Abstract
Purpose
Atrial fibrillation is associated with an increased risk of cognitive impairment. It is unclear whether the restoration of sinus rhythm with catheter ablation may modify this risk. We conducted a systematic review of studies comparing cognitive outcomes following catheter ablation with medical therapy (rate and/or rhythm control) in atrial fibrillation.
Methods
Searches were performed on the following databases from their inception to 17 October 2021: PubMed, OVID Medline, Embase and Cochrane Library. The inclusion criteria comprised studies comparing catheter ablation against medical therapy (rate and/or rhythm control in conjunction with anticoagulation where appropriate) which included cognitive assessment and/or a diagnosis of dementia as an outcome.
Results
A total of 599 records were screened. Ten studies including 15,886 patients treated with catheter ablation and 42,684 patients treated with medical therapy were included. Studies which compared the impact of catheter ablation versus medical therapy on quantitative assessments of cognitive function yielded conflicting results. In studies, examining new onset dementia during follow-up, catheter ablation was associated with a lower risk of subsequent dementia diagnosis compared to medical therapy (hazard ratio: 0.60 (95% confidence interval 0.42–0.88, p < 0.05)).
Conclusion
The accumulating evidence linking atrial fibrillation with cognitive impairment warrants the design of atrial fibrillation treatment strategies aimed at minimising cognitive decline. However, the impact of catheter ablation and atrial fibrillation medical therapy on cognitive decline is currently uncertain. Future studies investigating atrial fibrillation treatment strategies should include cognitive outcomes as important clinical endpoints.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The prevalence of atrial fibrillation increases with age and atrial fibrillation results in an increased risk of morbidity and mortality from stroke and congestive cardiac failure amongst other chronic diseases [1]. Improvements in life expectancy have contributed to an increased prevalence of dementia [2]. Although there is accumulating evidence of a causal link between atrial fibrillation and cognitive impairment [3], the mechanism of interaction is unknown.
Atrial fibrillation treatment is heterogenous comprising the use of rhythm control, rate control and anticoagulation therapy. The impact of these treatment strategies on cognition is unclear. Rhythm control with catheter ablation may be more successful at restoring and maintaining sinus rhythm than anti-arrhythmic drugs [4]. However, catheter ablation is also associated with an increased risk of cerebral emboli, particularly in the immediate post-ablation period [5]. Studies which have examined cognition before and after atrial fibrillation ablation have provided conflicting results [6,7,8,9]. We hypothesised that the risk of cognitive decline may differ in atrial fibrillation patients treated with catheter ablation compared with medical therapy.
The aim of this study was therefore to provide a systematic assessment of the effect of catheter ablation versus medical therapy on cognitive function. We present a systematic review of the available literature assessing cognitive function following catheter ablation compared to medical therapy (comprising rhythm and/or rate control in conjunction with anticoagulation where appropriate) for all patients with atrial fibrillation.
2 Methods
This study was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines [10].
2.1 Data sources and searches
The PubMed, Ovid MEDLINE, Embase and Cochrane Library databases were searched from their inception to 17 October 2021. Reference lists of included articles were examined for additional studies. The search terms utilised were as follows: “atrial fibrillation” or “a fib” or “afib” or “AF” AND “cognition” or “cognitive impairment” or “cognitive” or “$dementia” or “$alzheimer” or “lewy” or “memory” or “vascular dementia” or “frontotemporal lobar” AND “catheter ablation” or “rfa” or “radiofrequency ablation” or “ablation” or “ca” or “cryoablation” or “cryoballoon” or “pulmonary vein.”
2.2 Study selection and outcomes
Studies were included according to the following criteria: (1) studies which assessed cognitive function; (2) studies which included a diagnosis of dementia and/or its subtypes as an outcome; (3) studies which included both a group of atrial fibrillation patients treated with catheter ablation and patients treated with medical therapy (rate and/or rhythm control in conjunction with anticoagulation where appropriate). The following exclusion criteria were applied: (1) studies which did not include a group of patients treated with catheter ablation; (2) studies which did not include a group of patients treated with medical therapy; (3) case reports, editorials, reviews, conference proceedings and guidelines were excluded.
