Abstract
Autistic youth have an increased risk of mental health problems. Despite the efficacy of various psychotherapeutic approaches for autistic youth, they often do not receive these interventions. Research is needed to identify patterns of effective treatment for autistic youth and whether they differ from those used for youth with other neurodevelopmental conditions (e.g., attention-deficit hyperactivity disorder; ADHD). We compared clinicians’ (N = 557) knowledge, confidence and practices when treating autistic youth and youth with ADHD. Although ratings were moderately high overall and similar interventions were used for both groups, clinicians were significantly less knowledgeable and confident when supporting autistic clients compared to clients with ADHD. Thus, improving clinician perspectives may help facilitate treatment for autistic youth with mental health problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well established that autisticFootnote 1 children and adolescents (hereafter referred to as youth) are more vulnerable to a range of mental health problems relative to their neurotypical peers, whether these problems are operationalized as discrete psychiatric diagnoses or in terms of elevated symptomatology. For example, a recent meta-analysis examining the prevalence of mental health challenges demonstrated that autistic people are significantly more likely than peers in the general population to have anxiety disorders, depressive disorders, bipolar and related disorders, schizophrenia spectrum and psychotic disorders, and obsessive compulsive and related disorders, with rates understandably being higher in clinic-based studies compared to population-based registries (Lai et al., 2019). Similarly, when investigating parent-reported emotional and behavioural problems, Totsika et al. (2011) found that autistic youth (with and without intellectual disability) were three to four times more likely to have clinically significant emotional and conduct problems compared to the general population and had higher rates than those observed among non-autistic youth with intellectual disabilities.
There is growing evidence that many of the interventions that are effective in addressing the mental health problems of youth without autism are also helpful for autistic youth when adapted (Weston et al., 2016). For example, the provision of cognitive behaviour therapy (CBT) to address anxiety (Perihan et al., 2020), emotional dysregulation (Weiss et al., 2018), and depressive symptoms (McGillivray & Evert, 2014), the use of mindfulness-based approaches to address anger (Singh et al., 2011), and the use of parent management training to assist with conduct problems (Sofronoff et al., 2004) have all shown promising results among autistic people. In fact, many of the interventions that have been studied in reference to autistic youth are adaptations of the same interventions that have been used by mental health clinicians for non-autistic clients, including Coping Cat (Kendall & Hedtke, 2006), Incredible Years (Hutchings et al., 2016), Parent–Child Interaction Therapy (Masse et al., 2016) and Triple P-Positive Parenting (Tellegen & Sanders, 2014). However, the extent to which therapists use the broader set of psychotherapeutic approaches (e.g., family therapy, Dialectical Behaviour Therapy [DBT], Interpersonal Therapy, etc.) for autistic youth, as they might for youth without autism, is largely unknown, and few have examined how helpful clinicians deem these approaches.
There are several ways that clinicians are adapting interventions to meet the unique needs of their autistic clients (Moree & Davis, 2010). In reference to CBT provision for autistic clients, National Institute for Health and Care Excellence (NICE, 2012) guidelines suggest that clinicians make adaptations that minimize the cognitive demands of CBT without altering its content, such as incorporating structured activities and written/visual information and using plain language. Indeed, Cooper et al. (2018) surveyed 54 clinicians before they attended a 1-day training workshop on adapting CBT for autistic people and found that clinicians already endorsed many adaptations in line with NICE guidelines, such as incorporating behavioural strategies (74% of providers sampled), taking a more structured and concrete approach (70%), simplifying language (70%), providing psychoeducation about emotional experiences (68%), and using visual or written aids (60%). A systematic review examining the adaptations employed in effective cognitive behavioural interventions for autistic youth noted that the most common adaptations included implementing visual aids or workbooks, incorporating child-specific interests, involving caregivers, providing structure, and incorporating emotion recognition training (Walters et al., 2016). In many cases, however, Walters et al. also noted that additional adaptations beyond NICE recommendations were made, demonstrating that different patterns or combinations of adaptations may be attempted. While these findings indicate that many clinicians are employing adaptations to serve autistic youth, they also highlight the variability that exists across providers in terms of the number and types of adaptations employed, and the literature to date has largely focussed on adaptations to CBT, rather than the broader spectrum of psychotherapeutic interventions provided to autistic youth.
Despite these advances, autistic youth continue to experience barriers in accessing psychotherapy for their mental health difficulties. There has been an increased interest in clinician-level barriers to care, such as low therapist confidence and self-perceived knowledge (Brookman-Frazee et al., 2012a, 2012b, 2012c; Maddox et al., 2019), as many therapists perceive themselves as unable to adapt their mental health treatments to support autistic clients (Adams & Young, 2020). In fact, when examining specific strengths and gaps in providers’ confidence to deliver CBT to autistic people, Cooper et al. (2018) found that providers were most confident in their ability to be empathetic, establish a therapeutic alliance, and collect information to understand their clients’ challenges, but lacked confidence in their ability to use appropriate assessments and identify effective therapeutic approaches for these clients. Interestingly, similar results have emerged in the context of intellectual disability, whereby providers report greater confidence in their general therapeutic abilities, such as their ability to empathize and establish a therapeutic connection with clients, and less confidence in more specific aspects of treatment, such as their use of assessments (Dagnan et al., 2015). Collectively, these results suggest that confidence may not be best gauged with an omnibus rating, which risks losing the nuances related to specific psychotherapeutic activities.
It has also been shown that many clinicians have limited knowledge about autism and have difficulties tailoring interventions to fit autistic youth’s needs. For instance, results indicate that over 75% of clinicians desire further information about mental health interventions for autistic clients, specifically in terms of how to engage in treatment planning and develop targeted strategies for autistic youth (Brookman-Frazee et al., 2012a, 2012b, 2012c). These gaps in knowledge can negatively impact clinicians’ attitudes about delivering psychotherapy to autistic clients, thereby affecting their intentions to treat this client group relative to neurotypical clients (Maddox et al., 2019). At the same time, training clinicians in children’s mental health agencies to use behavioural parent-mediated and child led evidence-based strategies can lead to increases in overall perceived knowledge and confidence in working with autistic children (Brookman-Frazee et al., 2012a, 2012b, 2012c), suggesting that these barriers can be overcome once identified.
There are three notable gaps in our current understanding of psychotherapy provision for autistic youth, which, if addressed, could further inform initiatives aimed at expanding clinicians’ capacity to work with this population. First, most research has focussed exclusively on the provision of CBT. In terms of psychotherapy for youth, varying presenting problems are associated with a multitude of intervention approaches, each with its own evidence base and commonplace within publicly funded mental health agencies (e.g., CBT, DBT, parent-mediated, attachment-focused, interpersonal, family therapy, etc.). Thus, a broader focus on psychotherapy for autistic youth will provide greater ecological validity. Second, most research on these constructs has emerged within the context of mental health care in the United States, which has a unique system of public–private insurance mechanisms. Accordingly, previous research may not reflect the socialized mental health care models found in other jurisdictions, such as Canada or the United Kingdom. Lastly, no study has explored whether these issues are specific to autism or whether they reflect how clinicians approach supporting youth with other neurodevelopmental conditions as well. By comparing mental health providers’ treatment approaches and adaptations, knowledge, and confidence for autistic clients to those with another neurodevelopmental condition, we can further elucidate whether patterns are autism-specific or more generally implicated in how clinicians support clients with neurodevelopmental disability.
