Abstract
Parents of children with developmental disabilities are susceptible to mental health problems. Mindfulness-based and acceptance and commitment therapy (ACT)-based interventions can improve their mental well-being. This review examined the effectiveness of mindfulness-based and ACT-based interventions in improving mental well-being and mindfulness among parents of children with developmental disabilities. Six electronic databases were searched, resulting in the inclusion of ten studies published between 2014 and 2020. Meta-analysis was conducted using the random-effect model. The results suggest that mindfulness-based and ACT-based interventions were effective in decreasing parental stress, anxiety and depression, however, the effectiveness of these interventions in increasing parental mindfulness was inconclusive. Based on these findings, we discussed considerations for implementing interventions and identified areas which warrant further research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
Developmental disabilities are a group of conditions that impairs one’s physical, learning, language or behavior areas (Rubin and Crocker 1989). They include autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), developmental delay, intellectual or cognitive disabilities, cerebral palsy, hearing losses, vision impairments, and learning disabilities (CDC 2019). They usually manifest during childhood and affect one’s daily functioning ability for a lifetime (Rubin and Crocker 1989). A recent study conducted in the United States showed that the proportion of children diagnosed with a developmental disability increased from 16.2% in 2011 to 17.8% in 2017 (Zablotsky et al., 2019). Globally, the number of people diagnosed with ASD, ADHD and intellectual disabilities increased from 1990s to 2017 (Ritchie 2020). The significant challenges associated with raising a child with a developmental disability cause parents of this group of children to experience higher stress levels and place them at higher risks of developing mental health problems (Carroll 2013; Estes et al. 2012). A previous study found that high levels of depressive symptoms were found in a third of mothers with developmentally disabled children (Singer 2006). Another study conducted on parents of children with complex needs reported that parents struggled significantly more to manage their child’s psychosocial needs instead of their physical limitations, resulting in them becoming mentally drained; an estimated 40% of them show signs of psychiatric distress (Thurston et al. 2011). Due to their poor mental well-being, these parents were also more susceptible to a plethora of physical health problems such as headaches, insomnia, muscle pains, high blood pressure, arthritis and stomach ulcers (Gallagher and Whiteley 2012; Lovell et al. 2012). Poor parental mental and physical health deserve attention because they directly affect children’s health outcomes (Karazsia and Wildman 2009). For instance, children of depressed parents are prone to developing depression themselves and the estimated rates of depression among children of depressed parents range from 20 to 40% (Goodman 2007). Therefore, there is a need to develop and implement interventions that promote mental well-being among parents of children with developmental disabilities.
The first step to improving one’s mental well-being is decreasing one’s stress level (Baum and Posluszny 1999). Stress can be defined as the experience of negative emotions brought about by various physiological, biochemical, cognitive and behavioral changes faced in life (Baum 1990). Chronic stress has shown to result in psychiatric distress, in the forms of anxiety disorders and major depressive disorders (Khan and Khan 2017). Therefore, addressing stress early is of paramount importance, especially for parents of children with developmental disabilities, who are prone to high stress levels. Psychoeducation and cognitive behavioral therapy (CBT) interventions have a longstanding history in stress management. They aim to teach one how to identify his or her source of stress and reduce it. However, evidence has suggested that these methods are not appropriate for reducing the stress of those caring for people with developmental disabilities and can increase their stress levels instead (Devereux et al. 2009; Noone and Hastings 2010). For instance, some parents of children with developmental disabilities who underwent CBT, reported that their daily concerns were dismissed and termed as ‘invalid’, hence adding to their frustrations (Singer et al. 2007). In recent years, researchers have explored the use of mindfulness-based interventions to manage the stress of these parents by educating them to accept their stress instead of removing or controlling their stressors (Lindahl 2015).
Mindfulness can be defined as the state of consciousness that one achieves by purposefully paying attention in each present moment in a non-judgmental manner (Kabat‐Zinn 2003). Practicing mindfulness can improve one’s attention and tolerance for unpleasant thoughts and emotions, hence allowing one to cope with life stressors better (Baer 2003). Mindfulness-based interventions include Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn 1990), Mindfulness-Based Cognitive Therapy (MBCT) (Teasdale et al. 1995) and Acceptance and Commitment Therapy (ACT) (Hayes et al. 1999). MBSR focuses on helping participants to enhance their awareness of the present moment as they undergo guided mindfulness practices that cover many aspects of daily life such as breathing, bodily sensations, movement and eating (Semple and Hatt 2012). It aims to increase one’s general well-being by relieving one’s stress and anxiety that accompanies daily life and chronic illness (Praissman 2008). MBCT combines the mindfulness practices of MBSR with the principles of CBT (Segal and Williams 2001). In addition to helping participants develop a heightened awareness of themselves, MBCT teaches participants to view their personal negative ruminative thoughts and feelings as transient events of their mind rather than unchangeable truths. It also teaches participants to identity their negative thoughts early and disengage from them to prevent themselves from entering a depressive cycle. MBCT was primarily developed to treat clinically depressed patients (Semple and Hatt 2012). On the other hand, ACT combines mindfulness principles with acceptance and behavioral therapies (Hayes and Strosahl 2004). It utilizes the principle of mindfulness to get participants to attain the awareness of their thoughts in the present moment and emotions before teaching them ways to accept and detach from them (Noone and Hastings 2010). ACT also focuses on helping participants to develop psychological flexibility, identify personal values and commitment to make changes (Hayes et al. 1999).
Both mindfulness-based and ACT-based interventions have shown promising results in reducing stress, depression and anxiety across different populations such as pregnant mothers, students and parents of children with special needs (Fung et al. 2018; Petcharat and Liehr 2017; Zhang et al. 2015). This demonstrates their ability to help improve the wellbeing of parents with children who have development disability. Duncan and colleagues theorized that when parents become more mindful, their mental well-being as well as their parenting skills will improve (Duncan et al. 2009). Being more mindful will allow them to have greater emotional awareness and self-regulation, hence improving their mental health. Moreover, learning to view themselves and others in a compassionate and non-judgmental manner will greatly improve their interactions with their children (Duncan et al. 2009). Therefore, mindfulness-based and ACT-based interventions for parents with children with developmental disabilities warrant more scrutiny.