References were obtained and uploaded to Rayyan software [11]. Duplicate articles were removed. Two independent reviewers (NB and RY) screened the titles and abstracts of the studies. Articles considered relevant were advanced to full text review. Disagreements were resolved by consensus decision amongst the two authors. It was planned for a third reviewer (SEW) to arbitrate if disagreements could not be resolved; however, this was not required.
Outcomes assessed included diagnosis of dementia and its subtypes. These were ascertained according to International Classification of Disease coding data. Changes in cognitive function were assessed. We categorised these changes as (1) changes ≤ 3 months after therapy and (2) changes > 3 months after therapy.
2.3 Data extraction and quality assessment
The following data from eligible studies were extracted (Table 1): PubMed ID, first author, year, country, follow up duration, study design, outcome measures, cognitive impairment ascertainment method, total number of study participants, number of patients who received catheter ablation, ablation procedure details, number of patients treated with medical therapy and details about the type of medical therapy used. Hazard ratios from propensity matched groups were used where available.
Quality assessment was performed using the Newcastle Ottawa Scale for cohort studies and a modified version for case–control studies. Three broad domains were evaluated including the selection of study groups, the comparability of these groups and the ascertainment of the exposure or assessment of outcome. An adequate follow up period was defined as 1 year for long-term cognitive function, and key control factors included stroke followed by age, gender and smoking history.
2.4 Statistical analysis
Statistical analyses were performed using Review Manager version 5.4.1. The individual studies included in the meta-analysis used Cox proportional hazard regression models to determine hazard ratios. Where meta-analysis was performed, heterogeneity was assessed, and an I2 value ≥ 50% was considered significant. In this instance, a random-effects model was used to provide a more conservative estimate and because it is less influenced by the weighting of each study [12]. The inverse variance method based on a random-effects model was used to quantitatively summarise the outcome results and derive a pooled hazard ratio for dementia incidence in patients treated with catheter ablation versus medical therapy. A plan was made to assess for publication bias using visual inspection of funnel plot asymmetry if a minimum of 10 studies were included in the meta-analysis [13].
3 Results
3.1 Screening
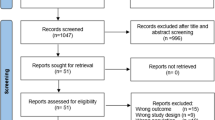
The search strategy yielded 599 studies after duplicate removal. Full-text screening was performed on 135 studies which identified 10 studies meeting the inclusion/exclusion criteria. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram is shown in Fig. 1.
3.2 Included studies
In the 10 included studies, 15,886 patients were treated with catheter ablation, and 42,684 patients were treated with medical therapy for atrial fibrillation. Detailed characteristics of the studies are provided in Table 1. Baseline characteristics of the study participants are detailed in supplementary Table S1.
3.3 Assessment of study quality
The 10 included studies comprised 6 cohort studies, 4 case–control studies and no randomised control trials. Newcastle–Ottawa Scale scores for the included studies are depicted in Table 2. The study scores ranged from 6/9–9/9. The cohort studies [14,15,16,17,18,19] presented suitable cohort comparability and outcome assessments, though often failed to demonstrate that the outcome of interest (dementia or impaired cognitive function) was not present at the start of the study. Jin et al. fulfilled all domains appropriately [20]. Medi et al. and Zhang et al. lacked the comparability of other studies due to their methods of recruiting consecutive patients awaiting catheter ablation [21, 22]. These studies were consequently unable to control for key control factors (stroke, age, gender and smoking history).
3.4 Cognitive function assessment
Numerous neuropsychological tests were utilised to assess cognitive function. These included mini mental state examination, Montreal cognitive assessment, Hasegwa dementia rating scale, national adult reading test, the visual analogue scale, the telephone interview for cognitive status-modified test and a well-established battery of 9 neuropsychological tests based on the Canadian Study of Health and Aging [23] (Table 1). Reliable change indices, as described by Chelune et al. [24] and Rasmussen et al. [25], were used to track changes in individuals’ test scores and assess for post ablation cognitive decline where reported.
