Abstract
Heart failure with preserved ejection fraction (HFpEF) does not exist as a singular clinical or pathological entity but as a syndrome encompassing a wide range of clinical and biological phenotypes. There is an urgent need to progress from the unsuccessful ‘one-size-fits-all’ approach to more precise disease classification, in order to develop targeted therapies, personalise risk stratification and guide future research. In this regard, this review discusses the current and emerging roles of cardiovascular imaging for the diagnosis of HFpEF, for distilling HFpEF into distinct disease entities according to underlying pathobiology and for risk stratification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure with preserved ejection fraction (HFpEF) does not exist as a singular entity but as a syndrome that encompasses a broad cohort of patients with a range of clinical and biological phenotypes [1, 2].
The utility of cardiovascular imaging in HFpEF serves three primary functions: (1) diagnosis: to determine whether patients’ symptoms and signs are due to heart failure (HF) and to identify specific causes of HF in the context of a normal or near normal left ventricular (LV) ejection fraction (EF); (2) biological classification: to characterise the underlying disease mechanisms; and (3) risk stratification: to guide prognosis.
The growing prevalence of HFpEF and its poor outcome dictate an urgent need for more precise disease classification in order to develop therapies that target specific pathophysiological mechanisms and to personalise risk stratification. The failure of multiple large phase III trials to identify an effective therapy serves to demonstrate that the “one-size fits all” approach to HFpEF is inadequate.
This review discusses the current and emerging roles of cardiac imaging for the diagnosis of HFpEF, for distilling HFpEF into distinct disease entities and for risk stratification.
Diagnosis
Diagnosing heart failure in the context of a preserved ejection fraction
Patients with suspected HFpEF represent a considerable diagnostic challenge, often having multiple co-morbid reasons for breathlessness, peripheral oedema and other clinical features consistent with HF. Whilst natriuretic peptides have increased diagnostic confidence for HF, they lack sensitivity and specificity in important subgroups such as obesity. Furthermore, their elevation may represent an advanced pathophysiological stage that may be less modifiable, where decompensation has already occurred [3, 4].
Cardiac imaging, most commonly echocardiography, is employed in this context to investigate for evidence of LV ‘diastolic dysfunction’. LV diastolic dysfunction is caused by impaired LV relaxation and increased LV chamber stiffness. When diastolic dysfunction leads to impaired LV filling, LV diastolic pressure becomes elevated as a compensatory mechanism in order to maintain cardiac output. Echocardiographic assessment of LV diastolic function includes a number of indices that, when combined, provide an indication of LV filling and the sequelae of abnormal LV filling, particularly raised left atrial pressure (LAP). Specifically, the 2016 European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE) recommendations advise a combination of four variables for diagnosing diastolic dysfunction in patients with normal LV EF: annular e′ velocity (septal e′ < 7 cm/s, lateral e′ < 10 cm/s), average E/e′ ratio > 14, LA maximum volume index > 34 mL/m2 and peak tricuspid regurgitant velocity > 2.8 m/s [5]. Understanding the basis of non-invasive indices of diastolic function is crucial for their interpretation and for understanding their utility for identifying patients for inclusion in trials and for measuring the effect of interventions. Table 1 and Fig. 1 describe commonly used imaging measurements of diastolic function.
Echocardiographic measures used to assess diastolic dysfunction. a Mitral valve (MV) E-wave and A-wave peak velocities, obtained on pulse-wave Doppler, are combined to generate the E/A ratio. b Mitral valve E-wave peak velocity and tissue Doppler (TDI) eʹ velocity (here measured at the lateral MV annulus; average eʹ is calculated from both the lateral and medial sites) are combined to generate the E/eʹ ratio. c Peak velocity of tricuspid valve (TV) regurgitation. d Apical 2-chamber view and measurement of left atrial (LA) volume. DT–deceleration time
It is important to recognise that diastolic dysfunction does not equate to a diagnosis of HF, rather a mechanism for its presence; indeed, it may identify an earlier stage of HF than natriuretic peptides [6]. It is also important to note that across HFpEF trials, a third of patients consistently have normal diastolic function, suggesting that diastolic dysfunction is not the causative mechanism in a significant proportion of patients [2].
