Abstract
Gattinoni’s equation, \({\text{MP}}_{{{\text{rs}}}} \, = \,0.098\, \times \,{\text{RR}}\, \times \,\left[ {{\text{V}}_{T} ^{2} \left( {\frac{1}{2}{\text{E}}_{{{\text{rs}}}} \, + \,{\text{RR}}\, \times \,\frac{{1\, + \,I:E}}{{60\, \times \,I:E}}\, \times \,{\text{R}}_{{{\text{aw}}}} } \right)\, + \,{\text{V}}_{{\text{T}}} \, \times \,{\text{PEEP}}} \right]\), now commonly used to calculate the mechanical power (MP) of ventilation. However, it calculates only inspiratory MP. In addition, the inclusion of PEEP in Gattinoni’s equation raises debate because PEEP does not produce net displacement or contribute to MP. Measuring the area within the pressure–volume loop accurately reflects the MP received in a whole ventilation cycle and the MP thus obtained is not influenced by PEEP. The MP of 25 invasively ventilated patients were calculated by Gattinoni’s equation and measured by integration of the areas within the pressure–volume loops of the ventilation cycles. The MP obtained from both methods were compared. The effects of PEEPs on MP were also evaluated. We found that the MP obtained from both methods were correlated by R2 = 0.75 and 0.66 at PEEP 5 and 10 cmH2O, respectively. The biases of the two methods were 3.13 (2.03 to 4.23) J/min (P < 0.0001) and − 1.23 (− 2.22 to − 0.24) J/min (P = 0.02) at PEEP 5 and 10 cmH2O, respectively. These P values suggested that both methods were significantly incongruent. When the tidal volume used was 6 ml/Kg, the MP by Gattinoni’s equation at PEEP 5 and 10 cmH2O were significantly different (4.51 vs 7.21 J/min, P < 0.001), but the MP by PV loop area was not influenced by PEEPs (6.46 vs 6.47 J/min, P = 0.331). Similar results were observed across all tidal volumes. We conclude that the Gattinoni’s equation is not accurate in calculating the MP of a whole ventilatory cycle and is significantly influenced by PEEP, which theoretically does not contribute to MP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In 2016, Gattinoni et al. proposed a hypothesis that mechanical power (MP) delivered to the mechanically ventilated patients contributes to their ventilator-induced lung injury (VILI). Since the MP is hard to measure directly in clinical practice, they invented a formula to estimate the MP by algebraic calculation. Their equation incorporates several routinely monitored ventilator parameters and is written as:
where \({\text{MP}}_{\text{rs}}\) is the MP received by the respiratory system, 0.098 is the conversion factor from \(\text{L*cmH}_{2}\text{O}\) to Joule, RR is respiratory rate, VT is the tidal volume, Ers is the elastance of the respiratory system, I: E is the inspiration to expiration ratio, Raw represents airway resistance and PEEP is the value of positive end-expiratory pressure. The equation can also be simplified to read.
where Ppeak is the peak inspiratory airway pressure and Pplat is the plateau pressure. Please refer to their original article for details of derivation of these equations [1].
Since its publication, this calculation equation has gained wide acceptance. It has been adopted as a reference standard for comparison with new MP estimation methods [2, 3]. It was also commonly used in clinical studies to examine the correlation between MP and outcomes of various kinds of patients [4,5,6].
Nevertheless, Gattinoni’s equation calculates only the work of inspiration. It was verified by comparing with the measured area between inspiratory pressure curve and volume axis, which represents the inspiratory work only (Fig. 1D). Gattinoni admitted that expiration ‘very possibly’ also contributes to MP [7, 8]. Actually, expiration is an integral part of a respiratory cycle and exerts its own mechanical work in a direction opposite to that of inspiration. So, the network of a tidal ventilation is obtained by subtracting the expiratory from the inspiratory works (Fig. 1E and F). Mechanical work of a complete tidal ventilation cycle, including both inspiratory and expiratory parts, is graphically represented by the hysteresis area surrounded by a pressure–volume (PV) loop [9, 10]. For any displacement with hysteresis, the work done is measured by the area enclosed in the loop of the movement path. This principle also holds true in the realms of thermodynamics [11] and cardiac physiology [12]. Theoretically, this measurement of mechanical work (or MP) is more accurate than those considering only one limb of hysteresis.