3.5 New-onset dementia
Of the 10 studies included, 4 reported hazard ratios for dementia incidence [14,15,16,17] according to International Classification of Disease coding data. Due to the small number of included studies, we did not test for publication bias. The duration of follow-up varied amongst the studies (Table 1). These studies demonstrated an association between patients treated with catheter ablation therapy and a lower incidence of dementia. The 95% confidence intervals were available for 3 of these studies (Fig. 2). A pooled meta-analysis of these studies demonstrated a hazard ratio of 0.60 (95% confidence interval 0.42–0.88, p < 0.05 with an I2 value of 50%). Hyogo et al. found that new onset dementia occurred in 8 of 2113 (0.4%) atrial fibrillation patients [18]. In the 614 patients who had been treated with catheter ablation, 3 (0.5%) had developed dementia over the 1 year follow up period. A hazard ratio was not obtained (potentially due to the low event rate). For the studies reporting numbers of patients who developed dementia, these data are summarised in supplementary Table S2.
3.6 Dementia subtypes
Two studies reported incidence of dementia subtypes: Alzheimer’s disease and vascular dementia [15, 17]. Both studies reported that catheter ablation was associated with lower rates of Alzheimer’s disease compared with medical therapy. (Bunch et al. — hazard ratio 0.33, Kim et al. — hazard ratio 0.77). Kim et al. reported that catheter ablation was associated with a lower incidence of vascular dementia (hazard ratio 0.50 (95% confidence interval 0.33–0.74), p < 0.001). This contrasted to Bunch et al., who did not report a statistically significant difference (hazard ratio 0.74, (95% confidence interval not available), p = 0.37).
3.7 Changes in cognitive function > 3 months after catheter ablation or medical therapy
Tischer et al. performed cognitive function assessments on patients in 1 centre recruited from the Catheter Ablation Versus Anti-arrhythmic Drug Therapy for Atrial Fibrillation Trial (CABANA) and Catheter Ablation versus Standard Conventional Therapy in Patients with Left Ventricular Dysfunction and Atrial Fibrillation (CASTLE AF) trials [26]. In these trials, patients with atrial fibrillation were randomly assigned to receive either catheter ablation or medical therapy. The group enrolled patients 12 months after trial randomisation and performed 2 cognitive function assessments at 6-month intervals to assess the impact of the aforementioned interventions. The study found no statistically significant changes in mini mental state examination or Montreal cognitive assessment scores in patients treated with catheter ablation or medical therapy. On the contrary, Jin et al. found that Montreal cognitive assessment scores improved 1 year post radiofrequency catheter ablation in a group of patients treated with catheter ablation (score at baseline: 25.4 ± 2.4, score after 1 year: 26.5 ± 2.3; p < 0.001), but not in a propensity-matched control group (score at baseline: 25.4 ± 2.5, score after 1 year: 24.8 ± 2.5; p = 0.012) [20]. Wang et al. used the telephone interview for cognitive status–modified test to assess cognitive function and found that scores improved in the catheter ablation arm (score at baseline: 36.74 ± 3.097, score at 1 year 39.56 ± 3.198) but not in the medical therapy arm (score at baseline: 36.41 ± 3.033, score at 1 year 34.44 ± 3.271) [19].
3.8 Changes in cognitive function ≤ 3 months after catheter ablation or medical therapy
Three studies reported outcomes ≤ 3 months after catheter ablation [20,21,22]. Medi et al. and Zhang et al. tested cognitive function 48 h after ablation [21, 22]. In the study by Medi et al., patients had their procedure performed under general anaesthesia whereas the patients in the study by Zhang et al. had their procedure under conscious sedation. Medi et al. found that post ablation cognitive decline occurred in 17 of 60 patients with paroxysmal atrial fibrillation (28%; 95% confidence interval 18% to 41%), 8 of 30 patients with persistent atrial fibrillation (27%; 95% confidence interval 13% to 44%) and 0 of 30 control patients at 48 h (p = 0.007). Zhang et al. assessed for post ablation cognitive decline 48 h after ablation using 9 tests, based on the Canadian study of health and aging [23]. The authors found that post ablation cognitive decline occurred in 26 out of 190 patients (13.7%) treated with catheter ablation for atrial fibrillation.
