Abstract
The variables measured in modern pulse oximetry apparatuses include a graphical pulse curve and a specified perfusion value (PV) that could be a sensitive marker for detecting differences in sympathetic activity. We hypothesized that there is a correlation between a reduction of PV and the time to eye opening after general anaesthesia. The objective was to investigate whether PV can predict eye opening after sevoflurane anaesthesia. Prospective, explorative clinical study included 20 patients, ASA physical status 1 or 2, at Skåne University Hospital, Lund, Sweden, from November 2012 to January 2013 scheduled for elective breast tumour surgery. A general anaesthesia was delivered with inhalation of oxygen, nitrous oxide and sevoflurane anaesthesia to a depth of 1.2 minimal alveolar concentration. Sevoflurane inspiratory and expiratory concentrations were measured. Bispectral index monitoring, PV as measured by pulse oximeter, heart rate and carbon dioxide were registered at before anaesthesia, 15 min after induction (at 1.2 minimal alveolar concentration), at end of surgery and at eye opening at the end of anaesthesia. PV values were lower before anaesthesia and at eye opening compared to at 15 min after induction and at end of surgery (P < 0.05). The reduction of PV between end of surgery and eye opening was 0.76. We conclude that the pulse oximeter PV could be a useful variable to assess the timing of recovery, in terms of eye opening after a general anaesthesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The homeostasis during general anaesthesia is governed by the pharmacological effects of the drugs used. General anaesthetic procedures often include hypnotic and analgesic drugs for induction and maintenance followed by an inhalation agent [1]. The physiological changes that occur in the anesthetized patient depend on factors that are controlled by the nature and quantity of drugs as well as the general condition and medical history of the patient [2]. One of the physiological effects of anaesthesia is dilation of peripheral blood vessels with a subsequent blood pressure drop as a result of decreased adrenergic outflow and/or response [3].
For early detection of adverse physiological changes electrocardiogram (ECG), blood pressure, pulse oximetry and airway gas need to be adequately monitored. Pulse oximetry is the method for measuring the oxygen saturation of the blood (SpO2) by registering the change in absorbance at different levels of oxyhaemoglobin, using a light beam transmitted through the tissues of a finger or an earlobe. Pulse oximetry is based on a non-invasive technique and is thus easy to use in everyday clinical practice.
The pulse oximetry unit uses two Light Emitting Diodes (LED) with different wavelengths, one of which emits visible red light at 660 nm and one infrared light at 940 nm and a light sensitive phototransistor which records the transmittance of the light in the tissue [4]. The variables measured in the modern pulse oximetry apparatuses include the SPO2 value, a pulse curve the amplitude of which can be read graphically, and/or as a specified perfusion value (PV). Some studies have suggested that the amplitude of the PV may be a sensitive estimate of the level of sympathetic activity [3, 5, 6].
In some studies parameters as e.g. eye opening, endotracheal extubation, orientation to person was used to document the recovery time after anaesthesia [7, 8]. The aim of the present study was to investigate whether PV is related to depth of anaesthesia and specifically to obtain a more predictable point of recovery in terms of eye opening after general anaesthesia.
2 Materials and methods
2.1 Ethics
Ethical approval for this study according to the standards set in the Helsinki declaration was provided by Regional Ethics Committee, Lund, Sweden on June 2012, Dnr: 2012/336. Patients scheduled for elective breast tumour surgery were enrolled by Surgery Reception nurses. Consent to participate in the study was received from each patient.
2.2 Patients
The investigation included 20 patients, ASA physical status 1 or 2, at Skåne University Hospital, Lund, Sweden, from November 2012 to January 2013. Patients were considered for inclusion in the trial if they were over 18 years age. Patients with known pulmonary or cardiovascular disease or pharmacological antihypertensive treatment were excluded. The study was prospective and descriptive.