The work done by a physiologic pathway with hysteresis is the area enclosed by a PV loop. The work during left ventricular systole is shown in (A), and the work during left ventricular diastole is shown in (B). Net work of a cardiac cycle is the work of systole subtracting that of diastole (C). By the same principle, the work done by inspiration (D) subtracting that of expiration (E) results in a net work of a respiratory cycle (F). Both net works of a cardiac and respiratory cycle are the hysteresis areas of PV loops
Considering only inspiratory limb also raises debate about including PEEP value in the calculation of work [13]. The work is defined by either force × distance, or pressure × volume. Since PEEP does not by itself produce displacement or volume change during tidal ventilation, its contribution to work is theoretically zero. If both inspiration and expiration are considered and work of ventilation is measured by the hysteresis area surrounded by PV loop, PEEP plays no role at all.
In this study, we compared MPs calculated from Gattinoni’s equation with those obtained from measuring the hysteresis area surrounded by the PV loop to evaluate the accuracy of this equation.
2 Methods
2.1 Study design
Invasively ventilated patients admitted to the intensive care units of Changhua Christian Hospital (Changhua, Taiwan) from Aug. 2019 to Apr. 2021 were prospectively enrolled. We excluded patients under 20 or over 90 years of age, with over 60% of the inspired fraction of O2, with Acute Physiology and Chronic Health Evaluation score over 30, with a plateau pressure over 30 cmH2O, or with unstable hemodynamics. The study was approved by the institutional review board of Changhua Christian Hospital (Approval No. 181262). Informed consents were obtained from surrogates of all participants.
2.2 Raw data acquisition
All patients were measured by an Evita 4 ventilator (Dräger Medical, Lübeck, Germany), which was connected to a laptop with Ventview (Dräger Medical, Lübeck, Germany) software for data collection. Appropriate sedation and muscle relaxation were given to patients with spontaneous respiration. Upon measurement, ventilators were set at volume-controlled mode with a constant flow which was adjusted to avoid harmfully high airway pressure. Inspiratory time was lengthened to generate an inspiratory hold long enough for measuring plateau pressure. Various combinations of VT (6, 8, and 10 ml per kg of body weight) and PEEPs (5 and 10 cmH2O) were set during measurement. Raw data of airway pressure, flow and volume during the measurement were downloaded to the laptop via Medibus protocol with a sampling rate of 67 Hz for subsequent offline analysis.
2.3 Derivation and calculation of ventilation-related parameters
The Pplat was defined by the last pressure value at the inspiratory plateau phase with zero airflow. The PEEP value was defined by the average of all pressure data of expiratory phase starting from flow drops to − 1 L/min. The Ers, Raw, RR, VT, I: E and the area inside the PV loop were calculated from the downloaded raw data breath by breath using an executable program written with MATLAB 7.2 (The MathWorks, Natick, MA, USA). The work of ventilation was assessed by both Gattinoni’s equation [1] and PV loop area. The work expressed in \({\text{L}}\,{\text{cmH}}_{2} {\text{O}}\) was converted to Joules by a factor of 0.098. The MP was obtained by multiplying the work per breath by the RR.
2.4 Statistical analysis
Data were expressed as number (percentage) for categorical data or median and interquartile range for continuous data. A simple regression model was performed to evaluate the correlation between MP values by Gattinoni’s equation and PV loop area. Bland–Altman analysis was used to evaluate the agreement between the two MP evaluation methods. Wilcoxon signed-rank test was used to compare two repeatedly measured works at PEEP levels of 5 and 10 cmH2O. The SAS 9.4 software (SAS Institute Inc., Cary, NC, USA) was used for statistical analysis. A two-tailed p value less than 0.05 was considered statistically significant.
3 Results
3.1 MP by Gattinoni’s equation and PV loop area
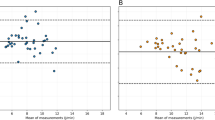
A total of 25 patients were enrolled and their baseline clinical characteristics were listed in Table 1. When the PEEP was 5 cmH2O, the MPs by both methods were correlated by a regression formula: MP by Gattinoni’s equation = 3.37 + 0.45 × MP by PV loop area, R2 = 0.75, P < 0.001 (Fig. 2A). When the PEEP was 10 cmH2O, the regression formula was: MP by Gattinoni’s equation = 5.51 + 0.63 × MP by PV loop area, R2 = 0.66, P < 0.001 (Fig. 2B). The Bland–Altman plot corresponding to PEEP 5 cmH2O was presented in Fig. 2C. The mean of difference was 3.13 J/min, and the 95% confidence interval was 2.03 to 4.23 J/min (lower limit = − 6.05 J/min, upper limit = 12.30 J/min). The P value for the null hypothesis (H0: mean of difference = 0) was less than 0.0001, which means that the results of both methods were significantly different. The Bland–Altman plot of PEEP 10 cmH2O was presented in Fig. 2D. The mean of difference was − 1.23 J/min, and the 95% confidence interval was − 2.22 to − 0.24 J/min (lower limit = − 9.47 J/min, upper limit = 7.01 J/min). The P value for the null hypothesis was 0.02, suggesting that the results of both methods were significantly different. The largest differences tended to be found when the mean MP was greater than 15 J/min. One of our patient’s PV loop at VT 10 ml/Kg and PEEP 10 cmH2O was plotted against the calculated area by Gattinoni’s equation (Fig. 3). A prominent incongruence of both areas can be easily observed. When the whole study population was divided into those with and without acute respiratory distress syndrome (ARDS), the results were similar except for ARDS patients under PEEP 10 cmH2O where no difference could be found probably because the case number of ARDS was too small (only 7). These data could be found in our supplemental Figs. s1 and s2.