Current Study
The objective of the current study was to better understand community-based clinicians’ knowledge, confidence and treatment approaches when working with autistic youth with mental health problems. We contrasted clinicians’ responses for autistic clients with their responses for clients with ADHD. Similar to autism, ADHD is chronic, impacts therapeutic interactions (Halldorsdottir & Ollendick, 2014), and often co-occurs with mental health problems (e.g., anxiety disorders, depression, oppositionality and conduct problems; Larson et al., 2011; Yoshimasu et al., 2012). It has been noted that youth with ADHD also have difficulty accessing mental health clinicians and that barriers to care exist as a result of a lack of clinician knowledge, competence, and confidence, along with a host of systems-level barriers (Brahmbhatt et al., 2016; French et al., 2019; Hoagwood et al., 2000). For example, reports indicate that less than half of families with a child with ADHD have met with a mental health provider in the prior year (Cuffe et al., 2009; Lesesne et al., 2003) and studies of adult mental health providers have highlighted the need for additional ADHD training, showing that the majority of providers have limited knowledge about ADHD and insufficient resources to effectively support these clients (Hall et al., 2013). These gaps in care provision are especially evident when clients with disabilities are compared to those without neurodevelopmental challenges. Indeed, a study by Maddox et al. (2019) showed that providers hold significantly worse attitudes towards, and lower intentions of, delivering psychotherapy to autistic clients relative to those without autism, while research comparing providers’ comfort levels has shown that they report greater comfortability when treating clients with mood-based challenges versus clients with ADHD (Adler et al., 2009; Miller et al., 2005). Identifying autism-specific deficits in clinician knowledge, confidence, or adaptations to care would suggest the need for autism-specific training and policies to address barriers, while similar levels may imply the need for similar approaches to neurodevelopmental conditions more broadly. Thus, the following research questions were examined:
-
1.
Do clinicians endorse using similar treatment approaches when treating mental health problems in autistic clients and clients with ADHD and do they rate these approaches as more helpful for one client group?
-
2.
Are clinicians less confident and knowledgeable about delivering psychotherapy to autistic clients compared to clients with ADHD?
-
3.
Do clinicians report using more adaptations when delivering psychotherapy to autistic clients compared to clients with ADHD?
Methods
Participants
The sample included 557 clinicians who reported delivering psychotherapy to autistic clients and to clients with ADHD to address mental health problems. As presented in Table 1, clinicians were between the ages of 20 and 75 years (M = 40.73, SD = 10.87) and the majority identified as women (83.2%) and White/Caucasian (80.2%). Most participants were employed full-time (92.3%) as direct service providers (88.6%) and had a post-secondary education, such as a bachelor’s degree (32.0%) or a master’s degree (36.0%). Participants were also primarily social workers (45.3%), child and youth workers (20.8%), and registered psychotherapists (20.1%), and indicated that their primary theoretical orientation was cognitive-behavioural (42.9%), eclectic (34.2%), behavioural (12.5%), or other (e.g., integrative; 10.4%). Further, participants had considerable experience, with approximately 61% having worked in the field for at least 10 years. On average, participants indicated that 20.8% (SD = 19.6%, Median = 15.0%) of their caseload involved autistic clients with mental health problems and 47.8% (SD = 24.6%, Median = 50.0%) of their caseload involved clients with ADHD and mental health problems. Further, provider-reported rates of mental health problems were similar across client groups, with anxiety, challenging behaviours, and depression being endorsed as the most common (see Table 1).
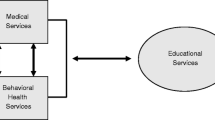
Publicly Funded Child and Youth Mental Health (CYMH) Context in Ontario, Canada
In Ontario, Canada, CYMH care is delivered through a number of service sectors, resulting in complex care pathways that are often difficult for families to navigate (Duncan et al., 2018). Further, there is little consistency in the provision of services across the country, as each province/territory is responsible for the management and delivery of its own CYMH programs; nonetheless, a number of families receive CYMH services in Ontario in the community via publicly funded agencies (Cappelli et al., 2019), which can be accessed through self-referrals or referrals from primary care providers and/or other relevant professionals (e.g., child protection workers, school personnel, etc.). Publicly funded children’s mental health agencies provide a range of core services to children and youth between the ages of 0 and 17 years, including brief walk-in services, family support, specialized consultations/assessments, service coordination, crisis support, and intensive treatments (Duncan et al., 2018). These agencies are funded by the Ministry of Children, Community, and Social Services (MCCSS) and treat children and youth across the spectrum of mental health need through interprofessional teams consisting of social workers, psychotherapists, child and youth workers, psychologists, and other mental health professionals. The interventions that are provided vary considerably based on the range of presenting problems, client ages, client preferences, and clinical capacity of each organization. Some agencies provide services across the age span, while others are more focused on specific age groups. Some agencies provide a large range of intervention modalities, while others are more focused on specific types.
In Ontario, to provide the controlled act of psychotherapy, one must be a registered member of one of the six authorized regulatory colleges: the College of Registered Psychotherapists of Ontario (CRPO), the College of Psychologists of Ontario (CPO), the Ontario College of Social Workers and Social Service Workers (OCSWSSW), the College of Nurses of Ontario (CNO), College of Occupational Therapists of Ontario (COTO), and the College of Physicians and Surgeons of Ontario (CPSO). Each regulatory college has its own educational and competency-based requirements and prescribed practices; however, in most cases, at least a master’s-level education is needed. For example, according to CRPO (2019), those seeking registration must have a master’s degree or an equivalent graduate diploma from a program with a bachelor’s-level degree as an admission requirement. Thus, practicing clinicians in Ontario may differ in their educational backgrounds, professional training, and therapeutic orientations, as demonstrated in Table 1.
Procedure
Using a cross-sectional design, publicly funded clinicians across Ontario, Canada were recruited by their agencies to complete an online survey assessing their experiences delivering psychotherapy to address the mental health needs of autistic youth and youth with ADHD. Specifically, clinical or administrative leads shared an anonymous survey link with frontline service providers who treat children and adolescents with mental health challenges. Each agency decided on its own process for informing providers about the survey. Survey questions about autism and ADHD were counterbalanced across participants, such that some participants were first asked to respond to questions about clients with ADHD, while others were first asked about autistic clients. All participants provided informed consent before completing the survey, and the survey was available in English or French. This research was approved by the University’s Ethics Review Board [#e2020-253].
The survey was piloted by clinicians from Ottawa and after the survey was further refined and finalized, data collection occurred at four time points. First, data was collected in December 2019 from eight core service providers who were affiliated with the Youth Services Bureau of Ottawa Lead Agency. Second, data was collected in June and July 2020 from service providers at Woodview Mental Health and Autism Services, while a third set of data was collected from August to September 2020 from Kinark Child and Family Services. Finally, Children’s Mental Health Ontario (CMHO) launched the survey throughout April and May 2021 to interested member agencies following a webinar on staff training initiatives. Ultimately, 66 publicly funded agencies across Ontario participated in the survey.
