing. Springer International Publishing. 2014.
Bellini V, Guzzon M, Bigliardi B, Mordonini M, Filippelli S, Bignami E. Artificial Intelligence: A New Tool in Operating Room Management. Role of Machine Learning Models in Operating Room Optimization. Journal of Medical Systems. 2019;44(1):1–10.
Cima RR, Brown MJ, Hebl JR, Moore R, Rogers JC, Kollengode A, et al. Use of Lean and Six Sigma Methodology to Improve Operating Room Efficiency in a High-Volume Tertiary-Care Academic Medical Center. ACS. 2011;213(1):83–92.
Lovejoy WS, Li Y. Hospital operating room capacity expansion. Management Science. 2002;48(11):1369–87.
Boggs SD, Tan DW, Watkins CL, Tsai MH. OR Management and Metrics: How It All Fits Together for the Healthcare System. Journal of Medical Systems. 2019;43(6).
Matern U, Koneczny S. Safety, hazards and ergonomics in the operating room. Surgical Endoscopy and Other Interventional Techniques. 2007;21(11):1965–9.
SER. The Future of Dutch Healthcare: A Study. Social and Economic Council. 2020;2(1):1–13.
NOS. Helft jonge artsen denkt weleens aan stoppen door hoge werkdruk [Internet]. 2020 [cited 2021 Jul 26]. Available from: https://nos.nl/artikel/2343153-helft-jonge-artsen-denkt-weleens-aan-stoppen-door-hoge-werkdruk
Fong AJ, Smith M, Langerman A. Efficiency improvement in the operating room. Journal of Surgical Research. 2016;204(2):371–83.
Marang-van de Mheen PJ, Putter H, Bastiaannet E, Bottle A. Competing risks in quality and safety research: a framework to guide choice of analysis and improve reporting. BMJ Quality & Safety. 2021 Dec;30(12):1031–7.
Sandbaek BE, Helgheim BI, Larsen OI, Fasting S. Impact of changed management policies on operating room efficiency. BMC health services research. 2014;14:224.
Arakelian E, Gunningberg L, Larsson J. Job satisfaction or production? How staff and leadership understand operating room efficiency: A qualitative study. Acta Anaesthesiologica Scandinavica. 2008;52(10):1423–8.
Friedman DM, Sokal SM, Chang Y, Berger DL. Increasing Operating Room Efficiency Through Parallel Processing. Annals of Surgery •. 2006;243(1).
Assad DBN, Spiegel T. Maximizing the efficiency of residents operating room scheduling: A case study at a teaching hospital. Production. 2019;29.
Al-Refaie A, Chen T, Judeh M. Optimal operating room scheduling for normal and unexpected events in a smart hospital. Operational Research. 2018;18(3):579–602.
Liu HC, Zhang LJ, Ping YJ, Wang L. Failure mode and effects analysis for proactive healthcare risk evaluation: A systematic literature review. Journal of Evaluation in Clinical Practice. 2020;26(4):1320–37.
Tanaka M, Lee J, Ikai H, Imanaka Y. Development of efficiency indicators of operating room management for multi-institutional comparisons. Journal of Evaluation in Clinical Practice. 2013;19(2):335–41.
Rhee D, Zhang Y, Papandria D, Ortega G, Abdullah F. Agency for healthcare research and quality pediatric indicators as a quality metric for surgery in children: Do they predict adverse outcomes? Journal of Pediatric Surgery. 2012;47(1):107–11.
Yu K-H, Beam AL, Kohane IS. Artificial intellegence in healthcare. Nature Biomedical Engineering. 2018;(2):719–31.
Kessler R, Glasgow RE. A proposal to speed translation of healthcare research into practice: Dramatic change is needed. American Journal of Preventive Medicine. 2011;40(6):637–44.
Erdemir A, Mulugeta L, Ku JP, Drach A, Horner M, Morrison TM, et al. Credible practice of modeling and simulation in healthcare: Ten rules from a multidisciplinary perspective. Journal of Translational Medicine. 2020;18(1):1–18.
Austin PC, Ceyisakar IE, Steyerberg EW, Lingsma HF, Marang-Van De Mheen PJ. Ranking hospital performance based on individual indicators: Can we increase reliability by creating composite indicators? BMC Medical Research Methodology. 2019 Jun 26;19(1).
Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Quality and Safety. 2014;23(4):290–8.
Duncan PG, Overdyk FJ, Harvey SC, Shippey F, Carolina S. Successful Strategies for Improving Efficiency at Academic Institutions. 1998;896–906.
Jreije K, Sachdeva S, Cull M, Diaz G, Romero J, Schweitzer J. Rewarding On Time Start Times in Operating Rooms Improves Efficiency. American Surgeon. 2020;86(10):1391–5.
Bas E. An integrated OSH risk management approach to surgical flow disruptions in operating rooms. Safety Science. 2018;109(September 2017):281–93.
Kaddoum R, Fadlallah R, Hitti E, El-Jardali F, El Eid G. Causes of cancellations on the day of surgery at a Tertiary Teaching Hospital. BMC Health Services Research. 2016;16(1):1–8.
Saha P, Pinjani A, Al-Shabibi N, Madari S, Ruston J, Magos A. Why we are wasting time in the operating theatre? International Journal of Health Planning and Management. 2009;24(3):225–32.
Aghaebrahim A, Granja MF, Agnoletto GJ, Aguilar-Salinas P, Cortez GM, Santos R, et al. Workflow Optimization for Ischemic Stroke in a Community-Based Stroke Center. World Neurosurgery. 2019;129:e273–8.
Venema E, Boodt N, Berkhemer OA, Rood PPM, Van Zwam WH, Van Oostenbrugge RJ, et al. Workflow and factors associated with delay in the delivery of intra-arterial treatment for acute ischemic stroke in the MR CLEAN trial. Journal of NeuroInterventional Surgery. 2018;10(5):424–8.
Nemati S, Shylo O V., Prokopyev OA, Schaefer AJ. The surgical patient routing problem: A central planner approach. INFORMS Journal on Computing. 2016;28(4):657–73.
Ajmi F, Zgaya H, Othman S Ben, Hammadi S. Agent-based dynamic optimization for managing the workflow of the patient’s pathway. Simulation Modelling Practice and Theory. 2019;96(May):101935.
Hur Y, Bard JF, Morrice DJ. Appointment scheduling at a multidisciplinary outpatient clinic using stochastic programming. Naval Research Logistics. 2021;68(1):134–55.
J. Morrice D, F. Bard J, M. Koenig K. Designing and scheduling a multi-disciplinary integrated practice unit for patient-centred care. Health Systems. 2020;9(4):293–316.
Tlapa D, Zepeda-Lugo CA, Tortorella GL, Baez-Lopez YA, Limon-Romero J, Alvarado-Iniesta A, et al. Effects of Lean Healthcare on Patient Flow: A Systematic Review. Value in Health. 2020;23(2):260–73.
Markazi-Moghaddam N, Jame SZB, Tofighi E. Evaluating patient flow in the operating theater: An exploratory data analysis of length of stay components. Informatics in Medicine Unlocked. 2020;19:100354.
Baranova K, Torti J, Goldszmidt M. Explicit Dialogue about the Purpose of Hospital Admission Is Essential: How Different Perspectives Affect Teamwork, Trust, and Patient Care. Academic Medicine. 2019;94(12):1922–30.
Zhang H, Best TJ, Chivu A, Meltzer DO. Simulation-based optimization to improve hospital patient assignment to physicians and clinical units. Health Care Management Science. 2020;23(1):117–41.
Andersen AR, Nielsen BF, Reinhardt LB, Stidsen TR. Staff optimization for time-dependent acute patient flow. European Journal of Operational Research. 2019;272(1):94–105.
Kang CW, Imran M, Omair M, Ahmed W, Ullah M, Sarkar B. Stochastic-Petri net modeling and optimization for outdoor patients in building sustainable healthcare system considering staff absenteeism. Mathematics. 2019;7(6).
Berg E, Weightman AT, Druga DA. Emergency Department Operations II: Patient Flow. Emergency Medicine Clinics of North America. 2020;38(2):323–37.
Merchant RN. Slated versus actual operating room entry time in a British Columbia health authority. Canadian Journal of Anesthesia. 2020;67(6):726–31.