Current Literature
There is limited literature that examined the effectiveness of mindfulness and ACT-based interventions on parental mental well-being. In addition, there are methodological flaws in the available literature. To date, five systematic reviews examined the effectiveness of mindfulness-based interventions (Burgdorf et al. 2019; Hartley et al. 2019; Rayan and Ahmad 2018; Sohmaran and Shorey 2019; Townshend et al. 2016), one systematic review examined the effectiveness of ACT-based interventions (Byrne et al. 2020) and one systematic review examined the effectiveness of both mindfulness-based and ACT-based interventions (Osborn et al. 2020) on the mental well-being of parents. The focus of these reviews were either very narrow, that is, only involving parents of children with ASD (Hartley et al. 2019), or too broad when parents of children from the general population who do not have any clinical conditions as well as children with clinical diagnoses such as depression and developmental disabilities were engaged (Burgdorf et al. 2019; Byrne et al. 2020; Townshend et al. 2016). Three reviews focused on parents of children with developmental disabilities (Osborn et al. 2020; Rayan and Ahmad 2018; Sohmaran and Shorey 2019), while two other reviews conducted secondary analyses on the well-being of parents with developmentally disabled children (Burgdorf et al. 2019; Byrne et al. 2020). Three reviews analyzed the outcomes of parental mental well-being and mindfulness but failed to conduct meta-analyses (Byrne et al. 2020; Osborn et al. 2020; Rayan and Ahmad, 2018), hence compromising the strength of their findings (Impellizzeri and Bizzini, 2012). Burgdorf et al. (2019) conducted meta-analyses for the parental stress outcome but included data from studies without control groups and hence did not isolate the impact of the independent variable such as mindfulness-based interventions on parental stress (Hunter et al. 2016). On the other hand, Sohmaran and Shorey (2019) conducted subgroup analysis to analyze the effect of type of psychological intervention on parental stress. As there was only one study in the mindfulness subgroup, the effectiveness of mindfulness-based interventions on parental stress could not be determined. Therefore, further rigorous reviews are needed to determine the effectiveness of mindfulness-based and ACT-based interventions on improving mental well-being among parents of children with developmental disabilities.
Aim
This review aimed to consolidate evidence on mindfulness-based and ACT-based interventions with respect to stress (primary outcome), anxiety, depression, and mindfulness (secondary outcomes) among parents of children with developmental disabilities. It was hypothesized that mindfulness-based and ACT-based interventions were effective at decreasing parental stress, anxiety and depression, in addition to increasing parental mindfulness at immediate post-intervention and follow-up time points.
Methods
This systematic review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al. 2009). A protocol can be found on PROSPERO (CRD42020191783).
Eligibility Criteria
Population
Parents of children with developmental disabilities were included in this review. In this review, the term ‘parent’ applies to the child’s biological or foster parents, guardians, or caregivers who cared for the child in a parental capacity. A child is anyone up to 19 years of age as defined by the World Health Organization (WHO 2013). Developmental disabilities include ASD, ADHD, developmental delays, intellectual or cognitive disabilities, cerebral palsy, hearing losses, vision impairments and learning disabilities (CDC 2019).
Intervention
Studies that conducted either mindfulness-based or ACT-based interventions or a combination of both that were delivered to parents of children with developmental disabilities with an aim to improve their mental well-being were included. Interventions that were delivered to either both parents and children or parents only were included. Studies that conducted mindfulness-based and/or ACT-based interventions on children only were excluded. Non-mindfulness-based and non-ACT-based interventions were also excluded.
Comparator
Studies with control groups that underwent no intervention, placebo interventions, standard care, or wait-list control were included.
Outcomes
The included studies had to measure self-reported parental stress pre- and post-intervention. Immediate post-intervention levels of parental stress were regarded as the review’s primary outcome. The secondary outcomes were self-reported parental anxiety, depression and mindfulness, and need not be measured by all included studies. Any follow-up measurements for all outcome measures were regarded as secondary outcomes.
Study Design
Only clinical controlled trials (CCTs), randomized controlled trials (RCTs), and cluster RCTs were included.
Language and Publication status
English-only peer-reviewed journal articles or unpublished dissertations were included. Other forms of grey literature, such as conference proceedings, posters, book reviews, abstracts, and brief summaries, were excluded.
Study Selection
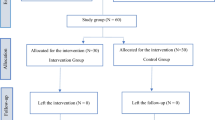
The PRISMA flow diagram guided the study selection process (Moher et al. 2009). Relevant studies were searched from six electronic databases (PubMed, Embase, CINAHL, PsycINFO, Web of Science, and ProQuest) from their respective inception dates to May 2020. The key search terms used were variations of (“child” OR “adolescent” OR “teen” OR “youth”) AND (“parent” OR “father” OR “mother” OR “caregiver” OR “guardian”) AND (“mindfulness” OR “acceptance commitment therapy”) AND (“developmental disorder” OR “autism” OR “asd” OR “adhd” OR “cerebral palsy” OR “intellectual disability” OR “hearing disability” OR “visual disorder” OR “learning disorder”). Variations of (“random” OR “control” OR “assign” OR “allocate” OR “trial” OR “group” OR “volunteer”) were added to the search strategy to select for RCTs and CCTs. The reference lists of relevant reviews and included articles were also examined, and backward searching was conducted to find additional relevant studies. When the full texts of potential studies were not available, their authors were contacted to obtain the papers. All search results were exported to Endnote Version X8 (Clarivate Analytics 2019), where they were categorized according to their databases and had their duplicates removed. All studies had their titles and abstracts screened against the eligibility criteria. Then, the full texts of selected studies were further analyzed to decide their inclusion statuses. This study selection process was conducted independently by two reviewers, and discussions were held to resolve any discrepancies that arose.
Data Extraction
A data extraction form was used to extract pertinent characteristics related to the study’s sample, design, data management, outcomes measured, intervention duration, format and delivery method. The mean and standard deviation values of the review’s primary and secondary outcomes were extracted. When these specific values were not provided, existing data were transformed using relevant formulas to obtain the values (Higgins and Green 2011). This process was performed independently by two reviewers and disagreements were resolved via discussions.
Quality Appraisal
The Cochrane’s risk of bias tool was used to evaluate risk of bias at the study level. Five types of biases in seven domains were examined: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other sources of bias (Higgins and Green 2011). Each domain was graded a ‘low’ or ‘high’ risk depending on each study’s details and an ‘unclear’ risk was given when inadequate details were available. Overall bias rating was determined by the worst score that each study received for any domain (Kempler et al. 2016). As a minimum of ten studies in a forest plot was recommended to produce a meaningful funnel plot to analyze publication bias, publication bias was not assessed in this review because there was no forest plot with at least ten studies (Sterne et al. 2011).
The quality of the overall body of evidence at the outcome level was rated as high, moderate, low, or very low according to the GRADE approach. All outcomes were initially rated as high quality, but this rating was dropped when any of the five following factors were compromised: risk of bias of individual studies, inconsistency, directness of evidence, precision of effect estimates, and publication bias (Higgins and Green 2011). All outcomes were rated separately using the online GRADEpro software (GRADEpro 2015). Both reviewers conducted the quality appraisal process independently and disagreements were resolved via discussions.
Data Synthesis
The characteristics of the included studies and the interventions were summarized narratively. Meta-analyses were conducted to pool data with the same outcomes using Review Manager 5.3 (RevMan 5.3, The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) under the random-effect model. As the included studies used different scales to measure each outcome, standardized mean differences (SMD) and 95% confidence intervals (CI) were used as the effect measure under the inverse-variance method (Higgins and Green 2011). Effect sizes were defined as very small, small, medium, large, very large, and huge according to their values of 0.1, 0.2, 0.5, 0.8, 1.2, and 2.0, respectively (Sawilowsky 2009). However, as two distinct outcomes of mindfulness were reported in the included studies (interpersonal mindfulness in parenting and parental mindfulness awareness), separate meta-analyses were conducted for each.
