Abstract
Alzheimer’s disease (AD) is prevalent throughout the world and is the leading cause of dementia in older individuals (aged ≥ 65 years). To gain a deeper understanding of the recent literature on the epidemiology of AD and its progression, we conducted a review of the PubMed-indexed literature (2014–2021) in North America, Europe, and Asia. The worldwide toll of AD is evidenced by rising prevalence, incidence, and mortality due to AD—estimates which are low because of underdiagnosis of AD. Mild cognitive impairment (MCI) due to AD can ultimately progress to AD dementia; estimates of AD dementia etiology among patients with MCI range from 40% to 75% depending on the populations studied and whether the MCI diagnosis was made clinically or in combination with biomarkers. The risk of AD dementia increases with progression from normal cognition with no amyloid-beta (Aβ) accumulation to early neurodegeneration and subsequently to MCI. For patients with Aβ accumulation and neurodegeneration, lifetime risk of AD dementia has been estimated to be 41.9% among women and 33.6% among men. Data on progression from preclinical AD to MCI are sparse, but an analysis of progression across the three preclinical National Institute on Aging and Alzheimer’s Association (NIA-AA) stages suggests that NIA-AA stage 3 (subtle cognitive decline with AD biomarker positivity) could be useful in combination with other tools for treatment decision-making. Factors shown to increase risk include lower Mini-Mental State Examination (MMSE) score, higher Alzheimer’s Disease Assessment Scale (ADAS-cog) score, positive APOE4 status, white matter hyperintensities volume, entorhinal cortex atrophy, cerebrospinal fluid (CSF) total tau, CSF neurogranin levels, dependency in instrumental activities of daily living (IADL), and being female. Results suggest that use of biomarkers alongside neurocognitive tests will become an important part of clinical practice as new disease-modifying therapies are introduced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Alzheimer’s disease (AD) dementia incidence and prevalence are high worldwide, increasing but likely underestimated because of underdiagnosis and misdiagnosis. |
The risk of dementia increases with stages of progression, from normal cognition with no amyloid-beta (Aβ) accumulation to degeneration and subsequently to mild cognitive impairment (MCI) due to AD. |
Studies of AD are challenged by disease classification due to differential diagnosis, multiple biomarkers and neuropsychiatric tests, and variation in consensus criteria. |
Measures to help determine AD dementia risk among people with MCI include neurocognitive test performance and biomarkers (e.g., tau/Aβ ratio, positive APOE4 status, white matter hyperintensities, atrophy in specific brain regions). |
With new therapies, clinicians must be able to identify patients with preclinical AD and MCI due to AD using combinations of diagnostic approaches. |
Introduction
Alzheimer’s disease (AD) is the leading cause of cognitive impairment and dementia in older individuals (aged ≥ 65 years) throughout the world [1]. AD follows a prolonged, progressive disease course that begins with pathophysiological changes in the brains of affected individuals years before any clinical manifestations are observed [2]. These pathophysiological changes include the accumulation of toxic species of amyloid-β (Aβ), the development of neurofibrillary tangles of hyperphosphorylated tau protein, and neurodegeneration that may result from uncontrolled activation of microglia in the brain leading to secretion of neurotoxins and inflammatory factors [3,4,5]. Individuals harboring such changes may be asymptomatic or may exhibit clinical manifestations varying from memory lapses to severe and debilitating loss of memory and cognitive function [2]. As AD progresses, additional neuropsychiatric symptoms may manifest, including periods of confusion, disorientation, mood change, aggression/agitation, and eventually delusion/hallucination in later stages.
Because normal aging involves subtle cognitive deterioration, it can often be difficult to distinguish cognitive decline due to AD from the declines associated with normal aging (e.g., declines in processing speed, and certain abilities related to memory, language, visuospatial, and executive function) [6, 7]. As a result of the challenges of diagnosis and of a historical perceived lack of benefit from diagnosis (due to the lack of an effective disease-modifying therapy, DMT), underdiagnosis is common, with some evidence suggesting that more than half of those who develop AD dementia may never be formally diagnosed [8,9,10]. However, because a novel DMT may be most effective before years of potentially irreversible pathologic changes have occurred, identifying individuals destined to develop AD dementia is vital [11]. The 2011 National Institute on Aging and Alzheimer’s Association (NIA-AA) guidelines defined three phases of AD: preclinical AD (early pathologic changes in the brains of cognitively normal individuals), MCI (symptomatic predementia), and dementia [12,13,14].
Preclinical AD, the earliest phase of the continuum from normal cognition to AD dementia, is characterized by the occurrence of the aforementioned pathophysiological changes including accumulation of toxic Aβ species and hyperphosphorylated tau protein [2, 5, 15]. Importantly, toxic Aβ species and hyperphosphorylated tau can be identified in cerebrospinal fluid (CSF) and blood and can therefore be employed as diagnostic biomarkers [16, 17]. Definitions for preclinical AD have been proposed by four different groups (NIA-AA criteria, Dubois criteria, International Working Group-2 criteria, and the NIA-AA Research Framework criteria) and based on various combinations of biomarkers [18]. There is some correspondence among categories in the four systems [18].
MCI identifies individuals who do not have dementia, but who do have some deficits in cognition. The definition of MCI has evolved over the past 50 years, and there are several clinical definitions [11, 19]. The Peterson criteria define MCI as individuals performing 1.5 standard deviations below normal on memory tasks, with preservation of activities of daily living (ADL) [19]. The Winblad criteria expand the definition to include and distinguish individuals with cognitive impairment in domains beyond memory impairment, resulting in amnestic MCI (aMCI; subjective and objective memory impairment) and non-amnestic MCI (naMCI; impairment in a cognitive domain other than memory) [11, 19, 20]. In addition, the range of cognitive deficit is further categorized as single-domain (sd) or multiple-domain (md) aMCI and naMCI [11, 19, 20]. However, clinical definitions of MCI that do not include neuropathologic changes in the brain as a criterion for diagnosis lack specificity for AD as the underlying cause of impaired cognition [15, 21].
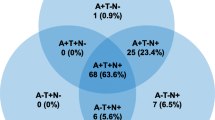
In 2018, the NIA-AA published a research framework that developed a biological rather than clinical definition of AD for use in clinical research [15]. The NIA framework defined AD on the basis of the AT(N) classification, which assessed the presence of amyloid pathology (A), tau pathology (T), and neuronal injury (N) to categorize the presence and extent of AD [15]. In the framework, the presence of amyloid pathology was indicative of AD pathologic change and amyloid pathology in combination with tau pathology and/or neuronal injury was indicative of AD [15]. In response, an International Working Group provided recommendations for a clinical-biological diagnosis of AD that incorporated both clinical (e.g., impaired cognition) and biomarker (amyloid and tau pathology) evidence to support a diagnosis. However, the International Working Group recommended against widespread biomarker testing of cognitively unimpaired individuals [21].
