Abstract
There is growing interest in offering Internet-delivered cognitive behaviour therapy (ICBT) to individuals with chronic health conditions, with this process often being guided by a single clinician. Due to lack of full time personnel, it is sometimes necessary to have multiple clinicians offer guidance or for no guidance to be offered. In this randomized trial, we compared team-guided ICBT (n = 90) to self-guided ICBT (n = 88). Participants completed measures at pre-, post-, and 3-months post-ICBT. Both groups showed similar rates of treatment completion and large improvements on depression and anxiety at post-treatment and follow-up. Unexpectedly, more participants in the self-guided versus team-guided condition showed clinically significant improvement on depression at post-treatment (76.5% vs 49.2%) and follow-up (70% vs 45.6%). Thus, team-guided ICBT may not provide significant benefits compared to self-guided ICBT. However, it may be an alternative approach to consider among a population of high risk individuals that wants or requires closer monitoring of symptoms.
Trail registration TRN: NCT03500237; Date: April 18, 2018.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, chronic health conditions represent a significant problem requiring attention given their prevalence, costs, and association with disability (Vos et al., 2020). Of concern, as the number of physical health conditions increases, rates of comorbid mental health concerns increase, and the co-existence of mental and physical conditions is associated with reduced quality of life, increased suicidal ideation, and increased healthcare utilization (Dai et al., 2020). Although psychosocial interventions are increasingly incorporated into routine care of chronic health conditions, accessing support for comorbid mental health concerns remains challenging for individuals (Barnett et al., 2012), suggesting a need for innovative approaches. Barriers to receiving mental health care include costs and availability of services, time and location restraints, and concerns about stigma (Andersson & Titov, 2014). This is problematic, as addressing anxiety and depression outcomes among those with chronic health conditions has been shown to improve disability outcomes (Jasper et al., 2014; Vallejo et al., 2015), pain severity (Buhrman et al., 2004; Chiauzzi et al., 2010; Dear et al., 2013, 2015), and fatigue (Friesen et al., 2017; Williams et al., 2010).
The need for accessible treatment options has been further exacerbated by the 2020 pandemic, as individuals with chronic health conditions have been disproportionately burdened by COVID-19 morbidity and mortality (WHO, 2020; Camacho-Rivera et al., 2020). Face-to-face health service utilization has significantly decreased since the onset of the COVID-19 outbreak (Wong et al., 2020). Thus, those managing chronic health conditions have been encouraged to engage in telehealth appointments to minimize risk exposure while maintaining continuity of care (Horrell et al., 2021). Remote interventions can improve access to care for those who have been underserved, or those who are unable to attend in-person appointments.
Internet-delivered cognitive-behavioural therapy (ICBT) shows particular promise in improving psychological outcomes among individuals with chronic health conditions (Mehta et al., 2018). In ICBT, participants access treatment materials that have been arranged into lessons online, and either navigate the course materials on their own, or with guidance from a guide or clinician typically over several months (Anderson & Titov, 2014). Numerous meta-analyses have reported that guided ICBT results in larger clinical improvements in symptoms of depression and anxiety than self-guided ICBT (Andersson et al., 2019; Etzelmueller et al., 2020). A recent systematic review and meta-analysis showed that self-guided ICBT generally results in small effects for depression and moderate effects for anxiety among people with chronic health conditions; outcomes appear superior when participants receive guidance (Mehta et al., 2018). Studies among those with chronic health conditions also note the potential need for greater support i.e. patients requesting twice a week check in from their guide (Hadjistavropoulos et al., 2019; Mehta et al., 2018). The downside of offering clinician guidance is that it is associated with increased costs, and having the same designated clinician over several months also presents organizational challenges when there is staff turn-over, holiday and sick time. Furthermore, if clinicians work part-time, participants may have to wait for a response to questions until the clinician next works. Thus, in order to provide more intensive care (i.e., response to clients within one-business day for those with chronic conditions among clinical settings where full-time staff are not always available), it may require more than one clinician to offer support to participants completing ICBT, creating a team-guided approach. To our knowledge, team-guided ICBT, where therapeutic workload is spread across several clinicians depending on their availability (e.g., first available guide responds), has not been studied. The approach, however, has potential to improve outcomes over self-guided ICBT, while reducing or buffering against organizational challenges involved in having a single designated clinician work with clients throughout treatment.
In the present study, we were interested in comparing two methods of offering ICBT for people with chronic health conditions, namely ICBT that was team-guided versus ICBT that was self-guided. In the team-guided condition, varying clinicians (depending on work schedule) would send weekly emails to participants and also respond to any participant email received from the participant from the previous day (one-business-day response). Primary outcomes were depression and anxiety, and secondary outcomes were psychological distress, disability, quality of life, pain, fatigue, life satisfaction, self-efficacy, healthcare use, and mental health medication use. Outcomes were assessed at 8-weeks post-treatment and 3 months follow-up. Groups were also compared on objective engagement (e.g., lessons accessed) and treatment satisfaction. It was hypothesized that the team-guided approach would improve outcomes, engagement, and satisfaction above self-guided ICBT.
Methods
Ethics and trial registration
This study was approved by the University of Regina Ethics Board and was registered on clinicaltrials.gov: NCT03500237. Participants were recruited from across Canada via strategic advertising (posters, advertising cards, and presentations), media attention, and collaborations (e.g. course referrals) with service providers and non-governmental organizations representing and or providing services to people with chronic health conditions. In terms of sample size, using WebPower (Zhang & Yuan, 2018) with alpha = 0.05 and power = 0.80, we estimated that we required a total sample of 164 participants to detect a moderate between group effect size. We enrolled additional participants, as we anticipated that some patients would not begin the intervention after randomization, resulting in a total sample size of 195 participants.
Intake and course progression
Participants first completed an online application on the Online Therapy Unit website (www.onlinetherapyuser.ca), a government- and research-funded unit that specializes in delivering ICBT for anxiety and depression routinely at no cost to participants. This online application collected background information and was followed by a telephone interview where screeners confirmed participants were: (1) at least 18 years of age; (2) residing in Canada; ((3) self-reported symptoms of anxiety/depression related to a chronic health condition, i.e.a physical health condition persisting for more than 3 months; (4) able to read and write in English; (5) consented to participate in ICBT; and (6) able to access the internet. During this interview, participants were excluded if they: (1) had a self-reported and/or clinician-identified difficulty with cognitive functioning that could impact their ability to fully engage in treatment (e.g., dementia); (2) were assessed as having a high risk of suicide; and (3) did not self-report having a chronic health condition. An emergency medical contact was required for participation in the course.