The heterogeneity of the results was assessed using the I2 statistics and Cochran Q chi-squared test. As per Cochrane hand book (Higgins and Green 2011), the I2 values were interpreted as low importance (≤ 40%), moderate (30–60%), substantial (50–90%), and considerable (75–100%). For the chi-squared test, statistically significant heterogeneity was identified when its corresponding p-value was less than 0.10 (Higgins and Green 2011). Subgroup analyses were conducted to reduce heterogeneity levels and analyze the effect of certain variables on the outcomes investigated (Higgins and Green 2011; Sedgwick 2014). The variables analyzed were type of intervention, geographical distribution of study, and intervention duration. One study that only used the distress subscale of the Parenting Stress Index–Short Form to measure parental stress levels, unlike the other included studies that measured total parental stress, was narratively synthesized (Neece 2014). Hilkey (2019) was also narratively synthesized and it was an unreviewed master’s dissertation with exceptionally low number of participants (three in intervention group; two in control group).
Results
Search Outcomes
A total of 1,753 articles were found from the six listed electronic databases and relevant reference lists. After removing 561 duplicates and excluding 1,101 articles based on their titles and abstracts, 91 articles were left for full-text screening. The full-text screening excluded another 81 articles, leaving ten relevant articles to be included in this review. Seven were peer-reviewed primary studies (Behbahani et al. 2018; Corti et al. 2018; Lo et al. 2017, 2020; Neece 2014; Rayan and Ahmad 2017; Whittingham et al. 2016), while three were unpublished dissertations (Hilkey 2019; Petcharat 2018; Zody 2018). Figure 1 details the PRISMA flow diagram.
Characteristics of the Included Studies
The ten included studies were conducted in seven different countries—Iran (n = 1), Jordan (n = 1), Hong Kong (n = 2), Thailand (n = 1), Italy (n = 1), Australia (n = 1), and the United States of America (n = 3)—that collectively analyzed 614 parents of children with developmental disabilities. Seven studies focused on parents of children with specific conditions—ADHD (n = 2), autism or ASD (n = 4), and cerebral palsy (n = 1)—while three studies recruited parents of children with a mixture of ASD, ADHD, and other developmental disabilities such as developmental delays and intellectual disabilities (Lo et al. 2017; Neece 2014; Petcharat 2018). There were seven RCTs and three CCTs. Four studies conducted ACT-based interventions, while the rest conducted mindfulness-based interventions (Corti et al. 2018; Hilkey 2019; Whittingham et al. 2016; Zody 2018). No study conducted a combination of mindfulness-based and ACT-based interventions. Nine studies conducted face-to-face group-based interventions that utilized interactive teaching methods (group discussions, mindfulness exercises, and activity worksheets), with two studies adopting mixed methods such as phone call consultations in addition to the face-to-face group sessions to deliver the intervention (Rayan and Ahmad 2017; Whittingham et al. 2016). One study designed an interactive online course for its participants to complete the course independently (Hilkey 2019). The summary of included studies is presented in Table 1.
Quality Appraisal (Study Level)
The Cochrane risk of bias tool was used to assess the risks of bias for all included trials. The overall bias was rated as unclear for two studies and high for the remaining studies (Hilkey 2019; Lo et al. 2017). Inter-rater agreement among both reviewers was approximately 97%, and the Cohen’s kappa value was 0.95. The risk of bias summary is shown in Online Resource 1, Fig. S1.
Parental Stress Scores at Immediate Post-Intervention
A meta-analysis was conducted for the eight studies that assessed parental stress immediately post-intervention (Behbahani et al. 2018; Corti et al. 2018; Lo et al. 2017, 2020; Petcharat 2018; Rayan and Ahmad 2017; Whittingham et al. 2016; Zody 2018). It showed a statistically significant medium effect among 563 participants, favoring the intervention group (SMD = − 0.50, 95% CI: − 0.88 to − 0.11, Z = 2.51, p = 0.01), with significant substantial statistical heterogeneity (I2 = 77%, p < 0.0001) (Fig. 2a).
Parental stress was not affected by intervention type and intervention duration as the subgroup analyses for these factors revealed statistically non-significant subgroup differences (p ≥ 0.05) (Online Resource 1, Fig. S2.1 and S2.3).
A subgroup analysis according to geographical distribution showed statistically significant subgroup differences (I2 = 91.1%, p < 0.0001) and reduced heterogeneity to low levels for the Middle Eastern countries subgroup (I2 = 12%, p = 0.29), the Western countries subgroup (I2 = 22%, p = 0.28), and the Asian countries subgroup (I2 = 0%, p = 0.48). The Middle Eastern countries subgroup had a statistically significant very large effect, while the Western countries subgroup had a statistically significant small effect and the Asian countries subgroup had a statistically non-significant very small effect (Online Resource 1, Fig. S2.2).
Parental Anxiety Scores at Immediate Post-Intervention
A meta-analysis was conducted for the four studies that assessed parental anxiety immediately post-intervention (Petcharat 2018; Rayan and Ahmad 2017; Whittingham et al. 2016; Zody 2018). It showed a statistically significant medium effect among 185 participants, favoring the intervention group (SMD = − 0.63, 95% CI: − 0.93 to − 0.34, Z = 4.17, p < 0.0001), with low statistical heterogeneity (I2 = 0%, p = 0.52) (Fig. 2b).
Parental anxiety was not affected by intervention type, geographical distribution and intervention duration as the subgroup analyses for these factors revealed statistically non-significant subgroup differences (p ≥ 0.05) (Online Resource 1, Fig. S3.1, S3.2, and S3.3).
Parental Depression Scores at Immediate Post-Intervention
A meta-analysis was conducted for the five studies that assessed parental depression immediately post-intervention (Lo et al. 2017; Neece 2014; Rayan and Ahmad 2017; Whittingham et al. 2016; Zody 2018). It showed a statistically significant medium effect among 389 participants, favoring the intervention group (SMD = − 0.72, 95% CI: − 1.34 to − 0.10, Z = 2.26, p = 0.02), with significant substantial to considerable statistical heterogeneity (I2 = 86%, p < 0.0001) (Fig. 2c).
Parental depression was not affected by intervention type and intervention duration as the subgroup analyses for these factors revealed statistically non-significant subgroup differences (p ≥ 0.05) (Online Resource 1, Fig. S4.1 and S4.3).
A subgroup analysis according to geographical distribution showed statistically significant subgroup differences (I2 = 92.6%, p < 0.00001) and reduced heterogeneity to low levels for the Western countries subgroup (I2 = 0%, p = 0.71), while the Middle Eastern countries subgroup and the Asian countries subgroup only had one study each hence heterogeneity levels could not be measured. The Western countries subgroup had a statistically significant medium effect, while the Middle Eastern countries subgroup had a statistically significant very large effect and the Asian countries subgroup had a statistically non-significant very small effect (Online Resource 1, Fig. S4.2).