2.3 Experimental procedure
Before start and throughout anaesthesia, all patients were monitored as described below. Before induction the first set of values were registered (time: Pre-anaesthesia) including; PV, Bispectral index monitoring (BIS), mean arterial blood pressures (MAP), ECG, heart rate, and SpO2. General anaesthesia was induced with propofol 1–3 mg kg1, fentanyl 25–50 μg and maintained with inhalation of oxygen, nitrous oxide and sevoflurane anaesthesia to a depth of 1.2 minimal alveolar concentration (MAC), measured between laryngeal mask and heat exchange filter. After induction rectal temperature and respiratory frequency was also monitored. The second sets of values were registered 15 min after induction (time: Anaesthesia 15 min), now complemented with carbon dioxide expiratory partial pressure (PETCO2) and Sevoflurane inspiratory and expiratory partial pressures (Fisevo, PETsevo). If mean blood pressure decreased below 60 mm Hg patients received ephedrine 5–10 mg intravenously. Thirty minutes before the expected end of the anaesthesia all patients received ketobemidon 5 mg intravenously to prevent postoperative pain. At completion of the last skin suture a third set of values (including all defined values) were registered (time: End of surgery). Intraoperative recovery time was defined as the time from the discontinuation of sevoflurane to eye opening when a fourth set of all above mentioned values were registered (time: Eye opening).
Patients were monitored with 3-lead ECG, heart rate, SpO2, BIS and PV with measured by the pulse oximeter probe (Intelli Vue MP70 Anesthesia, Philips Medizin System, Boeblingen Germany), the amplitude were displayed as an electronically number and were documented in a case report form. Sevoflurane, inspiratory and expiratory partial pressure (Fisevo, PETsevo) and PETCO2 as analyzed by the ventilator (Dräger Primus™, Dräger Medical, Lübeck, Germany). Total ventilation min−1, tidal volumes (VT), were measured and documented at the same intervals. Pulse oximeter sensor wavelength range was 500–1,000 nm and emitted light energy was ≤15 mW. The first author performed and documented all the procedures.
2.4 Statistical analysis
All statistical analysis was performed with SPSS 20.0 for Windows, (SPSS Inc., Chicago, Illinois, USA). A power analysis was performed for the main outcome parameter: differences between PV during anaesthesia and eye opening. A P value <0.05 was considered to indicate statistical significance. With a difference of 3.5 with a standard deviation (SD) of 3, a power of 0.8 was achieved with 14 patients. All data are reported as mean and SD.
The values of demographic data (age, height, weight, BMI), MAP, heart rate, oxygen saturation, perfusion, BIS and PETCO2 are presented as mean ± SD. For interpreting the relationship between different variables a multiple regression analysis with Durbin–Watsons test was used. For change of values over time, one-way repeated measurement analysis of variance (ANOVA) was used. The ANOVA analysis was followed by Tukey and Scheffe post hoc tests. A P value <0.05 was considered to indicate statistical significance.
3 Result
Patient characteristics are presented in Table 1. No intraoperative problems were noted during the study. All patients recovered from anaesthesia and left the postoperative unit in accordance with the routines assigned for the surgical procedure.
The values of mean non invasive blood pressure and heart rate were similar Pre-anaesthesia versus the time point of Eye opening but statistically significant larger compared to the Anaesthesia 15 min and End of surgery (P < 0.05, Table 2).
The values of sevoflurane tension and respiratory rate were lower at time of Eye opening compared to Anaesthesia 15 min (P < 0.05, Table 3). The values of VT were larger at time point Eye opening compared to Anaesthesia 15 min (P < 0.05, Table 3). The data of SPO2 and PETCO2 was similar at all time points (Table 3).
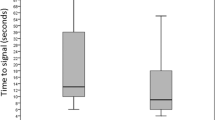
The PV values were lower at Pre-anaesthesia and Eye opening compared to at Anaesthesia 15 min and End of surgery (P < 0.05, Table 4; Fig. 1). The PV correlation between End of surgery and Eye opening was r 2 = 0.76 ± 0.09 (Table 4, Fig. 2). In the same timeframe the correlation (r2) between PV and MAC was 0.60 (P < 0.05).