LV filling
LV filling pressure refers to the pressure difference between the left atrium (LA) and LV that is responsible for LV filling during diastole. In the healthy heart at end-diastole, pulmonary artery pressure (PAP), LAP and LV end-diastolic pressures (LVEDP) effectively equalise and can collectively be referred to as ‘LV filling pressures’ [7]. However, in disease, this equilibrium is disturbed in an unpredictable manner and thus whilst widely used, the term ‘LV filling pressures’ is ambiguous and can be misleading. Studies generally include one of these measurements to indicate LV filling pressure, the choice of which depends upon what is available and the purpose of the study (idealistically LAP when the focus is pulmonary congestion and LVEDP when the focus is myocardial mechanical function). Indeed, the variable strength of association between echocardiographic diastolic indices and invasive haemodynamic measurements in part reflects the use of different invasive correlates (Table 1).
LV filling is determined by ventricular relaxation and chamber compliance [8]. Ventricular relaxation, defined by the rate and duration of LV pressure decay, begins in mid-systole and ends in early diastole and is an active process related to myofibrillar dissociation and calcium reuptake [9]. A number of mechanisms contribute to dysfunctional ventricular relaxation, including delayed inactivation, reduced restoring forces, diminished load dependence, increased mechanical non-uniformity of relaxation and the inability to increase relaxation rate in response to exercise (reduced diastolic reserve) [10]. The time constant (tau) of the isovolumetric fall in LV pressure is considered the gold standard invasive measurement of LV relaxation (Table 2).
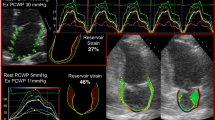
Early diastolic mitral annular velocity (e′), measured using tissue Doppler imaging (TDI), provides a reflection of myocardial fibre lengthening and is used to assess ventricular relaxation; however, e′ is also determined by other factors, including elastic restoring forces, ventricular loading and acquisition angle, and as a result, the association between e′ and tau is variable (Table 1). A number of novel echocardiographic indices of ventricular relaxation have been proposed. Peak global longitudinal diastolic strain rate during isovolumetric relaxation (SRIVR), measured with speckle-tracking, is a potentially load-independent measure of global ventricular relaxation and shows a moderately strong inverse correlation with tau (r = − 0.74), although it is image quality-dependent (Fig. 2) [11]. Peak reverse ejection intraventricular pressure difference, measured using colour M-mode Doppler, also shows a moderately strong inverse correlation with tau (r = − 0.71), which improves when combined with e′ (r = − 0.84), and colour M-mode Doppler flow propagation velocity (Vp) has shown strong inverse correlation with tau (r = − 0.75), although neither method measures myocardial deformation directly and both are technically demanding [12, 13].
Speckle-tracking measures on echocardiography. a Peak apical rotation and untwist measurements from the apical short-axis view (SHAX). b Basal rotation and apical rotation generates peak left ventricular (LV) twist, measured from the basal-SHAX and apical-SHAX, respectively. c Peak LV untwisting rate, measured from the apical-SHAX. d Peak global longitudinal strain rate during isovolumetric relaxation (SRIVR). e Left atrial (LA) strain in the apical 4-chamber view measured as reservoir, conduit, and booster strain. AVC–aortic valve closure; MVO–mitral valve opening
LV untwisting during isovolumetric relaxation releases energy stored during systolic twisting in the extracellular matrix (ECM) and in the sarcomeric macromolecule titin and is purported as a measurement of LV relaxation. Peak LV untwisting rate has shown load-independent associations with tau in preclinical studies [14, 15].
