Abstract
Nickel-titanium alloy (nitinol, NiTi) is a biomaterial with unique thermal shape memory, superelasticity and high damping properties. Therefore NiTi has been used in medical applications. In this in vitro study, the effect of NiTi alloy (with two surface modifications – helium and hydrogen) on gene expression profile of selected interleukins (IL-1β, IL-6 and IL-8) and matrix metalloproteinases (MMP-1 and MMP-2) in human physiological osteoblasts and human osteoarthritic osteoblasts was examined to respond to a question of the different behavior of bone tissue in the implantation of metallic materials in the presence of cells affected by the osteoarthritic process. The cells were cultivated in contact with NiTi and with or without LPS (bacterial lipolysaccharide). Changes in expression of target genes were calculated by 2-ΔΔCt method. An increased gene expression of IL-1β in osteoarthritic osteoblasts, with even higher expression in cells collected directly from the metal surface was observed. In case of physiological osteoblasts, the change in expression was detected after LPS treatment in cells surrounding the disc. Higher expression levels of IL-8 were observed in osteoarthritic osteoblasts after NiTi treatment in contact with alloy, and in physiological osteoblasts without relation to location in combination of NiTi and LPS. IL-6 was slightly increased in physiological osteoblastes after application of LPS. MMP-1 expression level was obviously significantly higher in osteoarthritic osteoblasts with differences regarding the metal surface and location. MMP-2 expression was decreased in both cell lines after LPS treatment. In conclusion, results of present study show that the NiTi alloy and the treatment by LPS, especially repeated doses of LPS, change the gene expression of selected ILs and MMPs in human osteoblast cell cultures. Some of the changes were depicted solely to osteoarthritic osteoblasts.






Similar content being viewed by others
References
Castleman LS, Motzkin SM, Alicandri FP, Bonawit VL. Biocompatibility of nitinol alloy as an implant material. J Biomed Mater Res. 1976;10:695–731.
Khasenov BP, Kadnikov AA, Rabkin DI. Use in technology and medicine of TiNi alloys revealing the shape memory effect. Met Sci Heat Treat. 1988;30:300–3.
Duerig TW. Present and Future Applications of Shape Memory and Superelastic Materials. MRS Online Proc. Libr. Arch. [Internet]. 1994 [cited2017 Jun 27];360. Available from: https://www.cambridge.org/core/journals/mrs-online-proceedings-library-archive/article/present-and-future-applications-of-shape-memory-and-superelastic-materials/8C81C41C01FE30B24E96408096D67562.
Ryhänen J, Niemi E, Serlo W, Niemelä E, Sandvik P, Pernu H, et al. Biocompatibility of nickel-titanium shape memory metal and its corrosion behavior in human cell cultures. J Biomed Mater Res. 1997;35:451–7.
Fonte M, Saigal A. Effects of crystallographic texture directionality on the compressive stress–strain response of shape recovered polycrystalline nitinol. Scr Mater. 2010;63:320–23.
Greiner C, Oppenheimer SM, Dunand DC. High strength, low stiffness, porous NiTi with superelastic properties. Acta Biomater. 2005;1:705–16.
Prymak O, Bogdanski D, Köller M, Esenwein SA, Muhr G, Beckmann F, et al. Morphological characterization and in vitro biocompatibility of a porous nickel–titanium alloy. Biomaterials. 2005;26:5801–7.
Wayman CM, Ōtsuka K. Shape memory materials [Internet]. Reprinted with corrections. Cambridge; New York: Cambridge University Press; 1998. http://trove.nla.gov.au/work/23711130.
Shabalovskaya SA. On the nature of the biocompatibility and on medical applications of NiTi shape memory and superelastic alloys. Biomed Mater Eng. 1996;6:267–89.
Leucht P, Kim J-B, Wazen R, Currey JA, Nanci A, Brunski JB, et al. Effect of mechanical stimuli on skeletal regeneration around implants. Bone. 2007;40:919–30.
Es-Souni M, Fischer-Brandies H, Es-Souni M. Human gingival fibroblast response to electropolished NiTi surfaces. J Biomed Mater Res A. 2007;80:159–66.