Jin et al. and Medi et al. assessed cognitive function at 3 months. The study by Jin et al. found that baseline Montreal cognitive assessment score improved from 25.36 ± 2.39 to 26.57 ± 2.29 (p < 0.001) after 3 months in a propensity matched ablation group (n = 150). The control group’s Montreal cognitive assessment scores were 25.39 ± 2.53 at baseline and 25.24 ± 2.31 after 3 months (p > 0.05). Medi et al. found that post ablation cognitive decline at 90 days occurred in 8 of 60 patients paroxysmal atrial fibrillation patients treated with catheter ablation (13%; 95% confidence interval: 6 to 24%), 6 of 30 persistent atrial fibrillation patients treated with catheter ablation (20%; 95% confidence interval: 9 to 37%) and 0 of 30 control patients with atrial fibrillation (p < 0.03).
4 Discussion
The major findings from this study were (1) there is a significant lack of randomised control trial evidence to assess the impact of catheter ablation versus medical therapy on cognitive outcomes in atrial fibrillation; (2) the impact of catheter ablation on the rate of cognitive decline in patients with and without pre-existing cognitive impairment is currently unknown; (3) the data currently available may suggest that patients treated with catheter ablation may have a lower risk of developing dementia; (4) the data regarding cognitive function in the immediate post ablation period are inconsistent necessitating further study to ascertain the short to medium term effects of catheter ablation on cognitive function.
4.1 Risk of dementia in catheter ablation versus medical therapy
The studies which examined the incidence of dementia all found catheter ablation may be associated with a lower risk of developing dementia during follow-up compared with medical therapy [14,15,16,17]. The studies varied in their follow up durations with Hsieh et al., demonstrating that this pattern persisted in patients with a follow up period of 9.0 years. These findings were consistent across populations studied in 3 different countries. It is important to interpret these findings with caution. Whilst attempts to correct for underlying baseline differences were made through propensity matching, it is possible that unmeasured differences amongst the groups may have contributed to the findings. Patients referred for catheter ablation may have been less likely to develop dementia for reasons other than the treatment modality itself. We therefore cannot exclude the possibility of a selection bias favouring catheter ablation. The answer to the question of whether catheter ablation can prevent the onset of dementia in atrial fibrillation will come in the form of a randomised controlled trial.
4.2 The link between catheter ablation and cognitive decline
The mechanistic link between catheter ablation and cognitive decline remains to be elucidated. The resolution of cerebral hypoperfusion with sinus rhythm restoration through catheter ablation may prevent cognitive decline [27]. Interestingly, Jin et al. found that patients with sustained atrial fibrillation after catheter ablation had lower improvements in cognitive function at 1 year compared with patients who maintained sinus rhythm [20] suggesting that sinus rhythm maintenance may attenuate cognitive decline. A study by Piccini et al. performed in patients treated with catheter ablation for atrial fibrillation found that patients with recurrent atrial tachycardia and/or atrial fibrillation after ablation had similar improvements in Montreal cognitive assessment scores after 3 months compared with those who did not [28]. This study was performed in patients recruited from the AXAFA-AFNET 5 trial, a study comparing continuous apixaban therapy to vitamin K antagonist therapy during ablation [8]. Unfortunately, these studies do not precisely quantify atrial fibrillation burden throughout their follow up periods. Studies which attempt to correlate cognitive function with duration in sinus rhythm will need to be performed over longer time periods. This could potentially be done with implantable and/or wearable technologies to quantify atrial fibrillation burden.