At the start of the survey, participants were provided with definitions of psychotherapy and mental health problems, consistent with the Regulated Health Professions Act (RHPA, 1991) and the Psychotherapy Act (2007), to establish a common understanding of these terms within the context of this research. Participants also had the opportunity to refer back to these definitions at any point throughout the survey. Psychotherapy was described broadly as interventions, delivered through a psychotherapeutic relationship, that treat an individual’s serious disorder of thought, cognition, mood, emotional regulation, perception or memory that may seriously impair the individual’s judgement, insight, behaviour, communication or social functioning. This could include CBT, counselling, psychodynamic therapy, play therapy, family systems therapy, or parent management training programs. The survey explicitly indicated that Applied Behavioural Analysis and Intensive Behavioural Intervention were not considered psychotherapy. Examples of mental health problems were provided to participants, such as anxiety disorder, bipolar disorder, challenging behaviours (e.g., aggression, irritability), oppositionality, conduct disorders, depression, eating disorders, gender dysphoria, obsessive–compulsive and related disorders, psychosis, post-traumatic stress disorders, or substance use. Neurodevelopmental disorders (e.g., autism, ADHD, learning disabilities, intellectual disability) were explicitly stated not to be regarded as mental health problems.
Measures
Online questionnaires were used to capture information about clinicians’ knowledge, confidence, treatment approaches and adaptations when treating mental health problems in autistic youth or youth with ADHD.Footnote 2
Demographic Information
Participants reported on demographic characteristics, including their age, gender, race/ethnicity, employment and educational training. They also reported on their professional background, including their primary theoretical orientation, the number of clients on their current caseload, their frequency of contact with different client groups, and the number of years they have been in professional practice.
Treatment Approaches
Participants were provided with a list of 19 treatment approaches and an open-ended ‘Other’ option and were asked to select those used when working with clients with mental health problems who also present with autism or ADHD. The list included various treatments such as CBT, emotion focused therapy, acceptance and commitment therapy, family therapy, sensory motor psychotherapy and psychodynamic therapy. Participants were asked to select all treatment approaches that applied and for each selected approach, they were asked: “On average, how helpful do you think each of these treatment approaches is for child/adolescent clients with mental health problems who also present with [autism or ADHD]?” Consistent with Cooper et al. (2018), each approach was rated using a 10-point Likert scale (1 = not at all helpful; 10 = extremely helpful), where higher scores indicate greater perceived helpfulness.
Treatment Adaptations
Participants were provided with a list of 14 adaptations for standard evidence-based interventions that were used in studies of treatment adaptations for CBT for autistic clients (Angus et al., 2014; Burke et al., 2017; Cooper et al., 2018); participants were asked to select any adaptations to psychotherapy that were made in the past for their autistic clients and clients with ADHD. The list included adaptations such as: making abstract concepts more concrete, providing structure and predictability, making use of special interests, and shortening the length of sessions. Participants also rated the helpfulness of each adaptation using a 3-point Likert scale (1 = not at all helpful; 3 = very helpful), such that higher scores indicated higher ratings of helpfulness.
Self-rated Knowledge
To assess participants’ knowledge, they completed a 6-item self-rated knowledge measure developed by Brookman-Frazee et al., (2012a, 2012b, 2012c) and later adapted by Maddox et al. (2019). Participants rated how knowledgeable they were on a series of mental health topics using a 5-point Likert scale (1 = not at all knowledgeable; 5 = extremely knowledgeable), and this was done separately for autistic clients and clients with ADHD. The items included: core symptoms of autism/ADHD, co-occurring problems with autism/ADHD, impact of [autism/ADHD] characteristics on behaviour, developing a treatment plan for a client with autism/ADHD, delivering treatment to a client with autism/ADHD and identifying progress toward treatment goals with a client with autism/ADHD. This measure showed excellent internal consistency across all items when completed in reference to autistic clients (α = 0.95) and clients with ADHD (α = 0.96). A mean self-knowledge score was derived by taking the average of all six items, such that higher mean scores reflected greater self-reported knowledge.
Confidence
Participants completed the Therapist Confidence Scale—Adapted for Autism (TCS-ASD; Cooper et al., 2018), a tool adapted from the original study by Dagnan et al. (2015). The TCS-ASD is a 14-item measure that assesses therapists’ confidence in enacting therapeutic activities that are common across many psychosocial interventions (e.g., developing empathy, communication, assessment, ending therapy). Using a 5-point Likert scale (1 = not confident; 5 = highly confident), participants completed the TCS with reference to autistic clients and those with ADHD. Previous studies have demonstrated the psychometric properties of the TCS and its single factor structure. For instance, Dagnan et al. (2015) showed that the TCS is positively correlated with clinicians’ level of training with individuals with disabilities and possesses good test–retest reliability over a 1 to 3-week period. In the current sample, the TCS exhibited excellent internal consistency when completed about both client groups (autistic clients: α = 0.95; clients with ADHD: α = 0.96). Accordingly, mean TCS scores were calculated by taking the average of all 14 items, such that higher scores reflected greater overall confidence.
Data Analysis
All data was analyzed using the Statistical Package for the Social Sciences (SPSS) version 28. Descriptive statistics were computed for clinician characteristics, treatment approaches, adaptations, confidence, and knowledge in reference to autistic clients and clients with ADHD. Group comparisons were conducted on the three professions with at least 100 participants (i.e., child and youth workers, social workers, and registered psychotherapists) and no significant differences were found in terms of mean confidence and knowledge, helpfulness ratings, and the total number of adaptations used; thus, all professional groups were combined for analysis. Wilcoxon signed-ranks tests were conducted to compare clinicians’ helpfulness ratings for each treatment and adaptation, their self-reported knowledge, and their confidence ratings on the specific items of the TCS-ASD across the two client groups. Separate Bonferroni corrections (α/k) were applied for each set of family-wise comparisons (i.e., approaches, adaptations, knowledge, and confidence). Overall mean scores were compared using paired samples t-tests, and relationships among overall knowledge, confidence, and adaptations were explored using Pearson product moment correlations and the 95% bias-corrected bootstrapped (N = 1000) confidence intervals. Statistical significance was evaluated at the alpha 0.05 level.
Results
Treatment Approaches
As shown in Table 2, CBT was the most frequently endorsed for treating mental health problems in both autistic youth (72.4%) and youth with ADHD (85.3%), followed by solution focused therapy (47.0% for autism and 63.2% for ADHD), family therapy (47.7% for autism and 55.1% for ADHD) and DBT (25.6% for autism and 35.9% for ADHD). For nine out of the 20 treatment approaches examined, Wilcoxon signed-ranks tests indicated that participants rated the interventions as more helpful for clients with ADHD compared to autistic clients (see Table 2; Bonferroni corrected alpha = 0.0025). In considering the most frequently employed interventions, 48.1% of participants rated CBT as helpful to extremely helpful for autistic clients, compared to 69.9% for clients with ADHD. Similarly, for solution focused therapy, 48.4% rated it as helpful to extremely helpful for autistic clients compared to 69.4% for clients with ADHD. For family therapy, 74.8% rated it as helpful to extremely helpful for autistic clients compared to 86.7% for clients with ADHD. Finally, for DBT, 59.2% rated it as helpful to extremely helpful for autistic clients compared to 77.2% for clients with ADHD. A paired samples t-test revealed that overall mean helpfulness ratings across all approaches were significantly lower for autistic clients (M = 6.51, SD = 1.65) compared to clients with ADHD (M = 7.28, SD = 1.32; t (544) = − 11.96, p < 0.001; d = 0.51).