Perfusion (PV) values at the end of surgery (End of surgery) and after anaesthesia end when the patient opens the eyes (Eye opening). The mean is indicated by a bolder dashed line, n = 20. The reduction of PV between End of surgery and Eye opening was 0.76 ± 0.09. PV was lower at the time of Eye opening compared to at the End of surgery (P < 0.05)
The values of BIS were larger at Pre-anaesthesia compared to at Anaesthesia 15 min, End of surgery and Eye opening (P < 0.05, Table 4; Figs. 3, 4). The mean BIS value was lower between End of surgery and Eye opening (r2 = 0.31 ± 0.17, Fig. 4, P < 0.05), and the correlation between BIS and MAC was r 2 = 0.50 (P < 0.05).
Bispectral index (BIS) values at the end of surgery (End of surgery) and after anaesthesia end when the patient opens the eyes (Eye opening). The mean is indicated by a bolder dashed line, n = 20. The increase of BIS between anaesthesia with End of surgery and Eye opening was 0.31 ± 0.17. BIS was larger in the time of Eye opening compared to at End of surgery (P < 0.05)
During the period from Pre-anaesthesia to Anaesthesia 15 min, the correlation between PV and BIS was at r 2 = 0.67 (P < 0.05) and during the period from End of surgery to Eye opening, the correlation between PV and BIS was r 2 = 0.36 (P < 0.05).
4 Discussion
In the present study, the PV was found to be larger during adequate anaesthesia (Anaesthesia 15 min) using 1.2 MAC and to return towards baseline after end of anaesthesia, when the patient regains consciousness and re-opens the eyes. We have observed that the PV value regularly increases after the start of anaesthesia to decrease during recovery.
In the present study, sevoflurane anaesthesia resulted in increased PV. A change in the PV amplitude is at least partly due to changes in the peripheral vascular bed, which is controlled by the sympathetic nervous system. Several studies have suggested that the amplitude of the pulse curve may be a marker sensitive for change of activity in the sympathetic nerves triggered by painful stimuli such as skin incision during anaesthesia [3, 5, 6]. Ginosar et al. [9, 10] demonstrated that an epidural block results in an increase in PV. This was interpreted as a sign of vasodilatation due to epidural-related change in sympathetic activity in the anesthetized area.
Additional reasons for PV changes could be that pharmacological hypotension or hypovolemia alters the plethysmographic waveform and pulse amplitude. Shamir et al. demonstrated that during pressure ventilation of the lungs, the amplitude of the plethysmographic wave varies synchronously with the respiratory cycle [11, 12]. In addition, with administration of an adrenergic agent, the drug-induced vasoconstriction reduces the pulse amplitude with a resulting lower PV. Cannesson et al. found a strong correlation between arterial pressure and plethysmographic wave amplitude. Both arterial waveform and plethysmographic waveform reflect cardiac stroke volume [13, 14]. In present study the patients consisted of a homogenous group of women, ASA 1 and 2, without any history of circulatory conditions undergoing surgery during standardized inhalation anaesthesia with spontaneous breathing. No hypovolemia or hypothermia was registered and no adrenergic drugs were given. It thus seems reasonable to assume that neither sympathetic blockade, other pharmacologic interference, hypovolaemia nor breathing cycle variation in the plethysmographic signal could explain the changes in observed PV values.
BIS is presented as a scale from 100 (awake) to 0 (isoelectric EEG). As used for ensuring adequate depth of anaesthesia, a BIS value lower than 60 should be aimed for to minimize awareness/recall during anaesthesia [15]. BIS was used in our study as a standard for anaesthesia depth and recovery. During induction and maintenance of anaesthesia at 1.2 MAC, BIS and PV levels matched each other well. However, during the recovery phase until eye opening the PV value returned to base line, while the BIS value only increased by 31 % from the value at adequate anaesthesia. An explanation why PV is faster than BIS could be that there is a calculating delay in EEG-based indices. BIS is reflecting the hypnotic drug effect in the brain in contrary to the local autonomic nervous system activity reflected by the nociceptive–antinociceptive balance at the finger tip.
Limitations in our study are that only healthy hemodynamic stable women under general sevoflurane anaesthesia were involved. Another limitation could be the small number of participants. However, considering the design of the study we believed it was still possible to achieve convincing results since the results is based on adequate statistical power. We also believe that being able to faster detect patients physiological changes could benefits both patient safety (time of unconsciousness) and have an impact on patient flow according to operating schedule. However, further studies are needed to determine if the perfusion value is useful also in other forms of anaesthesia and procedures to predict recovery times by detecting adrenergic circulatory response.