If sinus rhythm-induced improvement in cerebral perfusion was indeed the mechanism by which catheter ablation halted neurocognitive decline, then one could speculate that any rhythm control therapy would result in improvements in cognitive function. However, studies which have compared rhythm control therapy to rate control have provided conflicting results [29,30,31]. One plausible explanation for this discrepancy may be the variable efficacy of anti-arrhythmic medications to restore and maintain sinus rhythm. The effects of anti-arrhythmic medications and chemical cardioversion on cerebral perfusion patterns are currently unclear presenting an area for further study.
Verification of the precise interaction between atrial fibrillation rhythm control strategies and cognitive decline may enable tailored treatment towards subtypes of dementia. Our study showed that catheter ablation might be associated with a lower risk of Alzheimer’s disease. Chronic cerebral hypoperfusion is thought to exacerbate amyloid-beta neuropathology, through the upregulation of amyloid-beta producing enzymes and lowering of amyloid-beta clearing proteins [32]. Catheter ablation-induced resolution of hypoperfusion could explain this association. Intriguingly, the risk of vascular dementia was not lessened to the same extent. This may result from the association between catheter ablation and subclinical cerebral emboli [5].
The association of catheter ablation with asymptomatic cerebral infarcts has led to speculation that the procedure may increase the risk of cognitive impairment. The clinical significance of post ablation infarcts is unclear at present [33]. Asymptomatic cerebral infarcts have been related to an increased risk of dementia in the general population [34]. Whether this is true for the cerebral emboli which result from catheter ablation is unclear. Further studies are warranted to examine the impact of post ablation asymptomatic cerebral infarcts on cognitive function in the longer term.
4.3 Changes in cognitive function > 3 months after ablation
Three studies performed repeated cognitive function assessments at intervals over specified time periods [19, 20, 26]. Tischer et al. recruited patients from the Catheter Ablation Versus Anti-arrhythmic Drug Therapy for Atrial Fibrillation Trial (CABANA) and Catheter Ablation versus Standard Conventional Therapy in Patients with Left Ventricular Dysfunction and Atrial Fibrillation (CASTLE AF) studies. Patients were assessed at least 12 months after randomisation to catheter ablation or medical therapy and cognitive tests performed at intervals of 6 months. The authors found no statistically significant changes in cognitive function. Jin et al. demonstrated that Montreal cognitive assessment scores improved 12 months after catheter ablation. These findings were corroborated by Wang et al., who found improvements in telephone interview for cognitive status-modified test scores at 12 months for patients treated with catheter ablation but not medical therapy. This discrepancy may be explained by the fact that patients recruited by Tischer et al. were older with a higher prevalence of pre-existing cognitive impairment compared with Wang et al. and Jin et al. Furthermore, cognitive decline is often a gradual process. The time periods between serial cognitive function testing differed amongst the studies and could have contributed to the differing results.
4.4 Cognitive function ≤ 3 months after ablation
The association between catheter ablation and subclinical cerebral emboli [5] has led to speculation that catheter ablation may worsen cognitive function. A notable finding from our study was that Jin et al. found that catheter ablation was associated with cognitive assessment score improvement after 3 months [20] whereas Medi et al. found a worsening of cognitive function at this time period [21]. The studies differed in the type of ablation catheter utilised, their method of anaesthesia and anticoagulation strategies. Differences in method of anaesthesia may also contribute to the difference in post ablation cognitive decline incidence at 2 days in the studies by Zhang et al. and Medi et al. [21, 22]. A lower proportion of patients in the study by Zhang et al. had their ablation under general anaesthesia compared with Medi et al. It is becomingly increasingly recognised that the procedural protocols and ablation tools used have an influence on the prevalence of silent cerebral infarcts [5]. Study heterogeneity is therefore likely to have contributed significantly to the differences in these results.