Treatment Adaptations
Participants indicated making similar types of modifications during psychotherapy when working with autistic youth and youth with ADHD (see Table 3). Over 60% of clinicians noted using the following adaptations with both groups of clients: providing structure and predictability, making use of special interests, making abstract concepts more concrete, supporting clients with processing verbal information (e.g., simplifying language), capitalizing on strengths, minimizing sensory distraction, involving family members, and shortening the length of sessions. For the majority of adaptations examined, there were no significant differences in helpfulness ratings between autistic clients and clients with ADHD (all p’s > Bonferroni corrected alpha = 0.003). For three adaptations, however, Wilcoxon signed-ranks tests indicated that helpfulness ratings were significantly higher for clients with ADHD compared to autistic clients (see Table 3): capitalizing on strengths, shortening the length of sessions, and providing opportunities for generalization and ongoing practice. A paired samples t-test indicated that overall mean helpfulness ratings across all adaptations were significantly lower for autistic clients (M = 2.62, SD = 0.29) than for clients with ADHD (M = 2.69, SD = 0.26; t (529) = − 6.52, p < 0.001; d = 0.28). Moreover, a paired samples t-test indicated that a greater number of adaptations were used for clients with ADHD (M = 8.29, SD = 3.00) compared to autistic clients (M = 8.06, SD = 3.10; t (554) = 2.12, p = 0.035; d = 0.09).
Self-rated Knowledge of Psychotherapy Practice
Although clinicians reported considerable knowledge in working with both client groups (see Table 4), for each knowledge item, clinicians rated themselves as significantly less knowledgeable in reference to autistic clients compared to clients with ADHD (Bonferroni corrected alpha = 0.008). More specifically, clinicians were more likely to endorse being not at all or only slightly knowledgeable about the following topics: the core symptoms of autism (20.4% vs. 4.1% for ADHD), co-occurring mental health problems in autistic clients (26.5% vs. 8.1% for ADHD), the impact of autism characteristics on behaviour (17.1% vs. 4.3% for ADHD), treatment planning for autistic clients (37.2% vs. 9.4% for ADHD), delivering mental health treatments to autistic clients (36.8% vs 10.1% for ADHD), and identifying progress among autistic youth (32.7% vs 8.6% for ADHD). A paired samples t-test revealed that clinician’s overall self-rated knowledge was significantly higher for clients with ADHD (M = 3.75, SD = 0.74) than for autistic clients (M = 3.04, SD = 0.85; t (553) = 20.04, p < 0.001), with a large effect size (d = 0.85).
Therapist Confidence in the Delivery of Psychotherapy Activities
As shown in Table 5, confidence ratings were generally high across all items. Nonetheless, clinicians reported feeling significantly less confident in their ability to implement each aspect of psychotherapy when supporting autistic clients compared to those with ADHD. Wilcoxon signed-ranks tests indicated that clinicians were significantly less confident on all 14 items of the TCS-ASD when referencing autistic clients versus clients with ADHD (Bonferroni corrected alpha = 0.0036). For example, clinicians’ confidence in listening to their clients’ concerns was significantly lower when referencing autistic clients (M = 4.17, SD = 0.83) compared to clients with ADHD (M = 4.41, SD = 0.64), z = − 7.52, p < 0.001. Similarly, clinicians were significantly less confident in their ability to be empathetic, communicate with clients, use their knowledge about mental health issues, and effectively end interventions when working with autistic clients versus clients with ADHD. Further, a paired samples t-test indicated that clinicians’ mean confidence levels on the TCS-ASD were significantly higher for clients with ADHD (M = 4.14, SD = 0.62) than for autistic clients (M = 3.55, SD = 0.76; t (554) = 20.99, p < 0.001; d = 0.89).
Bivariate Correlations Among Knowledge, Confidence, and Helpfulness Ratings
For autistic clients, clinicians’ mean knowledge ratings were found to be positively associated with mean confidence ratings (r = 0.73, p < 0.001, 95% CI [0.69, 0.77]), mean helpfulness ratings for all treatment approaches (r = 0.45, p < 0.001, 95% CI [0.38, 0.51]), the number of adaptations implemented (r = 0.31, p < 0.001, 95% CI [0.23, 0.38]), as well as mean helpfulness ratings for all adaptations (r = 0.34, p < 0.001, 95% CI [0.26, 0.41]). Similarly, for clients with ADHD, clinicians’ knowledge ratings were positively associated with mean confidence levels (r = 0.74, p < 0.001, 95% CI [0.70, 0.78]), mean helpfulness rating for all treatment approaches (r = 0.44, p < 0.001, 95% CI [0.37, 0.50]), the number of adaptations implemented (r = 0.35, p < 0.001, 95% CI [0.26, 0.43]), and mean helpfulness ratings for all adaptations (r = 0.35, p < 0.001, 95% CI [0.28, 0.42]).
Discussion
To our knowledge, this study is among the first to assess publicly funded mental health providers’ confidence, knowledge, and use of various therapeutic practices when treating youth with neurodevelopmental conditions and co-occurring mental health challenges. In particular, to identify whether clinician-level barriers to treatment are specific to the autistic community, we compared clinicians’ perceptions, approaches, and use of adaptations among two groups of clients – autistic youth and youth with ADHD. While there is evidence that autistic individuals experience more barriers to care relative to their neurotypical peers (Adams & Young, 2020), this study extends existing work by demonstrating that care provision also varies between youth with different neurodevelopmental conditions. Further, this research contributes to our understanding of community-based practices in a Canadian context, building on established findings regarding adults and CBT (see Maddox et al., 2019) and exploring a wide range of psychotherapeutic techniques used to address young clients’ mental health needs.
Treatment Approaches
Overall, clinicians reported using similar evidence-based interventions when working with autistic clients and clients with ADHD. Specifically, in both groups, CBT was the most common treatment approach, consistent with initial expectations and the extensive literature demonstrating its efficacy among those with disabilities (White et al., 2018). Indeed, studies examining the use of CBT in autism have shown moderate to large improvements in psychiatric symptomatology, such as anxiety and depression (Sukhodolsky et al., 2013; Weiss & Lunsky, 2010; Weston et al., 2016), and across investigations, CBT has been recognized as an effective treatment for co-occurring mental health challenges in those with ADHD (Houghton et al., 2017; Sciberras et al., 2018). The frequent use of CBT in the current sample is promising, as it illustrates progress in bridging the research-to-practice gap. In fact, a number of other established approaches were recognized by clinicians, including solution-focused therapy and family therapy, and here too, the rates of use were similar across both client groups. Although these interventions have not received as much empirical attention in the context of disabilities relative to CBT (Dickson et al., 2021), their utility among neurotypical populations with mental health difficulties is well supported (Bond et al., 2013; Carr, 2019; Schmit et al., 2016; van der Pol et al., 2017). Moreover, the wide use of family therapy among our sample is compatible with studies demonstrating a reciprocal relationship between family distress and child behavioural difficulties (Allen et al., 2010; Baker et al., 2002, 2011), further indicating that clinicians’ approaches are informed by the research base, whether they are treating autistic youth or youth with ADHD.