Lausmaa J, Mattsson L, Rolander U, Kasemo B. Chemical composition and morphology of titanium surface oxides. MRS Online Proc. Libr. Arch. [Internet]. 1985 [cited2017 Jun 27];55. Available from: https://www.cambridge.org/core/journals/mrs-online-proceedings-library-archive/article/div-classtitlechemical-composition-and-morphology-of-titanium-surface-oxidesdiv/49A8E8B4AE348E8BDB6351C773590B9D.
Alvarez K, Nakajima H. Metallic scaffolds for bone regeneration. Materials. 2009;2:790–832.
Denkhaus E, Salnikow K. Nickel essentiality, toxicity, and carcinogenicity. Crit Rev Oncol Hematol. 2002;42:35–56.
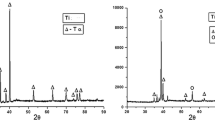
Ševčíková J, Bártková D, Goldbergová M, Kuběnová M, Čermák J, Frenzel J, et al. On the Ni-Ion release rate from surfaces of binary NiTi shape memory alloys. Appl Surf Sci. 2018;427:434–43.
Sellam J, Berenbaum F. The role of synovitis in pathophysiology and clinical symptoms of osteoarthritis. Nat Rev Rheumatol. 2010;6:625–35.
Wang H, Xu DX. A research review: poisonous bacteria lipopolysaccharide and development. Foreign Med Sci Hyg. 2008;35:170–3.
Shi H, Guo Y, Liu Y, Shi B, Guo X, Jin L, et al. The in vitro effect of lipopolysaccharide on proliferation, inflammatory factors and antioxidant enzyme activity in bovine mammary epithelial cells. Anim Nutr. 2016;2:99–104.
Caccese RG, Zimmerman JL, Carlson RP. Bacterial lipopolysaccharide potentiates type II collagen-induced arthritis in mice. Mediat Inflamm. 1992;1:273–9.
Lorenz W, Buhrmann C, Mobasheri A, Lueders C, Shakibaei M. Bacterial lipopolysaccharides form procollagen-endotoxin complexes that trigger cartilage inflammation and degeneration: implications for the development of rheumatoid arthritis. Arthritis Res Ther. 2013;15:R111.
Huang Z, Stabler T, Pei F, Kraus VB. Both systemic and local lipopolysaccharide (LPS) burden are associated with knee OA severity and inflammation Authors. Osteoarthr Cartil OARS Osteoarthr Res Soc. 2016;24:1769–75.
Krasnokutsky S, Samuels J, Abramson SB. Osteoarthritis in 2007. Bull NYU Hosp Jt Dis. 2007;65:222–8.
Liu-Bryan R. Synovium and the innate inflammatory network in osteoarthritis progression. Curr Rheumatol Rep. 2013;15:323.
Triantafilou M, Triantafilou K. Lipopolysaccharide recognition: CD14, TLRs and the LPS-activation cluster. Trends Immunol. 2002;23:301–4.
Cho J-S, Kang J-H, Um J-Y, Han I-H, Park I-H, Lee H-M. Lipopolysaccharide induces pro-inflammatory cytokines and mmp production via TLR4 in nasal polyp-derived fibroblast and organ culture. PLoS ONE. 2014;9:e90683.
Balkwill FR, Burke F. The cytokine network. Immunol Today. 1989;10:299–304.
Hoekzema R, Murray PI, van Haren MA, Helle M, Kijlstra A. Analysis of interleukin-6 in endotoxin-induced uveitis. Invest Ophthalmol Vis Sci. 1991;32:88–95.
Shida J, Trindade MC, Goodman SB, Schurman DJ, Smith RL. Induction of interleukin-6 release in human osteoblast-like cells exposed to titanium particles in vitro. Calcif Tissue Int. 2000;67:151–5.
Kapanen A, Kinnunen A, Ryhänen J, Tuukkanen J. TGF-β1 secretion of ROS-17/2.8 cultures on NiTi implant material. Biomaterials. 2002;23:3341–6.
Matsukawa A, Yoshimura T, Maeda T, Ohkawara S, Takagi K, Yoshinaga M. Neutrophil accumulation and activation by homologous IL-8 in rabbits. IL-8 induces destruction of cartilage and production of IL-1 and IL-1 receptor antagonist in vivo. J Immunol Baltim Md 1950. 1995;154:5418–25.
Birkedal-Hansen H, Moore WG, Bodden MK, Windsor LJ, Birkedal-Hansen B, DeCarlo A, et al. Matrix metalloproteinases: a review. Crit Rev Oral Biol Med Off Publ Am Assoc Oral Biol. 1993;4:197–250.