4.5 Limitations
The main limitation of our study was the lack of randomised control trial level evidence. This makes it difficult to make firm conclusions based on the data currently available. Questions pertaining to the impact of catheter ablation on cognitive function in patients with pre-existing cognitive impairment, risk of dementia and short- to medium-term cognitive function remain unanswered based on the evidence reviewed in this study. The lack of such data stresses the requirement for further study to investigate the impact of atrial fibrillation treatment modalities on cognitive function.
Selection bias may have contributed to the findings of this review. For example, variations in age, sex and cardiovascular comorbidities between groups treated with either medical therapy or catheter ablation in the available literature may have contributed to differences in cognitive outcomes between groups. Most of the studies identified were observational in nature. Whilst 7 of the 10 studies attempted to match for confounders, unaccounted-for confounders could have explained some of the results observed. Additionally, various assessments of cognition were used. Some studies used an International Classification of Disease diagnosis of dementia as an endpoint whereas others used cognitive function assessments. Given the heterogeneity of these cognitive assessment methods, it is possible that the type of assessment used may have influenced the results observed. Most of the outcomes discussed in this review are therefore reported descriptively. This limitation reflects the limitations inherent in the available published data, again highlighting the need for further mechanistic research in this area.
The medical management and types of anticoagulation strategies utilised also differed likely resulting in variability amongst the studies. The same can be said of the ablation procedures used. Many of the studies included in the systematic review failed to provide details about the medical management and/or catheter ablation strategies employed (Table 1). This is likely to have affected the results obtained and importantly precludes meaningful assessment of the influence of procedural characteristics and choice of ablation technology on cognitive outcomes. Furthermore, baseline cranial imaging was not performed in the studies included. We cannot exclude the possibility of pre-existing abnormalities affecting the results of the studies.
4.6 Future directions
To mitigate the risk of selection bias, randomised trials are required to compare the effects of atrial fibrillation treatment strategies on cognition. The Cognitive Impairment in Atrial Fibrillation study (DIAL-F, ClinicalTrials.gov Identifier: NCT01816308) will compare catheter ablation against antiarrhythmic drug therapy. Future trials to assess the impact of other modalities such as electrical cardioversion and rate control would also be useful. Catheter ablation itself is also heterogeneous, and it is therefore feasible that different catheter ablation techniques will have differing effects on cognition presenting another important area for future study.
Studies should also be designed to investigate the mechanisms through which atrial fibrillation treatment strategies may affect cognition. The Neurocognition and Greater Maintenance of Sinus Rhythm in Atrial Fibrillation (NOGGIN AF, project number 1R01AG074185-01) trial will compare cognitive function in patients treated with catheter ablation versus medical therapy. This study will compare structural cortical characteristics and cerebral perfusion patterns providing important information about how such treatment strategies could differentially affect cerebral structure and function. Additionally, it would be useful to ascertain whether there is a relationship between atrial fibrillation treatment and levels of biomarkers indicative of cognitive impairment in plasma and cerebrospinal fluid.
Studies should also be designed to identify whether catheter ablation–induced changes in other parameters such as cardiac function and/or symptom burden correlate with changes in cognitive function. This could enable a greater understanding of the mechanistic link between atrial fibrillation and cognitive decline. It would also be useful to examine whether a patient’s atrial fibrillation classification influences the risk of cognitive decline with medical or interventional therapy. This information could be used to identify the patient groups most likely to benefit from atrial fibrillation treatment strategies aimed at halting cognitive decline.
5 Conclusion
The link between atrial fibrillation and dementia is increasingly reported. Treatment strategies should be aimed at minimising the cognitive decline process observed in patients with atrial fibrillation. Given the limitations of the available data, we are unable to make firm conclusions; however, this study suggests that catheter ablation may offer promise to prevent neurocognitive decline in atrial fibrillation. Further studies are therefore warranted to elucidate the mechanistic link between atrial fibrillation and cognitive decline, delineate the true impact of catheter ablation versus medical therapy on cognitive function, and to strive to identify the patient groups most likely to benefit from treatment aimed at halting cognitive decline.
References
Stewart S, Hart CL, Hole DJ, McMurray JJV. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113(5):359–64. https://doi.org/10.1016/S0002-9343(02)01236-6.