Parental Mindfulness
There are two aspects of parental mindfulness covered by the studies in this review: interpersonal mindfulness in parenting and parental mindfulness awareness. Interpersonal mindfulness in parenting measures the degree of mindfulness parents show when interacting with their children (de Bruin et al. 2014). Conversely, mindfulness awareness measures one’s overall ability to be aware of each present moment, which is non-specific to parenting (Brown and Ryan 2003).
Interpersonal Mindfulness in Parenting Scores at Immediate Post-Intervention
A meta-analysis was conducted for the two studies that assessed interpersonal mindfulness in parenting immediately post-intervention (Lo et al. 2017, 2020). It showed a statistically non-significant negligible effect among 280 participants, favoring the intervention group (SMD = 0.01, 95% CI: − 0.23 to 0.24, Z = 0.06, p = 0.96), with low statistical heterogeneity (I2 = 0%, p = 0.91) (Online Resource 1, Fig. S5.1). No subgroup analyses were conducted for this outcome.
Parental Mindfulness Awareness Scores at Immediate Post-Intervention
A meta-analysis was conducted for the two studies that assessed parental mindfulness awareness post-intervention (Corti et al. 2018; Petcharat 2018). It showed a statistically non-significant small effect among 64 participants, favoring the control group (SMD = − 0.33, 95% CI: − 1.67 to 1.00, Z = 0.49, p = 0.62), with statistically significant substantial to considerable statistical heterogeneity (I2 = 84%, p = 0.01) (Online Resource 1, Fig. S5.2). No subgroup analyses were conducted for this outcome.
Quality Appraisal (Outcome Level)
The GRADE approach was used to conduct quality appraisal at the outcome level. The following outcomes were rated as very low quality: (1) parental stress, (2) parental anxiety, (3) parental depression, and (4) parental mindfulness awareness. The outcome of interpersonal mindfulness in parenting was rated high quality. The GRADE summary of evidence is presented in Online Resource 2, Table S1.
Narrative Synthesis
Only one study used the parental distress subscale of the Parenting Stress Index–Short Form to measure parental stress levels, unlike the other included studies that measured total parental stress, and was hence excluded from the meta-analyses (Neece 2014). At post-intervention, the intervention group reported statistically significantly lower stress levels compared to those of the control group. A medium effect size of 0.70 was reported. Hilkey (2019) was also excluded from meta-analyses as it was an unreviewed master’s dissertation and had an exceptionally low number of participants. The study reported a statistically non-significant very small effect of 0.17, favoring the control group at post-intervention (Hilkey 2019).
Only four studies conducted follow-up measurements at various timepoints (Behbahani et al. 2018; Petcharat 2018; Whittingham et al. 2016; Zody 2018). However, three out of four did not provide follow-up data for the control group, hence meta-analyses could not be conducted (Petcharat 2018; Whittingham et al. 2016; Zody 2018). Petcharat (2018) reported that the intervention group did not show any statistically significant increase in stress and anxiety scores, or decrease in mindfulness awareness scores at the two-week follow-up compared to post-intervention. Both Whittingham et al. (2016) and Zody (2018) reported that their respective intervention groups did not show any statistically significant increase in stress, anxiety, and depression scores at the six-month and the three-month follow-up respectively, compared to post-intervention. As for Behbehani et al. (2018), the parental stress scores of the intervention group at the eight-week follow-up were statistically significantly lower than those of the control group.
Discussion
This review examined the effect of mindfulness-based and ACT-based interventions on improving stress, anxiety, depression and mindfulness among parents of children with developmental disabilities. The results from the meta-analyses showed that both mindfulness-based and ACT-based interventions were effective in decreasing stress, anxiety and depression among parents of children with developmental disabilities. This shows that promoting mindfulness among parents of children with developmental disabilities can help to improve their mental well-being. Similar results have been reported by previous reviews that analyzed the effect of mindfulness-based interventions on stress among parents of children with developmental disabilities (Burgdorf et al. 2019; Rayan and Ahmad 2018). However, the current review did not show significant improvement for both outcomes of parental mindfulness (interpersonal mindfulness in parenting and parental mindfulness awareness) post-intervention. The findings from this study differed from those reported by Rayan and Ahmad (2018) which reported improvements in parental mindfulness at post-intervention for five out of six trials. As Rayan and Ahmad (2018) did not conduct meta-analysis and analyzed data from trials without control groups, direct comparisons could not be drawn. This review’s lack of improvement in mindfulness scores could have been contributed by the participants’ initial self-reporting of higher mindfulness scores due to social desirability bias; they could have realized their own limitations at post-intervention and were more likely to rate themselves honestly (Coatsworth et al. 2015). Moreover, their inadequate understanding of mindfulness pre-intervention could have resulted in them scoring themselves higher. After undergoing the intervention, they would have acquired a better understanding of mindfulness and hence scored themselves more accurately (Coatsworth et al. 2015). Both factors could account for the lower scores of mindfulness reported by the intervention groups post-intervention.
Another previous study suggested that the lower post-intervention mindfulness scores demonstrated an increase in psychological awareness brought about by the intervention, and indicated the possibility of improvements in the future (Corti et al. 2018). This is further substantiated by other studies which reported marked improvement in mindfulness scores at follow-up timepoints only (Gould et al. 2018; Kohtala et al. 2017). As only four included studies measured parental mindfulness, conclusive findings could not be provided in this review. Hence, future trials should make it a point to assess mindfulness scores at immediate post-intervention and follow-up timepoints to better examine the effectiveness of mindfulness-based and ACT-based interventions in improving parental mindfulness. However, there is a possibility that mindfulness-based and ACT-based interventions might not increase parental mindfulness among parents of children with development disabilities. Since almost all the studies conducted group-based interventions, the parents might have reported improvement in mental well-being post-intervention due to the social support that they received by being in contact with other parents who were facing similar parenting challenges (Zody 2018). Future studies could conduct comparison trials between group-based versus individual-based mindfulness-based and ACT-based interventions to further examine the influence of social support on parents’ mental well-being and mindfulness.
The results showed no significant difference in parental stress, anxiety, and depression between the scores of mindfulness-based and ACT-based subgroups, indicating that both types of interventions might be similarly effective in promoting mental well-being among parents of children with developmental disabilities. This could be due to the same mindfulness principle used in both types of interventions. These interventions also encouraged their participants to adopt the coping approach to deal with stress, which has been advised as suitable for prolonged stressors such as caring for a developmentally disabled child for an extended period of time (Mullen and Suls 1982). However, this review’s analysis was limited to only the immediate post-intervention timepoint due to a lack of follow-up data for most studies. Hence, further research, especially those related to follow-up assessments, should be conducted to explore the differences between the effectiveness of mindfulness-based interventions and ACT-based interventions on short-term and long-term parental mental well-being.