As new DMTs are introduced into practice, it is useful to understand what is currently known about the clinical burden of AD across the spectrum of the disease. To gain a deeper understanding of the clinical burden of AD in terms of prevalence, incidence, mortality, and progression (including preclinical AD and that of MCI due to AD), we reviewed the epidemiologic and clinical literature on AD with a focus on recent English-language literature published in North America, Europe, and Asia.
Methods
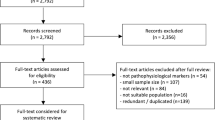
A review of the recent literature on the epidemiology and clinical burden of AD in North America, Europe, and Asia was conducted. Our primary literature search covered the PubMed-indexed literature published between 2014 and January 2021 and included search terms related to AD (including MCI) and epidemiology (e.g., “incidence”, “prevalence”, “epidemiology”, “risk factors”) or clinical burden (e.g., “morality”, “progression”, “stages”) as well as relevant Medical Subject Heading (MeSH) terms for AD epidemiology and clinical burden. Supplemental searches of indexed and non-indexed literature were also conducted. The year 2014 was selected as a cutoff date in an effort to focus our review on studies published after the publication of the 2011 NIA-AA; additionally, we did not want to look further back than 2014 for studies of epidemiologic data as such data may be outdated.
While this research is not based on a systematic literature review, articles identified in the literature search were considered for inclusion if they reported relevant outcomes and were conducted globally or in the United States (USA), France, Germany, Italy, Spain, the United Kingdom (UK), China, and Japan. Articles reporting on patients with AD were prioritized, whereas articles reporting on related populations (e.g., patients with dementia, AD and related dementia [ADRD], or AD and other dementia [ADOD]) were not prioritized unless they reported specific information on patients with AD. Where many articles on a specific topic were identified, those publishing unique information were prioritized for inclusion. Additional priorities included more recently published articles and, where relevant, studies of larger patient populations and studies reporting on longer periods of follow-up. In total, 53 articles were selected for inclusion in the literature review. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Epidemiology of AD and MCI
Prevalence of Clinical AD Dementia
The prevalence of clinically diagnosed AD dementia is high and expected to rise over time consistent with the aging of the population [8, 22, 23]. According to a range of estimates from different studies (Table 1), AD dementia affects 3–4% of adults in their late working or retirement years [24,25,26,27,28]. These estimates may reflect regional differences or differences in study design (e.g., varying ages of study populations, diagnostic criteria for AD dementia) [24, 26].
The prevalence of clinically diagnosed AD dementia rises with increasing age [25, 26]. In China, 2010 estimates of prevalence from a systematic review increased with advancing age from 0.2% among persons aged 55–59 to 48.2% among persons aged 95–99 [29]. AD dementia is also more common among women than among men, as evidenced by a systematic review in which all five studies that included prevalence in men and women reported a higher prevalence in women, and by a meta-analysis that found AD affected 3.31% (95% confidence interval [CI] 2.85, 3.80) of men and 7.13% (95% CI 6.56, 7.72) of women [25]. A separate study conducted in China similarly found that women were more than twice as likely to have AD dementia than men (prevalence ratio, 2.37, 95% CI 1.90, 2.96, p < 0.0001) after adjustment for age, period of study, and region (urban or rural) [29].
Incidence of Clinical AD
The incidence of clinically diagnosed AD dementia reported in studies (Table 2) varies from 2.0 to 16.8 new cases of AD per 1000 person-years across studies in the USA, Europe, Japan, and China [23,24,25,26, 29, 30]. Some of the wide variation in incidence may be due to variations in age ranges of included study populations, country population characteristics, time periods studied, and operational diagnosis of AD dementia. For example, a meta-analysis investigating the incidence of clinical AD in Europe found that incidence rose with increasing age strata (cases of clinical AD per 1000 person-years: 65–74 years, 3.4; 75–84 years, 13.8; ≥ 85 years, 35.8) [25]. As with prevalence, the incidence of AD dementia rises with age: a recent systematic review found that seven of nine studies reported a positive association with age [26]. A meta-analysis of studies conducted in Europe also observed a higher incidence of AD dementia in women than in men (women, 13.3 cases per 1000 person-years [95% CI 12.1, 14.5]; men, 7.02 cases per 1000 person-years [95% CI 6.1, 8.1]), although study authors did not report on the relationship between patient age and sex [25].
Mortality
Globally, dementia (all-cause) is the fifth leading cause of death, with 4.4% of all deaths attributable to dementia in 2016 [31]. Deaths due to dementia have steadily increased over time, partly due to population growth and population aging, more than doubling from 1990 to 2016 [31]. AD dementia-related deaths have also risen. An analysis of AD dementia mortality in Europe found that deaths from AD among patients aged ≥ 50 years (as identified by diagnostic codes) more than doubled from 1994 [41,255 deaths] to 2013 [86,822 deaths] [32]. The age-standardized mortality rate for deaths caused by AD dementia in Europe was 45.2 per 100,000 in 2013 [32].
Recording of cause of death is variable and AD dementia may be either a contributing cause or an underlying cause [33, 34]. In the USA in 2017, 46.4% of dementia-related deaths were attributable to AD [34]. One study of AD dementia in Canada investigated multiple causes of death when AD was listed on death certificates [33]. In this analysis, 4.3% of all deaths occurring from 2004 to 2011 were AD dementia-related, but 2.6% of deaths had AD dementia as an underlying cause, in contrast to 1.7% of deaths having AD dementia as a contributing cause [33]. Usually, when AD dementia was listed as an underlying cause, cardiovascular disease was the most common contributing cause (46%); when AD dementia was listed as a contributing cause, cardiovascular disease was the most common underlying cause (41%) [33]. The crude mortality rate in Canada for deaths from AD dementia as an underlying cause increased over the period 2004 to 2011, from 10.1 to 11.5 per 100,000 for men and from 24.4 to 25.4 per 100,000 for women [33].
Data on survival from early stages of AD dementia are scarce. However, median survival among persons with AD dementia has been estimated to be approximately 7 years from presentation with cognitive decline (according to an analysis of data from one geographic area in England) [35].