Ahmadi-Abhari S, et al. Temporal trend in dementia incidence since 2002 and projections for prevalence in England and Wales to 2040: modelling study. BMJ. 2017;358. https://doi.org/10.1136/bmj.j2856.
Kandimalla R, et al. Association between atrial fibrillation and dementia: a meta-analysis. Anal Front Aging Neurosci. 2019;11:305. https://doi.org/10.3389/fnagi.2019.00305.
Wilber DJ, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010;303(4):333–40. https://doi.org/10.1001/jama.2009.2029.
Gaita F, et al. Radiofrequency catheter ablation of atrial fibrillation: a cause of silent thromboembolism? Magnetic resonance imaging assessment of cerebral thromboembolism in patients undergoing ablation of atrial fibrillation. Circulation. 2010;122(17):1667–73. https://doi.org/10.1161/CIRCULATIONAHA.110.937953.
Schwarz N, et al. Neuropsychological decline after catheter ablation of atrial fibrillation. Hear Rhythm. 2010;7(12):1761–7. https://doi.org/10.1016/j.hrthm.2010.07.035.
Kochhäuser S, et al. Neuropsychological impact of cerebral microemboli in ablation of atrial fibrillation. Clin Res Cardiol. 2015;104(3):234–40. https://doi.org/10.1007/s00392-014-0777-0.
Kirchhof P, et al. Apixaban in patients at risk of stroke undergoing atrial fibrillation ablation. Eur Heart J. 2018;39(32):2942–55. https://doi.org/10.1093/eurheartj/ehy176.
Kato N, et al. Brain magnetic resonance imaging and cognitive alterations after ablation in patients with atrial fibrillation. Sci Rep. 2021;11(1):18995. https://doi.org/10.1038/s41598-021-98484-w.
Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:1–11. https://doi.org/10.1016/j.ijsu.2021.105906.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1). https://doi.org/10.1186/s13643-016-0384-4.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Cochrane Handbook for Systematic Reviews of Interventions | Cochrane Training. https://training.cochrane.org/handbook/current. Accessed 7 Feb 2022.
Hsieh YC, et al. Catheter ablation of atrial fibrillation reduces the risk of dementia and hospitalization during a very long-term follow-up. Int J Cardiol. 2020;304:75–81. https://doi.org/10.1016/j.ijcard.2019.12.016.
Kim D, et al. Less dementia after catheter ablation for atrial fibrillation: a nationwide cohort study. Eur Heart J. 2020;41(47):4483–93. https://doi.org/10.1093/eurheartj/ehaa726.
Bunch TJ, et al. Stroke and dementia risk in patients with and without atrial fibrillation and carotid arterial disease. Heart Rhythm. 2020;17(1):20–6. https://doi.org/10.1016/j.hrthm.2019.07.007.
Bunch TJ, et al. Patients treated with catheter ablation for atrial fibrillation have long-term rates of death, stroke, and dementia similar to patients without atrial fibrillation. J Cardiovasc Electrophysiol. 2011;22(8):839–45. https://doi.org/10.1111/j.1540-8167.2011.02035.x.
Hyogo K, et al. One-year clinical outcomes of anticoagulation therapy among Japanese patients with atrial fibrillation: The Hyogo AF Network (HAF-NET) Registry. J Arrhythmia. 2019;35(5):697–708. https://doi.org/10.1002/joa3.12226.
Wang X, Wang Z, Yan X, Huang M, Wu Y. Radiofrequency and cryoballoon ablation improve cognitive function in patients with atrial fibrillation. Medicine (Baltimore). 2021;100(32):e26914–e26914. https://doi.org/10.1097/MD.0000000000026914.
Jin MN, et al. Atrial fibrillation catheter ablation improves 1-year follow-up cognitive function, especially in patients with impaired cognitive function. Circ: Arrhythm Electrophysiol. 2019;12(7). https://doi.org/10.1161/CIRCEP.119.007197.