Evidence suggests that the studies conducted in the Middle Eastern countries were more effective in reducing parental stress, anxiety and depression compared to studies conducted in Western and Asian countries. Although subgroup analyses according to geographical location for parental anxiety showed non-significant subgroup differences, the Middle Eastern countries subgroup reported a statistically significant large effect while the Western countries and Asian countries subgroups reported statistically non-significant results. Studies conducted in the Middle Eastern countries could have reported greater improvements in parental mental well-being because the Muslim participants were able to integrate mindfulness practices into their daily lives more easily. A previous mindfulness-based program conducted on Muslim women discovered that the participants were able to spontaneously make connections between mindfulness practices and their own religious practices such as daily prayers (Thomas et al. 2016). As an estimated 99% of Iranians and 92% of Jordanians are Muslims (The Embassy of the Hashemite Kingdom of Jordan 2020; World Population Review 2020), the participants of the studies conducted in the Middle Eastern countries may have been more receptive to adopt mindfulness practices as part of their daily routine because these practices strongly resemble those of their own religious practices. The participants of the included study in this review (Rayan and Ahmad 2017) could have found it even easier as their mindfulness program included elements from Islamic teachings. In an another study, a depressed Christian client who underwent mindfulness-based therapy said that the non-judgmental and self-compassionate principles of mindfulness reflected God’s nature and that this connection helped her to recover from depression better (Hathaway and Tan 2009). Mindfulness and ACT also share similar links of self-compassion and acceptance with the principles of Buddhism (Santiago and Gall 2016; Semple and Hatt, 2012). A previous study that integrated Buddhist teachings in an ACT program for patients with chronic major mood and anxiety disorders reported positive changes in patients’ conditions, and one patient even remitted shortly after the program (Fung 2015). Therefore, mindfulness practices can become more meaningful when participants link them to their own religious and spiritual beliefs.
A subgroup analysis on intervention duration (one day, up to one month, between one to three months, and longer than three months) showed no significant differences (based on the duration) between the effectiveness of mindfulness-based and ACT-based interventions on parental stress, anxiety, and depression. However, significant improvements in parental stress, anxiety and depression were reported for the ‘up to one month’ category, while the other intervention duration categories reported non-significant results. This is in contrast with a previous review that reported no relationship between the duration of the mindfulness-based intervention and parenting stress (Burgdorf et al. 2019). However, as the review analyzed parents of children with and without clinical diagnoses such as depression and developmental disabilities, direct comparisons could not be drawn (Burgdorf et al. 2019). Recent studies have reported that for mindfulness practices to bring about optimum mental health benefits, they need to be conducted regularly (Chiam et al. 2020; Seabrook et al. 2020). However, longer interventions have also been found to be ineffective due to problems such as poor attendance rates. An increase in attrition rate from around 9% at immediate post-intervention timepoint to over 50% at the six-month follow-up for the intervention group was observed in one of the included studies which conducted the longest follow-up time period (Whittingham et al. 2016). This can be especially problematic for this group of parents as childcare arrangements for children with developmental disabilities may be harder to make due to their children’s challenging behavioral problems (Beer et al. 2013; Lloyd and Hastings 2009). Hence, parents may not be able to attend multiple intervention sessions due to the lack of available childcare. Specialized schools catering to children with developmental disabilities can help with the childcare issue by engaging experienced mindfulness and ACT trainers to conduct such programs for parents of special needs children at their schools while their children are attending lessons. Therefore, future intervention programs can consider multiple sessions up to one month long to instill the notion of regular mindfulness practice as well as organize intervention programs when children are engaged at school to avoid attendance issues due to difficult childcare arrangements.
Limitations
This review has limitations. Only trials and dissertations published in English were included, which may pose potential publication bias. All studies utilized the self-report method to assess the outcomes of parental mental well-being and mindfulness, and this can result in risks of social desirability bias. Seven out of the ten included studies had small sample sizes, and this may have compromised the results’ reliability and validity. Due to the limited number of overall included studies (only 10 included studies and eight included in meta-analysis), and the fact that not all studies assessed outcomes of parental stress, anxiety and depression, some subgroup analysis ended up having only one or two studies in each subgroup. This could potentially affect the results’ reliability and validity. Only four studies conducted follow-up assessments, and only one out of the four conducted follow-up assessments on both the intervention and control groups, limiting the review’s ability to examine the durability of the intervention effects. Although a subgroup analysis according to geographical distribution was conducted, subgroup analyses based on ethnicity and religion could not be conducted as each trial was conducted on a mixture of ethnic groups and religions. Hence, the variables of ethnicity and religion were not explored. Future research should consider examining these variables. Baseline disparities between the intervention and control groups were not considered in this review as only endpoint data were extracted for meta-analyses instead of mean differences. Four out of five outcomes were rated as very low quality via the GRADE approach, indicating that the true effect size is likely to be significantly different from this review’s effect size estimates. Lastly, this review could not examine the effect of children’s age or type of developmental disability on parental mental well-being and mindfulness due to the wide age range of the children included in the studies and their different developmental disabilities. As evidence suggests that parents’ stress levels are affected by their child’s age and type of developmental disability, future research should seek to explore these variables (DePape and Lindsay 2015). All these limitations may limit the accuracy of this review’s findings.
Implications for Future Practice and Research
Clinical psychologists and psychiatrists who conduct regular medical reviews for children with development disabilities can adopt family-focused approaches and offer mindfulness-based and ACT-based therapies to improve these parents’ mental well-being. The use of technology can be explored as an additional mode of intervention delivery to maximize attendance rates. Various types of technology, such as web-based and virtual reality, have been proven to be effective in delivering mindfulness-based interventions (Seabrook et al. 2020; Sevilla-Llewellyn-Jones et al. 2018), and future trials can consider using technology to support parents. In light of the current COVID-19 pandemic situation where anxiety is heightened and daily schedules are disrupted, technology-based interventions should be developed and implemented for parents of children with developmental disabilities to access at home. An example would be a web-based pandemic mental health intervention offering different modules for participants to select those applicable to their current situation (Arnold et al. 2020). A similar mindfulness-based and ACT-based intervention could also be developed to help parents during this difficult pandemic period.
Specialized schools that cater to children with developmental disabilities can also engage experienced mindfulness and ACT trainers to organize such programs for these children’s parents. Conducting such programs for parents while their children attend school activities could encourage more parents to participate in these programs. Moreover, healthcare providers, community workers and researchers can collaborate with religious leaders to modify current mindfulness-based and ACT-based programs to incorporate various religious teachings within these interventions. Future trials can develop interventions in which participants are grouped according to their religions for some segments and the respective religious leaders can be invited to deliver certain aspects of the interventions. For instance, a monk was engaged by a psychiatrist to conduct Buddhist teachings as part of a hybrid ACT program, and the participants both enjoyed and benefitted from his teachings (Fung 2015). This may help to make mindfulness-based practices more meaningful and relatable for parents of children with developmental disabilities, and allow them to integrate these practices in their daily lives more seamlessly, hence bringing about greater improvements to their mental well-being.