Yip K, Huang K, Chang S, Chui E. A mathematical optimization model for efficient management of Nurses’ Quarters in a teaching and referral hospital in Hong Kong. Operations Research for Health Care. 2016;8:1–8.
Sasanfar S, Bagherpour M, Moatari-Kazerouni A. Improving emergency departments: Simulation-based optimization of patients waiting time and staff allocation in an Iranian hospital. International Journal of Healthcare Management. 2020;0(0):1–8.
Harvey LFB, Smith KA, Curlin H. Physician Engagement in Improving Operative Supply Chain Efficiency Through Review of Surgeon Preference Cards. The Journal of Minimally Invasive Gynecology. 2015;24(7):1116–20.
Lau H, Dadich A, Nakandala D, Evans H, Zhao L. Development of a cost-optimization model to reduce bottlenecks: A health service case study. Expert Systems. 2018;35(6):1–13.
Lee DJ, Ding J, Guzzo TJ. Improving Operating Room Efficiency. Current Urology Reports. 2019;20(6).
Halim UA, Khan MA, Ali AM. Strategies to Improve Start Time in the Operating Theatre: a Systematic Review. Journal of Medical Systems. 2018;42(9).
Glennie RA, Barry SP, Alant J, Christie S, Oxner WM. Will cost transparency in the operating theatre cause surgeons to change their practice? Journal of Clinical Neuroscience. 2019;60:1–6.
Xiang W, Li C. Surgery scheduling optimization considering real life constraints and comprehensive operation cost of operating room. Technology and Health Care. 2015;23(5):605–17.
Robinson ST. Lean Strategies in the Operating Room. Anesthesiology Clinics. 2015;33(4):713–30.
Ramos P, Bonfá E, Goulart P, Medeiros M, Cruz N, Puceh-leão P, et al. Perioperative Care and Operating Room Management First-case tardiness reduction in a tertiary academic medical center operating room : A lean six sigma perspective. Perioperative Care and Operating Room Management. 2016;5(December):7–12.
Pegoraro F, Portela Santos EA, de Freitas Rocha Loures E, Laus FW. A hybrid model to support decision making in emergency department management. Knowledge-Based Systems. 2020;203:106148.
Hu X, Barnes S, Golden B. Applying queueing theory to the study of emergency department operations: a survey and a discussion of comparable simulation studies. International Transactions in Operational Research. 2018;25(1):7–49.
Niñerola A, Sánchez-Rebull MV, Hernández-Lara AB. Quality improvement in healthcare: Six Sigma systematic review. Health Policy. 2020;124(4):438–45.
Sommer AC, Blumenthal EZ. Implementation of Lean and Six Sigma principles in ophthalmology for improving quality of care and patient flow. Survey of Ophthalmology. 2019;64(5):720–8.
Crown W, Buyukkaramikli N, Sir MY, Thokala P, Morton A, Marshall DA, et al. Application of Constrained Optimization Methods in Health Services Research: Report 2 of the ISPOR Optimization Methods Emerging Good Practices Task Force. Value in Health. 2018;21(9):1019–28.
Mitteregger M, Köhler G, Szyszkowitz A, Uranitsch S, Stiegler M, Aigner F, et al. Increasing Operating Room Efficiency with Shop Floor Management: an Empirical, Code-Based, Retrospective Analysis. Journal of Medical Systems. 2020;44(9).
Baccei SJ, Henderson SR, Lo HS, Reynolds K. Using Quality Improvement Methodology to Reduce Costs while Improving Efficiency and Provider Satisfaction in a Busy, Academic Musculoskeletal Radiology Division. Journal of Medical Systems. 2020;44(6).
Letelier P, Guzmán N, Medina G, Calcumil L, Huencho P, Mora J, et al. Workflow optimization in a clinical laboratory using Lean management principles in the pre-analytical phase. Journal of Medical Biochemistry. 2021;40(1):26–32.
Campbell K, Louie P, Levine B, Gililland J. Using Patient Engagement Platforms in the Postoperative Management of Patients. Current Reviews in Musculoskeletal Medicine. 2020;13(4):479–84.