In conclusion, in haemodynamically stable patients pulse oximeter perfusion values could be a useful variable to assess timing of recovery in patients after a general anaesthesia.
References
Stenqvist O. Inhalationsanestesi. Halldin, Lindahl S, editors. Anestesi. Stockholm: Liber AB; 2000. p. 243–264.
Enekvist B, Bodelsson M, Johansson A. Increased apparatus dead space and tidal volume increase blood concentrations of oxygen and sevoflurane in overweight patients: a randomised controlled clinical study. Eur J Anaesthesiol. 2011;28:382–6.
Korhonen I, Yli-Hankala A. Photoplethysmography and nociception. Acta Anesthesiol Scand. 2009;53:975–85.
Jubran A. Pulse oximetry. Crit Care. 1999;3:R11–7.
Seitsonen ERJ, Korhonen IKJ, van Gils MJ, Huiku M, Lötjönen JMP, Kortitila KT, Yli-Hankala AM. EEG spectral entropy, heart rate, photoplethysmography and motor responses to skin incision during sevoflurane anaesthesia. Acta Anesthesiol Scand. 2005;49:284–92.
Takeyama M, Matsunaga A, Kakihana Y, Masuda M, Kuniyoshi T, Kanmura Y. Impact of skin incision on the pleth variability index. J Clin Monit Comput. 2011;25:215–21.
Locher S, Stadler K, Boehlen T, Bouillon T, Leibundgut D, Eng M, Schumacher PM, Wymann R, Zbinden AM. A new closed-loop control system for isoflurane using bispectral index outperforms manual control. Anesthesiology. 2004;101:591–602.
Ahmad S, Yilmaz M, Marcus R-J, Glisson S, Kinsella A. Impact of bispectral index monitoring on fast tracking of gynecologic patients undergoing laparoscopic surgery. Anesthesiology. 2003;98:849–52.
Ginosar Y, Weiniger CF, Meroz V, Bdolah-Abram T, Babchenko A, Nitzan M, Davidson EM. Pulse oximeter perfusion index as early indicator of sympathhectomy after epidural anesthesia. Acta Anesthesiol Scand. 2009;53:1018–26.
Ginosar Y, Weiniger CF, Kurz V, Babchenko A, Nitzan M, Davidson E. Sympathectomy mediated vasodilatation: a randomized concentration ranging study of epidural bupivacaine. Can J Anesth. 2009;56:213–21.
Golparvar M, Naddafnia H, Saghaei M. Evaluating the relationship between arterial blood pressure changes and indices of pulse oximeteric plethysmography. Anesth Analg. 2002;95:1686–90.
Shamir M, Eidelman LA, Floman Y, Kaplan L, Pizov R. Puls oximeter plethysmographic waveform during changes in blood volume. Br J Anaesth. 1999;82:178–81.
Cannesson M, Besnard C, Durand P, Bohe J, Jacques D. Relation between respiratory variations in pulse oximetry plethysmographic waveform amplitude and arterial pulse pressure in ventilated patients. Crit Care. 2005;9:R562–8.
Desgranges FP, Desebbe O, Ghazouani A, Gilbert K, Keller G, Chiari P, Robin J, Bastien O, Lehot J-J, Cannesson M. Influence of the site of measurement on the ability of plethysmographic index to predict fluid responsiveness. Br J Anaesth. 2011;107:329–35.
Chin KJ, Yeo SW. BIS-guided study of sevoflurane requirements for adequate depth of anaesthesia in caesarean section. Anaesthesia. 2004;59:1064–8.
Conflict of interest
The authors declare there were no conflicts of interest.
Ethical standard
Ethical approval for this study according to the standards set in the Helsinki declaration was provided by Regional Ethics Committee, Lund, Sweden on June 2012, Dnr: 2012/336.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Enekvist, B., Johansson, A. Pulse perfusion value predicts eye opening after sevoflurane anaesthesia: an explorative study. J Clin Monit Comput 29, 461–465 (2015). https://doi.org/10.1007/s10877-014-9623-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9623-1