Effective LV chamber compliance is defined as change in volume over change in pressure and is conceptualised as a passive process related to viscoelastic properties of the myocardium, which are governed by factors such as aging, the ECM and titin. Broader LV compliance is determined by additional factors such as the pericardium and ventricular interaction. Chamber stiffness is the reciprocal of chamber compliance and can be measured invasively in a number of ways (Table 2). The end-diastolic pressure–volume relationship (EDPVR) is exponential and measures LV chamber stiffness from multiple measurements of LVEDP and LV end-diastolic volume (EDV). A curve-fit equation (most commonly a power function or exponential equation) generates α (a curve-fitting constant) and β (the LV ‘stiffness constant’), the latter of which is influenced by geometrical changes, such as LV hypertrophy, and intrinsic myocardial stiffness. Using this equation, an echocardiographic method has been developed to estimate single-beat β, in which LVEDP is estimated from E/e′. To account for covariance between α and β, calculated LV EDV at an idealised LVEDP (e.g. 20 mmHg, denoted by EDV20) can compare LV stiffness between groups in cohort studies [16]. In a large prospective observational study (n = 419), in which patients with HFpEF were enrolled following HF hospitalisation, decreased LV compliance, indicated by reduced EDV20, was independently associated with HF hospitalisation (adjusted hazard ratio (HR) 1.67 [confidence interval: 1.22–2.30]) and combined cardiovascular hospitalisation and/or death (adjusted HR 1.39 [confidence interval: 1.10–1.75]) in multivariable analysis [17].
Rather than evaluating its constituent components, LV filling is usually assessed more broadly using mitral inflow indices such as E/A ratio and E wave velocity deceleration time (Table 1). However, as is well recognised, mitral E/A ratio has a U-shaped relationship with LVEDP, making it difficult to differentiate normal from abnormal (‘pseudo-normalisation’), particularly in the setting of normal LVEF, and mitral E wave deceleration time does not relate to LVEDP when LVEF is normal [18].
LA pressure
Raised LAP is the key marker for identifying cardiac-induced pulmonary venous congestion [7]. LAP is rarely measured directly; instead, a number of invasive surrogates have historically been used, including pulmonary capillary wedge pressure (PCWP), pre-a-wave LV pressure (pre-a-LVP), mean LV diastolic pressure (mLVDP) and LVEDP. Each of these measurements shows a strong correlation with LAP in health, but in disease, the relationships are more variable. For example, LVEDP can be elevated without an increase in LAP, which is important when considering the validity of non-invasive assessments [18,19,20].
There have been many attempts to identify a non-invasive measurement of LAP; however, all are influenced by factors other than LAP. LA volume is used as a relatively straightforward assessment of LAP; however, it is neither sensitive nor specific. One-third to one-half of patients in HFpEF studies have normal LA size and the relationship between LA size and outcome is variable [21, 22]. In the echocardiographic substudy of TOPCAT (Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist Trial), patients enrolled on the basis of elevated natriuretic peptides did have larger LA volumes than those enrolled on the basis of previous hospitalization, but median LA volume was lower than the EACVI/ASE threshold for diastolic dysfunction (30.3 [23.0–38.9] mL/m2) [22]. Borlaug et al. [23] showed that a third of patients with HFpEF, diagnosed using invasive haemodynamic measurements made during exercise (exercise PCWP ≥ 25 mmHg), had normal LA size. Furthermore, in around a third of patients with HFpEF included in a comprehensive phenotyping study by Shah et al. [24], LA volume was lower than the EACVI/ASE threshold despite PCWP being elevated (19.0 ± 6.3 mmHg). Conversely, one-third of patients with hypertension without HF have LA enlargement, and half of patients with normal resting and exercise PCWP have LA dilatation [25, 26].
The E/e′ ratio (Table 1) was developed in order to correct mitral E-wave velocity, which reflects the LA-LV pressure gradient during early diastole and is dependent on the rate of LV relaxation and LAP as well as a number of confounding factors, for LV relaxation in order to provide a more discriminatory indication of LAP, and hence differentiate normal from pseudo-normal mitral inflow. Indeed, studies do generally agree that a markedly elevated E/e′ ratio (> 13–15) is highly specific for increased ‘LV filling pressures’ and a ratio of < 8 usually indicates normal ‘LV filling pressures’ [18]. However, E/e′ ratio is influenced by mitral valve and pericardial disease and there remains a wide grey-zone where it is unhelpful. In patients with preserved LVEF (> 50%), E/e′ ratio does associate with mLVDP more closely than other echocardiographic indices; however, the relationship is modest (r = 0.47 in the study by Ommen et al.[18]), and much less strong than in patients with reduced LVEF [8].
Exercise
It is increasingly recognised that LAP may only become elevated during exercise [26, 27]. This group of patients, which describe exertional dyspnoea but have normal resting diastolic function and normal natriuretic peptides, represent a particular diagnostic challenge.