Conley J, Bohan JS, Baugh CW. The Establishment and Management of an Observation Unit. Emergency Medicine Clinics of North America. 2017;35(3):519–33.
Stepaniak P, Vrijland W, de Quelerij M, de Vries G, Heij C. Working With a Fixed Operating Room Team on Consecutive Similar Cases and the Effect on Case Duration and Turnover Time. 2010;145(12):1165–70.
Reznick D, Niazov L, Holizna E, Keebler A, Siperstein A. Perioperative Care and Operating Room Management Dedicated teams to improve operative room ef fi ciency. Perioperative Care and Operating Room Management. 2016;3:1–5.
Volpin A, Khan O, Haddad FS. Theater Cost Is £16/Minute So What Are You Doing Just Standing There? Journal of Arthroplasty. 2016;31(1):22–6.
Durojaiye AB, Levin S, Toerper M, Kharrazi H, Lehmann HP, Gurses AP. Evaluation of multidisciplinary collaboration in pediatric trauma care using EHR data. Journal of the American Medical Informatics Association. 2019;26(6):506–15.
Hicks C, Petrosoniak A. The Human Factor: Optimizing Trauma Team Performance in Dynamic Clinical Environments. Emergency Medicine Clinics of North America. 2018;36(1):1–17.
Kawaguchi AL, Kao LS. Teamwork and Surgical Team–Based Training. Surgical Clinics of North America. 2021;101(1):15–27.
Nanah A, Bayoumi AB. The pros and cons of digital health communication tools in neurosurgery: a systematic review of literature. Neurosurgical Review. 2020;43(3):835–46.
Harders M, Malangoni MA, Weight S, Sidhu T. Improving operating room efficiency through process redesign. 2006;509–16.
Koçkaya G, Koçkaya PD, Özbaǧriaçik Ö, Oba S. Improving cost-efficiency at a hospital by showing the time-saving effect of using different neuromuscular blockers for short operations. Journal of Pharmaceutical Health Services Research. 2014;5(1):61–6.
Lai HC, Chan SM, Lu CH, Wong CS, Cherng CH, Wu ZF. Planning for operating room efficiency and faster anesthesia wake-up time in open major upper abdominal surgery. Medicine (United States). 2017;96(7):1–5.
Navidi B, Kiai K. Efficiency and scheduling in the nonoperating room anesthesia suite: Implications from patient satisfaction to increased revenue operating room: A common (Dollars and Sense) approach. Current Opinion in Anaesthesiology. 2019;32(4):498–503.
Abouleish A, Hudson M, Whitten C. Measuring Clinical Productivity of Anesthsiology Groups. Anesthesiol. 2019;130(2):336–48.
Boggs SD, Barnett SR, Urman RD. The future of nonoperating room anesthesia in the 21st century: Emphasis on quality and safety. Current Opinion in Anaesthesiology. 2017;30(6):644–51.
Fairley M, Scheinker D, Brandeau ML. Improving the efficiency of the operating room environment with an optimization and machine learning model. Health Care Management Science. 2019;22(4):756–67.
Ringoir J, Van Biesen S, Pauwels J, Pannier E, Wouters P, Van de Velde M, et al. Improving compliance with hospital accreditation standards for anesthesia through repetitive feedback and education: a cross-sectional study. Acta Anaesthesiologica Belgica. 2019;70(3):119–28.
Ramme AJ, Hutzler LH, Cerfolio RJ, Bosco JA. Applying systems engineering to increase operating room efficiency. Bulletin of the Hospital for Joint Diseases. 2020;78(1):26–32.
Heider S, Schoenfelder J, McRae S, Koperna T, Brunner JO. Tactical scheduling of surgeries to level bed utilization in the intensive care unit. IISE Transactions on Healthcare Systems Engineering. 2020;5579:1–14.
Zhu S, Fan W, Yang S, Pei J, Pardalos PM. Operating room planning and surgical case scheduling: a review of literature. Journal of Combinatorial Optimization. 2019;37(3):757–805.
Morris AJ, Sanford JA, Damrose EJ, Wald SH, Kadry B, Macario A. Overlapping Surgery: A Case Study in Operating Room Throughput and Efficiency. Anesthesiology Clinics. 2018;36(2):161–76.