For the purposes of this study, chronic health conditions were characterized as any physical health condition sustained over 3 months or longer to distinguish conditions from those likely to be acute or transient (Perrin et al., 1993). See Table 1 for a list of common chronic health conditions. Participants who fully met eligibility criteria in the telephone screen were randomized into one of two groups (team-guided or self-guided) using Research Electronic Data Capture (REDCap) in a 1:1 ratio in blocks of 24 without matching. Telephone screeners did not know what condition the participant would be assigned until after the participant was accepted into the trial. Clinicians could not be blinded to randomization because the randomization group was related to the type of contact the participant received (i.e., team-guided vs self-guided).
Participants in the self-guided condition did not receive regular communication with a clinician and worked through the course materials independently. Each week, an assigned clinician, however, briefly reviewed the participant profile to monitor scores on symptom measures for signs the participant was experiencing increased distress (a 5-point increase in primary measure of depression or anxiety, or endorsed the presence of suicidal thoughts more than half the days per week on the primary depression measure). Participants who showed increased distress were contacted by the clinician by telephone to ensure safety. Otherwise, contact was only made if participants reported needing technical support to use the platform.
Those randomized to the team-guided condition received a once-weekly email from a team of up to five guides during treatment on the same day each week. Additionally, the team was instructed to check for messages from clients each day and send an additional email if they had received a message from the client. The number of guides that interacted with each client ranged from 2 to 5 with clients interacting with a mean of 3.79 guides during treatment (1.1% 2 guides, 32.2% 3 guides, 53.3% 4 guides, 13.3% 5 guides). Guides included 5 registered clinicians: 1 Master’s level registered social worker, 2 Master’s level certified counselors, 1 Master’s level registered psychologist, and 1 Master’s level provisionally registered psychologist. All guides had had at least 1 year experience delivering ICBT at the Online Therapy Unit. The guide with provisional status was supervised by a clinician with over 5 years of experience delivering ICBT. Training for all guides included a 2 days workshop on delivering the ICBT program, as well as supervised practice by a clinician with over 10 years’ experience in delivering ICBT. More information on the Online Therapy Unit is provided in Hadjistavropoulos et al. (2020a, 2020b). Guides also met monthly over the course of the study to discuss concerns in service delivery, ensure standardization of message delivery, and engage in strategies to help promote therapeutic alliance. Additionally, auditing of messages were conducted to ensure treatment fidelity. Guides primarily communicated with participants through emails on the treatment platform and were instructed to spend approximately 15 min per email to each participant on a weekly basis. In the email, guides highlighted content of the course, and offered feedback on symptom scores from the previous week. Guides were encouraged to build rapport with clients, answer client questions, assist clients in tailoring activities to their condition, reinforce completion of lessons, activities, and progress, and assist clients with challenges in applying skills and barriers to using skills. As noted above, guides sent one weekly message and then responded to any message the participant sent during the week within one-business day. Phone calls were rare and only made if risk was apparent as described above, if the participant had not logged in for over 7 days, or if the participant requested a phone call instead of email support. Guides were instructed to spend approximately 10 min on phone calls that were intended to facilitate understanding or provide psychoeducation. To appropriately test the team-guided approach, guides were scheduled each week to ensure participants had the experience of multiple guides, and the same guide did not send all emails or check in with the participant on the same day each week.
Both groups received access to a transdiagnostic ICBT program called the Chronic Conditions Course—developed by the eCentreClinic at Macquarie University, Australia and licensed by the Online Therapy Unit. The Chronic Conditions Course is made up of five easy to follow core lessons released sequentially during an 8-weeks period (Dear et al., 2018, 2022; Gandy et al., 2016; Mehta et al., 2020). Lessons are based on cognitive behaviour therapy and focus on helping participants learn concepts such as: identifying symptoms, thought challenging, de-arousal strategies, planning pleasant activities, graded exposure, activity pacing, and relapse prevention. Additional resources are made available to all participants in an open access format, which provide further detail on topics including sleep, assertiveness, attention, managing beliefs, managing chronic conditions, working with health professionals, mental skills, acute and chronic pain, panic and physical sensations, structured problem solving and worry time, and communication skills. Participants also have access to case stories designed to help participants learn to apply skills, and “do-it-yourself” guides that summarize lesson content and suggested homework for each lesson. All participants received weekly automated emails informing them of the content of the upcoming lesson.
Measures
Primary and secondary measures were administered at pre-treatment, post-treatment, and 3-months-follow-up. Primary measures were also administered at the beginning of lessons 2–5 to facilitate symptom monitoring in both the self-guided and team-guided conditions.
Primary outcome measures
Patient health questionnaire-9 (PHQ-9)
The PHQ-9 is a nine-item self-report questionnaire designed to assess symptoms of depression over the past two weeks (Kroenke et al., 2001). Total scores range from 0 to 27, with scores ≥ 10 suggesting presence of major depressive disorder (Manea et al., 2012). The PHQ-9 has been shown to have high internal consistency (α = 0.86–0.89) and good construct validity (Kroenke et al., 2001).
Generalized anxiety disorder-7 (GAD-7)
The GAD-7 consists of 7 statements designed to measure symptoms of anxiety within the past two weeks. Total scores range from 0 to 21, with scores ≥ 10 indicating likely clinical levels of anxiety (Spitzer et al., 2006). Psychometric studies show that GAD-7 has excellent internal consistency (α = 0.92) and strong construct validity (Spitzer et al., 2006).
Secondary measures
World Health Organization disability assessment schedule (WHODAS)
The WHODAS is a 12-item self-report measure designed to assess several different aspects of functioning and disability over the last 30 days, including cognition, self-care, and life-activities (Axelsson et al., 2017). Total scores range from 0 to 48, with higher scores indicating increased disability (Axelsson, et al., 2017). Among those with physical health conditions, the WHODAS has been shown to have alpha estimates varying from 0.81 up to 0.96 (Saltychev et al., 2021).
The EuroQol-5D (EQ5D)
The EQ5D is a self-report measure used to assess quality of life (i.e., mobility, self-care, pain, and anxiety/depression) and overall health (rating scale of 0-worst health to 100-best health; EuroQol Research, 2015). The current study analyzed only data from the overall health scale (i.e., Visual Analogue Scale; VAS). The EQ-5D-5L demonstrates test–retest reliability, high internal consistency (α = 0.83), and good validity (Marti et al., 2016).