Despite employing comparable approaches, differences emerged when clinicians were asked to evaluate the perceived helpfulness of their endorsed interventions, often rating their use with autistic clients as less helpful than for clients with ADHD. At the same time, absolute helpfulness ratings were generally high in both client groups, suggesting that clinicians recognize the challenges of working with autistic youth but do not view their efforts as entirely unhelpful or ineffective. Indeed, when investigating providers’ perspectives about supporting autistic children, Brookman-Frazee et al., (2012a, 2012b, 2012c) found that frustration was common, as progress was often slow, rapport was difficult to establish, and care was often uncoordinated. In a similar vein, studies have shown that interventions are not always delivered with the same intensity when working with autistic clients in the community compared to research settings (Brookman-Frazee et al., 2010). The lower ratings observed for autistic clients may reflect the realities of community-based work and clinicians’ recognition of the practical challenges associated with treating this complex group. It may also be that some clinicians believe autistic clients to be less capable of engaging in types of psychotherapy that emphasize cognitive and verbal communication demands (Heidgerken et al., 2005; Maddox et al., 2020), which is consistent with the discrepant ratings we observed for CBT but not interventions with fewer cognitive demands.
Treatment Adaptations
Clinicians reported using several adaptations to address the mental health needs of their clients, and in general, these modifications were comparable in both neurodevelopmental groups. In contrast to previous work showing that therapists typically do not implement specific strategies without autism training (Hurwich-Reiss et al., 2021), most clinicians in our sample reported using adaptations designed to promote client engagement, such as incorporating special interests and providing additional structure within sessions. Similarly, across both neurodevelopmental groups, it was common for clinicians to capitalize on clients’ strengths and facilitate verbal information processing, indicating that they are not only adapting their practice to assist autistic clients, but also applying these strategies more broadly to maximize outcomes for all youth. Accordingly, clinicians viewed many of these adjustments as equally useful among autistic clients and those with ADHD—particularly those aimed at improving client engagement—implying that some adaptations are transdiagnostic rather than autism-specific. Consistent with this notion, previous studies have found that providers trained in mental health interventions for autistic individuals often generalize their skills to assist other client groups (Brookman-Frazee et al., 2012a, 2012b, 2012c). Although extant work has primarily focused on clinicians’ adaptations when delivering CBT (e.g., Cooper et al., 2018; Walters et al., 2016), this study provides novel insights by demonstrating that many of the same, evidence-based adaptations are used when implementing a broad range of therapeutic techniques. Though additional adaptations, such as emotion recognition training and psychoeducation (e.g., Hurwich-Reiss et al., 2021; Kerns et al., 2016), could be incorporated to tailor treatment to autistic clients’ needs, most of the adaptations endorsed are consistent with those identified in the literature (Moree & Davis, 2010; White et al., 2018).
Knowledge and Confidence
In line with initial hypotheses and the broader literature, clinicians reported that they were less knowledgeable about treating co-occurring mental health challenges in autistic youth compared to youth with ADHD. This was true across all knowledge areas assessed, including the symptoms of autism, its impact on mental health presentations and behaviour, ways to plan and deliver treatment to these clients, and how to track their progress. Parents of autistic people have expressed similar concerns about clinicians’ understanding of autism (Brookman-Frazee et al., 2012a, 2012b, 2012c), and past work has indicated that very few mental health providers view themselves as autism specialists (Brookman-Frazee et al., 2012a, 2012b, 2012c). Our findings underscore the need to build clinicians’ knowledge in this area through comprehensive, autism-specific training, which goes beyond introductions to the core features of autism itself and is focused on the application of mental health treatments for this population. Our results mirror those of Maddox et al. (2021), demonstrating that mental health providers working with youth possess similar knowledge gaps as those working with autistic adults. This finding is particularly concerning, as therapists’ limited knowledge was associated with lower helpfulness ratings for various interventions and adaptations and has been noted as a barrier to effective care (Brookman-Frazee et al., 2012a, 2012b, 2012c).
Relatedly, the current study revealed that clinicians were significantly less confident in their ability to effectively treat autistic clients relative to clients with ADHD. This pattern emerged across all items of the TCS-ASD, even when evaluating clinicians’ confidence in using core therapeutic skills (e.g., listening, exhibiting empathy, etc.), suggesting that they feel less confident regardless of the specific stage or component of therapy assessed. Though these findings may be a biproduct of the shared variance across TCS-ASD items, they reinforce qualitative reports indicating that providers are reluctant to treat mental health problems in autistic people (Crane et al., 2019), and they are compatible with previous studies linking self-confidence and knowledge (Crane et al., 2019; Maddox et al., 2021). It may be that the core symptoms of ADHD are more relatable than the sociocommunicative and behavioural expressions of autism since they represent clinically significant forms of common externalizing behaviours that can reflect many underlying causes (e.g., inattention, distractibility, impulsivity, etc.). In turn, this lack of familiarity may impact clinicians’ confidence in delivering treatment to this group. Despite these disparities, it is important to note that clinician confidence levels remained high for both groups. Across most items, average ratings were above the ‘moderately confident’ threshold (i.e., a score of 3) and higher than those reported in previous investigations focusing on autistic clients (Cooper et al., 2018) and clients with intellectual disabilities (Dagnan et al., 2015). In contrast to these earlier investigations, however, the current study did not employ a convenience sample of therapists seeking additional training to adapt their practice for those with developmental disabilities. Thus, the high confidence levels observed herein may be more representative of therapists in general, rather than those who are actively pursuing training in this area. Nonetheless, consistent with past work, clinicians were most confident in using their generic therapeutic skills and were least confident in their ability to select appropriate treatments and assessments for both autistic youth and youth with ADHD. Collectively, these findings shed light on potential areas of improvement and can help to develop autism training programs, which have been found to increase clinicians’ self-confidence and knowledge (Brookman-Frazee et al., 2012a, 2012b, 2012c).
Limitations
Several limitations warrant discussion. First, variables were exclusively assessed through self-report measures, which are susceptible to reporting bias and may not correspond to more objective assessment approaches (e.g., achievement-based tests of knowledge, observations of clinical practices, etc.). For instance, we are unable to determine how clinicians evaluated youth with co-occurring autism and ADHD, given that they were not provided with specific instructions about such clients. Likewise, given that helpfulness ratings were only completed by those who reported using the listed interventions and adaptations in their clinical practice, and clinicians are likely to only employ techniques they perceived to be useful, the variability of these ratings may be restricted, and they may not reflect the perceived therapeutic value of these techniques across the entire sample of clinicians. Nonetheless, the validity of providers’ self-reports is well established. Notable relationships have been demonstrated between providers’ subjective measures of competence and their disability-related experience and training (Cooper et al., 2018; Strike et al., 2004), and self-assessments have shown impressive predictive utility in applied contexts (Maddox et al., 2019). Second, although the survey was piloted among a subset of clinicians prior to its distribution, it should be noted that we did not systematically evaluate the validity and test–retest reliability of all survey measures. Third, the current sample primarily consisted of social workers with cognitive-behavioural orientations to care, which may impact the generalizability of these findings to clinicians with other professional backgrounds and theoretical perspectives. Further, the majority of the participating clinicians identified as women and as White and were situated in the Central and East regions of the province. As such, the reports provided may not be representative of those with different profiles and may not be generalizable to clinicians across Canada and in countries with privately funded care systems. Indeed, while the professional and demographic characteristics of the current sample are similar to those of previous investigations (e.g., Barwick et al., 2008), future work should explore response patterns across different professional groups, geographical areas, and funding systems. It is also important to acknowledge that we did not assess the full range of interventions that are implemented to support pediatric mental health and focused our investigation on the provision of psychotherapy. Accordingly, extensions of this work could evaluate other treatments (e.g., initiatives provided via population health, occupational or school-based supports, psychopharmacological treatments, etc.). Moreover, given that survey recruitment occurred during the pandemic, some agencies declined to participate to avoid adding to staff workloads. Thus, the timing of the survey may have negatively impacted the overall response rate, and those electing to participate may systematically differ from those who declined.