In the healthy heart, both early diastolic suction (increasing mitral valve flow) and myocardial relaxation are augmented during exercise; thus, E/e′ ratio is preserved. In a group of 74 consecutive patients with EF ≥ 50% referred for haemodynamic investigations for exertional dyspnoea, elevated PCWP (≥ 25 mmHg) was evident during exercise in around a third of patients [26]. Addition of exercise E/e′ to resting E/e′ improved sensitivity for identifying patients with HFpEF to 90%, albeit the cost of reduced specificity (75%).
Current guidelines recommend exercise echocardiography in patients with indeterminate resting measurements (i.e. grey-zone E/e′) and in patients with diagnostic uncertainty [5]. Recently, LA strain measured using speckle-tracking echocardiography at rest has shown comparable sensitivity and specificity (86% and 79%, respectively) for identifying elevated exercise PCWP [28]. The utility of exercise LA strain is yet to be determined.
Specific causes of HFpEF
There are a number of specific causes of HF in the context of a normal EF (e.g. amyloid, hypertrophic cardiomyopathy, Fabry disease etc.) that potentially account for as many as 25% of patients with a label of ‘HFpEF’ (Fig. 3) [29]. This has important implications both for clinical trials, where their inclusion may negate the beneficial effect of the intervention (as cited in the recent prospective comparison of angiotensin receptor-neprilysin inhibitor with angiotensin-receptor blockers Global Outcomes in HF with Preserved Ejection Fraction (PARAGON-HF) trial [30]), and clinical management, where specific therapies are available (e.g. light-chain amyloidosis). Incorporating advanced imaging, such as cardiovascular magnetic resonance (CMR) imaging, into HFpEF trial recruitment, at least for patients displaying notable characteristics such as very high natriuretic peptide levels, may be beneficial.
Specific causes of heart failure with preserved ejection fraction (HFpEF) diagnosed on cardiac magnetic resonance imaging (CMR). a Short axis late-gadolinium enhancement (LGE) sequence in a patient with HFpEF secondary to cardiac amyloidosis. Diffuse subendocardial enhancement is seen in the left and right ventricles. b Apical 4-chamber view in the same patient showing subendocardial LGE. c Apical 4-chamber cine in a patient initially diagnosed with ‘HFpEF’. Increased wall thickening and hypertrophy are seen at the left ventricular (LV) apex typical of apical hypertrophic cardiomyopathy. d Short axis cine in a patient presenting with ‘HFpEF’, demonstrating pericardial thickening and ‘D’ shaped flattening of the septum towards the LV during diastole. Subsequently diagnosed with pericardial constriction
Biological classification
HFpEF involves multiple pathophysiological mechanisms, which drive the heterogeneous phenotypes that are evident clinically [2]. By characterising these biological processes, cardiovascular imaging has the potential to distil HFpEF into distinct disease entities, which may provide more precise risk stratification and identify individual patients for targeted interventions.
Myocardial fibrosis
ECM expansion secondary to collagen accumulation is associated with increased myocardial stiffness [31, 32]. Extracellular volume fraction (ECV), measured using CMR, provides a non-invasive measurement of myocardial fibrosis (Fig. 4) [33]. Elevated ECV is common in HFpEF but not universal; Schelbert et al. [34] showed that at least a quarter of patients diagnosed with HFpEF have an ECV less than the median value of a non-HFpEF control group. Furthermore, elevated ECV can be seen in hypertensive patients without HF [35]. As such, while ECV should not be regarded as a diagnostic biomarker for ‘HFpEF’ as a single entity, it can be used to identify a subgroup of patients with a fibrotic phenotype.
Rommel et al. [36] demonstrated a strong correlation between ECV and invasively measured LV stiffness constant β (r = 0.75, p < 0.01), and ECV was the only independent predictor of β on multivariable analysis. To illustrate the potential utility of ECV for identifying phenotypic subtypes of HFpEF, when patients in the study by Rommel et al. were dichotomized according to median ECV, both groups showed a pathological upward shift of the end-diastolic pressure–volume relationship during exercise; however, the dominant pathophysiology was an increase in myocardial passive stiffness in patients with elevated ECM volume, whereas the dominant mechanisms were arterial stiffness and impaired active relaxation in patients with a below-median ECM volume.