MCI due to AD
Patients with MCI due to AD are more likely to progress to dementia than those with MCI that is not associated with toxic species of Aβ and/or the development of neurofibrillary tangles of hyperphosphorylated tau protein [5, 15, 21, 36,37,38]. Data from 13 cohort studies representative of multiple countries has demonstrated a high prevalence of AD at the MCI stage according to the IWG-1, IWG-2, and NIA-AA criteria, which identifies patients at higher risk of dementia based on the presence of AD-related biomarkers (abnormal Aβ and/or tau) and or neuronal injury [38]. On the basis of the IWG criteria, 53% (IWG-1) and 40% (IWG-2) of subjects with MCI were identified as having AD; 3-year progression rates were 50% (IWG-1 criteria) in persons with prodromal AD versus 21% without prodromal AD, and 61% (IWG-2) with prodromal AD versus 22% without prodromal AD. On the basis of NIA-AA criteria, 46% of subjects with MCI were classified as being in the “high likelihood AD” group [38]; and the 3-year progression rate was 59% (subjects in lower risk groups had 3-year progression rates of 5–24%).
The incidence of clinically diagnosed MCI has been examined in a systematic review of studies in Europe, the Americas, and Australia [39]. Incidence rates ranged from 22.5 to 60.1 per 1000 person-years depending on age, but meta-analysis suggests substantial heterogeneity in incidence estimates due to methodological and population sample characteristics in the included studies. Analyses resulted in MCI incidence of 22.5 (95% CI 5.1, 51.4) per 1000 person-years for ages 75–79, 40.9 (95% CI 7.7, 97.5) for ages 80–84, and 60.1 (95% CI 6.7, 159.0) for ages 85 and older [39]. Other research has examined etiologic diagnoses of AD in MCI (as evidenced by NIA-AA clinical criteria), finding that 75% of subjects with MCI had an etiology of AD, while the remainder were classified with etiologies such as CVD and Lewy body dementia [40].
Several recent studies in China have documented population-based prevalence of clinically diagnosed MCI [37, 41, 42]. In a meta-analysis of 41 studies of Chinese community-dwelling populations over 55 years of age, the pooled prevalence of MCI was 12.2% (95% CI 10.6, 14.2) for MCI and 10.9% (95% CI 7.7, 15.4) for amnestic MCI. There were slight differences in prevalence according to diagnostic criteria, with rates of MCI of 13.5% using the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria, 12.9% using the Petersen criteria, and 10.3% using NIA-AA [42]. There was a higher prevalence among women than men (13.8% [95% CI 9.7, 13.6] vs. 11.5% [95% CI 11.7, 16.3]), and people living alone versus in families (18.2% [95% CI 13.6, 24.4] vs. 14.1% [95% CI 11.0, 18.2]); those that had education levels lower than primary school had much higher prevalence of MCI (17.2% [95% CI 12.2, 24.3]) when compared to persons with higher levels of education. Studies in this meta-analysis based on more recent observation periods resulted in higher prevalence estimates (before 2005, 3.7% [95% CI 1.6, 8.7]; in 2005 or later, 14.1 [95% CI 12.4, 16.0]) [42]. One study of a rural area in Northern China in 2015 reported prevalence of MCI and AD, finding rates of 27.8% (overall MCI), 18.4% (MCI due to AD), and 6.5% (AD) [41]. Another national cross-sectional study of adults over the age of 60 in China reported age- and sex-adjusted overall MCI prevalence of 15.5% (95% CI 15.2, 15.9) [37].
Preclinical Stages of AD
AD dementia develops by progression through several stages, from no accumulation of toxic Aβ species to normal cognition with Aβ deposition and then neurodegeneration (as evidenced by elevated CSF tau protein and fluorodeoxyglucose (FDG) positron electron tomography (PET) imaging), and subsequently to MCI. According to a multistate disease model, the lifetime risk of AD for a 60-year-old person with normal cognition and no toxic Aβ accumulation has been estimated to be 20.1% (range 10.6–34.0%) among women and 13.9% (range 6.9–25.1%) among men [43]. For patients with Aβ deposition and neurodegeneration, estimates of lifetime risk are 41.9% among women and 33.6% among men, and for patients with MCI, lifetime risk is more than twice that of the earlier stage. By contrast, a much higher percentage of patients with MCI due to AD were estimated to progress to dementia (men 92.9%; women 95.6%).
Prevalence estimates studied in a systematic literature review that measured amyloid PET or CSF in subjects with normal pathology showed rates of 22% (CI 18–27%) and 21% (CI 15–29%) for PET and CSF, respectively; however, prevalence rates across the studies including biomarker data ranged widely (7–48% for PET studies, and 4–52% for CSF studies) [44]. Nevertheless, results suggest that measuring biomarkers is an important component of identifying risk of progression from preclinical AD to MCI and ultimately to AD dementia. In the same systematic literature review, an analysis of the studies that provided data across NIA-AA preclinical stages resulted in prevalence estimates of 13% (CI 9–18%), 16% (CI 9–25%), and 5% (CI 3–9%) for stages 1, 2, and 3, respectively.
Other research using the NIA-AA criteria has estimated the prevalence of preclinical and clinical AD by stage [36]. Rates were calculated on the basis of a multistate Markov model with data on incidence from longitudinal studies, as well as mortality rates and population projections. Most cases with AD pathology (i.e., Aβ deposition, CSF tau, and neurodegeneration based on FDG-PET imaging) were preclinical, with rates from this model declining from early to later stages of AD owing primarily to attrition from death (from age, other conditions, or dementia). Projected 2060 prevalence estimates increased across all stages from 2015, more than doubling for each of the later stages: MCI due to AD (2.4 million in 2017; 5.7 million in 2060), early-stage AD dementia (2.1 million in 2017; 5.3 million in 2060), and late-stage AD dementia (1.5 million in 2017; 4.0 million in 2060). Prevalence estimates for preclinical AD also increased in patients with Aβ deposition only (22.1 million in 2017; 31.9 million in 2060) and in those with Aβ deposition and neurodegeneration (16.2 million in 2017; 30.2 million in 2060).
This multistate model was also used to assess the impact of hypothetical disease-modifying health interventions on forecasts. In one scenario, an intervention delaying the annual risk of progression to MCI by 50% resulted in a decrease in the prevalence of MCI (from 5.70 million to 5.01 million) as well as a decrease in the prevalence of AD dementia (from 9.3 million to 6.95 million) [36].