Kessler-10 distress scale (K10)
The K10 is a self-report measure designed to assess psychological distress over the past 30 days (Kessler et al., 2002). Total scores range from 0 to 40, with higher scores indicating more severe psychological distress. K10 presented excellent Cronbach’s alpha (α) (0.93).
Brief pain inventory (BPI)
The short-form BPI consists of four items related to pain severity and seven items related to pain interference (Cleeland & Ryan, 1994). A mean score is created for the pain severity (range: 0–10) and pain interference (range: 0–10) factors, with higher scores indicating more severe pain and greater pain-related interference, respectively. Of note, there was a problem with the administration of the BPI questions at 3-month follow-up, where only participants who answered “yes” to the first question were administered the rest of the BPI; because of this error it was not possible to compare pre- and post-BPI to the 3-months BPI. Good internal consistency, ranging from 0.80 to 0.87 are reported for pain severity items and from 0.89 to 0.92 for the interference items (Cleeland & Ryan, 1994).
Fatigue symptom inventory (FSI)
The FSI consists of 14 items designed to assess fatigue (Shahid et al., 2011). Consistent with the literature, responses for 13 of the items were summed to create a total fatigue score with a range from 0 to 130 (Shahid et al., 2011). Alpha coefficients for multi-item scales ranged from 0.84 to 0.96 (Donovan & Jacobsen, 2011).
Satisfaction with life scale (SWLS)
The SWLS consists of 5 items designed to assess global-life satisfaction (Deiner et al., 1985). Total scores on the SWLS range from 5 to 35, with higher scores indicating greater life satisfaction (Deiner et al., 1985). Internal consistency, estimated by coefficient α, ranged from 0.81 to 0.96 for the individual subscales (Deiner et al., 1985).
Self-efficacy for managing chronic disease-6 (SES-6)
This 6-item measure assesses participants’ confidence with managing chronic health conditions and their symptoms (Lorig et al., 2001). Responses to each question are made on a 10-point Likert scale; the measure is scored by calculating the average of the six items. Mean scores range from 0 to 10, with higher scores indicating greater confidence at managing chronic health conditions (Lorig et al., 2001). Cronbach's alpha of 0.88 was seen, minimal floor and ceiling effects were observed, and the measure was sensitive to change (Ritter & Lorig, 2014).
Treatment inventory of costs in psychiatric patients (TIC-P)
A modified version of the TIC-P (Bouwmans et al., 2013) was administered at pre-treatment and at 3-months follow-up. At pre-treatment, participants answered questions related to lifetime use and use in the past 3 months of mental health services (i.e., family doctor/walk-in clinic, psychiatrist, psychologist, social worker, counsellor, nurse/community nurse/psychiatric nurse, occupational therapist, medical specialist, or other health care professional), treatment programs (i.e., psychiatry day/part-time treatment program, alcohol or drug treatment program, self-help group, occupational stress injury program), hospital and crisis services (i.e., emergency room, ambulance, crisis service, and hospital admission), and mental health medication use (Bouwmans et al., 2013). At 3-months follow-up, they were asked if they had utilized any of the above services and mental health medication use in the previous 3-months period.
Credibility and expectancy questionnaire (CEQ)
The CEQ (Devilly & Borkovec, 2000) assesses participants’ perceived credibility and expected success of treatment and was administered at pre-treatment. The three items of the CEQ assessing treatment credibility were summed to create a total score ranging from 3 to 27, with higher scores indicating greater perceived credibility.
Treatment satisfaction
Participants completed the ICBT treatment satisfaction questions (Dear et al., 2011) at post-treatment. Items included forced-choice questions related to satisfaction with the course (i.e., overall, lessons/DIY guides, treatment platform) rated on a scale of 1 (Very Dissatisfied) to 5 (Very Satisfied), and yes/no questions about whether they would recommend the course to a friend, if the course was worth their time, and whether they experienced negative effects during the course.
Treatment engagement
Treatment engagement was assessed by the number of lessons accessed, days logging into the website, emails sent to guide, emails from guide to participant, and phone calls between participant and guide.
Guide feedback
At the end of the trial, all guides were asked to submit written feedback on the benefits and challenges of both team- and self-guided approaches. Feedback was summarized and reported in the results.
Analyses
All analyses were completed using Statistical Package for the Social Sciences version 26 (SPSS) and R version 4.0.5. Internal consistency was examined on all measures and found acceptable (alpha > 0.83) at all time points. Demographic variables, such as age and injury type, were examined using descriptive statistics to describe the sample. Generalized estimating equations (GEE) (Hardin et al., 2013) were used to examine the effect of the Chronic Conditions Course on primary and secondary outcome measures. GEE analyses allow for measurements of changes over time while taking within-subject variance into consideration. GEE models for the VAS, SWLS, and SES-6 used a Gaussian distribution with identity link function. All other GEE models used a Gamma distribution with log link. All GEE models used an exchangeable working correlation structure and fully iterated jackknife estimates of variance. A number of statistical tests were employed based on GEE analyses to help interpret the results: (1) average percentage change across time with 95% confidence intervals; and (2) bias-corrected Cohen’s dunb effect sizes for within and between group effects based on the estimated marginal means taken from the GEE models. Further analysis examined any potential differences between the team-guided condition and the self-guided condition, as well as clinically significant improvements of at least 30% or greater. As was previously recommended, outcome deteriorations greater than 30% for GAD-7 and PHQ9 outcomes were noted for post-treatment measures (Rozental et al., 2014). One-way ANOVAs were used to compare groups on continuous variables (e.g., number of messages sent to guide) and chi-square tests were used to compare groups on categorical variables (e.g., treatment satisfaction).
Missing data
39% (69/178) of participants were missing at least one primary measure at post-treatment and 26% (46/178) were missing at least one primary measure at follow-up. Multiple imputation were used to replace missing values before fitting the GEE models or calculating clinically significant improvements. In creating the imputation models, we found that course completion was significantly associated with missingness. Participants who did not complete at least 4 lessons were significantly less likely to have post-treatment (7.1% vs 77.2%, p < 0.001) or follow-up measures (16.4% vs 83.8%, p < 0.001). We were not able to adjust for course completion at post-treatment because there were only 3 participants who did not complete the course but did complete post-treatment measures. Therefore, when imputing missing values, we adjusted for randomization group and any observed measures for that participant at post-treatment, and when imputing follow-up measures, we additionally adjusted for course completion.
