Abstract
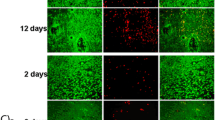
The aim was to evaluate the biocompatibility of osteosynthesis plates of the MgYREZr/WE43 alloy by using human cells in vitro. Eluates of degradable magnesium osteosynthesis plates as well as halved plates were used for incubation with human osteoblasts, fibroblasts and osteosarcoma cells. The cell viability was evaluated by using FDA/PI-Staining and LDH analysis. Cell proliferation was assessed by MTT, WST-Test and BrdU-ELISA. Scanning electron microscope was used for investigation of the cell adhesion. The number of devitalized cells in all treatment groups did not significantly deviate from the control group. According to MTT results, the number of metabolically active cells was not significantly affected by the addition of the eluates. The number of metabolically active cells was reduced by 24 to 38% compared to the control on incubation in direct contact with the osteosynthesis plates. The proliferation of the cells was inhibited by the addition of the eluates. While the eluate of the half-hour elution has only a very small effect, the 24 h eluate significantly inhibits proliferation by 23–25% compared to the control. The roughened surface of the magnesium osteosynthesis plate after incubation showed adherent cells. However, some areas of the plates were also free of adherent cells. WE43 based magnesium alloys showed favorable biocompatibility considering the viability of the cells evaluated; however, proliferation rates were reduced in a time dependent manner, especially in fibroblast group. This might be a potential clinical benefit of magnesium osteosynthesis plates and their superiority to titanium, thus the fibroblastic ingrowth might negatively influence the bone-plate contact.
Graphical abstract







Similar content being viewed by others
References
Park HC, Kim SG (2016) Mini-plate Remov Maxillofac Trauma Patients a five-year Retrosp Study 42(4):182–6. doi:10.5125/jkaoms.2016.42.4.182.
Rallis G, Mourouzis C, Papakosta V, Papanastasiou G, Zachariades N. Reasons for miniplate removal following maxillofacial trauma: a 4-year study. J Cranio-Maxillo-Facial Surg. 2006;34(7):435–9. doi:10.1016/j.jcms.2006.07.001.
Pan Z, Patil PM. Titanium osteosynthesis hardware in maxillofacial trauma surgery: to remove or remain? A retrospective study. Eur J Trauma Emerg Surg. 2014;40(5):587–91. doi:10.1007/s00068-013-0348-5.
Falter B, Schepers S, Vrielinck L, Lambrichts I, Politis C. Plate removal following orthognathic surgery. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endod. 2011;112(6):737–43. doi:10.1016/j.tripleo.2011.01.011.
Arnett TR. Extracellular pH regulates bone cell function. J Nutr. 2008;138(2):415S–8S.
Sun H, Luo CF, Zhong B, Shi HP, Zhang CQ, Zeng BF. A prospective, randomised trial comparing the use of absorbable and metallic screws in the fixation of distal tibiofibular syndesmosis injuries: mid-term follow-up. Bone Jt J. 2014;96-B(4):548–54. doi:10.1302/0301-620X.96B4.32171.
Ahmad N, Lyles J, Panchal J, Deschamps-Braly J. Outcomes and complications based on experience with resorbable plates in pediatric craniosynostosis patients. J Craniofacial Surg. 2008;19(3):855–60. doi:10.1097/SCS.0b013e31816ae358.
Arnaud E, Renier D. Pediatric craniofacial osteosynthesis and distraction using an ultrasonic-assisted pinned resorbable system: a prospective report with a minimum 30 months’ follow-up. J Craniofacial Surg. 2009;20(6):2081–6. doi:10.1097/SCS.0b013e3181be8854.
Weizbauer A, Modrejewski C, Behrens S, Klein H, Helmecke P, Seitz JM, et al. Comparative in vitro study and biomechanical testing of two different magnesium alloys. J Biomater Appl. 2014;28(8):1264–73. doi:10.1177/0885328213506758.
Willbold E, Kalla K, Bartsch I, Bobe K, Brauneis M, Remennik S, et al. Biocompatibility of rapidly solidified magnesium alloy RS66 as a temporary biodegradable metal. Acta Biomater. 2013;9(10):8509–17. doi:10.1016/j.actbio.2013.02.015.