Disease Progression
Progressive deterioration of cognitive function in persons with AD varies according to the affected elements of cognition. In an analysis of data from 1495 adults with clinically diagnosed AD dementia from the Geriatric Education and Research in Aging Sciences (GERAS) study, deterioration on both the Mini Mental State Exam (MMSE) and the Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-cog) showed a similar pattern of progressive decline in which word recall and orientation were affected first, with declines in attention and concentration, language, constructional praxis, and executive function occurring next, and immediate memory deteriorating in severe AD dementia [45]. A systematic literature review of studies examining acceleration points in cognitive decline showed that verbal memory deficits appeared first, followed by deficits in visuospatial ability, executive functions, fluency, and verbal IQ [46].
Data on the risk of progression from preclinical AD to MCI are sparse, but a systematic literature review and meta-analysis (2011–2018) included studies that provided progression data across the three preclinical NIA-AA stages [44]. Rates of progression increased across stages: 73% (95% CI 40–92%) at the preclinical AD stage 3 (subtle cognitive decline with AD biomarker positivity), 38% (95% CI 21–59%) at stage 2 (toxic Aβ accumulation and neurodegeneration), and 20% (95% CI 10–34%) at stage 1 (toxic Aβ accumulation but asymptomatic) [44]. The relative risk of progression increased across stage and was over six times higher at stage 3 (RR = 6.38; 95% CI 3.33–12.24) compared to individuals with normal biomarkers [44]. Authors suggested that on the basis of these data, NIA-AA stage 3 should be used along with MCI due to AD in treatment decision-making [44].
Data from studies of progression from clinically diagnosed MCI to AD dementia have shown that the majority of patients with MCI either remain cognitively stable or revert to normal values, versus progressing to AD [11, 20, 47, 48]. However, comparing results across studies can be challenging because of inconsistent study designs, differing clinical definitions of MCI, and differences in patient populations [20]. For example, in a meta-analysis of 28 studies (through 2014) including 2365 patients with MCI, 38.7% progressed to AD dementia over a mean follow-up of 31 months; however, progression rates in the individual studies varied from 6% to 39% per year.
One factor that has implications for estimating progression rates is the subtype of MCI. A meta-analysis of 33 studies (1999–2017) of 4907 patients with clinically diagnosed MCI showed that approximately half of patients with sd-aMCI or md-aMCI progressed (sd-aMCI odds of progression to AD, 0.47; 95% CI 0.33, 0.66; p < 0.001; md-aMCI odds of progression to AD dementia, 0.52; 95% CI 0.36, 0.75; p < 0.001), but that risk of progression was substantially lower for patients with naMCI (sd-naMCI odds of progression to AD dementia, 0.11; 95% CI 0.07, 0.16; p < 0.001; md-naMCI odds of progression to AD dementia, 0.18; 95% CI 0.11, 0.27; p < 0.001) [20]. This was also illustrated in the prospective Australian Imaging, Biomarkers and Lifestyle (AIBL) study in which patients (n = 866) were classified by subtype of clinically diagnosed MCI and then also by the severity of their memory impairment [11]. After 3 years, patients with aMCI were more likely than the healthy controls to develop AD dementia (positive predictive value [PPV] 24.1%; 95% CI 18.4, 30.6), and risk increased with the severity of memory impairment (grade 1 PPV = 10.0%; 95% CI 5.1, 17.2; grade 2 PPV = 43.0%; 95% CI 32.8, 53.7) [11]. Patients with md-aMCI had a higher risk of progression vs. sd-aMCI (PPV of 47.3%; 95% CI 33.7, 61.2 vs. PPV of 15.5%; 95% CI 10.1, 22.4), and risk also increased with increasing severity of memory loss [11]. The annual progression rates were 8.0% for aMCI, 5.2% for sd-aMCI, and 15.8% for md-aMCI [11]. Other studies have reported rates of progression from clinically diagnosed MCI to AD dementia varying from 18.3% (9 of 51 people) to 48.3% (86 of 178 people) within 2 years [49, 50]. A larger study found that 33.3% (181 of 544 patients) progressed from clinically diagnosed MCI to AD dementia within a median of 46 months [51].
The progression rates reported in studies can also be influenced by the source of recruitment of patients: the aforementioned meta-analysis of 33 studies also classified patients as community-dwelling or from specialist clinics and showed that rates of progression were higher for patients from specialist clinics vs. community samples (sd-aMCI, 40% vs. 18%; md-aMCI, 35% vs. 21%) [20]. This concept was also demonstrated in a systematic literature review and meta-analysis of 59 studies (1999–2016) [52]. The overall progression rate (timeframe not reported) from clinically diagnosed MCI (subtype not stated) to AD dementia (adjusted for prevalence and weighted by follow-up time) was 28% (95% CI 22, 33) and to dementia was 34% (95% CI 27, 40), with 45% (95% CI 34, 55) remaining stable and 15% (95% CI 10, 19) improving their status to normal [52]. When the data were grouped according to community vs. specialist clinic patients, progression to AD was higher in the clinic sample compared to the community sample (31% vs. 13%), which may be due differences between clinic and community populations [52].
Another confounding factor is that a sizable percentage of healthy elderly adults score below normal on at least one cognitive test when given a battery of tests [47]. In order to resolve this issue, some researchers used the concept of “base rate of low scores” (BRLS) to classify patients from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database [47]. According to this approach, a person was deemed to have MCI if their number of low scores on a panel of cognitive tests was greater than or equal to the number of the 10% of worst-performing patients [47]. According to these criteria, 34% of patients defined as MCI progressed to AD dementia, compared to 22% defined by the Petersen criteria, and 11% of sd-aMCI and 29% of md-aMCI defined by the Winblad criteria [47].
Several modeling studies have estimated the progression of dementia severity in patients with AD. An analysis based on patients from the National Alzheimer’s Coordinating Center (NACC) (n = 3009) estimated that a starting population of patients with mild (69.5%) or moderate (30.5%) dementia would progress to mild (38.6%), moderate (44.1%), or severe (7.3%) dementia or death (10.0%) after 1 year [53]. Another analysis based on a larger NACC population (n = 18,103) estimated that patients aged 65 years with mild AD dementia had a 25% chance of progression to moderate (19%) or severe (1%) dementia or death (4%) within 1 year, whereas those with moderate AD dementia would have a 36% chance of progression to severe dementia (27%) or deal (9%) [54]. Slightly higher progression rates were estimated for patients aged 75 years. Unfortunately, neither of these studies took patient amyloid status into consideration. A more recent analysis limited to Aβ-positive patients estimated higher annual rates of progression. Among Aβ-positive patients with mild dementia, 45.1% of patients with progressed to moderate (31.6%) or severe (4.3%) dementia or death (9.2%) within 1 year. Among those with moderate dementia, 59.8% progressed to severe dementia (28.6%) or death (31.2%) [55]. These analyses highlight the limitation of studying AD progression without incorporating biomarker estimates including amyloid status.