Simple regression models expressing the correlations between MPs by both methods at PEEP 5 (A) and 10 cmH2O (B). Bland–Altman plots depicting differences between the two methods of evaluating MP at PEEP 5 (C) and 10 cmH2O (D). The differences were more prominent when the mean MP was larger than 15 J/min
One patient’s PV loop (orange area) at VT 10 ml/Kg and PEEP 10 cmH2O was plotted against the calculated area (elastic work in blue plus resistive work in yellow) by the Gattinoni’s equation. A prominent incongruence of both areas can be easily observed. The work of ventilation by hysteresis area of PV loop was 0.27 J, while the work by Gattinoni’s equation was 0.70 J
3.2 Assessing effects of PEEP on MP by both methods
Because PEEP does not by itself produce any air displacement during tidal ventilation, its contribution to MP is theoretically zero. The MPs, by integration of the areas inside the PV loop, were not significantly different at PEEP 5 and PEEP 10 cmH2O. On the other hand, the MPs calculated by Gattinoni’s equation, at PEEP 5 cmH2O were significantly smaller than those at PEEP 10 cmH2O (Table 2). The MPs by Gattinoni’s equation of ARDS patients did not differ significantly at PEEP 5 and 10 cmH2O. This may be due to small case numbers in this group.
4 Discussion
In this study, we provided evidence to challenge the accuracy and validity of Gattinoni’s equation. In his original publication, the MPs by Gattinoni’s equation were in very good correlation with the measured ones by R2 of 0.96 to 0.99 and the mean biases between the two methods were minimal (around ± 0.5 J/min) [1]. In contrast, our data revealed a less than perfect agreement between MPs by Gattinoni’s equation and measured ones. This discrepancy lies in the difference in MP measurement. Gattinoni’s measured areas between inspiratory pressure curve and ordinate of volume, but we measured areas surrounded by the PV loop. Gattinoni’s measurement was restricted to the inspiratory phase, while ours took both inspiration and expiration into account and was a more reliable value of the MP received during the tidal ventilatory cycle.
There is growing awareness of the important role played by expiration during a ventilatory cycle. The MP accumulated at end-inspiration is eliminated by exhaling into the atmosphere or dissipating into lung tissue during the expiratory phase [7]. Therefore, expiration surely contributes to MP and the consequential VILI. By manipulating the expiratory flow of mechanical ventilation, we can achieve more lung recruitment [14], more homogeneous lung aeration [15], better gas exchange [16], and less VILI [17]. So, neglecting expiration makes Gattinoni’s equation prone to inaccuracy in assessing the MP that a ventilated patient received.
We think the most crucial origin of inaccuracy stems from including PEEP in the calculating equation of Gattinoni’s et al. Our data demonstrated that the PEEP value did not influence MP measured by PV loop method, but it falsely increased the MP calculated by using Gattinoni’s equation (Table 2). As we mentioned in the introduction, incorporating a static pressure without net displacement, like PEEP, into the calculation of MP is contradictory to the basic law of physics. Moreover, Gattinoni’s equation suggested that a high PEEP can increase both the MP and the chance of subsequent VILI. However, this assumption could find support from neither animal studies nor clinical trials. High PEEPs failed to produce evidence of VILI in the lungs of the experimental animals [18, 19]. According to a metanalysis of 8 randomized trials on ARDS patients, high PEEPs did not lead to worse clinical outcomes and can even reduce some patients’ mortality [20].
Gattinoni’s original hypothesis that MP induces VILI and subsequent poor clinical outcomes has never been unequivocally proved [8]. Studies on the clinical implications of MP were currently all observational. Some studies showed a good correlation between MP and mortality [21, 22], whereas some did not [23, 24]. Still, some studies barely established a correlation by modifying the definition of MP calculated [4, 25].