Results
Demographic variables
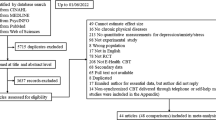
In total, 424 participants completed the online screen and were directed to the telephone screening. Of those participants, 261 completed the telephone screen and 195 participants were randomized into two groups. Of those randomized, 178 started the intervention, including 90 participants in the team-guided group, and 88 in the self-guided group. See Fig. 1 for participant flow. Table 1 includes the pre-treatment characteristics of the overall sample and each group. The average age of participants was 45.75 years (SD = 13.61), and most participants were female (76.4%, n = 136), married or common law (67.4%, n = 120), had more than a high school diploma (82.6%, n = 147), and Caucasian (89.3%, n = 159). Most participants also resided outside of large cities (55.5%, n = 97). At pre-treatment, 66.9% (n = 119) reported experiencing pain, 76.4% (n = 136) reported having more than one chronic health condition, and 41.6% (n = 74) reported having had a chronic health condition for more than 5 years. Depression was in the clinical range for 57.3% (n = 102) of participants while anxiety was in the clinical range for 55.6% (n = 99) of participants. No significant differences in baseline symptom scores were found between the randomization groups.
Primary analyses
Results from the GEE models are given in Table 2. While statistically significant time effects were found on the PHQ-9 (F(2, 319) = 60.1, p < 0.001) and GAD-7 (F(2, 293) = 48.0, p < 0.001), no time*group interaction effects were found on the PHQ-9 (F(2, 282) = 2.22, p = 0.11) or GAD-7 (F(2, 284) = 1.23, p = 0.29). Cohen’s dunb within-group effect sizes from pre-treatment to post-treatment and follow-up were medium to large in the team-guided condition, and large in the self-guided condition and overall sample.
The self-guided condition had significantly higher rates of PHQ-9 clinically significant improvement at both post-treatment (76.5% vs 49.2%, p = 0.004) and follow-up (70.0% vs 45.6%, p = 0.005). Group differences in GAD-7 improvement rates (71.9% for self-guided and 63.4% for team-guided) and in PHQ-9 or GAD-7 deterioration rates (PHQ-9: 4.7% for self-guided and 6.7% for team-guided; GAD-7: 8.5% for self-guided and 6.9% for team-guided) were not significant.
On the secondary measures, the GEE analysis found statistically significant time effects on the WHODAS (F(2, 234) = 15.5, p < 0.001), EQ-5D VAS (F(2, 316) = 15.3, p < 0.001), K10 (F(2, 253) = 28.9, p < 0.001), BPI Interference (F(2, 132) = 8.0, p = 0.006), FSI (F(2, 258) = 9.1, p < 0.001), SWLS (F(2, 238) = 5.7, p = 0.004), and SES-6 (F(2, 271) = 23.0, p < 0.001). Time effects were not significant on the BPI Severity (F(2, 190) = 3.6, p = 0.06). There were no significant time*group interaction effects on any secondary measure (p range 0.05–0.90). dunb within-group effect sizes were medium to large on the K10, medium to small on the SES-6, medium to very small on the EQ-5D VAS, and small to very small on all other secondary measures. There was a statistically significant between-group dunb effect size at post-treatment on the K10, with the team-guided group having higher K10 post-treatment scores suggesting poorer outcomes (24.02 vs 21.41, dunb = 0.35).
Health service and medication use
No differences were found from pre-treatment to 3-months follow-up in the proportion of participants who saw a family doctor/walk-in clinic/nurse/other health professional (43.8%, n = 78/178 vs 39.5%, n = 50/127, p = 0.75), or psychiatrist (11.8%, n = 21/178 vs 14.2%, n = 18/127, p = 1.00). However, there was an increase in the proportion of participants who reported seeing a psychologist/counsellor/social worker, from 30.3% (n = 54/178) to 39.4% (n = 50/127), p = 0.04. Health service usage did not differ between team-guided and self-guided participants at 3-months follow-up (p range: 0.19–0.89). Further, no differences were found from pre-treatment to 3 months follow-up in the proportion of participants who reported taking medication for their mental health in the previous 3 months (39.3%, n = 70/178 vs 37.0%, n = 47/127, p = 1.00). Medication use at 3-months follow-up did not differ between team-guided (35.8%, n = 24/67) and self-guided (38.3%, n = p = 0.77) conditions.
Program engagement
Table 3 displays program engagement measures separated by group, with some significant differences found. As would be expected, team-guided participants received more messages from the guide than the self-guided participants (an average of 10.99 vs 0.45), as well as more phone calls (1.61 vs 0.59). Participants sent more messages to guides in the team-guided condition than self-guided condition (3.27 vs 0.47) and logged in a greater number of times (17.79 vs 14.18). No differences were found in terms of completion rates for the first four lessons (p = 0.14) or all five lessons (p = 0.13) or for completion of the post-treatment (p = 0.38) or 3-months (p = 0.27) primary outcome measures.
Program satisfaction and negative effects
Table 3 shows ratings of participants’ satisfaction and negative effects. Group differences were not significant (p range: 0.26–0.64). As demonstrated in Table 3, 96.1% (n = 99) of participants completing measures reported that the course was worth their time taking, 95.1% (n = 98) said that they would recommend the course to a friend, and 87.4% (n = 90) said that they were either “satisfied” or “very satisfied” with the course. Out of 103 participants who responded, 20 (19.4%) reported that they had experienced unwanted negative effects during the course, with most of those participants reporting that the negative effect had a “moderate” impact on their lives (65.0%, 13/20). The most common negative effect reported was a feeling of pressure or guilt related to the course’s expectations (40.0%, 8/20; e.g., “Slight stress with getting the lessons done”ID 8205). Other negative effects were related to an increase in symptoms (20.0%, 4/20), external stressors (15.0%, 3/20), health-related limitations (15.0%, 3/20), and difficulties with self-reflection (10.0%, 2/20).
Guide feedback
In terms of the team-guided approach, guides reported that because they had a shared caseload, it was easier to seek support from each other when they experienced challenges delivering support to participants (e.g., were uncertain how to respond to a unique question about a chronic health condition). In the self-guided approach, guides reported that monitoring of symptoms was typically brief and efficient, and the need to follow-up with participants was rare. In both approaches, the guides noted that having a shared caseload often resulted in guides feeling unfamiliar with the participants they were emailing. They noted that before emailing participants, they would review the participant files to better understand the participants’ treatment experience. This process was especially challenging within the team-guided approach, as guides felt the need to thoroughly review participant files during each contact to ensure they were familiar with previous interactions and progress with a different guide, and noted this process took additional time. Concerns about unfamiliarity were less common in the self-guided approach, given that contact would only happen in exceptional circumstances (i.e., increased suicide risk), but guides noted that they also required additional time to review the participant file if an elevated score was found.