Risk Factors for Disease Progression
Understanding risk factors associated with disease progression can help individual patients make decisions regarding their future as well as guide clinical development and use of treatments for slowing progression [56, 57]. However, the factors noted previously that influence data on reported rates of progression also are likely to influence data on risk factors, sometimes resulting in conflicting results.
Some researchers have examined which tests (neurocognitive or biomarkers) might be the most valuable in identifying patients who are likely to progress from clinically diagnosed MCI to AD dementia or from mild to more severe AD dementia. In the meta-analysis of 28 studies (through 2014) that included 2365 patients with MCI, described previously, the objective was to evaluate the predictive value of neurocognitive tests for progression to dementia [48]. Five tests were shown to have excellent (≥ 0.90) sensitivity and specificity: Addenbrooke’s Cognitive Examination (a global measure), Visual Object and Space Perception Silhouettes (visuospatial), Object Function Recognition (language), and three tests of verbal episodic memory (Face–Name Association Task; Rey Auditory Verbal Learning Test, and Guild Paragraph) [48]. The meta-analysis of 24 studies (through 2018) that included 2689 patients with clinically diagnosed MCI (primarily aMCI) examined the ability of neuropsychological testing to predict progression to AD dementia [58]. A mean of 37% of these patients progressed to AD dementia [58]. Overall, patients who progressed did worse on a variety of measures than did non-progressors, affirming the relevance of neuropsychiatric testing [58]. In a systematic analysis of 48 studies that examined biomarkers in patients with AD dementia, little information was available from studies with follow-up of more than 2.5 years or with repeated testing [59]. Although magnetic resonance imaging (MRI) scan of whole brain or hippocampal atrophy was the most common testing measure, the investigators noted it is not specific to AD [59]. In most studies, evaluation of progression was based on cognitive testing, but there was no consensus on which tests or combinations of tests were most valuable [59].
Risk factors for progressing from unimpaired cognition to aMCI were evaluated on the basis of data from approximately 1500 individuals in the ADNI database [60]. Over 4 years, 17% of unimpaired participants converted to aMCI [60]. Significant risk factors for this conversion were low hippocampal volume, a high CSF tau/Aβ ratio, and a low memory score; neither increasing age nor family history of AD was significant [60]. The risk of conversion from no impairment to aMCI increased with the number of risk factors; participants with three risk factors had an estimated probability of developing aMCI of 0.35 over 4 years of follow-up [60].
Multiple risk factors for progressing from MCI to AD dementia have been proposed. A meta-analysis of 53 studies with 12,396 patients with AD dementia and 1934 with MCI examined progression risk [61]. For patients with MCI, rapid progression to AD dementia was associated with positive APOE4, greater white matter hyperintensity volume, entorhinal cortex atrophy, high CSF neurogranin levels, and high dependency in instrumental activities of daily living (IADLs) [61]. More engagement in social activities and a higher body mass index (BMI) were associated with slower progression to AD dementia [61]. Evaluation of the ADNI database showed that of patients with aMCI at baseline, 35% had progressed to AD dementia by 4 years [60]. Significant risk factors for progression were APOE4 positive, high FAQ score, a low memory score, hippocampal atrophy, and a high tau/Aβ ratio [60]. Risk increased with the number of risk factors; participants with five risk factors had an estimated probability of developing aMCI of 0.90 over 4 years of follow-up [60]. In a meta-analysis of 60 studies (1966–2015) of patients with MCI, the greatest risk factors for progression to AD dementia were abnormal CSF tau, abnormal CSF tau/Aβ ratio, hippocampal atrophy, medial temporal lobe atrophy, and entorhinal atrophy [62]. Other risk factors were APOE4 positive, CSF total tau, white matter hyperintensity volume, depression, diabetes, hypertension, older age, female gender, lower MMSE score, and higher ADAS-cog score [62]. Protective factors were high BMI and higher auditory verbal learning test delay score. Individuals with a combination of risk factors had an even greater risk for progression [62]. It has been demonstrated that declines in both cognitive and financial skills in patients with clinically diagnosed MCI are significant predictors of clinical progression [50].
Many studies have attempted to identify risk factors for progression from mild to more severe AD dementia. Several factors increasing the risk of AD dementia have been identified in this review (Table 3). There are conflicting results for some factors (e.g., age, comorbidities, education level), but many studies agree that atrophy in various brain regions, poor baseline memory and ADAS-cog scores, and abnormal CSF biomarkers are risk factors [49]. Other potential factors that vary by AD dementia severity include hair cortisol levels, which have been observed to be higher in patients with more severe dementia compared to those with mild dementia, and salivary IgA levels, which exhibit the inverse pattern [63]. Systemic inflammation, as evidenced by consistently elevated concentrations of inflammatory biomarkers and cytokines, has been observed in patients with AD dementia [64]. However, inflammatory biomarkers have not always been associated with measures of clinical disease progression in patients with clinically diagnosed MCI or AD dementia [65]. A recent study in a small number of patients (n = 39 patients with AD dementia and n = 21 healthy controls) found that the levels of oligomeric Aβ in nasal discharge were higher in patients with AD dementia and that the presence of specific Aβ oligomers could distinguish between patients with mild and moderate cognitive dysfunction [66].
Some analyses have focused on factors associated with rapid or slow decline. The previously described systematic literature review of 53 studies of patients with MCI and AD dementia reported that risk factors for rapid progression in patients with dementia were APOE4 positive, early age at onset, higher level of education, early appearance of extrapyramidal signs, and neuropsychiatric conditions [61]. Factors such as age ≥ 75 years, diabetes, and multidrug therapy lowered the risk of rapid progression [61]. In the Impact of Cholinergic Use (ICTUS) study, a prospective study in 12 European countries that followed 1005 patients with AD dementia, a worse baseline ADAS-cog score was significantly associated with rapid decline, while increased age at baseline was a protective factor [57]. The Progression of Alzheimer's Disease and Resource use (PADR) study evaluated 282 Norwegian patients with AD dementia for a mean of 2 years [67]. Over 40% of patients progressed slowly (47% by change in Clinical Dementia Rating Scale-Sum of Boxes [CDR-SB] and 44% by change in MMSE) [67]. Baseline factors associated with slower progression on the CDR-SB were younger age at diagnosis, higher education, better IADL function, better scores on cognitive tests, used fewer drugs, and 1-point lower CSR-SB score, while better scores on cognitive tests and better CDR-SB score were associated with slower progression on the MMSE and IADL [67].