Proposing a revised version of Gattinoni’s equation is beyond the scope of this article. It cannot be done by simply subtracting PEEP from the equation. We have tried to calculate the MP of our patients by using Gattinoni’s equation without PEEP term, but the results are still unsatisfactory (Please refer to our supplement Fig. s3).
There are two limitations to our study that worth mentioning. First, our ARDS patient number was too small to draw a solid conclusion regarding this subgroup. The insignificant results from analysis within this group are all subject to type II error. Second, to avoid harmful VILI, we did not apply a VT of more than 10 ml/Kg or a PEEP over 10 cmH2O during MP measurement. Extrapolating our results beyond these VT or PEEP limitations is subject to imprecision.
In conclusion, Gattinoni’s equation is not accurate in the calculation of the MP during a whole ventilatory cycle and is significantly influenced by PEEP, which theoretically does not contribute to MP.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- Ers :
-
Elastance of respiratory system
- I:E:
-
Inspiratory to expiratory ratio
- MP:
-
Mechanical power
- PEEP:
-
Positive end-expiratory pressure
- Ppeak :
-
Peak airway pressure
- Pplat :
-
Plateau pressure
- Raw:
-
Airway resistance
- PV:
-
Pressure–volume
- RR:
-
Respiratory rate
- VILI:
-
Ventilator-induced lung injury
- VT :
-
Tidal volume
References
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, Protti A, Gotti M, Chiurazzi C, Carlesso E, Chiumello D, Quintel M. Ventilator-related causes of lung injury: the mechanical power. Intens Care Med. 2016;42:1567–75.
Giosa L, Busana M, Pasticci I, Bonifazi M, Macrì MM, Romitti F, Vassalli F, Chiumello D, Quintel M, Marini JJ, Gattinoni L. Mechanical power at a glance: a simple surrogate for volume-controlled ventilation. Intens Care Med Exp. 2019;7:61.
Chi Y, He H, Long Y. A simple method of mechanical power calculation: using mean airway pressure to replace plateau pressure. J Clin Monit Comp. 2020. https://doi.org/10.1007/s10877-020-00575-y.
Coppola S, Caccioppola A, Froio S, Formenti P, De Giorgis V, Galanti V, Consonni D, Chiumello D. Effect of mechanical power on intensive care mortality in ARDS patients. Crit Care. 2020;24:246.
Chiu LC, Lin SW, Chuang LP, Li HH, Liu PH, Tsai FC, Chang CH, Hung CY, Lee CS, Leu SW, Hu HC, Huang CC, Wu HP, Kao KC. Mechanical power during extracorporeal membrane oxygenation and hospital mortality in patients with acute respiratory distress syndrome. Crit Care. 2021;25:13.
Schuijt MTU, Schultz MJ, Paulus F, Serpa NA. Association of intensity of ventilation with 28-day mortality in COVID-19 patients with acute respiratory failure: insights from the PRoVENT-COVID study. Crit Care. 2021;25:283.
Gattinoni L, Marini JJ, Collino F, Maiolo G, Rapetti F, Tonetti T, Vasques F, Quintel M. The future of mechanical ventilation: lessons from the present and the past. Crit Care. 2017;21:183.
Vasques F, Duscio E, Pasticci I, Romitti F, Vassalli F, Quintel M, Gattinoni L. Is the mechanical power the final word on ventilator-induced lung injury?—we are not sure. Ann Transl Med. 2018;6:395.
French CJ. Work of breathing measurement in the critically ill patient. Anaesth Intens Care. 1999;27:561–73.
Becher T, van der Staay M, Schädler D, Frerichs I, Weiler N. Calculation of mechanical power for pressure-controlled ventilation. Intens Care Med. 2019;45:1321–3.
Halliday D, Resnick R. Heat and the first law of thermodynamics. In: Fundamentals of physics. New York: Wiley; 1974. p. 468–9.
Boulpaep EL. The heart as a pump. In: Boron WF, editor. Medical physiology. Elsevier Inc.; 2017. p. 507–32.
Huhle R, Serpa Neto A, Schultz MJ, Gama de Abreu M. Is mechanical power the final word on ventilator-induced lung injury?—no. Ann Transl Med. 2018;6:394.
Borgmann S, Schmidt J, Goebel U, Haberstroh J, Guttmann J, Schumann S. Dorsal recruitment with flow-controlled expiration (FLEX): an experimental study in mechanically ventilated lung-healthy and lung-injured pigs. Crit Care. 2018;22:245.
Wirth S, Springer S, Spaeth J, Borgmann S, Goebel U, Schumann S. Application of the novel ventilation mode flow-controlled expiration (FLEX): a crossover proof-of-principle study in lung-healthy patients. Anesth Analg. 2017;125:1246–52.