Discussion
The current study is the first to examine the efficacy of a team-guided approach compared to a self-guided approach when delivering ICBT for people with chronic health conditions. Improvements were observed across both groups for all primary outcome measures and most secondary outcomes, and no significant differences in outcomes were observed between the groups. The outcomes were large for depression and anxiety (our primary outcome measures); moderate for psychological distress, self-efficacy, and the EQ-5D VAS; small for fatigue, life satisfaction, and pain interference; and non-significant for pain at post-treatment. The findings were unexpected for two reasons. Firstly, a recent systematic review and meta-analysis showed that self-guided ICBT generally results in small effects for depression and moderate effects for anxiety (Mehta et al., 2018); as such, finding large effects for depression and anxiety in the current study was unexpected. A recent study examining the Chronic Conditions Course found small but significant improvements in depression (d = 0.47), anxiety (d = 0.32), and disability (d = 0.17) at post-treatment in the ICBT group compared to a waitlist control group (Dear et al., 2022). Secondly, the same systematic review suggested that ICBT outcomes are superior when participants receive guidance (Mehta et al., 2018), and as noted above, the team-guided approach was not superior to the self-guided approach. Also unexpected was the fact that the self-guided group had a greater portion of participants report a 30% decrease in depressive symptoms compared to the team-guided group at post-treatment (76.5% vs 49.2%) and at 3-months follow-up (70.0% vs 45.6%). Several factors may have contributed to the current findings.
One factor may be the relatively high level of adherence observed among both groups, with no differences in completion of lessons (overall 76.4% completed four lessons and 65.7% completed all five lessons). It was surprising that the team-guided approach did not result in significantly greater completion of lessons than the self-guided approach given that past studies find greater adherence to ICBT in guided programs compared to self-guided programs (Richards & Richardson, 2012). Previous systematic reviews also found that small difference in adherence amongst self- and guided-ICBT groups resulted in slight differences in effect size between the groups (Cuijpers et al. 2009). Previously, only one study evaluated the efficacy of guided ICBT compared to self-guided ICBT (Dear et al., 2015). The study found no significant difference between the two groups in outcomes. Similar high levels of adherence were seen in the study for both guided and self-guided ICBT, 82% vs 78% respectively (Dear et al., 2015).
Additionally, although self-guided participants worked primarily independently, they all received a telephone interview at pre-treatment, which can help prepare participants for treatment (Titov et al., 2015). In addition, they all received automated messages and had a clinician that monitored their progress and symptoms, which may have led them to feel more supported than if the program was strictly self-guided. Furthermore, the treatment content and methods for facilitating engagement have been carefully developed over numerous trials and consistent with this, we found that all participants were highly satisfied with the program materials. These factors have been previously recognised as important in facilitating improvements in self-guided interventions (Andersson & Titov, 2014; Dear et al., 2016). Recent research suggests that “alliance with the program” is predictive of outcomes in ICBT (Zalaznik et al., 2021) and thus perhaps it was high alliance with the program in both the self-directed and team-guided groups that accounts for lack of differences between groups.
It is possible that the team-guided approach resulted in a level of support that was not well-matched to the participants’ needs. Participants received a minimum of once-weekly contact, but could receive additional responses within one-business day if they messaged their guide. In previous research on once-weekly therapist support plus one-business-day responses to participant emails, no benefits were found for this type of contact compared to once-weekly support in a general population without chronic health conditions (Hadjistavropoulos et al., 2020a, 2020b). Furthermore, in one previous study, there was some indication that increased therapist contact was associated with participants feeling lower confidence in their ability to manage symptoms than once-weekly contact (Hadjistavropoulos et al., 2020a, 2020b). Therefore, it is possible that increasing contact beyond once weekly in the team-guided appropriate in this study inadvertently undermined the benefits of team-guided support.
The other factor that could be at play is that receiving feedback from several different clinicians could have altered the participant-clinician rapport. There is conflicting evidence about the role of therapeutic alliance on participant outcomes in internet interventions; there is at least some research to suggest that some aspects of alliance (e.g., agreement with tasks and goals) are related to outcomes of ICBT (see Berger et al., 2017). Although the guides in the current study attempted to use strategies to enhance alliance, it may be that inconsistent contact with team-guided clinicians altered perceptions of therapeutic alliance, thereby affecting participant outcomes. Clinicians in the current study did not specifically report on alliance with participants—their feedback indicated they experienced challenges following participant progress in the team-guided condition which may indicate some alterations to alliance. As no previous research has evaluated the role of therapeutic alliance when ICBT is delivered by multiple clinicians, future research on its role is warranted.
The study was not without its limitations. First, although completion of 3-months follow-up measures was quite high (team-guided 77.8%; self-guided 70.5%), post-treatment completion rates (64.4% team-guided; 58.0% self-guided) were lower than we anticipated given our previous research (Hadjistavropoulos et al., 2018). Completion rates may have been lower at post-treatment because participants had to log back onto the website to complete them, whereas at 3-months follow-up, they were emailed a link to complete them. As with all studies, there is always a question about generalizability of study findings to other settings and thus replication of findings is needed. We also did not measure therapeutic alliance with clinicians and this may have provided useful information that could assist with interpreting findings. We were also not powered to identify small differences between groups and only tracked mental health medication use at 3-months follow-up. Further, the study involved a 3-months follow-up and it is possible that differences may have emerged longer term. Finally, it has been noted that the use of brief screening measures (e.g., the PHQ-9 and GAD-7) may over-estimate the prevalence of depression and anxiety and have the potential to pathologize normal human distress (Titov & Andersson, 2021).
Despite these limitations, the current study has several strengths. This is the first trial evaluating the effects of a team-guided approach when delivering ICBT, and thus adds to the literature on models for offering ICBT. The study evaluated ICBT for diverse chronic health conditions, which is often not examined in the literature, with most previous research focussing on ICBT for single health conditions (e.g., pain, cancer; see Mehta et al., 2018). The study also evaluated several outcome measures, and showed that outcomes are particularly strong for depression, anxiety, psychological distress and self-efficacy, while improvements for disability, fatigue, pain-interference and life satisfaction are considerably smaller. Pain intensity itself was not impacted by the chronic conditions course and may represent an opportunity to improve the course given that 66.9% of participants endorsed having difficulties with pain.