Conclusions
By examining clinicians’ perspectives and practices in community-based settings, this study provides novel insights into the provision of mental health services among Canadian youth with neurodevelopmental conditions. Although many clinicians worked with autistic youth in their clinical practice and confidence and knowledge ratings were relatively high overall, several potential barriers to treatment delivery were identified. Given the demonstrated link between clinician perceptions and treatment intentions (Maddox et al., 2019) and the prevalence of autistic youth requiring mental health care (Joshi et al., 2010), additional capacity-building efforts are needed to improve clinicians’ knowledge and build their self-efficacy. Extensions of this work could monitor how clinician perceptions and practices change as a function of targeted training efforts and explore how these clinician-level factors relate to client outcomes in community settings.
Notes
In this article, we use identity-first language when communicating about autism. It is recognized that differences still exist in terms of how to refer to autism; however, in line with recent literature on this issue (Bottema-Beutel et al., 2021; Kenny et al., 2016), our use of identity-first language is intended to acknowledge, affirm, and validate the ownership of identity for autistic people.
The online survey included several questionnaires by Maddox et al. (2019), which were adapted for this study. For example, measures were adapted by substituting the word “adult” with “child and/or adolescent,” including ADHD versions of questions, and referring to psychotherapy rather than CBT.
References
Adams, D., & Young, K. (2020). A systematic review of the perceived barriers and facilitators to accessing psychological treatment for mental health problems in individuals on the autism spectrum. Review Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s40489-020-00226-7
Adler, L., Shaw, D., Sitt, D., Maya, E., & Morrill, M. I. (2009). Issues in the diagnosis and treatment of adult ADHD by primary care physicians. Primary Psychiatry, 16(5), 57–63.
Allen, J. P., Manning, N., & Meyer, J. (2010). Tightly linked systems: Reciprocal relations between maternal depressive symptoms and maternal reports of adolescent externalizing behavior. Journal of Abnormal Psychology, 119(4), 825–835. https://doi.org/10.1037/a0021081
Angus, B., Monson, K., Fleming, M., Grant, R., Kentmann, C., & Mitchell, J. (2014). Working with young people with autism spectrum disorder and comorbid mental disorders manual. Orygen Youth Health. https://oyh.org.au/sites/oyh.org.au/files/ASD-manual_0.pdf
Baker, B. L., Blacher, J., Crnic, K., & Edelbrock, C. (2002). Behaviour problems and parenting stress in families of three-year-old children with and without developmental delays. American Journal of Mental Retardation, 107(6), 433–444. https://doi.org/10.1352/0895-8017(2002)107%3c0433:BPAPSI%3e2.0.CO;2
Baker, J. K., Seltzer, M. M., & Greenberg, J. S. (2011). Longitudinal effects of adaptability on behavior problems and maternal depression in families of adolescents with autism. Journal of Family Psychology, 25(4), 601–609. https://doi.org/10.1037/a0024409
Barwick, M. A., Boydell, K. M., Stasiulis, E., Ferguson, H. B., Blase, K., & Fixsen, D. (2008). Research utilization among children’s mental health providers. Implementation Science, 3(1), 1–10. https://doi.org/10.1186/1748-5908-3-19
Bond, C., Woods, K., Humphrey, N., Symes, W., & Green, L. (2013). Practitioner review: The effectiveness of solutions focused brief therapy with children and families: A systematic and critical evaluation of the literature from 1990–2010. Journal of Child Psychology and Psychiatry, 54, 707–723. https://doi.org/10.1111/jcpp.12058
Bottema-Beutel, K., Kapp, S. K., Lester, J. N., Sasson, N. J., & Hand, B. N. (2021). Avoiding ableist language: Suggestions for autism researchers. Autism in Adulthood, 3(1), 18–29. https://doi.org/10.1089/aut.2020.0014
Brahmbhatt, K., Hilty, D. M., Hah, M., Han, J., Angkustsiri, K., & Schweitzer, J. B. (2016). Diagnosis and treatment of attention deficit hyperactivity disorder during adolescence in the primary care setting: A concise review. Journal of Adolescent Health, 59(2), 135–143. https://doi.org/10.1016/j.jadohealth.2016.03.025
Brookman-Frazee, L., Baker-Ericze, M., Stadnick, N., & Taylor, R. (2012a). Parent perspectives on community mental health services for children with autism spectrum disorders. Journal of Child and Family Studies, 21(4), 533–544. https://doi.org/10.1007/s10826-011-9506-8
Brookman-Frazee, L. I., Drahota, A., & Stadnick, N. (2012c). Training community mental health therapists to deliver a package of evidence-based practice strategies for school- age children with autism spectrum disorders: A pilot study. Journal of Autism and Developmental Disorders, 42(8), 1651–1661. https://doi.org/10.1007/s10803-011-1406-7
Brookman-Frazee, L., Drahota, A., Stadnick, N., & Palinkas, L. A. (2012b). Therapist perspectives on community mental health services for children with autism spectrum disorders. Administration and Policy in Mental Health, 39(5), 365–373. https://doi.org/10.1007/s10488-011-0355-y
Burke, M., Prendeville, P., & Angela, V. (2017). An evaluation of the ‘FRIENDS for Life’ programme among children presenting with autism spectrum disorder. Educational Psychology in Practice, 33(4), 435–449. https://doi.org/10.1080/02667363.2017.1367648
Cappelli, M., Cloutier, P., Newton, A. S., Fitzpatrick, E., Ali, S., Dong, K. A., Gray, C., Kennedy, A., Lyons, J. S., Polihronis, C., & Rosychuk, R. J. (2019). Evaluating mental health service use during and after emergency department visits in a multisite cohort of Canadian children and youth. Canadian Journal of Emergency Medicine, 21(1), 75–86. https://doi.org/10.1017/cem.2017.416
Carr, A. (2019). Family therapy and systemic interventions for child-focused problems: The current evidence base. Journal of Family Therapy, 41(2), 153–213. https://doi.org/10.1111/1467-6427.12226
College of Registered Psychotherapists of Ontario. (2019). Professional Practice Standards for Registered Psychotherapists. https://www.crpo.ca/wp-content/uploads/2021/07/Professional-Practice-Standards-EN-v-6.0.pdf
Cooper, K., Loades, M. E., & Russell, A. (2018). Adapting psychological therapies for autism. Research in Autism Spectrum Disorders, 45, 43–50. https://doi.org/10.1016/j.rasd.2017.11.002
Crane, L., Adams, F., Harper, G., Welch, J., & Pellicano, E. (2019). ‘Something needs to change’: Mental health experiences of young autistic adults in England. Autism, 23(2), 477–493. https://doi.org/10.1177/1362361318757048
Cuffe, S. P., Moore, C. G., & McKeown, R. (2009). ADHD and health services utilization in the national health interview survey. Journal of Attention Disorders, 12(4), 330–340. https://doi.org/10.1177/1087054708323248
Dagnan, D., Masson, J., Cavagin, A., Thwaites, R., & Hatton, C. (2015). The development of a measure of confidence in delivering therapy to people with intellectual disabilities. Clinical Psychology & Psychotherapy, 22(5), 392–398. https://doi.org/10.1002/cpp.189
Dickson, K. S., Lind, T., Jobin, A., Kinnear, M., Lok, H., & Brookman-Frazee, L. (2021). Correction to: A Systematic Review of Mental Health Interventions for ASD: Characterizing Interventions, Intervention Adaptations, and Implementation Outcomes. Administration and Policy in Mental Health and Mental Health Services Research, 48(5), 884–908. https://doi.org/10.1007/s10488-021-01144-4
Duncan, L., Boyle, M. H., Abelson, J., & Waddell, C. (2018). Measuring children’s mental health in Ontario: Policy issues and prospects for change. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 27(2), 88–98.