Medi C, et al. Subtle post-procedural cognitive dysfunction after atrial fibrillation ablation. J Am Coll Cardiol. 2013;62(6):531–9. https://doi.org/10.1016/j.jacc.2013.03.073.
Zhang J, et al. Incidence and risk factors of post-operative cognitive decline after ablation for atrial fibrillation. BMC Cardiovasc Disord. 2021;21(1):341. https://doi.org/10.1186/s12872-021-02139-7.
Canadian study of health and aging: study methods and prevalence of dementia. C Can Med Assoc J = J l’Association medicale Can. 1994;150( 6):899–913.
Chelune GJ, Naugle RI, Lüders H, Sedlak J, Awad IA. Individual change after epilepsy surgery: practice effects and base-rate information. Neuropsychology. 1993;7(1):41–52. https://doi.org/10.1037/0894-4105.7.1.41.
Rasmussen LS, Larsen K, Houx P, Skovgaard LT, Hanning CD, Moller JT. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand. 2001;45(3):275–89. https://doi.org/10.1034/j.1399-6576.2001.045003275.x.
Tischer TS, et al. Prevalence and progression of cognitive impairment in atrial fibrillation patients after treatment with catheter ablation or drug therapy. Cardiol Res Pract. 2019;2019:4–7. https://doi.org/10.1155/2019/7216598.
Kanmanthareddy A, et al. The impact of atrial fibrillation and its treatment on dementia. Curr Cardiol Rep. 2014;16(8). Current Medicine Group LLC 1. https://doi.org/10.1007/s11886-014-0519-y.
Piccini JP, et al. Changes in quality of life, cognition and functional status following catheter ablation of atrial fibrillation. Heart. 2020;106(24):1919–26. https://doi.org/10.1136/heartjnl-2020-316612.
Chung MK, et al. Functional status in rate- versus rhythm-control strategies for atrial fibrillation: Results of the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) functional status substudy. J Am Coll Cardiol. 2005;46(10):1891–9. https://doi.org/10.1016/j.jacc.2005.07.040.
Damanti S, Pasina L, Cortesi L, Rossi PD, Cesari M. Atrial fibrillation: possible influences of rate and rhythm control strategy on cognitive performance. J Am Geriatr Soc. 2018;66(11):2178–82. https://doi.org/10.1111/jgs.15568.
Kirchhof P, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med. 2020;383(14):1305–16. https://doi.org/10.1056/nejmoa2019422.
Ihara M, Washida K. Linking atrial fibrillation with Alzheimer’s disease: epidemiological, pathological, and mechanistic evidence. J Alzheimer’s Dis. 2018;62(1):61–72. IOS Press. https://doi.org/10.3233/JAD-170970.
Deneke T, et al. Silent cerebral events/lesions related to atrial fibrillation ablation: a clinical review. J Cardiovasc Electrophysiol. 2015;26(4):455–63. https://doi.org/10.1111/jce.12608.
Sigurdsson S, et al. Incidence of brain infarcts, cognitive change, and risk of dementia in the general population: the AGES-Reykjavik Study (Age Gene/Environment Susceptibility-Reykjavik Study). Stroke. 2017;48(9):2353–60. https://doi.org/10.1161/STROKEAHA.117.017357.
Funding
This research was supported by the British Heart Foundation (PG/19/44/34368), the British Heart Foundation Centre for Research Excellence at the University of Edinburgh (RE/18/5/34216) and by core funding from the Wellcome/ESPRC Centre for Medical Engineering at King’s College London (WT203148/Z/16/Z). Dr Williams is supported by the British Heart Foundation (FS/20/26/34952).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This is a systematic review of the literature. No ethical approval was required.
Informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bodagh, N., Yap, R., Kotadia, I. et al. Impact of catheter ablation versus medical therapy on cognitive function in atrial fibrillation: a systematic review. J Interv Card Electrophysiol 65, 271–286 (2022). https://doi.org/10.1007/s10840-022-01196-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01196-y