Abstract
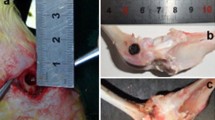
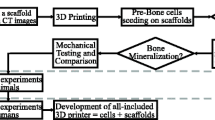
In the surgical treatment of tuberculosis of the bones, excision of the lesion site leaves defects in the bone structure. Recent research has shown benefits for bone tissue support, such as tricalcium phosphate, as regrowth materials. These biocompatible engineering materials have good bone inductivity and biologic mechanical performance. The goal of this study was to evaluate the use of 3D printing, a new technology, to design and build 3-dimensional support structures for use in grafting at lesion sites and for use in embedding the sustained release anti-tuberculosis drugs Rifampin and Isoniazid and determine the in vivo performance of these structures. In addition to mechanical studies, osteogenesis, cell viability, and migration were all observed, using Wistar rat models, to determine the effectiveness of this material as a biological support. The bone support showed good resistance to compression, similar to the spongiest bone tissue, and high porosity. In vivo studies showed that the material had a stable time release of Rifampin and Isoniazid through 90 days and achieved effective killing of the tuberculosis-causing bacteria. Finally, the support allowed for good migration and survival of rat bone marrow mesenchymal stem cells, leading to successful bone regrowth and repair. These results imply that the use of 3D printing of tricalcium phosphate scaffolds for bone excision repair and time-release treatment of tuberculosis shows great promise for future treatment of patients with tuberculosis of the bones.







Similar content being viewed by others
References
Pigrau-Serrallach C, Rodríguez-Pardo D (2013) Bone and joint tuberculosis. Eur Spine J 22(4):556–566
Ye X, Zhen P, Li X et al (2010) Study on preparation and properties of novel anti-TB porous calcium phosphate cement. Orthop J Chin 18(23):1981–1986
Gu Y, Chen X, Lee J-H et al (2012) Inkjet printed antibiotic-and calcium-eluting bioresorbable nanocomposite micropatterns for orthopedic implants. Acta Biomater 8(1):424–431
Wu W, Zheng Q, Guo X (2010) Experimental Study of a Rifampicine-isoniazid-controlled Release Drug Implant. Chin J Biomed Eng 1:137–143
Liu P, Jiang J (2011) High performance liquid chromatagraphy to test rifampin and desacetylrifampin in spinal tuberculosis. J Chin Med Univ 40(7):665–668
Li D, Ma Y (2013) Research progresses of drug delivery material in the treatment of osteoaticular tuberculosis. Chin J Antituberc 35(5):25–32
Chen Q (2013) Study on the Toxicity of Isoniazide with Various Concentrations on Cultured Osteoblasts in vitro[D]. huazhong university of science and technology 31(3):21–27
Guo D, Wu H, Xue G et al (2011) The hepatocyet toxicity and the effect of Isoniazid and Rifampicin on the activities of CYP2E1 and CYP3A in mouse primary hepatocytes. Pham J Chin PLA 27(3):221–223
Mao K, Yang Y, Li J et al (2009) Investigation of the histology and interfacial bonding between carbonated hydroxyapatite cement and bone. Biomed Mater 4(4):045003
Rihn JA, Kirkpatrick K, Albert TJ (2010) Graft options in posterolateral and posterior interbody lumbar fusion. Spine 35(17):1629–1639
Schroeder JE, Mosheiff (2011) Tissue engineering approaches for bone repair: concepts and evidence. Injury 42(6):609–613
Sugawara A, Asaoka K, Ding SJ (2013) Calcium phosphate-based cements: clinical needs and recent progress. J Mater Chem B 1(8):1081–1089
Dorozhkin SV (2010) Bioceramics of calcium orthophosphates. Biomaterials 31(7):1465–1485
Wu C, Chang J (2013) A review of bioactive silicate ceramics. Biomed Mater 8(3):032001
Nischang I, Teasdale I, Brüggemann O (2011) Porous polymer monoliths for small molecule separations: advancements and limitations. Anal Bioanal Chem 400(8):2289–2304
Lu L, Zhang Q, Wootton D et al (2012) Biocompatibility and biodegradation studies of PCL/β-TCP bone tissue scaffold fabricated by structural porogen method. J Mater Sci 23(9):2217–2226
Butscher A, Bohner M, Hofmann S et al (2011) Structural and material approaches to bone tissue engineering in powder-based three-dimensional printing. Acta Biomater 7(3):907–920