Furthermore, future trials should aim to recruit larger sample sizes and across more regions such as in Africa and South America to understand the mental well-being of parents with children who have development disability in other cultures. They should also aim to conduct follow-up assessments of at least six months to assess the long-term effects of these interventions as a previous study only reported marked improvements in mindfulness at the six months’ time point (Gould et al. 2018). Due to the very low quality of almost all of the review outcomes, future research should examine outcomes of parental stress, anxiety, depression and mindfulness (interpersonal mindfulness in parenting and mindfulness awareness) to validate this review’s findings.
Conclusion
In this review, mindfulness-based and ACT-based interventions were found to be effective in improving mental well-being in terms of stress, anxiety and depression among parents of children with developmental disabilities at post-intervention. However, these interventions were not effective in improving parental mindfulness post-intervention. The effectiveness of these interventions at their follow-up timepoints cannot be adequately determined due to insufficient data. The findings of this review suggest that mindfulness-based and ACT-based interventions can be considered by healthcare professionals, community workers and authorities from specialized schools for children with development disability to support parents of children with special needs. Future trials can also leverage on technology to deliver mindfulness-based and ACT-based interventions to boost attendance rates and offer support to parents during the current stressful pandemic situation. Moreover, religious leaders can be engaged to incorporate various religious teachings into existing mindfulness-based and ACT-based interventions to offer more meaningful mindfulness practices for participants. Considering the very low quality of evidence, as rated using the GRADE approach for almost all outcomes, future reviews are needed to corroborate current findings.
References
Arnold, T., Rogers, B. G., Norris, A. L., Scherr, A. S., Haubrick, K., Renna, M. E., et al. (2020). A brief transdiagnostic pandemic mental health maintenance intervention. Counselling Psychology Quarterly. https://doi.org/10.1080/09515070.2020.1769026.
Baer, R. A. (2003). Mindfulness Training as a Clinical Intervention: A Conceptual and Empirical Review. Clinical Psychology: Science and Practice, 10(2), 125–143. https://doi.org/10.1093/clipsy.bpg015.
Baum, A. (1990). Stress, intrusive imagery, and chronic distress. Health Psychology, 9(6), 653–675. https://doi.org/10.1037/0278-6133.9.6.653.
Baum, A., & Posluszny, D. M. (1999). Health psychology: mapping biobehavioral contributions to health and illness. Annual review of psychology, 50(1), 137–163. https://doi.org/10.1146/annurev.psych.50.1.137.
Beer, M., Ward, L., & Moar, K. (2013). The Relationship Between Mindful Parenting and Distress in Parents of Children with an Autism Spectrum Disorder. Mindfulness (N Y), 4(2), 102–112. https://doi.org/10.1007/s12671-012-0192-4.
Behbahani, M., Zargar, F., Assarian, F., & Akbari, H. (2018). Effects of mindful parenting training on clinical symptoms in children with attention deficit hyperactivity disorder and parenting stress: Randomized controlled trial. Iran J Med Sci, 43(6), 596–604.
Brown, K. W., & Ryan, R. M. (2003). The Benefits of Being Present: Mindfulness and Its Role in Psychological Well-Being. Journal of Personality and Social Psychology, 84(4), 822–848. https://doi.org/10.1037/0022-3514.84.4.822.
Burgdorf, V., Szabó, M., & Abbott, M. J. (2019). The Effect of Mindfulness Interventions for Parents on Parenting Stress and Youth Psychological Outcomes: A Systematic Review and Meta-Analysis. Front Psychol, 10, 1336. https://doi.org/10.3389/fpsyg.2019.01336.
Byrne, G., Ghráda, Á. N., O’Mahony, T., & Brennan, E. (2020). A systematic review of the use of acceptance and commitment therapy in supporting parents. Psychology and Psychotherapy: Theory, Research and Practice. https://doi.org/10.1111/papt.12282.
Clarivate Analytics (2019). EndNote X8. Available from: https://endnote.com/.
Carroll, D. W. (2013). Families of children with developmental disabilities: understanding stress and opportunities for growth. American Psychological Association.
Centres for Disease Control and Prevention, (2019). Facts about Developmental Disabilities. Centres for Disease Control and Prevention. https://www.cdc.gov/ncbddd/developmentaldisabilities/facts.html Accessed 20 May, 2020.
Chiam, E. Y. X., Lopez, V., & Klainin-Yobas, P. (2020). Perception on the mind-nurse program among nursing students: A descriptive qualitative study. Nurse Education Today. https://doi.org/10.1016/j.nedt.2020.104492.
Coatsworth, J. D., Duncan, L. G., Nix, R. L., Greenberg, M. T., Gayles, J. G., Bamberger, K. T., et al. (2015). Integrating mindfulness with parent training: effects of the Mindfulness-Enhanced Strengthening Families Program. Developmental Psychology, 51(1), 26–35. https://doi.org/10.1037/a0038212.
Corti, C., Pergolizzi, F., Vanzin, L., Cargasacchi, G., Villa, L., Pozzi, M., & Molteni, M. (2018). Acceptance and commitment therapy-oriented parent-training for parents of children with autism [Psychotherapy & Psychotherapeutic Counseling 3310]. Journal of Child and Family Studies, 27(9), 2887–2900. https://doi.org/10.1007/s10826-018-1123-3.
de Bruin, E. I., Zijlstra, B. J. H., Geurtzen, N., van Zundert, R. M. P., van de Weijer-Bergsma, E., Hartman, E. E., et al. (2014). Mindful Parenting Assessed Further: Psychometric Properties of the Dutch Version of the Interpersonal Mindfulness in Parenting Scale (IM-P). Mindfulness (N Y), 5(2), 200–212. https://doi.org/10.1007/s12671-012-0168-4.
DePape, A. M., & Lindsay, S. (2015). Parents’ experiences of caring for a child with autism spectrum disorder. Qualitative Health Research, 25(4), 569–583. https://doi.org/10.1177/1049732314552455.
Devereux, J., Hastings, R., & Noone, S. (2009). Staff Stress and Burnout in Intellectual Disability Services: Work Stress Theory and its Application. Journal of Applied Research in Intellectual Disabilities, 22(6), 561–573. https://doi.org/10.1111/j.1468-3148.2009.00509.x.
Duncan, L. G., Coatsworth, J. D., & Greenberg, M. T. (2009). A model of mindful parenting: implications for parent-child relationships and prevention research. Clinical Child and Family Psychology Review, 12(3), 255–270. https://doi.org/10.1007/s10567-009-0046-3.
Estes, A., Olson, E., Sullivan, K., Greenson, J., Winter, J., Dawson, G., & Munson, J. (2012). Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain & Development, 35(2), 133–138. https://doi.org/10.1016/j.braindev.2012.10.004.
Fung, K. (2015). Acceptance and Commitment Therapy: Western adoption of Buddhist tenets? Transcult Psychiatry, 52(4), 561–576. https://doi.org/10.1177/1363461514537544.