Importantly, myocardial fibrosis, measured using ECV, strongly associates with adverse outcome in patients with HFpEF, including death and hospitalisation for HF [34], and as such, myocardial fibrosis is identified as a potentially important therapeutic target.
Impaired myocardial energetics
Active LV relaxation, occurring in late systole and early diastole, is an adenosine triphosphate (ATP)-consuming process. Metabolomic profiling has demonstrated dysfunctional fatty acid oxidation in HFpEF [37], and myocardial fibrosis and microvascular dysfunction potentially render cardiomyocytes prone to hypoxia [38]. Phosphorous-31 magnetic resonance spectroscopy (31P-MRS) can non-invasively quantify the phosphocreatine (PCr) to ATP ratio, an index of energetic status that reflects the creatine kinase energy shuttle (Fig. 5) [39]. Phan et al. [40] showed HFpEF to be associated with significantly reduced resting PCr to ATP ratio compared with healthy controls (1.57 ± 0.52 and 2.14 ± 0.63 respectively, p = 0.003) and prolonged time to peak diastolic filling (a measure of active relaxation) during exercise. Proton magnetic resonance spectroscopy (1H-MRS) provides non-invasive measurement of myocardial triglyceride content and the identification of myocardial steatosis. Mahmod et al. [41], who measured both 31P-MRS and 1H-MRS, demonstrated significantly reduced PCr to ATP ratio and greater MTG in patients with HFpEF compared with healthy controls, with triglyceride content (but not PCr to ATP ratio) being independently associated with diastolic strain on multivariable analysis. The on-going phase 2 Pirfenidone in Heart Failure with Preserved Ejection Fraction (PIROUETTE) trial [42] includes assessment of the relationship between myocardial fibrosis and energetics, measured using 31P-MRS, and the impact of an antifibrotic intervention.
Myocardial energetics assessed by 31phosphorous-magnetic resonance spectroscopy (31P-MRS). A chemical-shift imaging 31P-MRS sequence, with voxel grid aligned to the ventricular septum, generates a frequency spectrum denoting phosphocreatine (PCr), γ-, α- and β-adenosine triphosphate (ATP), thus calculating the PCr to ATP ratio
Myocardial microvascular dysfunction
Invasive studies have demonstrated reduced myocardial oxygen delivery during exercise in a small group of HFpEF patients (n = 9) compared with hypertensive and normotensive controls [43]. In the absence of significant epicardial coronary artery disease, such findings likely reflect microvascular dysfunction, which may occur due to impaired endothelial function and blunted response to local vasoactive mediators (e.g. nitric oxide) [44]. Non-invasive assessment of coronary flow reserve (CFR) has been performed with Rubidium-82 cardiac positron emission tomography (PET) and phase-contrast CMR coronary sinus blood flow, with both techniques demonstrating reduced CFR on pharmacological stress in HFpEF patients compared with hypertensive and healthy controls [45, 46]. In a cohort of patients (n = 201) without significant epicardial coronary artery disease undergoing clinically indicated Rubidium-82 PET, Taqueti et al. [47] showed that a CFR of < 2.0 was associated with an increased risk of incident HFpEF hospitalisation on multivariable analysis (HR 2.47, adjusted for estimated glomerular filtration rate (eGFR), E/e′, LVEF, troponin and history of atrial fibrillation (AF)).
The PROMIS-HFpEF study [48] measured CRF in 202 HFpEF patients using echocardiographic pulse-wave Doppler of the left anterior descending artery via a modified 2-chamber apical view at rest and during adenosine stress, a method previously shown to be reproducible and demonstrate good agreement with cardiac PET-measured CFR [49]. Coronary microvascular dysfunction (defined as CFR < 2.5) was highly prevalent, seen in 75% of patients, and a CFR < 2.5 was associated with elevated N-terminal pro-brain natriuretic peptide (NTproBNP) and lower reactive hyperaemic index (a measure of flow-mediated dilatation following brachial artery occlusion) on multivariable analysis, potentially supporting the hypothesis of systemic endothelial dysfunction.