Pap T, Pap G, Hummel KM, Franz JK, Jeisy E, Sainsbury I, et al. Membrane-type-1 matrix metalloproteinase is abundantly expressed in fibroblasts and osteoclasts at the bone-implant interface of aseptically loosened joint arthroplasties in situ. J Rheumatol. 1999;26:166–9.
Murphy G, Nagase H. Reappraising metalloproteinases in rheumatoid arthritis and osteoarthritis: destruction or repair? Nat Clin Pract Rheumatol. 2008;4:128–35.
Karlsson C, Dehne T, Lindahl A, Brittberg M, Pruss A, Sittinger M, et al. Genome-wide expression profiling reveals new candidate genes associated with osteoarthritis. Osteoarthr Cartil. 2010;18:581–92.
Westacott CI, Sharif M. Cytokines in osteoarthritis: mediators or markers of joint destruction? Semin Arthritis Rheum. 1996;25:254–72.
Clements KM, Price JS, Chambers MG, Visco DM, Poole AR, Mason RM. Gene deletion of either interleukin-1beta, interleukin-1beta-converting enzyme, inducible nitric oxide synthase, or stromelysin 1 accelerates the development of knee osteoarthritis in mice after surgical transection of the medial collateral ligament and partial medial meniscectomy. Arthritis Rheum. 2003;48:3452–63.
Dinarello CA. Interleukin-1 and interleukin-1 antagonism. Blood. 1991;77:1627–52.
Goekoop RJ, Kloppenburg M, Kroon HM, Frölich M, Huizinga TWJ, Westendorp RGJ, et al. Low innate production of interleukin-1beta and interleukin-6 is associated with the absence of osteoarthritis in old age. Osteoarthr Cartil. 2010;18:942–7.
Henrotin YE, De Groote DD, Labasse AH, Gaspar SE, Zheng SX, Geenen VG, et al. Effects of exogenous IL-1 beta, TNF alpha, IL-6, IL-8 and LIF on cytokine production by human articular chondrocytes. Osteoarthr Cartil. 1996;4:163–73.
Guerne PA, Carson DA, Lotz M. IL-6 production by human articular chondrocytes. Modulation of its synthesis by cytokines, growth factors, and hormones in vitro. J Immunol Baltim Md 1950. 1990;144:499–505.
Lotz M, Terkeltaub R, Villiger PM. Cartilage and joint inflammation. Regulation of IL-8 expression by human articular chondrocytes. J Immunol Baltim Md 1950. 1992;148:466–73.
Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier J-P, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol. 2011;7:33–42.
de Isla NG, Stoltz JF. In vitro inhibition of IL-1beta catabolic effects on cartilage: a mechanism involved on diacerein anti-OA properties. Biorheology. 2008;45:433–8.
Logar DB, Komadina R, Prezelj J, Ostanek B, Trost Z, Marc J. Expression of bone resorption genes in osteoarthritis and in osteoporosis. J Bone Miner Metab. 2007;25:219–25.
Ray A, Kuroki K, Cook JL, Bal BS, Kenter K, Aust G, et al. Induction of matrix metalloproteinase 1 gene expression is regulated by inflammation-responsive transcription factor SAF-1 in osteoarthritis. Arthritis Rheum. 2003;48:134–45.
Heinrich PC, Castell JV, Andus T. Interleukin-6 and the acute phase response. Biochem J. 1990;265:621–36.
Evans CA, Jellis J, Hughes SP, Remick DG, Friedland JS. Tumor necrosis factor-alpha, interleukin-6, and interleukin-8 secretion and the acute-phase response in patients with bacterial and tuberculous osteomyelitis. J Infect Dis. 1998;177:1582–7.
Massicotte F, Lajeunesse D, Benderdour M, Pelletier J-P, Hilal G, Duval N, et al. Can altered production of interleukin-1beta, interleukin-6, transforming growth factor-beta and prostaglandin E(2) by isolated human subchondral osteoblasts identify two subgroups of osteoarthritic patients. Osteoarthr Cartil. 2002;10:491–500.
Kwan Tat S, Pelletier J-P, Lajeunesse D, Fahmi H, Lavigne M, Martel-Pelletier J. The differential expression of osteoprotegerin (OPG) and receptor activator of nuclear factor kappaB ligand (RANKL) in human osteoarthritic subchondral bone osteoblasts is an indicator of the metabolic state of these disease cells. Clin Exp Rheumatol. 2008;26:295–304.