The Canadian Outcomes Study in Dementia (COSID) evaluated overall progression using data from 488 patients with AD dementia [68]. After adjustment for age, patients who progressed were significantly more likely at baseline to have poorer cognition, greater dependence, and more neuropsychiatric symptoms [68]. Male sex and having a worse baseline Global Deterioration Scale (GDS) score were significant protective factors [68]. A systematic literature review of 11 studies (to 2016) evaluating the influence of comorbid conditions on progression of late-onset AD dementia [56] found associations between comorbidities and declines in cognitive function and functional abilities, as well as increases in neuropsychiatric symptoms [56]. Other studies have examined specific factors protective or predictive of clinical progression. Blood pressure variability [69] has been proposed as a risk factor for progression, and cognitive reserve (e.g., IQ prior to disease onset) [70] has been proposed as a protective factor. A recent analysis of healthy controls (n = 318) and individuals with MCI (n = 168) or AD dementia (n = 269) found that neuroinflammation (as evidenced by translocator protein (TSPO) identified during PET) increases with more severe AD dementia [71]. Compared with healthy controls, individuals with MCI had increased TSPO levels in the neocortex and those with AD had even greater levels of TSPO present throughout the brain [71]. There was a significant inverse association between TSPO levels in the parietal region of the brain and MMSE scores (p = 0.024) [71].
Discussion
This review of the literature on epidemiology and clinical progression of AD underscores the importance of identifying patients who are most at risk of developing AD dementia. The worldwide toll of AD is evidenced by rising prevalence and mortality due to AD dementia. With many countries experiencing population aging, the prevalence of AD dementia continues to rise, thereby increasing the already substantial clinical and socioeconomic burden of this disease. The state of knowledge regarding AD epidemiology suggests that clinicians will face significant and increasing numbers of patients presenting with potential risk factors for progression to clinical AD, and thus will need to have the capability to identify patients early in the disease process who are most likely to benefit from treatment. However, studies of AD prevalence, incidence and mortality face challenges in diagnosis as well as classification of disease stage.
The criteria developed to classify patients into categories of preclinical AD, MCI due to AD, and AD dementia, while aligned in some ways, vary enough to prevent accurate comparisons across studies of epidemiology and progression risk. It is particularly difficult to distinguish MCI with AD etiology from MCI due to other etiologies such as CVD and Lewy body dementia.
The risk of dementia increases with stages of progression, from normal cognition with no Aβ deposition to Aβ deposition, hyperphosphorylated tau, and neuronal injury, and subsequently to MCI due to AD. More research is needed to understand the spectrum of disease from preclinical AD to clinical dementia. While data on progression of preclinical AD to MCI are sparse, evidence is available on the progression from MCI to dementia [11, 20, 44, 47, 48]. Current research suggests that almost 40% of patients with clinically diagnosed MCI progress to AD dementia over an average of 18 months [48]. Key risk or protective factors for progression to AD dementia from clinically diagnosed MCI include MCI subtype (e.g., aMCI, naMCI), poor performance on various neurocognitive tests, and biomarkers such as abnormal CSF tau or tau/Aβ ratio, APOE4 positive status, white matter hyperintensities, and atrophy in the hippocampal, medial temporal, or entorhinal regions [20, 58, 61]. Newer emerging treatments are more likely to prevent or delay further progression of AD dementia than to reverse it [11].
Unfortunately, most of the literature on AD reports on patients diagnosed on the basis of clinical criteria such as the DSM-IV, the 1984 National Institute of Neurological and Communicative Disorders and Stroke (NINCDS)/Alzheimer’s Disease and Related Disorders Association (ADRDA), or the 2011 NIA-AA [12,13,14, 72, 73]. To treat individuals most likely to benefit from a DMT, it is important for clinicians to have the ability to identify patients at risk of AD in early stages, prior to progressive deterioration. Biomarker identification added to neurocognitive testing will be an increasingly important component of diagnosis and measurement of progression and is likely to improve the ability of practicing clinicians to identify patients who will experience a treatment benefit.
Conclusion
AD dementia incidence and prevalence are high worldwide and likely underestimated. Recent studies show that the risk of AD dementia is significant among older people with normal pathology and increases with progression from normal pathology to neurodegeneration and MCI. Studies of AD remain challenged by disease classification due to differential diagnosis, multiple biomarkers and neuropsychiatric tests, and variation in consensus criteria. As new DMTs are introduced, clinicians will require combinations of diagnostic approaches to identify patients with preclinical AD and MCI due to AD and to assess the impact of treatment on slowing progression.
References
Atri A. The Alzheimer’s disease clinical spectrum: diagnosis and management. Med Clin North Am. 2019;103(2):263–93.
Jack CR Jr, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12(2):207–16.
Li Q, Wu Y, Chen J, et al. Microglia and immunotherapy in Alzheimer’s disease. Acta Neurol Scand. 2022;145(3):273–8.
Spanic E, Langer Horvat L, Hof PR, et al. Role of microglial cells in Alzheimer’s disease tau propagation. Front Aging Neurosci. 2019;11:271.
Scheltens P, Blennow K, Breteler MM, et al. Alzheimer’s disease. Lancet. 2016;388(10043):505–17.
Harada CN, Natelson Love MC, Triebel KL. Normal cognitive aging. Clin Geriatr Med. 2013;29(4):737–52.
Steiner ABQ, Jacinto AF, Mayoral VFS, et al. Mild cognitive impairment and progression to dementia of Alzheimer's disease. Rev Assoc Med Bras (1992). 2017;63(7):651–5.
Alzheimer's Association. 2021 Alzheimer's disease facts and figures. Alzheimers Dement. 2021;17(3):327–406.
Marasco RA. Current and evolving treatment strategies for the Alzheimer disease continuum. Am J Manag Care. 2020;26(8 Suppl):S167–76.
Wong W. Economic burden of Alzheimer disease and managed care considerations. Am J Manag Care. 2020;26(8 Suppl):S177–83.
Bradfield NI, Ellis KA, Savage G, et al. Baseline amnestic severity predicts progression from amnestic mild cognitive impairment to Alzheimer disease dementia at 3 years. Alzheimer Dis Assoc Disord. 2018;32(3):190–6.
Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9.
McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–9.
Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):280–92.