Several directions for research related to the team-guided approach exist. As noted above, if the team-guided approach is used in the future, it would be valuable to study if there is a way to implement the approach that would improve outcomes beyond what was found in the current approach, such as consistently having two designated clinicians offer support with a predictable schedule known to patients rather than an unknown, unpredictable schedule and typically 3 to 4 clinicians providing support as was done in this study. It would also be valuable to examine if the team-guided approach may mitigate adverse events among those with greater levels of suicide risk or severe symptoms compared to the self-guided approach. Furthermore, with larger samples it would be valuable to explore if clinician support is more important for some chronic health conditions than others. It would also be valuable to explore if the self-guided condition would be effective if it did not involve the initial telephone interview or involve monitoring of participant symptoms during treatment. Future research could also examine the role of participant preferences, by exploring participant preference for the self-guided vs team-guided version. Additionally, research examining longer-term outcomes beyond 3-months follow-up is warranted.
In conclusion, the results from the current study suggest that both team-guided and self-guided ICBT for chronic health conditions have similar effects in improving symptoms of anxiety and depression. Although, the current study shows non-inferiority of self-guided vs team-guided approach, the team-guided approach may still be an alternative approach to consider among a population of high risk individuals that wants or requires closer monitoring of symptoms (n = 99) perhaps related to symptom severity of risk. The use of team-guided approaches may be a more preferred option than self-guided apps which provide no symptom monitoring. Further research is needed examining different approaches for supporting people with chronic health conditions through ICBT, particularly looking at participant (e.g., different chronic health conditions, preferences) and intervention characteristics (e.g., with or without telephone assessment), that may influence engagement and outcomes.
Availability of data and material
Not applicable.
References
Andersson, G., & Titov, N. (2014). Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry, 13, 4–11. https://doi.org/10.1002/wps.20083
Andersson, G., Titov, N., Dear, B. F., Rozental, A., & Carlbring, P. (2019). Internet-delivered psychological treatments: From innovation to implementation. World Psychiatry, 18, 20–28. https://doi.org/10.1002/wps.20610
Axelsson, E., Lindsäter, E., Ljótsson, B., Andersson, E., & Hedman-Lagerlöf, E. (2017). The 12-item self-report world health organization disability assessment schedule (WHODAS) 2.0 administered via the internet to individuals with anxiety and stress disorders: A psychometric investigation based on data from two clinical trials. JMIR Mental Health, 4, e58. https://doi.org/10.2196/mental.7497
Barnett, K., Mercer, S. W., Norbury, M., Watt, G., Wyke, S., & Guthrie, B. (2012). Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. The Lancet, 380, 37–43. https://doi.org/10.1016/SO140-6736(12)60240-2
Berger, T. (2017). The therapeutic alliance in internet interventions: A narrative review and suggestions for future research. Psychotherapy Research, 27, 511–524. https://doi.org/10.1080/10503307.2015.1119908
Bouwmans, C., De Jong, K., Timman, R., Zijlstra-Vlasveld, M., Van der Feltz-Cornelis, C., Tan Swan, S., & Hakkaart-van Roijen, L. (2013). Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Services Research, 13, 217. https://doi.org/10.1186/1472-6963-13-217
Buhrman, M., Fältenhag, S., Ström, L., & Andersson, G. (2004). Controlled trial of Internet-based treatment with telephone support for chronic back pain. Pain, 111(3), 368–377. https://doi.org/10.1016/j.pain.2004.07.021
Camacho-Rivera, M., Islam, J. Y., Rivera, A., & Vidot, D. C. (2020). Attitudes toward using COVID-19 mHealth tools among adults with chronic health conditions: Secondary data analysis of the COVID-19 impact survey. JMIR Mhealth, 8(12), e24693. https://doi.org/10.2196/24693
Chiauzzi, E., Pujol, L. A., Wood, M., Bond, K., Black, R., Yiu, E., & Zacharoff, K. (2010). Pain action-back pain: A self-management website for people with chronic back pain. Pain Medicine, 11(7), 1044–1058. https://doi.org/10.1111/j.1526-4637.2010.00879.x
Cleeland, C. S., & Ryan, K. M. (1994). Pain assessment: Global use of the brief pain inventory. Annals of the Academy of Medicine Singapore, 23, 129–138.
Cuijpers, P., Marks, I. M., van Straten, A., Cavanagh, K., Gega, L., & Andersson, G. (2009). Computer-aided psychotherapy for anxiety disorders: A meta‐analytic review. Cognitive Behaviour Therapy, 38(2), 66–82.
Dai, H. H., Mei, Z., An, A. J., & Wu, J. H. (2020). Epidemiology of physical and mental comorbidity in Canada and implications for health-related quality of life, suicidal ideation, and healthcare utilization: A nationwide cross-sectional study. Journal of Affective Disorders, 263, 209–215. https://doi.org/10.1016/j/jad.2019.11.146
Dear, B. F., Fogliati, V. J., Fogliati, R., Gandy, M., McDonald, S., Talley, N., Holtmann, G., Titov, N., & Jones, M. (2018). Transdiagnostic internet-delivered cognitive-behaviour therapy (CBT) for adults with functional gastrointestinal disorders (FGID): A feasibility open trial. Journal of Psychosomatic Research, 108, 61–69. https://doi.org/10.1016/j.jpsychores.2018.02.015
Dear, B. F., Gandy, M., Karin, E., Staples, L. G., Johnston, L., Fogliati, V. J., Wootton, B. M., Terides, M. D., Kayrouz, R., Perry, K. N., Sharpe, L., Nicholas, M. K., & Titov, N. (2015). The pain course: A randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. Pain, 156, 1920–1935. https://doi.org/10.1097/j.pain.0000000000000251
Dear, B. F., Scott, A. J., Fogliati, R., Gandy, M., Karin, E., Dudeney, J., Nielssen, O., McDonald, S., Heriseanu, A. I., Bisby, M. A., Sharpe, L., Jones, M. P., Ali, S., & Titov, N. (2022). The chronic conditions course: A Randomised controlled trial of an internet-delivered transdiagnostic psychological intervention for people with chronic health conditions. Psychotherapy and Psychosomatics. https://doi.org/10.1159/000522530
Dear, B. F., Staples, L. G., Terides, M. D., Fogliati, V. J., Sheehan, J., Johnston, L., Kayrouz, R., Dear, R., McEvoy, P. M., & Titov, N. (2016). Transdiagnostic versus disorder-specific and clinician-guided versus self-guided internet-delivered treatment for Social Anxiety Disorder and comorbid disorders: A randomized controlled trial. Journal of Anxiety Disorders, 42, 30–44.