French, B., Sayal, K., & Daley, D. (2019). Barriers and facilitators to understanding of ADHD in primary care: A mixed-method systematic review. European Child & Adolescent Psychiatry, 28(8), 1037–1064. https://doi.org/10.1007/s00787-018-1256-3
Hall, C. L., Newell, K., Taylor, J., Sayal, K., Swift, K. D., & Hollis, C. (2013). ‘Mind the gap’-Mapping services for young people with ADHD transitioning from child to adult mental health services. BMC Psychiatry, 13(1), 1–8. https://doi.org/10.1186/1471-244X-13-186
Halldorsdottir, T., & Ollendick, T. H. (2014). Comorbid ADHD: Implications for the treatment of anxiety disorders in children and adolescents. Cognitive and Behavioral Practice, 21(3), 310–322. https://doi.org/10.1016/j.cbpra.2013.08.003
Heidgerken, A. D., Geffken, G., Modi, A., & Frakey, L. (2005). A survey of autism knowledge in a health care setting. Journal of Autism and Developmental Disorders, 35(3), 323–330. https://doi.org/10.1007/s10803-005-3298-x
Hoagwood, K., Kelleher, K. J., Feil, M., & Comer, D. M. (2000). Treatment services for children with ADHD: A national perspective. Journal of the American Academy of Child & Adolescent Psychiatry, 39(2), 198–206. https://doi.org/10.1097/00004583-200002000-00020
Houghton, S., Alsalmi, N., Tan, C., Taylor, M., & Durkin, K. (2017). Treating comorbid anxiety in adolescents with ADHD using a cognitive behavior therapy program approach. Journal of Attention Disorders, 21(13), 1094–1104. https://doi.org/10.1177/1087054712473182
Hurwich-Reiss, E., Chlebowski, C., Lind, T., Martinez, K., Best, K. M., & Brookman-Frazee, L. (2021). Characterizing therapist delivery of evidence-based intervention strategies in publicly funded mental health services for children with autism spectrum disorder: Differentiating practice patterns in usual care and AIM HI delivery. Autism, 25(6), 1709–1720. https://doi.org/10.1177/13623613211001614
Hutchings, J., Pearson-Blunt, R., Pasteur, M. A., Healy, H., & Williams, M. E. (2016). A pilot trial of the Incredible Years® Autism Spectrum and Language Delays Programme. Good Autism Practice (GAP), 17(1), 15–22.
Joshi, G., Petty, C., Wozniak, J., Henin, A., Fried, R., Galdo, M., Kotarski, M., Walls, S., & Biederman, J. (2010). The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: A large comparative study of a psychiatrically referred population. Journal of Autism and Developmental Disorders, 40(11), 1361–1370. https://doi.org/10.1007/s10803-010-0996-9
Kendall, P. C., & Hedtke, K. (2006). Cognitive-behavioral therapy for anxious children: Therapist manual (3rd ed.). Workbook Publishing.
Kenny, L., Hattersley, C., Molins, B., Buckley, C., Povey, C., & Pellicano, E. (2016). Which terms should be used to describe autism? Perspectives from the UK autism community. Autism, 20(4), 442–462. https://doi.org/10.1177/1362361315588200
Kerns, C. M., Roux, A. M., Connell, J. E., & Shattuck, P. T. (2016). Adapting cognitive behavioral techniques to address anxiety and depression in cognitively able emerging adults on the autism spectrum. Cognitive and Behavioral Practice, 23(3), 329–340. https://doi.org/10.1016/j.cbpra.2016.06.002
Lai, M. C., Kassee, C., Besney, R., Bonato, S., Hull, L., Mandy, W., Szatmari, P., & Ameis, S. H. (2019). Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. The Lancet Psychiatry, 6(10), 819–829. https://doi.org/10.1016/S2215-0366(19)30289-5
Larson, K., Russ, S. A., Kahn, R. S., & Halfon, N. (2011). Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics, 127(3), 462–470. https://doi.org/10.1542/peds.2010-0165
Lesesne, C. A., Visser, S. N., & White, C. P. (2003). Attention-deficit/hyperactivity disorder in school-aged children: Association with maternal mental health and use of health care resources. Pediatrics, 111(Supplement_1), 1232–1237. doi: https://doi.org/10.1542/peds.111.S1.1232
Maddox, B., Crabbe, S., Fishman, J., Beidas, R., Brookman-Frazee, L., Miller, J., Nicolaidis, C., & Mandell, D. (2019). Factors influencing the use of cognitive-behavioral therapy with autistic adults: A survey of community mental health clinicians. Journal of Autism and Developmental Disorders, 49, 4421–4428. https://doi.org/10.1007/s10803-019-04156-0
Maddox, B. B., Dickson, K. S., Stadnick, N. A., Mandell, D. S., & Brookman-Frazee, L. (2021). Mental health services for autistic individuals across the lifespan: Recent advances and current gaps. Current Psychiatry Reports, 23(10), 1–9. https://doi.org/10.1007/s11920-021-01278-0
Masse, J. J., McNeil, C. B., Wagner, S., & Quetsch, L. B. (2016). Examining the efficacy of parent–child interaction therapy with children on the autism spectrum. Journal of Child and Family Studies, 25(8), 2508–2525. https://doi.org/10.1007/s10826-016-0424-7
McGillivray, J. A., & Evert, H. T. (2014). Group cognitive behavioural therapy program shows potential in reducing symptoms of depression and stress among young people with ASD. Journal of Autism and Developmental Disorders, 44(8), 2041–2051. https://doi.org/10.1007/s10803-014-2087-9
Miller, A. R., Johnston, C., Klassen, A. F., Fine, S., & Papsdorf, M. (2005). Family physicians’ involvement and self-reported comfort and skill in care of children with behavioral and emotional problems: A population-based survey. BMC Family Practice, 6(1), 1–10. https://doi.org/10.1186/1471-2296-6-12
Moree, B. N., & Davis, T. E., III. (2010). Cognitive-behavioral therapy for anxiety in children diagnosed with autism spectrum disorders: Modification trends. Research in Autism Spectrum Disorders, 4(3), 346–354. https://doi.org/10.1016/j.rasd.2009.10.015
NICE. (2012, June 27). Autism spectrum disorder in adults: Diagnosis and management. Retrieved from www.nice.org.uk/guidance/cg142
Perihan, C., Burke, M., Bowman-Perrott, L., Bicer, A., Gallup, J., Thompson, J., & Sallese, M. (2020). Effects of cognitive behavioral therapy for reducing anxiety in children with high functioning ASD: A systematic review and meta-analysis. Journal of Autism and Developmental Disorders, 50(6), 1958–1972. https://doi.org/10.1007/s10803-019-03949-7
Psychotherapy Act, Statute of Ontario. (2007). c 10. Retrirved from www.ontario.ca/laws/statute/07p10