Jack CR Jr, Bennett DA, Blennow K, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14(4):535–62.
Babic M, Svob Strac D, Muck-Seler D, et al. Update on the core and developing cerebrospinal fluid biomarkers for Alzheimer disease. Croat Med J. 2014;55(4):347–65.
Qu Y, Ma YH, Huang YY, et al. Blood biomarkers for the diagnosis of amnestic mild cognitive impairment and Alzheimer’s disease: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;128:479–86.
Kern S, Zetterberg H, Kern J, et al. Prevalence of preclinical Alzheimer disease: comparison of current classification systems. Neurology. 2018;90(19):e1682–91.
Bradfield NI, Ames D. Mild cognitive impairment: narrative review of taxonomies and systematic review of their prediction of incident Alzheimer’s disease dementia. BJPsych Bull. 2020;44(2):67–74.
Oltra-Cucarella J, Ferrer-Cascales R, Alegret M, et al. Risk of progression to Alzheimer’s disease for different neuropsychological mild cognitive impairment subtypes: a hierarchical meta-analysis of longitudinal studies. Psychol Aging. 2018;33(7):1007–21.
Dubois B, Villain N, Frisoni GB, et al. Clinical diagnosis of Alzheimer’s disease: recommendations of the International Working Group. Lancet Neurol. 2021;20(6):484–96.
Asada T. Epidemiology of dementia in Japan. In: Matsuda H, Adada T, Tokumaru AM, editors. Neuroimaging diagnosis for Alzheimer’s disease and other dementias. Tokyo: Springer; 2017.
Montgomery W, Ueda K, Jorgensen M, et al. Epidemiology, associated burden, and current clinical practice for the diagnosis and management of Alzheimer’s disease in Japan. ClinicoEcon Outcomes Res. 2018;10:13–28.
Fiest KM, Roberts JI, Maxwell CJ, et al. The prevalence and incidence of dementia due to Alzheimer’s disease: a systematic review and meta-analysis. Can J Neurol Sci. 2016;43(Suppl 1):S51-82.
Niu H, Alvarez-Alvarez I, Guillen-Grima F, et al. Prevalence and incidence of Alzheimer’s disease in Europe: a meta-analysis. Neurologia. 2017;32(8):523–32.
Takizawa C, Thompson PL, van Walsem A, et al. Epidemiological and economic burden of Alzheimer’s disease: a systematic literature review of data across Europe and the United States of America. J Alzheimers Dis. 2015;43(4):1271–84.
Cui L, Hou NN, Wu HM, et al. Prevalence of Alzheimer’s disease and Parkinson’s disease in China: an updated systematical analysis. Front Aging Neurosci. 2020;12: 603854.
Zhao X, Li X. The prevalence of Alzheimer’s disease in the Chinese Han population: a meta-analysis. Neurol Res. 2020;42(4):291–8.
Chan KY, Wang W, Wu JJ, et al. Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990–2010: a systematic review and analysis. Lancet. 2013;381(9882):2016–23.
Rajan KB, Weuve J, Barnes LL, et al. Prevalence and incidence of clinically diagnosed Alzheimer’s disease dementia from 1994 to 2012 in a population study. Alzheimers Dement. 2019;15(1):1–7.
Collaborators GBDD. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18(1):88–106.
Niu H, Alvarez-Alvarez I, Guillen-Grima F, et al. Trends of mortality from Alzheimer’s disease in the European Union, 1994–2013. Eur J Neurol. 2017;24(6):858–66.
Park J. Mortality from Alzheimer’s disease in Canada: a multiple-cause-of-death analysis, 2004 to 2011. Health Rep. 2016;27(5):17–21.
Kramarow EA, Tejada-Vera B. Dementia mortality in the United States, 2000–2017. Natl Vital Stat Rep. 2019;68(2):1–29.
Price A, Farooq R, Yuan JM, et al. Mortality in dementia with Lewy bodies compared with Alzheimer’s dementia: a retrospective naturalistic cohort study. BMJ Open. 2017;7(11): e017504.
Brookmeyer R, Abdalla N, Kawas CH, et al. Forecasting the prevalence of preclinical and clinical Alzheimer’s disease in the United States. Alzheimers Dement. 2018;14(2):121–9.
Jia L, Du Y, Chu L, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. 2020;5(12):e661–71.
Vos SJ, Verhey F, Frölich L, et al. Prevalence and prognosis of Alzheimer’s disease at the mild cognitive impairment stage. Brain. 2015;138(Pt 5):1327–38.
Gillis C, Mirzaei F, Potashman M, et al. The incidence of mild cognitive impairment: a systematic review and data synthesis. Alzheimers Dement (Amst). 2019;11:248–56.
Knopman DS, Gottesman RF, Sharrett AR, et al. Mild cognitive impairment and dementia prevalence: the atherosclerosis risk in communities neurocognitive study (ARIC-NCS). Alzheimers Dement (Amst). 2016;2:1–11.
Lu H, Wang XD, Shi Z, et al. Comparative analysis of cognitive impairment prevalence and its etiological subtypes in a rural area of northern China between 2010 and 2015. Sci Rep. 2019;9(1):851.
Lu Y, Liu C, Yu D, et al. Prevalence of mild cognitive impairment in community-dwelling Chinese populations aged over 55 years: a meta-analysis and systematic review. BMC Geriatr. 2021;21(1):10.
Brookmeyer R, Abdalla N. Estimation of lifetime risks of Alzheimer’s disease dementia using biomarkers for preclinical disease. Alzheimers Dement. 2018;14(8):981–8.
Parnetti L, Chipi E, Salvadori N, et al. Prevalence and risk of progression of preclinical Alzheimer’s disease stages: a systematic review and meta-analysis. Alzheimers Res Ther. 2019;11(1):7.
Henneges C, Reed C, Chen YF, et al. Describing the sequence of cognitive decline in Alzheimer’s disease patients: results from an observational study. J Alzheimers Dis. 2016;52(3):1065–80.
Karr JE, Graham RB, Hofer SM, et al. When does cognitive decline begin? A systematic review of change point studies on accelerated decline in cognitive and neurological outcomes preceding mild cognitive impairment, dementia, and death. Psychol Aging. 2018;33(2):195–218.
Oltra-Cucarella J, Sanchez-SanSegundo M, Lipnicki DM, et al. Using base rate of low scores to identify progression from amnestic mild cognitive impairment to Alzheimer’s disease. J Am Geriatr Soc. 2018;66(7):1360–6.