Fung, K., Lake, J., Steel, L., Bryce, K., & Lunsky, Y. (2018). ACT Processes in Group Intervention for Mothers of Children with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 48(8), 2740–2747. https://doi.org/10.1007/s10803-018-3525-x.
Gallagher, S., & Whiteley, J. (2012). Social support is associated with blood pressure responses in parents caring for children with developmental disabilities. Research in Developmental Disabilities, 33(6), 2099–2105. https://doi.org/10.1016/j.ridd.2012.06.007.
Goodman, S. H. (2007). Depression in mothers. Annual review of clinical psychology, 3(1), 107–135. https://doi.org/10.1146/annurev.clinpsy.3.022806.091401.
Gould, E. R., Tarbox, J., & Coyne, L. (2018). Evaluating the effects of Acceptance and Commitment Training on the overt behavior of parents of children with autism. Journal of Contextual Behavioral Science, 7, 81–88. https://doi.org/10.1016/j.jcbs.2017.06.003.
GRADEpro. (2015). GRADEpro. https://gradepro.org Accessed 9 June, 2020.
Hartley, M., Dorstyn, D., & Due, C. (2019). Mindfulness for Children and Adults with Autism Spectrum Disorder and Their Caregivers: A Meta-analysis. Journal of Autism and Developmental Disorders, 49(10), 4306–4319. https://doi.org/10.1007/s10803-019-04145-3.
Hathaway, W., & Tan, E. (2009). Religiously oriented mindfulness-based cognitive therapy. Journal of Clinical Psychology, 65(2), 158–171. https://doi.org/10.1002/jclp.20569.
Hayes, S. C., & Strosahl, K. (2004). A practical guide to acceptance and commitment therapy. New York: Springer.
Hayes, S. C., Strosahl, K., & Wilson, K. G. (1999). Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford Press.
Higgins, J. P., & Green, S. (2011). Cochrane handbook for systematic reviews of interventions. New Jersey: Wiley.
Hilkey, D. (2019). Utilizing Online Learning of Acceptance and Commitment Training and Evaluating Corresponding Changes in Parent Stress. Southern Illinois University at Carbondale.
Hunter, J. E., Jensen, J. L., & Rodgers, R. (2016). The Control Group and Meta-Analysis. Journal of Methods and Measurement in the Social Sciences. https://doi.org/10.2458/azu_jmmss.v5i1.18302.
Impellizzeri, F. M., & Bizzini, M. (2012). Systematic review and meta-analysis: a primer. International Journal of Sports Physical Therapy, 7, 493–503.
Kabat-Zinn, J. (1990). Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Delacorte Press.
Kabat-Zinn, J. (2003). Mindfulness-Based Interventions in Context: Past, Present, and Future. Clinical Psychology: Science and Practice, 10(2), 144–156. https://doi.org/10.1093/clipsy.bpg016.
Karazsia, B. T., & Wildman, B. G. (2009). The mediating effects of parenting behaviors on maternal affect and reports of children’s behavior. Journal of Child and Family Studies, 18(3), 342. https://doi.org/10.1007/s10826-008-9236-8.
Kempler, L., Sharpe, L., Miller, C. B., & Bartlett, D. J. (2016). Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep Medicine Reviews, 29, 15–22. https://doi.org/10.1016/j.smrv.2015.08.002.
Khan, S., & Khan, R. A. (2017). Chronic Stress Leads to Anxiety and Depression. Annals of Psychiatry and Mental Health, 5(1), 1091.
Kohtala, A., Muotka, J., & Lappalainen, R. (2017). What happens after five years?: The long-term effects of a four-session Acceptance and Commitment Therapy delivered by student therapists for depressive symptoms. Journal of Contextual Behavioral Science, 6(2), 230–238. https://doi.org/10.1016/j.jcbs.2017.03.003.
Lindahl, J. R. (2015). Why Right Mindfulness Might Not Be Right for Mindfulness. Mindfulness (N Y), 6(1), 57–62. https://doi.org/10.1007/s12671-014-0380-5.
Lloyd, T. J., & Hastings, R. (2009). Hope as a psychological resilience factor in mothers and fathers of children with intellectual disabilities. Journal of Intellectual Disability Research, 53(12), 957–968. https://doi.org/10.1111/j.1365-2788.2009.01206.x.
Lo, H. H. M., Chan, S. K. C., Szeto, M. P., Chan, C. Y. H., & Choi, C. W. (2017). A feasibility study of a brief mindfulness-based program for parents of preschool children with developmental disabilities [Cognitive Therapy 3311]. Mindfulness (N Y), 8(6), 1665–1673. https://doi.org/10.1007/s12671-017-0741-y.
Lo, H. H. M., Wong, S. W. L., Wong, J. Y. H., Yeung, J. W. K., Snel, E., & Wong, S. Y. S. (2020). The Effects of Family-Based Mindfulness Intervention on ADHD Symptomology in Young Children and Their Parents: A Randomized Control Trial. J Atten Disord, 24(5), 667–680. https://doi.org/10.1177/1087054717743330.
Lovell, B., Moss, M., & Wetherell, M. A. (2012). With a little help from my friends: Psychological, endocrine and health corollaries of social support in parental caregivers of children with autism or ADHD. Research in Developmental Disabilities, 33(2), 682–687. https://doi.org/10.1016/j.ridd.2011.11.014.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med, 6(7), e1000097–e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Mullen, B., & Suls, J. (1982). The effectiveness of attention and rejection as coping styles: A meta-analysis of temporal differences. Journal of Psychosomatic Research, 26(1), 43–49. https://doi.org/10.1016/0022-3999(82)90061-7.
Neece, C. L. (2014). Mindfulness-based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. Journal of Applied Research in Intellectual Disabilities, 27(2), 174–186. https://doi.org/10.1111/jar.12064.
Noone, S. J., & Hastings, R. P. (2010). Using Acceptance and Mindfulness-Based Workshops with Support Staff Caring for Adults with Intellectual Disabilities. Mindfulness (N Y), 1(2), 67–73. https://doi.org/10.1007/s12671-010-0007-4.
Osborn, R., Dorstyn, D., Roberts, L., & Kneebone, I. (2020). Mindfulness Therapies for Improving Mental Health in Parents of Children with a Developmental Disability: a Systematic Review. Journal of Developmental and Physical Disabilities. https://doi.org/10.1007/s10882-020-09753-x.
Petcharat, M. (2018). The Effects of a Brief Culturally Tailored Thai Mindfulness Intervention on Stress, Anxiety, and Mindfulness in Thai Parents of Children with Developmental Disabilities. Boca Raton: Florida Atlantic University.
Petcharat, M., & Liehr, P. (2017). Mindfulness training for parents of children with special needs: Guidance for nurses in mental health practice. Journal of Child and Adolescent Psychiatric Nursing, 30(1), 35–46. https://doi.org/10.1111/jcap.12169.
Praissman, S. (2008). Mindfulness-based stress reduction: a literature review and clinician’s guide. J Am Acad Nurse Pract, 20(4), 212–216. https://doi.org/10.1111/j.1745-7599.2008.00306.x.