Imwinkelried T, Beck S, Iizuka T, Schaller B. Effect of a plasmaelectrolytic coating on the strength retention of in vivo and in vitro degraded magnesium implants. Acta Biomater. 2013;9(10):8643–9. doi:10.1016/j.actbio.2012.08.047.
Sonnow L, Konneker S, Vogt PM, Wacker F, von Falck C. Biodegradable magnesium Herbert screw - image quality and artifacts with radiography, CT and MRI. BMC Med Imaging. 2017;17(1):16 doi:10.1186/s12880-017-0187-7.
Hampp C, Angrisani N, Reifenrath J, Bormann D, Seitz JM, Meyer-Lindenberg A. Evaluation of the biocompatibility of two magnesium alloys as degradable implant materials in comparison to titanium as non-resorbable material in the rabbit. Mater Sci & Eng C, Mater Biol Appl. 2013;33(1):317–26. doi:10.1016/j.msec.2012.08.046.
Schaller B, Saulacic N, Beck S, Imwinkelried T, Goh BT, Nakahara K, et al. In vivo degradation of a new concept of magnesium-based rivet-screws in the minipig mandibular bone. Mater Sci & Eng C, Mater Biol Appl. 2016;69:247–54. doi:10.1016/j.msec.2016.06.085.
Castellani C, Lindtner RA, Hausbrandt P, Tschegg E, Stanzl-Tschegg SE, Zanoni G, et al. Bone-implant interface strength and osseointegration: biodegradable magnesium alloy versus standard titanium control. Acta Biomater. 2011;7(1):432–40. doi:10.1016/j.actbio.2010.08.020.
Tamimi F, Le Nihouannen D, Bassett DC, Ibasco S, Gbureck U, Knowles J, et al. Biocompatibility of magnesium phosphate minerals and their stability under physiological conditions. Acta Biomater. 2011;7(6):2678–85. doi:10.1016/j.actbio.2011.02.007.
Charyeva O, Dakischew O, Sommer U, Heiss C, Schnettler R, Lips KS. Biocompatibility of magnesium implants in primary human reaming debris-derived cells stem cells in vitro. J Orthop Traumatol. 2016;17(1):63–73. doi:10.1007/s10195-015-0364-9.
Liao Y, Xu Q, Zhang J, Niu J, Yuan G, Jiang Y, et al. Cellular response of chondrocytes to magnesium alloys for orthopedic applications. Int J Mol Med. 2015;36(1):73–82. doi:10.3892/ijmm.2015.2211.
Yu W, Zhao H, Ding Z, Zhang Z, Sun B, Shen J, et al. In vitro and in vivo evaluation of MgF2 coated AZ31 magnesium alloy porous scaffolds for bone regeneration. Colloids Surf B, Biointerfaces. 2017;149:330–40. doi:10.1016/j.colsurfb.2016.10.037.
Ahmad Agha N, Willumeit-Romer R, Laipple D, Luthringer B, Feyerabend F. The degradation interface of magnesium based alloys in direct contact with human primary osteoblast cells. PloS ONE. 2016;11(6):e0157874 doi:10.1371/journal.pone.0157874.
Guo Y, Liu W, Ma S, Wang J, Zou J, Liu Z, et al. A preliminary study for novel use of two Mg alloys (WE43 and Mg3Gd). J Mater Sci Mater Med. 2016;27(5):82 doi:10.1007/s10856-016-5691-8.
Okawachi H, Ayukawa Y, Atsuta I, Furuhashi A, Sakaguchi M, Yamane K, et al. Effect of titanium surface calcium and magnesium on adhesive activity of epithelial-like cells and fibroblasts. Biointerphases. 2012;7(1-4):27 doi:10.1007/s13758-012-0027-9.
Tsutsumi K, Fujikawa H, Kajikawa T, Takedachi M, Yamamoto T, Murakami S. Effects of L-ascorbic acid 2-phosphate magnesium salt on the properties of human gingival fibroblasts. J Periodontal Res. 2012;47(2):263–71. doi:10.1111/j.1600-0765.2011.01430.x.