Bai M, Pasupathy KS, Sir MY. Pattern-based strategic surgical capacity allocation. Journal of Biomedical Informatics. 2019;94(August 2018):103170.
Wiyartanti L, Lim CH, Park MW, Kim JK, Kwon GH, Kim L. Resilience in the surgical scheduling to support adaptive scheduling system. International Journal of Environmental Research and Public Health. 2020;17(10).
Gür Ş, Eren T. Application of Operational Research Techniques in Operating Room Scheduling Problems: Literature Overview. Journal of Healthcare Engineering. 2018;2018.
Watanabe Y, Noguchi H, Nakata Y. How efficient are surgical treatments in Japan? The case of a high-volume Japanese hospital. Health Care Management Science. 2020;23(3):401–13.
Agnetis A, Coppi A, Corsini M, Dellino G, Meloni C, Pranzo M. Long term evaluation of operating theater planning policies. Operations Research for Health Care. 2012;1(4):95–104.
Park HS, Kim SH, Bong MR, Choi DK, Kim WJ, Ku SW, et al. Optimization of the Operating Room Scheduling Process for Improving Efficiency in a Tertiary Hospital. Journal of Medical Systems. 2020;44(9).
Fügener A, Schiffels S, Kolisch R. Overutilization and underutilization of operating rooms - insights from behavioral health care operations management. Health Care Management Science. 2017;20(1):115–28.
Devi SP, Rao KS, Sangeetha SS. Prediction of surgery times and scheduling of operation theaters in optholmology department. Journal of Medical Systems. 2012;36(2):415–30.
Ayala R, Ruiz G, Valdivielso T. Automatizing a nonscripting TPS for optimizing clinical workflow and reoptimizing IMRT/VMAT plans. Medical Dosimetry. 2019;44(4):409–14.
Neumuth T. Surgical process modeling. Innovative Surgical Sciences. 2020;2(3):123–37.
Tan A, Durbin M, Chung FR, Rubin AL, Cuthel AM, McQuilkin JA, et al. Design and implementation of a clinical decision support tool for primary palliative Care for Emergency Medicine (PRIM-ER). BMC Medical Informatics and Decision Making. 2020;20(1):1–11.
Wang C, Zhu X, Hong JC, Zheng D. Artificial Intelligence in Radiotherapy Treatment Planning: Present and Future. Technology in cancer research & treatment. 2019;18:1–11.
Souza TA, Roehe Vaccaro GL, Lima RM. Operating room effectiveness: a lean health-care performance indicator. International Journal of Lean Six Sigma. 2020;11(5):987–1002.
Nino V, Claudio D, Valladares L, Harris S. An enhanced kaizen event in a sterile processing department of a rural hospital: A case study. International Journal of Environmental Research and Public Health. 2020;17(23):1–20.
del Carmen León-Araujo M, Gómez-Inhiesto E, Acaiturri-Ayesta MT. Implementation and Evaluation of a RFID Smart Cabinet to Improve Traceability and the Efficient Consumption of High Cost Medical Supplies in a Large Hospital (Journal of Medical Systems, (2019), 43, 6, (178), https://doi.org/10.1007/s10916-019-1269-6). Journal of Medical Systems. 2019;43(12).
Ahmadi E, Masel DT, Metcalf AY, Schuller K. Inventory management of surgical supplies and sterile instruments in hospitals: a literature review. Health Systems. 2019;8(2):134–51.
Briatte I, Allix-Béguec C, Garnier G, Michel M. Revision of hospital work organization using nurse and healthcare assistant workload indicators as decision aid tools. BMC Health Services Research. 2019;19(1):1–9.
Antunes RS, Seewald LA, Rodrigues VF, Da Costa CA, Gonzaga L, Righi RR, et al. A survey of sensors in healthcare workflow monitoring. ACM Computing Surveys. 2018;51(2).
Koch A, Burns J, Catchpole K, Weigl M. Associations of workflow disruptions in the operating room with surgical outcomes: A systematic review and narrative synthesis. BMJ Quality and Safety. 2020;29(12):1033–45.
Chadebecq F, Vasconcelos F, Mazomenos E, Stoyanov D. Computer Vision in the Surgical Operating Room. Visceral Medicine. 2020;43–5.