Regulated Health Professions Act, Statute of Ontario. (1991). c 18. Retrirved from www.ontario.ca/laws/statute/91r18
Schmit, E. L., Schmit, M. K., & Lenz, A. S. (2016). Meta-analysis of solution-focused brief therapy for treating symptoms of internalizing disorders. Counseling Outcome Research and Evaluation, 7(1), 21–39. https://doi.org/10.1177/2150137815623836
Sciberras, E., Mulraney, M., Anderson, V., Rapee, R. M., Nicholson, J. M., Efron, D., Lee, K., Markopoulos, Z., & Hiscock, H. (2018). Managing anxiety in children with ADHD using cognitive-behavioral therapy: A pilot randomized controlled trial. Journal of Attention Disorders, 22(5), 515–520. https://doi.org/10.1177/1087054715584054
Singh, N. N., Lancioni, G. E., Manikam, R., Winton, A. S., Singh, A. N., Singh, J., & Singh, A. D. (2011). A mindfulness-based strategy for self-management of aggressive behavior in adolescents with autism. Research in Autism Spectrum Disorders, 5(3), 1153–1158. https://doi.org/10.1016/j.rasd.2010.12.012
Sofronoff, K., Leslie, A., & Brown, W. (2004). Parent management training and asperger syndrome: A randomized controlled trial to evaluate a parent based intervention. Autism: the International Journal of Research and Practice, 8(3), 301–317. https://doi.org/10.1177/1362361304045215
Strike, D. L., Skovholt, T. M., & Hummel, T. J. (2004). mental health professionals’ disability competence: Measuring self-awareness, perceived knowledge, and perceived skills. Rehabilitation Psychology, 49(4), 321–327. https://doi.org/10.1037/0090-5550.49.4.321
Sukhodolsky, D. G., Bloch, M. H., Panza, K. E., & Reichow, B. (2013). Cognitive-behavioral therapy for anxiety in children with high-functioning autism: A meta-analysis. Pediatrics, 132(5), e1341–e1350. https://doi.org/10.1542/peds.2013-1193
Tellegen, C. L., & Sanders, M. R. (2014). A randomized controlled trial evaluating a brief parenting program with children with autism spectrum disorders. Journal of Consulting and Clinical Psychology, 82(6), 1193–1200. https://doi.org/10.1037/a0037246
Totsika, V., Hastings, R. P., Emerson, E., Lancaster, G. A., & Berridge, D. M. (2011). A population-based investigation of behavioural and emotional problems and maternal mental health: Associations with autism spectrum disorder and intellectual disability. Journal of Child Psychology and Psychiatry, 52(1), 91–99. https://doi.org/10.1111/j.1469-7610.2010.02295.x
van der Pol, T. M., Hoeve, M., Noom, M. J., Stams, G. J. J., Doreleijers, T. A., van Domburgh, L., & Vermeiren, R. R. (2017). Research review: The effectiveness of multidimensional family therapy in treating adolescents with multiple behavior problems–a meta-analysis. Journal of Child Psychology and Psychiatry, 58(5), 532–545. https://doi.org/10.1111/jcpp.12685
Walters, S., Loades, M., & Russell, A. (2016). A systematic review of effective modifications to cognitive behavioural therapy for young people with autism spectrum disorders. Review Journal of Autism and Developmental Disorders, 3(2), 137–153. https://doi.org/10.1007/s40489-016-0072-2
Weiss, J. A., & Lunsky, Y. (2010). Group cognitive behaviour therapy for adults with Asperger syndrome and anxiety or mood disorder: A case series. Clinical Psychology & Psychotherapy, 17(5), 438–446. https://doi.org/10.1002/cpp.694
Weiss, J. A., Thomson, K., Burnham Riosa, P., Albaum, C., Chan, V., Maughan, A., Tablon, P., & Black, K. (2018). A randomized waitlist-controlled trial of cognitive behavior therapy to improve emotion regulation in children with autism. Journal of Child Psychology and Psychiatry, 59(11), 1180–1191. https://doi.org/10.1111/jcpp.12915
Weston, L., Hodgekins, J., & Langdon, P. E. (2016). Effectiveness of cognitive behavioural therapy with people who have autistic spectrum disorders: A systematic review and meta-analysis. Clinical Psychology Review, 49, 41–54. https://doi.org/10.1016/j.cpr.2016.08.001
White, S. W., Simmons, G. L., Gotham, K. O., Conner, C. M., Smith, I. C., Beck, K. B., & Mazefsky, C. A. (2018). Psychosocial treatments targeting anxiety and depression in adolescents and adults on the autism spectrum: Review of the latest research and recommended future directions. Current Psychiatry Reports, 20(10), 1–10. https://doi.org/10.1007/s11920-018-0949-0
Yoshimasu, K., Barbaresi, W. J., Colligan, R. C., Voigt, R. G., Killian, J. M., Weaver, A. L., & Katusic, S. K. (2012). Childhood ADHD is strongly associated with a broad range of psychiatric disorders during adolescence: A population-based birth cohort study. Journal of Child Psychology and Psychiatry, 53(10), 1036–1043. https://doi.org/10.1111/j.1469-7610.2012.02567.x
Acknowledgements
The authors thank the clinicians who participated in this research study.
Funding
The author(s) disclose receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the York University Research Chair in Autism and Neurodevelopmental Disability Mental Health, the LaMarsh Centre for Child and Youth Research, and by Children’s Mental Health Ontario.
Author information
Authors and Affiliations
Contributions
CG helped conduct data analysis, interpret the data, and drafted the manuscript. FR helped design the study survey, collect the data, interpret the data, and write the manuscript. AI conducted data analysis, helped to interpret the data and edited the manuscript. BM aided with survey preparation and edited the manuscript. JW conceived of the study, designed and coordinated the study, collected data, helped interpret the data, and aided in the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Informed Consent
Informed consent was obtained from all individual participants involved in the study.
Research Involving Human and Animal Rights
All procedures performed in our study involving human participants were in accordance with the ethical standards of the York University Office of Research Ethics and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gallant, C., Roudbarani, F., Ibrahim, A. et al. Clinician Knowledge, Confidence, and Treatment Practices in Their Provision of Psychotherapy to Autistic Youth and Youth with ADHD. J Autism Dev Disord 53, 4214–4228 (2023). https://doi.org/10.1007/s10803-022-05722-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05722-9