Dear, B. F., Titov, N., Perry, K. N., Johnston, L., Wootton, B. M., Terides, M. D., Rapee, R. M., & Hudson, J. L. (2013). The pain course : A randomised controlled trial of a clinician-guided Internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain, 154, 942–950. https://doi.org/10.1016/j.pain.2013.03.005
Dear, B. F., Titov, N., Schwencke, G., Andrews, G., Johnston, L., Craske, M. G., & McEvoy, P. (2011). An open trial of a brief transdiagnostic internet treatment for anxiety and depression. Behaviour Research and Therapy, 49, 830–837. https://doi.org/10.1016/j.brat.2011.09.007
Deiner, E., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49, 71–75. https://doi.org/10.1207/s15327752jpa4901_13
Devilly, G. J., & Borkovec, T. D. (2000). Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry, 31(2), 73–86.
Donovan, K. A., & Jacobsen, P. B. (2011). The fatigue symptom inventory: A systematic review of its psychometric properties. Supportive Care in Cancer, 19, 169–185. https://doi.org/10.1007/s00520-010-0989-4
Etzelmueller, A., Vis, C., Karyotaki, E., Baumeister, H., Titov, N., Berking, M., Cuijpers, M., Riper, P., & Ebert, D. D. (2020). Effects of Internet-based cognitive behavioral therapy in routine care for adults in treatment for depression and anxiety: A systematic review and meta-analysis. Journal of Medical Internet Research, 22, e18100. https://doi.org/10.2196/18100
EuroQol Research. (2015). EQ-5D-5L user guide. Basic Information on How to Use the EQ-5D-5L Instrument. EQ-5D.
Friesen, L. N., Hadjistavropoulos, H. D., Schneider, L. H., Alberts, N. M., Titov, N., & Dear, B. F. (2017). Examination of an internet-delivered cognitive behavioural pain management course for adults with fibromyalgia: A randomized controlled trial. Pain, 158, 593–604.
Gandy, M., Karin, E., Fogliati, V. J., McDonald, S., Titov, N., & Dear, B. F. (2016). A feasibility trial of an Internet-delivered and transdiagnostic cognitive behavioral therapy treatment program for anxiety, depression, and disability among adults with epilepsy. Epilepsia, 57, 1887–1896. https://doi.org/10.1111/epi.13569
Hadjistavropoulos, H. D., Peynenburg, V., Nugent, M., Karin, E., Titov, N., & Dear, B. F. (2020a). Transdiagnostic Internet-delivered cognitive behaviour therapy with therapist support offered once-weekly or once-weekly supplemented with one-business-day: Pragmatic randomized controlled trial. Internet Interventions, 22, 100347. https://doi.org/10.1016/j.invent.2020.100347
Hadjistavropoulos, H. D., Peynenburg, V., Thiessen, D., Nugent, M., Adlam, K., Owens, K., Dear, B. F., & Titov, N. (2020b). A pragmatic factorial randomized controlled transdiagnostic Internet-delivered cognitive behavioural therapy trial: Exploring benefits of homework reflection questionnaires and twice-weekly therapist support. Internet Interventions. https://doi.org/10.1016/j.invent.2020.100357
Hadjistavropoulos, H. D., Schneider, L. H., Hadjistavropoulos, T., Titov, N., & Dear, B. F. (2018). Effectiveness, acceptability and feasibility of an Internet-delivered cognitive behavioral pain management program in a routine online therapy clinic in Canada. Canadian Journal of Pain, 2, 62–73. https://doi.org/10.1080/24740527.2018.1442675
Hadjistavropoulos, H. D., Schneider, L. H., Mehta, S., Karin, E., Dear, B. F., & Titov, N. (2019). Preference trial of internet-delivered cognitive behaviour therapy comparing standard weekly versus optional weekly therapist support. Journal of Anxiety Disorders, 63, 51–60. https://doi.org/10.1016/j.janxdis.2019.02.002
Hardin, J. W., & Hilbe, J. M. (2013). Generalized estimating equations. Taylor & Francis.
Horrell, L. N., Hayes, S., Herbert, L. B., MacTurk, K., Lawhon, L., Valle, C. G., & Bhowmick, A. (2021). Telemedicine use and health-related concerns of patients with chronic health conditions during COVID-19: Survey of members of online health communities. Journal of Medical Internet Research, 23, e23795. https://doi.org/10.2196/23795
Jasper, K., Weise, C., Conrad, I., Andersson, G., Hiller, W., & Kleinstaeuber, M. (2014). Internet-based guided self-help versus group cognitive behavioral therapy for chronic tinnitus: A randomized controlled trial. Psychotherapy and Psychosomatics, 83, 234–246. https://doi.org/10.1159/000360705
Kessler, R. C., Andrews, G., Colpe, L. J., Hiripi, E., Mroczek, D. K., Normand, S. L. T., Walters, E. E., & Zaslavasky, A. M. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32, 959–976. https://doi.org/10.1017/s0033291702006074
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Lorig, K. R., Sobel, D. S., Ritter, P. L., Laurent, D., & Hobbs, M. (2001). Effect of a self-management program for patients with chronic disease. Effective Clinical Practice, 4, 256–262.
Manea, L., Gilbody, S., & McMillan, D. (2012). Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. Canadian Medical Association Journal, 184, E191–E196. https://doi.org/10.1503/cmaj.110829
Marti, C., Hensler, S., Herren, D. B., Niedermann, K., & Marks, M. (2016). Measurement properties of the EuroQoL EQ-5D-5L to assess quality of life in patients undergoing carpal tunnel release. Journal of Hand Surgery (European Volume), 41(9), 957–962.