Harada A, Sekido N, Akahoshi T, Wada T, Mukaida N, Matsushima K. Essential involvement of interleukin-8 (IL-8) in acute inflammation. J Leukoc Biol. 1994;56:559–64.
Takahashi A, de Andrés MC, Hashimoto K, Itoi E, Oreffo ROC. Epigenetic regulation of interleukin-8, an inflammatory chemokine, in osteoarthritis. Osteoarthr Cartil. 2015;23:1946–54.
Yoshihara Y, Nakamura H, Obata K, Yamada H, Hayakawa T, Fujikawa K, et al. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in synovial fluids from patients with rheumatoid arthritis or osteoarthritis. Ann Rheum Dis. 2000;59:455–61.
Jackson MT, Moradi B, Smith MM, Jackson CJ, Little CB. Activation of matrix metalloproteinases 2, 9, and 13 by activated protein C in human osteoarthritic cartilage chondrocytes. Arthritis Rheumatol Hoboken Nj. 2014;66:1525–36.
Tío L, Martel-Pelletier J, Pelletier J-P, Bishop PN, Roughley P, Farran A, et al. Characterization of opticin digestion by proteases involved in osteoarthritis development. Jt Bone Spine Rev Rhum. 2014;81:137–41.
Zeng GQ, Chen AB, Li W, Song JH, Gao CY. High MMP-1, MMP-2, and MMP-9 protein levels in osteoarthritis. Genet Mol Res Gmr. 2015;14:14811–22.
Goldring MB, Marcu KB. Cartilage homeostasis in health and rheumatic diseases. Arthritis Res Ther. 2009;11:224.
Sakao K, Takahashi KA, Arai Y, Saito M, Honjo K, Hiraoka N, et al. Osteoblasts derived from osteophytes produce interleukin-6, interleukin-8, and matrix metalloproteinase-13 in osteoarthritis. J Bone Miner Metab. 2009;27:412–23.
Ohta S. Recent progress toward hydrogen medicine: potential of molecular hydrogen for preventive and therapeutic applications. Curr Pharm Des. 2011;17:2241–52.
Ohta S. Molecular hydrogen as a preventive and therapeutic medical gas: initiation, development and potential of hydrogen medicine. Pharmacol Ther. 2014;144:1–11.
Ishibashi T. Molecular hydrogen: new antioxidant and anti-inflammatory therapy for rheumatoid arthritis and related diseases. Curr Pharm Des. 2013;19:6375–81.
Iuchi K, Imoto A, Kamimura N, Nishimaki K, Ichimiya H, Yokota T, et al. Molecular hydrogen regulates gene expression by modifying the free radical chain reaction-dependent generation of oxidized phospholipid mediators. Sci Rep. 2016;6:18971.
Yeung KWK, Poon RWY, Chu PK, Chung CY, Liu XY, Lu WW, et al. Surface mechanical properties, corrosion resistance, and cytocompatibility of nitrogen plasma-implanted nickel-titanium alloys: a comparative study with commonly used medical grade materials. J Biomed Mater Res A. 2007;82:403–14.
Li Q, Xia Y-Y, Tang J-C, Wang R-Y, Bei C-Y, Zeng Y. In vitro and in vivo biocompatibility investigation of diamond-like carbon coated nickel-titanium shape memory alloy. Artif Cells Blood Substit Immobil Biotechnol. 2011;39:137–42.
Sun T, Wang L-P, Wang M, Tong H-W, Lu WW. Characteristics and in vitro biological assessment of (Ti, O, N)/Ti composite coating formed on NiTi shape memory alloy. Thin Solid Films. 2011;519:4623–8.
Markhoff J, Krogull M, Schulze C, Rotsch C, Hunger S, Bader R. Biocompatibility and Inflammatory Potential of Titanium Alloys Cultivated with Human Osteoblasts, Fibroblasts and Macrophages. Materials. 2017;10:52.
Acknowledgements
The authors acknowledge financial support from Czech Science Foundation under the contract no. 15-16336 S.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Válková, L., Ševčíková, J., Pávková Goldbergová, M. et al. Osteoarthritic process modifies expression response to NiTi alloy presence. J Mater Sci: Mater Med 29, 146 (2018). https://doi.org/10.1007/s10856-018-6156-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-018-6156-z