Wei X, Zhao N, Lin Z et al (2013) Preparation and characterization of three-dimensional porus β-tricalcium phosphate scaffold with controlled porous. J Funct Mater 43(23):3217–3221
Bao Y, Zhang W, Wang Y et al (2012) Preparation and release features of long-term slow-release two-component drug artificial bone. Chin J Tissue Eng Res 16(38):7126–7130
Karageorgiou V, Kaplan D (2005) Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 26(27):5474–5491
Miranda P, Pajares A, Saiz E et al (2007) Fracture modes under uniaxial compression in hydroxyapatite scaffolds fabricated by robocasting. J Biomed Mater Res Part A 83(3):646–655
Miranda P, Pajares A, Guiberteau F (2008) Finite element modeling as a tool for predicting the fracture behavior of robocast scaffolds. Acta Biomater 4(6):1715–1724
Bandyopadhyay A, Petersen J, Fielding G et al (2012) ZnO, SiO2, and SrO doping in resorbable tricalcium phosphates: Influence on strength degradation, mechanical properties, and in vitro bone–cell material interactions. J Biomed Mater Res B 100(8):2203–2212
Olszta MJ, Cheng X, Jee SS et al (2007) Bone structure and formation: A new perspective. Mater Sci Eng 58(3):77–116
Libicher M, Vetter M, Wolf I et al (2005) CT volumetry of intravertebral cement after kyphoplasty. Comparison of polymethylmethacrylate and calcium phosphate in a 12-month follow-up. Eur Radiol 15(8):1544–1549
Walsh WR, Vizesi F, Michael D et al (2008) β-TCP bone graft substitutes in a bilateral rabbit tibial defect model. Biomaterials 29(3):266–271
Santos CF, Silva AP, Lopes L et al (2012) Design and production of sintered β-tricalcium phosphate 3D scaffolds for bone tissue regeneration. Mater Sci Eng C 32(5):1293–1298
Wu Q, Zhang X, Wu B et al (2013) Fabrication and characterization of porous HA/β-TCP scaffolds strengthened with micro-ribs structure. Mater Lett 92:274–277
Best S, Porter A, Thian E et al (2008) Bioceramics: past, present and for the future. J Eur Ceram Soc 28(7):1319–1327
Cao H, Kuboyama N (2010) A biodegradable porous composite scaffold of PGA/β-TCP for bone tissue engineering. Bone 46(2):386–395
Wu S, Liu X, Yeung KW et al (2014) Biomimetic porous scaffolds for bone tissue engineering. Mater Sci Eng 80:1–36
Chu X, Zhao P, Sun K et al (2009) Properties research of β-tricalcium phosphate bone cements. J Ceram 3:295–299
Bose S, Vahabzadeh S, Bandyopadhyay A (2013) Bone tissue engineering using 3D printing. Mater Today 16(12):496–504
Li M, Liu X, Liu X et al (2009) Development of macroporous calcium phosphate cements as bone substitutes by using gelatin microspheres. Orthop J Chin 7:526–529
Saifullah B, Hussein M, Hussein Al Ali S (2011) Controlled-release approaches towards the chemotherapy of tuberculosis. Int J Nanomed 7:5451–5463
Sweetman SC (2005) Martindale: the extra pharmacopoeia. Pharmaceutical Press, London, pp 1371–1377
Rang H, Dale M, Rither J (1999) Drugs used to treat tuberculosis. Pharmacology, 4th edn. Churchill Livingstone, London, pp 703–707
Li G, Zhang J, Zhao X et al (2012) Correlation between levels of isoniazid and rifampicin resistance andlargeted gene mutation in mycobacrerium tuberculosis. Chin J Antituberc 34(6):360–365
Wang Z, Shi J, Geng G et al (2013) Ultra-short-course chemotherapy for spinal tuberculosis: five years of observation. Eur Spine J 22(2):274–281
Bose S, Roy M, Bandyopadhyay A (2012) Recent advances in bone tissue engineering scaffolds. Trends Biotechnol 30(10):546–554
Duarte Campos DF, Vogt M, Lindner M et al (2014) Two-photon laser scanning microscopy as a useful tool for imaging and evaluating macrophage-, IL-4 activated macrophage-and osteoclast-based in vitro degradation of beta-tricalcium phosphate bone substitute material. Microsc Res Tech 77(2):143–152
Acknowledgements
The authors wish to thank the Lanzhou Military Region General Hospital Orthopedics Research Institute and Professor Zhen Ping. This study was funded by the National Natural Sciences Fund (81371983).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yuan, J., Zhen, P., Zhao, H. et al. The preliminary performance study of the 3D printing of a tricalcium phosphate scaffold for the loading of sustained release anti-tuberculosis drugs. J Mater Sci 50, 2138–2147 (2015). https://doi.org/10.1007/s10853-014-8776-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-014-8776-0