Abstract
Purpose
This study aimed to explore the feasibility of ultra-short-course chemotherapy in the treatment of spinal tuberculosis.
Methods
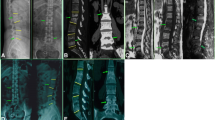
One hundred and eighty-five patients with confirmed spinal tuberculosis and surgical indication were included. The chemotherapy regimen was 2SHRZ/XHRZ. According to the duration of the chemotherapy, the patients were divided into two groups, the ultra-short-course chemotherapy group with an average duration of 4.5 months, and the standard chemotherapy group with an average duration of 9 months. The same surgery was performed for patients in the two groups.
Results
The duration of the follow-up ranged from 61 to 87 months, with an average of 69.1 months. Erythrocyte sedimentation rate and C-reactive protein, kyphosis and nerve function, recovery of work, and activities of daily living were not significantly different between the two groups before or after treatment; however, the aforementioned indices were significantly different before and after treatment within groups. There was no significant difference in postoperative bone graft healing between the two groups. The drug side effects were significantly different between the two groups.
Conclusions
With thorough focus debridement, bone grafting, and internal fixation, the efficacy of ultra-short chemotherapy was similar to that of standard chemotherapy for the treatment of spinal tuberculosis. The ultra-short-course chemotherapy can shorten the course of treatment and reduce drug side effects.
Similar content being viewed by others
References
Jain AK (2010) Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br 92(7):905–913
Tuli SM (2007) Tuberculosis of the spine: a historical review. Clin Orthop Relat Res 460:29–38
Won Park Dae, Sohn JW, Kim E-H et al (2007) Outcome and management of spinal tuberculosis according to the severity of disease. Spine 32(4):E130–E135
Rosenthal IM, Zhang M, Williams KN et al (2007) Daily dosing of rifapentine cures tuberculosis in three months or less in the murine model. PLoS Med. 4(12):e344
Davies GR, Nuermberger EL (2008) Pharmacokinetics and pharmacodynamics in the development of anti-tuberculosis drugs. Tuberculosis (Edinb) 88(S1):S65–S74
Nuermberger EL, Spigelman MK, Yew WW (2010) Current development and future prospects in chemotherapy of tuberculosis. Respirology 15(5):764–778
Young DB, Perkins MD, Duncan K (2008) Confronting the scientific obstacles to global control of tuberculosis. J Clin Invest 118(4):1255–1265
Kreis B, Pretet S, Birenbaum J et al (1976) Two three-month treatment regimens for pulmonary tuberculosis. Bull Int Union Tuberc 51(1):71–75
National Collaborative Group of short-course chemotherapy for pulmonary tuberculosis (1998) Five-month short-course chemotherapy and six-month whole-course intermittent regimen for the treatment of smear-positive pulmonary tuberculosis: a controlled clinical study. Chin J Tuberc Respir Dis 21:388–391
Wang Z, Ge Z, Jin W et al (2007) Treatment of spinal tuberculosis with ultrashort-course chemotherapy in conjunction with partial excision of pathologic vertebrae. Spine J. 7(6):671–681
Moon MS, Woo YK, Lee KS et al (1995) Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine 20:1910–1916
Xia A, Zhan S (2007) Comprehensive analysis of the incidence of anti-tuberculosis drug-induced adverse reactions in China. Chin J Tuberc Respir Dis 30:419–423
Jin W, Wang Z, Ma X et al (2009) Clinical analysis of side effects of anti-tuberculosis drugs in 156 patients with spinal tuberculosis. Trans Third Military Med Univ 31:1932–1936
East African/British Medical Reasearch Council (1972) Controlled clinical trial of short-course (6-month) regimens of chemotherapy for treatmen of pulmonary tuberculosis. Lanced, 1:1079–1085
Cattamanchi A, Dantes RB, Metcalfe JZ et al (2009) Clinical characteristics and treatment outcomes of patients with isoniazid-monoresistant tuberculosis. Clin Infect Dis 48(2):179–185
Swaminathan S, Deivanayagam CN, Rajasekaran S et al (2008) Long term follow up of HIV-infected patients with tuberculosis treated with 6-month intermittent short course chemotherapy. Natl Med J India 21(1):3–8
Guo LX, Ma YZ, Chen X et al (2010) Clinical study of short-course chemotherapy combined with radical operation in retreating spinal tuberculosis. Zhongguo Gu Shang. 23(7):491–494
Parthasarathy R, Sriram K, Santha T et al (1999) Short-course chemotherapy for tuberculosis of the spine A comparison between ambulant treatmentand radical surgery-ten-year report. J BoneJoint Surge (Br). 81:464–471
Xiao C, Fu Y, Li Z et al (1997) Initial studies on short-course chemotherapy with irregular chemotherapeutic terms. Chin J Tuberc Respir 20:258–260
Blumberg HM, Burman WJ, Chaisson RE et al (2003) American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med 167:603–662
Arora S, Sabat D, Maini L et al (2011) The results of nonoperative treatment of craniovertebral junction tuberculosis: a review of twenty-six cases. J Bone Joint Surg Am 93(6):540–547
Mwachaka PM, Ranketi SS et al (2011) Spinal tuberculosis among human immunodeficiency virus-negative patients in a Kenyan tertiary hospital: a 5-year synopsis. Spine J. 11(4):265–269
Hoffman EB, Crosier JH, Cremin BJ (1993) Imaging in children with spinal tuberculosis: a comparison of radiography, computed tomography and magnetic resonance imaging. J Bone Joint Surg [Br] 75-B:233–239
Ge Z, Wang Z, Wei M (2008) Measurement of the concentration of three antituberculosis drugs in the focus of spinal tuberculosis. Eur Spine J 17(11):1482–1487
Erturer E, Tezer M, Aydogan M et al (2010) The results of simultaneous posterior-anterior-posterior surgery in multilevel tuberculosis spondylitis associated with severe kyphosis. Eur Spine J 19(12):2209–2215
Moon MS, Kim SS, Lee BJ et al (2011) Surgical management of severe rigid tuberculous kyphosis of dorsolumbar spine. Int Orthop 35(1):75–81
Erturer E, Tezer M, Aydogan M et al (2010) The results of simultaneous posterior-anterior-posterior surgery in multilevel tuberculosis spondylitis associated with severe kyphosis. Eur Spine J 19(12):2209–2215
Wang Y, Zhang Y, Zhang X et al (2009) Posterior-only multilevel modified vertebral column resection for extremely severe Pott’s kyphotic deformity. Eur Spine J 18(10):1436–1441
Steffen R, Menzies D, Oxlade O et al (2010) Patients’ costs and cost-effectiveness of tuberculosis treatment in DOTS and non-DOTS facilities in Rio de Janeiro, Brazil. PLoS ONE 5(11):e14014
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Z., Shi, J., Geng, G. et al. Ultra-short-course chemotherapy for spinal tuberculosis: five years of observation. Eur Spine J 22, 274–281 (2013). https://doi.org/10.1007/s00586-012-2536-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2536-0