Padoy N. Machine and deep learning for workflow recognition during surgery. Minimally Invasive Therapy and Allied Technologies. 2019;28(2):82–90.
Perez B, Lang C, Henriet J, Philippe L, Auber F. Risk prediction in surgery using case-based reasoning and agent-based modelization. Computers in Biology and Medicine. 2021;128(October 2020):1–11.
Tellis R, Starobinets O, Prokle M, Raghavan UN, Hall C, Chugh T, et al. Identifying Areas for Operational Improvement and Growth in IR Workflow Using Workflow Modeling, Simulation, and Optimization Techniques. Journal of Digital Imaging. 2021;34(1):75–84.
Wang Y, Yan F, Lu X, Zheng G, Zhang X, Wang C, et al. IILS: Intelligent imaging layout system for automatic imaging report standardization and intra-interdisciplinary clinical workflow optimization. EBioMedicine. 2019;44:162–81.
Spini G, van Heesch M, Veugen T, Chatterjea S. Private Hospital Workflow Optimization via Secure k-Means Clustering. Journal of Medical Systems. 2020;44(1).
Overmann K, Wu D, Xu C, Bindhu S, Barrick L. Real-time locating systems to improve healthcare delivery: A systematic review. Journal of the American Medical Informatics Association. 2021;
Kawamoto K, McDonald CJ. Designing, Conducting, and Reporting Clinical Decision Support Studies: Recommendations and Call to Action. Annals of internal medicine. 2020;172(11):S101–9.
Shailam R, Botwin A, Stout M, Gee MS. Real-Time Electronic Dashboard Technology and Its Use to Improve Pediatric Radiology Workflow. Current Problems in Diagnostic Radiology. 2018;47(1):3–5.
Badilla-Murillo F, Vargas-Vargas B, Víquez-Acuña O, García-Sanz-Calcedo J. Analysis of the installed productive capacity in a medical angiography room through discrete event simulation. Processes. 2020;8(6).
Marjamaa RA, Torkki PM, Hirvensalo EJ, Kirvelä OA. What is the best workflow for an operating room? A simulation study of five scenarios. Health Care Management Science. 2009;12(2):142–6.
Neumann J, Angrick C, Höhn C, Zajonz D, Ghanem M, Roth A, et al. Surgical workflow simulation for the design and assessment of operating room setups in orthopedic surgery. BMC Medical Informatics and Decision Making. 2020;20(1):1–20.
Benitez GB, Da Silveira GJC, Fogliatto FS. Layout Planning in Healthcare Facilities: A Systematic Review. Health Environments Research and Design Journal. 2019;12(3):31–44.
Fogliatto FS, Tortorella GL, Anzanello MJ, Tonetto LM. Lean-oriented layout design of a health care facility. Quality Management in Health Care. 2019;28(1):25–32.
Katz JD. Control of the Environment in the Operating Room. Anesthesia and Analgesia. 2017;125(4):1214–8.
Mcleod R, Myint-Wilks L, Davies S, Elhassan H. The impact of noise in the operating theatre: a review of the evidence. The Annals of The Royal College of Surgeons of England. 2021;103(2):83–7.
Kim JH, Parameshwara N, Guo W, Pasupathy KS. The Impact of Interrupting Nurses on Mental Workload in Emergency Departments. International Journal of Human-Computer Interaction. 2019;35(3):206–17.
Fishbein D, Nambiar S, McKenzie K, Mayorga M, Miller K, Tran K, et al. Objective measures of workload in healthcare: a narrative review. International Journal of Health Care Quality Assurance. 2019;33(1):1–17.
Acknowledgements
Not Applicable
Funding
Medical Delta.
Author information
Authors and Affiliations
Contributions
J.D. and F.J. and A.S. conceived of the presented idea. K.N. verified selection of the articles. A.S., S.F., J.D. and A.E. contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Availability of supporting data
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Human and animal ethics
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schouten, A.M., Flipse, S.M., van Nieuwenhuizen, K.E. et al. Operating Room Performance Optimization Metrics: a Systematic Review. J Med Syst 47, 19 (2023). https://doi.org/10.1007/s10916-023-01912-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-023-01912-9