Rayan, A., & Ahmad, M. (2017). Effectiveness of mindfulness-based intervention on perceived stress, anxiety, and depression among parents of children with autism spectrum disorder [Cognitive Therapy 3311]. Mindfulness (N Y), 8(3), 677–690. https://doi.org/10.1007/s12671-016-0595-8.
Rayan, A., & Ahmad, M. (2018). Mindfulness and parenting distress among parents of children with disabilities: A literature review. Perspect Psychiatr Care, 54(2), 324–330. https://doi.org/10.1111/ppc.12217.
Ritchie, H. (n.d.) Neurodevelopmental disorders. Our World in Data. https://ourworldindata.org/neurodevelopmental-disorders Accessed 4 December, 2020.
Rubin, I. L., & Crocker, A. C. (1989). Developmental disabilities: delivery of medical care for children and adults. Palo Alto: Lea & Febiger.
Santiago, P. N., & Gall, T. L. (2016). Acceptance and Commitment Therapy as a Spiritually Integrated Psychotherapy. Counseling and Values, 61(2), 239–254. https://doi.org/10.1002/cvj.12040.
Sawilowsky, S. S. (2009). New Effect Size Rules of Thumb. Journal of Modern Applied Statistical Methods, 8(2), 597–599. https://doi.org/10.22237/jmasm/1257035100.
Seabrook, E., Kelly, R., Foley, F., Theiler, S., Thomas, N., Wadley, G., & Nedeljkovic, M. (2020). Understanding How Virtual Reality Can Support Mindfulness Practice: Mixed Methods Study. J Med Internet Res, 22(3), e16106. https://doi.org/10.2196/16106.
Sedgwick, P. (2014). Randomised Controlled Trials: Subgroup Analyses. BMJ, 349, g7513. https://doi.org/10.1136/bmj.g7513.
Segal, Z., & Williams, J. M. G. (2001). Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York: Guilford Publications.
Semple, R. J., & Hatt, S. P. (2012). Translation of Eastern Meditative Disciplines Into Western Psychotherapy, 1. Oxford: Oxford University Press.
Sevilla-Llewellyn-Jones, J., Santesteban-Echarri, O., Pryor, I., McGorry, P., & Alvarez-Jimenez, M. (2018). Web-Based Mindfulness Interventions for Mental Health Treatment: Systematic Review and Meta-Analysis. JMIR Ment Health, 5(3), e10278–e10278. https://doi.org/10.2196/10278.
Singer, G. H. S. (2006). Meta-Analysis of Comparative Studies of Depression in Mothers of Children With and Without Developmental Disabilities. American journal of mental retardation : AJMR, 111(3), 155. https://doi.org/10.1352/0895-8017(2006)111[155:MOCSOD]2.0.CO;2.
Singer, G. H. S., Ethridge, B. L., & Aldana, S. I. (2007). Primary and secondary effects of parenting and stress management interventions for parents of children with developmental disabilities: A meta-analysis. Mental Retardation and Developmental Disabilities Research Reviews, 13(4), 357–369. https://doi.org/10.1002/mrdd.20175.
Sohmaran, C., & Shorey, S. (2019). Psychological interventions in reducing stress, depression and anxiety among parents of children and adolescents with developmental disabilities: A systematic review and meta-analysis. Journal of Advanced Nursing, 75(12), 3316–3330. https://doi.org/10.1111/jan.14166.
Sterne, J. A. C., Sutton, A. J., Ioannidis, J. P. A., Terrin, N., Jones, D. R., Lau, J., et al. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ, 343, d4002. https://doi.org/10.1136/bmj.d4002.
Teasdale, J. D., Segal, Z., & Williams, J. M. G. (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy, 33(1), 25–39. https://doi.org/10.1016/0005-7967(94)E0011-7.
The Embassy of the Hashemite Kingdom of Jordan. (2020). Culture and Religion. The Embassy of the Hashemite Kingdom of Jordan. http://www.jordanembassyus.org/page/culture-and-religion Accessed 15 June, 2020.
Thomas, J., Raynor, M., & Bakker, M.-C. (2016). Mindfulness-based stress reduction among Emirati Muslim women. Mental Health, Religion & Culture, 19(3), 295–304. https://doi.org/10.1080/13674676.2016.1168389.
Thurston, S., Paul, L., Loney, P., Ye, C., Wong, M., & Browne, G. (2011). Associations and costs of parental symptoms of psychiatric distress in a multi-diagnosis group of children with special needs. Journal of Intellectual Disability Research, 55(3), 263–280. https://doi.org/10.1111/j.1365-2788.2010.01356.x.
Townshend, K., Jordan, Z., Stephenson, M., & Tsey, K. (2016). The effectiveness of mindful parenting programs in promoting parents’ and children’s wellbeing: A systematic review. JBI Database System Rev Implement Rep, 14(3), 139–178. https://doi.org/10.11124/JBISRIR-2016-2314.
Whittingham, K., Sanders, M. R., McKinlay, L., & Boyd, R. N. (2016). Parenting Intervention Combined With Acceptance and Commitment Therapy: A Trial With Families of Children With Cerebral Palsy. Journal of Pediatric Psychology, 41(5), 531–542. https://doi.org/10.1093/jpepsy/jsv118.
World Health Organisation, (2013). Definition of key terms. World Health Organisation. https://www.who.int/hiv/pub/guidelines/arv2013/intro/keyterms/en/ Accessed 13 May, 2020.
World Population Review. (2020). Iran Population 2020. World Population Review. https://worldpopulationreview.com/countries/iran-population/ Accessed 15 June, 2020.
Zablotsky, B., Black, L. I., Maenner, M. J., Schieve, L. A., Danielson, M. L., Bitsko, R. H., et al. (2019). Prevalence and Trends of Developmental Disabilities among Children in the United States: 2009–2017. Pediatrics, 144(4), e20190811. https://doi.org/10.1542/peds.2019-0811.
Zhang, H., Zhang, H., Emory, E. K., & Emory, E. K. (2015). A Mindfulness-Based Intervention for Pregnant African-American Women. Mindfulness (N Y), 6(3), 663–674. https://doi.org/10.1007/s12671-014-0304-4.
Zody, M. C. (2018). Acceptance and Commitment Therapy (ACT) as a one-day workshop for parents of children with an Autism Spectrum Disorder. Wright Institute Graduate School of Psychology.
Acknowledgments
The authors would like to thank the National University Health System, Research Support Unit, for assistance in the language editing of this manuscript.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
YXJC contributed to Data curation, formal analysis, writing first draft. SS contributed to Conceptualisation, methodology, supervision, visualization, final review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chua, J.Y.X., Shorey, S. The Effect of Mindfulness-Based and Acceptance Commitment Therapy-Based Interventions to Improve the Mental Well-Being Among Parents of Children with Developmental Disabilities: A Systematic Review and Meta-Analysis. J Autism Dev Disord 52, 2770–2783 (2022). https://doi.org/10.1007/s10803-021-04893-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-021-04893-1