Weber J, Schmidt J, Straka L, Wirth S, Schumann S. Flow-controlled ventilation improves gas exchange in lung-healthy patients—a randomized interventional cross-over study. Acta Anaesth Scand. 2020;64:481–8.
Goebel U, Haberstroh J, Foerster K, Dassow C, Priebe HJ, Guttmann J, Schumann S. Flow-controlled expiration: a novel ventilation mode to attenuate experimental porcine lung injury. Brit J Anaesth. 2014;113:474–83.
Collino F, Rapetti F, Vasques F, Maiolo G, Tonetti T, Romitti F, Niewenhuys J, Behnemann T, Camporota L, Hahn G, Reupke V, Holke K, Herrmann P, Duscio E, Cipulli F, Moerer O, Marini JJ, Quintel M, Gattinoni L. Positive end-expiratory pressure and mechanical power. Anesthesiology. 2019;130:119–30.
Vassalli F, Pasticci I, Romitti F, Duscio E, Aßmann DJ, Grünhagen H, Vasques F, Bonifazi M, Busana M, Macrì MM, Giosa L, Reupke V, Herrmann P, Hahn G, Leopardi O, Moerer O, Quintel M, Marini JJ, Gattinoni L. Does iso-mechanical power lead to iso-lung damage?: an experimental study in a porcine model. Anesthesiology. 2020;132:1126–37.
Walkey AJ, Del Sorbo L, Hodgson CL, Adhikari NKJ, Wunsch H, Meade MO, Uleryk E, Hess D, Talmor DS, Thompson BT, Brower RG, Fan E. Higher PEEP versus lower PEEP strategies for patients with acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14:297–303.
Costa ELV, Slutsky AS, Brochard LJ, Brower R, Serpa-Neto A, Cavalcanti AB, Mercat A, Meade M, Morais CCA, Goligher E, Carvalho CRR, Amato MBP. Ventilatory variables and mechanical power in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2021;204:303–31.
Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, Cazati DC, Cordioli RL, Correa TD, Pollard TJ, Schettino GPP, Timenetsky KT, Celi LA, Pelosi P, Gama de Abreu M, Schultz MJ. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intens Care Med. 2018;44:1914–22.
Dianti J, Matelski J, Tisminetzky M, Walkey AJ, Munshi L, Del Sorbo L, Fan E, Costa EL, Hodgson CL, Brochard L, Goligher EC. Comparing the effects of tidal volume, driving pressure, and mechanical power on mortality in trials of lung-protective mechanical ventilation. Respir Care. 2021;66:221–7.
Belliato M, Epis F, Cremascoli L, Ferrari F, Quattrone MG, Fisser C, Malfertheiner MV, Taccone FS, Di Nardo M, Broman LM, Lorusso R. Mechanical power during veno-venous extracorporeal membrane oxygenation initiation: a pilot-study. Membranes. 2021;11:30.
Ghiani A, Paderewska J, Walcher S, Neurohr C. Mechanical power normalized to lung-thorax compliance predicts prolonged ventilation weaning failure: a prospective study. BMC Pul Med. 2021;21:202.
Acknowledgements
This study was supported by Grant 108-CCH-IRP-081 of Changhua Christian Hospital (Changhua, Taiwan) and Grant V96C1-153 of Taipei Veterans General Hospital (Taipei, Taiwan). We thank Mr. Jian-Nan Pan, manager of Dräger Medical (Lübeck, Germany), for technical support in MP measurement. We thank respiratory therapists Ji-Yuan Ke, Ya-Yun Chuang, and Shu-Hua Hsieh for ventilatory raw data acquisition. We thank Ms. Tzu-Ling Tsai for her secretarial assistance.
Funding
This study was funded by Changhua Christian Hospital, (Grant No. 108-CCH-IRP-081) to Shin-Hwar Wu; Taipei Veterans General Hospital (Grant V96C1-153) to Cheng-Deng Kuo.
Author information
Authors and Affiliations
Contributions
SHW drafted the manuscript. CTK analyzed the data and performed statistical calculations. ICM, CCC, and KHL collected clinical data and took care of the study patients. CDK was involved in the conception of the study and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no competing interest.
Ethical approval
The study was approved by the Institutional Review Board of Changhua Christian Hospital (Approval No. 181262).
Informed consent
Informed consents were obtained from surrogates of all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, SH., Kor, CT., Mao, IC. et al. Accuracy of calculating mechanical power of ventilation by one commonly used equation. J Clin Monit Comput 36, 1753–1759 (2022). https://doi.org/10.1007/s10877-022-00823-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-022-00823-3