Belleville S, Fouquet C, Hudon C, et al. Neuropsychological measures that predict progression from mild cognitive impairment to Alzheimer’s type dementia in older adults: a systematic review and meta-analysis. Neuropsychol Rev. 2017;27(4):328–53.
Fang Y, Du N, Xing L, et al. Evaluation of hippocampal volume and serum brain-derived neurotrophic factor as potential diagnostic markers of conversion from amnestic mild cognitive impairment to Alzheimer disease: a STROBE-compliant article. Medicine (Baltimore). 2019;98(30): e16604.
Gerstenecker A, Triebel KL, Martin R, et al. Both financial and cognitive decline predict clinical progression in MCI. Alzheimer Dis Assoc Disord. 2016;30(1):27–34.
Sörensen A, Blazhenets G, Rücker G, et al. Prognosis of conversion of mild cognitive impairment to Alzheimer’s dementia by voxel-wise Cox regression based on FDG PET data. Neuroimage Clin. 2019;21: 101637.
Hu C, Yu D, Sun X, et al. The prevalence and progression of mild cognitive impairment among clinic and community populations: a systematic review and meta-analysis. Int Psychogeriatr. 2017;29(10):1595–608.
Green C, Zhang S. Predicting the progression of Alzheimer’s disease dementia: a multidomain health policy model. Alzheimers Dement. 2016;12(7):776–85.
Davis M, O’Connell T, Johnson S, et al. Estimating Alzheimer’s disease progression rates from normal cognition through mild cognitive impairment and stages of dementia. Curr Alzheimer Res. 2018;15(8):777–88.
Potashman M, Buessing M, Levitchi Benea M, et al. Estimating progression rates across the spectrum of Alzheimer’s disease for amyloid-positive individuals using national Alzheimer’s coordinating center data. Neurol Ther. 2021;10(2):941–53.
Haaksma ML, Vilela LR, Marengoni A, et al. Comorbidity and progression of late onset Alzheimer’s disease: a systematic review. PLoS ONE. 2017;12(5): e0177044.
Canevelli M, Kelaiditi E, Del Campo N, et al. Predicting the rate of cognitive decline in Alzheimer disease: data from the ICTUS study. Alzheimer Dis Assoc Disord. 2016;30(3):237–42.
Prado CE, Watt S, Treeby MS, et al. Performance on neuropsychological assessment and progression to dementia: a meta-analysis. Psychol Aging. 2019;34(7):954–77.
Lawrence E, Vegvari C, Ower A, et al. A systematic review of longitudinal studies which measure Alzheimer’s disease biomarkers. J Alzheimers Dis. 2017;59(4):1359–79.
Steenland K, Zhao L, John SE, et al. A “Framingham-like” algorithm for predicting 4-year risk of progression to amnestic mild cognitive impairment or Alzheimer’s disease using multidomain information. J Alzheimers Dis. 2018;63(4):1383–93.
Song YN, Wang P, Xu W, et al. Risk factors of rapid cognitive decline in Alzheimer’s disease and mild cognitive impairment: a systematic review and meta-analysis. J Alzheimers Dis. 2018;66(2):497–515.
Li JQ, Tan L, Wang HF, et al. Risk factors for predicting progression from mild cognitive impairment to Alzheimer’s disease: a systematic review and meta-analysis of cohort studies. J Neurol Neurosurg Psychiatry. 2016;87(5):476–84.
de la Rubia Ortí JE, Prado-Gascó V, Sancho Castillo S, et al. Cortisol and IgA are involved in the progression of Alzheimer’s disease. A pilot study. Cell Mol Neurobiol. 2019;39(7):1061–5.
Su C, Zhao K, Xia H, et al. Peripheral inflammatory biomarkers in Alzheimer’s disease and mild cognitive impairment: a systematic review and meta-analysis. Psychogeriatrics. 2019;19(4):300–9.
Hazen J, Vistnes M, Barca ML, et al. The Association between circulating inflammatory markers and the progression of Alzheimer disease in Norwegian memory clinic patients with mild cognitive impairment or dementia. Alzheimer Dis Assoc Disord. 2020;34(1):47–53.
Yoo SJ, Son G, Bae J, et al. Longitudinal profiling of oligomeric Aβ in human nasal discharge reflecting cognitive decline in probable Alzheimer’s disease. Sci Rep. 2020;10(1):11234.
Eldholm RS, Barca ML, Persson K, et al. Progression of Alzheimer’s disease: a longitudinal study in Norwegian memory clinics. J Alzheimers Dis. 2018;61(3):1221–32.
Herrmann N, Harimoto T, Balshaw R, et al. Risk factors for progression of Alzheimer disease in a Canadian population: the Canadian outcomes study in dementia (COSID). Can J Psychiatry. 2015;60(4):189–99.
de Heus RAA, Olde Rikkert MGM, Tully PJ, et al. Blood pressure variability and progression of clinical Alzheimer disease. Hypertension. 2019;74(5):1172–80.
Osone A, Arai R, Hakamada R, et al. Impact of cognitive reserve on the progression of mild cognitive impairment to Alzheimer’s disease in Japan. Geriatr Gerontol Int. 2015;15(4):428–34.
Bradburn S, Murgatroyd C, Ray N. Neuroinflammation in mild cognitive impairment and Alzheimer’s disease: a meta-analysis. Ageing Res Rev. 2019;50:1–8.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. 4th ed. Washington: American Psychiatric Association; 1994.
McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s disease. Neurology. 1984;34(7):939–44.
Acknowledgements
Funding
Eisai provided the funding for the literature review and the manuscript, including the journal’s Rapid Service Fees.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICJME) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the conception and design of the manuscript. Amir Abbas Tahami Monfared and Quanwu Zhang provided the idea behind the article, Michael Byrnes conducted the literature review, Michael Byrnes and Leigh Ann White designed and drafted the manuscript, and Amir Abbas Tahami Monfared and Quanwu Zhang provided feedback and critical analysis of literature review methods, manuscript outlines, and manuscript text. Karin Hawkinson, a former employee of Evidera, contributed to the development of the sections of the manuscript focused on humanistic burden.
Disclosures
Amir Abbas Tahami Monfared and Quanwu Zhang are employees of Eisai; Michael Byrnes and Leigh Ann White are employees of Evidera, Inc.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tahami Monfared, A.A., Byrnes, M.J., White, L.A. et al. Alzheimer’s Disease: Epidemiology and Clinical Progression. Neurol Ther 11, 553–569 (2022). https://doi.org/10.1007/s40120-022-00338-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-022-00338-8