Mehta, S., Hadjistavropoulos, H., Nugent, M., Karin, E., Titov, N., & Dear, B. F. (2020). Guided internet-delivered cognitive-behaviour therapy for persons with spinal cord injury: A feasibility trial. Spinal Cord, 58, 544–552. https://doi.org/10.1038/s41393-019-0398-6
Mehta, S., Peynenburg, V. A., & Hadjistavropoulos, H. D. (2018). Internet-delivered cognitive behaviour therapy for chronic health conditions: A systematic review and meta-analysis. Journal of Behavioral Medicine. https://doi.org/10.1007/s10865-018-9984-x
Perrin, E. C., Paul Newacheck, I., Pless, B., Drotar, D., Gortmaker, S. L., Leventhal, J., Perrin, J. M., Stein, R. E. K., Walker, D. K., & Weitzman, M. (1993). Issues involved in the definition and classification of chronic health conditions. Pediatrics, 91, 787–793. https://doi.org/10.1542/peds.91.4.787
Richards, D., & Richardson, T. (2012). Computer-based psychological treatments for depression: A systematic review and meta-analysis. Clinical Psychology Review, 32, 329–342. https://doi.org/10.1016/j.cpr.2012.02.004
Ritter, P. L., & Lorig, K. (2014). The English and Spanish self-efficacy to manage chronic disease scale measures were validated using multiple studies. Journal of Clinical Epidemiology, 67, 1265–1273. https://doi.org/10.1016/j.jclinepi.2014.06.009
Rozental, A., Andersson, G., Boettcher, J., Ebert, D. D., Cuijpers, P., Knaevelsrud, C., Ljótsson, B., Kaldo, V., Titov, N., & Carlbring, P. (2014). Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interventions, 1, 12–19. https://doi.org/10.1016/j.invent.2014.02.001
Saltychev, M., Katajapuu, N., Bärlund, E., & Laimi, K. (2021). Psychometric properties of 12-item self-administered World Health Organization disability assessment schedule 2.0 (WHODAS 2.0) among general population and people with non-acute physical causes of disability: Systematic review. Disability and Rehabilitation, 43, 789–794. https://doi.org/10.1080/09638288.2019.1643416
Shahid, A., Wilkinson, K., Marcu, S., & Shapiro, C. M. (2012). Fatigue symptom inventory (FSI). In A. Shahid, K. Wilkinson, S. Marcu, & C. M. Shapiro (Eds.), STOP, THAT and one hundred other sleep scales. Springer. https://doi.org/10.1007/978-1-4419-9893-4_36
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Titov, N., & Andersson, G. (2021). Using brief measures to identify depression and other mental disorders: A challenge for research and clinical practice. Internet Interventions. https://doi.org/10.1016/j.invent.2021.100450
Titov, N., Dear, B. F., Staples, L. G., Terides, M. D., Karin, E., Sheehan, J., Johnston, L., Gandy, M., Fogliati, V. J., Wootton, B. M., & McEvoy, P. M. (2015). Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: A randomized controlled trial. Journal of Anxiety Disorders, 35, 88–102. https://doi.org/10.1016/j.janxdis.2015.08.002
Vallejo, M. A., Ortega, J., Rivera, J., Comeche, M. I., & Vallejo-Slocker, L. (2015). Internet versus face-to-face group cognitive-behavioral therapy for fibromyalgia: A randomized control trial. Journal of Psychiatric Research, 68, 106–113. https://doi.org/10.1016/j.psychires.2015.06.006
Vos, T., Lim, S. S., Abbafati, C., Abbas, K. M., Abbasi, M., Abbasifard, M., Abbasi-Kangevari, M., Abbastabar, H., Abd-Allah, F., Abdelalim, A., Abdollahi, M., Abdollahpour, I., Abolhassani, H., Aboyans, V., Abrams, E. M., Abreu, L. G., Abrigo, M. R. M., Abu-Raddad, L. J., Abushouk, A. I., … Adabi, M. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396, 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
Williams, D. A., Kuper, D., Segar, M., Mohan, N., Sheth, M., & Clauw, D. J. (2010). Internet-enhanced management of fibromyalgia: A randomized controlled trial. Pain, 151, 694–702. https://doi.org/10.1016/j.pain.2010.08.034
Wong, S. Y. S., Zhang, D., Sit, R. W. S., Yip, B. H. K., Chung, R. Y., Wong, C. K. M., Chan, D. C. C., Sun, W., Kwok, K. O., & Mercer, S. W. (2020). Impact of COVID-19 on loneliness, mental health, and health service utilisation: A prospective cohort study of older adults with multimorbidity in primary care. British Journal of General Practice, 70, e817–e824. https://doi.org/10.3399/bjgp20X713021
World Health Organization. (2020). Disability considerations during the COVID-19 outbreak. https://www.who.int/publications/i/item/WHO-2019-nCoV-Disability-2020-1
Zalaznik, D., Strauss, A. Y., Halaj, A., Barzilay, S., Fradkin, I., Katz, B. A., Ganor, T., Ebert, D. D., Andersson, G., & Huppert, J. D. (2021). Patient alliance with the program predicts treatment outcomes whereas alliance with the therapist predicts adherence in internet-based therapy for panic disorder. Psychotherapy Research, 31, 1022–1035. https://doi.org/10.1080/10503307.2021.1882712
Zhang, Z., & Yuan, K.-H. (2018). Practical Statistical Power Analysis Using Webpower and R (Eds). Granger, ISDSA Press.
Funding
The Saskatchewan Ministry of Health provides funding to The Online Therapy Unit to deliver online therapy in Saskatchewan. Study of outcomes was made possible in part by funding awarded to Dr. Heather Hadjistavropoulos by the Canadian Institutes of Health Research (Reference Number 152917). The Chronic Conditions Course was developed with funding from Macquarie University and the Australian National Health and Medical Research Council.
Author information
Authors and Affiliations
Contributions
HDH, MN, SHM designed the study. SHM and MN were involved in study set-up and data collection. HDH, SHM, GLP, MN, VP, DT all were involved in various aspects of data analysis, interpretation, and co-drafted the article. BD, and NT assisted with design of the study and revised the paper for important intellectual content. All authors approved the final version of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare relevant to the content of this article. Dr. Blake Dear and Professor Nickolai Titov are developers of the Chronic Conditions Course, but derive no personal or financial benefit from it.
Ethical approval
Approval for this study was obtained from the ethics committee of the University of Regina.
Consent to participate
Informed consent to participate in the study was obtained from all participants.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mehta, S.H., Nugent, M., Peynenburg, V. et al. Internet-delivered cognitive behaviour therapy for chronic health conditions: self-guided versus team-guided. J Behav Med 45, 674–689 (2022). https://doi.org/10.1007/s10865-022-00346-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-022-00346-x