Bornapour M, Muja N, Shum-Tim D, Cerruti M, Pekguleryuz M. Biocompatibility and biodegradability of Mg-Sr alloys: the formation of Sr-substituted hydroxyapatite. Acta Biomater. 2013;9(2):5319–30. doi:10.1016/j.actbio.2012.07.045.
Witte F, Fischer J, Nellesen J, Crostack HA, Kaese V, Pisch A, et al. In vitro and in vivo corrosion measurements of magnesium alloys. Biomaterials. 2006;27(7):1013–8. doi:10.1016/j.biomaterials.2005.07.037.
Kubasek J, Vojtech D, Lipov J, Ruml T. Structure, mechanical properties, corrosion behavior and cytotoxicity of biodegradable Mg-X (X = Sn, Ga, In) alloys. Mater Sci & Eng C, Mater Biol Appl. 2013;33(4):2421–32. doi:10.1016/j.msec.2013.02.005.
Kraus T, Fischerauer SF, Hanzi AC, Uggowitzer PJ, Loffler JF, Weinberg AM. Magnesium alloys for temporary implants in osteosynthesis: in vivo studies of their degradation and interaction with bone. Acta Biomater. 2012;8(3):1230–8. doi:10.1016/j.actbio.2011.11.008.
Li Z, Gu X, Lou S, Zheng Y. The development of binary Mg-Ca alloys for use as biodegradable materials within bone. Biomaterials. 2008;29(10):1329–44. doi:10.1016/j.biomaterials.2007.12.021.
Witte F, Ulrich H, Rudert M, Willbold E. Biodegradable magnesium scaffolds: Part 1: appropriate inflammatory response. J Biomed Mater Res Part A. 2007;81(3):748–56. doi:10.1002/jbm.a.31170.
Kuhlmann J, Bartsch I, Willbold E, Schuchardt S, Holz O, Hort N, et al. Fast escape of hydrogen from gas cavities around corroding magnesium implants. Acta Biomater. 2013;9(10):8714–21. doi:10.1016/j.actbio.2012.10.008.
Wang J, Jiang H, Bi Y, Sun J, Chen M, Liu D. Effects of gas produced by degradation of Mg-Zn-Zr alloy on cancellous bone tissue. Mater Sci & Eng C, Mater Biol Appl. 2015;55:556–61. doi:10.1016/j.msec.2015.05.082.
Schaller B, Saulacic N, Imwinkelried T, Beck S, Liu EW, Gralla J, et al. In vivo degradation of magnesium plate/screw osteosynthesis implant systems: Soft and hard tissue response in a calvarial model in miniature pigs. J Cranio-Maxillo-Facial Surg. 2016;44(3):309–17. doi:10.1016/j.jcms.2015.12.009.
Thomann M, Krause C, Angrisani N, Bormann D, Hassel T, Windhagen H, et al. Influence of a magnesium-fluoride coating of magnesium-based implants (MgCa0.8) on degradation in a rabbit model. J Biomed Mater Res Part A. 2010;93(4):1609–19. doi:10.1002/jbm.a.32639.
Keim S, Brunner JG, Fabry B, Virtanen S. Control of magnesium corrosion and biocompatibility with biomimetic coatings. J Biomed Mater Res Part B, Appl Biomater. 2011;96(1):84–90. doi:10.1002/jbm.b.31742.
Yang J, Cui F, Lee IS. Surface modifications of magnesium alloys for biomedical applications. Ann Biomed Eng. 2011;39(7):1857–71. doi:10.1007/s10439-011-0300-y.
Cui W, Beniash E, Gawalt E, Xu Z, Sfeir C. Biomimetic coating of magnesium alloy for enhanced corrosion resistance and calcium phosphate deposition. Acta Biomater. 2013;9(10):8650–9. doi:10.1016/j.actbio.2013.06.031.
Acknowledgements
Funding
This research was funded by the Medical Faculty of the University of Kiel (Junior Research Funding/financing key F355930).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Naujokat, H., Gülses, A., Wiltfang, J. et al. Effects of degradable osteosynthesis plates of MgYREZr alloy on cell function of human osteoblasts, fibroblasts and osteosarcoma cells. J Mater Sci: Mater Med 28, 126 (2017). https://doi.org/10.1007/s10856-017-5938-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-017-5938-z