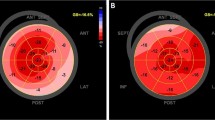
LV systolic dysfunction
Cardiomyocyte dysfunction is recognised in HFpEF. In a large study (n = 2042), Borlaug et al. [50] compared echocardiographic load-independent measures (Fig. 2) of systolic function between HFpEF (defined clinically based on Framingham diagnostic criteria), healthy and hypertensive controls. In comparison with healthy controls, mid-wall fractional shortening, a measure of myocardial contractility used to negate the effect of cross-fibre shortening and radial-axis thickening in concentric hypertrophy, was shown to be significantly increased in patients with hypertension without HFpEF but decreased in patients with HFpEF. The difference remained after correcting for afterload and was seen despite similar increases in end-systolic elastance (EES), a reflection of systolic workload and stiffness measured as the slope of the end-systolic pressure–volume relationship (ESPVR), thus highlighting the presence of contractile abnormalities despite preserved EF and EES [51]. Similarly, Kraigher-Krainer et al. [52] demonstrated reduced circumferential and global longitudinal LV strains (GLS), measured using speckle-tracking echocardiography, in patients with HFpEF compared with each of healthy and hypertensive controls. GLS was independently associated with natriuretic peptide levels in multivariable analysis but did not associate with eʹ (both septal and lateral measures), E/eʹ ratio (septal), or indexed LA volume, suggesting systolic dysfunction as a mechanistic driver of HFpEF independent of diastolic function. In a substudy from the TOPCAT trial, impaired GLS was common (52%) and the strongest echocardiographic predictor of the primary outcome (cardiovascular death, HF hospitalisation or aborted cardiac arrest) with an adjusted HR 1.14 [confidence interval: 1.04–1.24] per 1% decrease on multivariable analysis [53].
Compared with age-matched healthy controls, Tan et al. [54] demonstrated reduced and delayed LV untwisting, both at rest and on exercise, in a small HFpEF cohort, without a significant difference in LV mass or wall thickness. Findings regarding LV twist in HFpEF are conflicting. Tan et al. [54] reported reduced apical rotation, the main determinant of LV twist in patients with HFpEF, compared with healthy controls, and Mordi et al. [35] demonstrated reduced LV torsion in HFpEF; however, other studies have not replicated these findings [55]. Further work is required to understand the utility of twist indices.
Atrial dysfunction
LA dysfunction is rarely seen without LV diastolic dysfunction and is strongly associated with progressive severity; however, the origin and independent relevance of atrial dysfunction in HFpEF remains contentious [56]. Telles et al. [28] recently demonstrated an inverse correlation between LA reservoir strain (Fig. 2) and exercise PCWP in HFpEF (r = − 0.64, p < 0.001), highlighting its potential utility as a marker of dynamic LAP elevation. Using speckle-tracking echocardiography in 308 patients with HFpEF, Freed et al. [57] found an independent relationship between reduced LA reservoir strain and adverse outcomes. As a potential mechanism, LA reservoir strain was associated with markers of pulmonary vascular dysfunction. LA reservoir strain can be used to calculate LA stiffness index (either as PCWP to LA reservoir strain ratio, or as E/eʹ to LA reservoir strain ratio), which may be a more discriminative prognostic measure [58]. The multivariable models described by Freed et al. [57] that include LA stiffness index demonstrate a HR 1.39 to 1.44 per standard deviation decrement for the combined outcome of cardiovascular hospitalisation, HF hospitalisation or death. Furthermore, the association remained when the model was adjusted for GLS, suggesting that the impact LA stiffness has on prognosis may be independent of LV function. In a group of 46 patients undergoing surgery for severe mitral regurgitation, Cemeli et al. [59] showed a strong inverse correlation between peak LA reservoir strain and LA fibrosis on histology (r = − 0.82, p < 0.0001). LA fibrotic burden has been estimated using CMR late-gadolinium enhancement in multiple AF studies; however, the technique is challenging and there is a paucity of histological validation. It is yet to be applied in HFpEF.
Central and peripheral vascular dysfunction
Manifestations of increased arterial stiffness, such as increased pulse wave velocity (PWV), reduced aortic distensibility and increased pulse-wave reflections (PWR), have all been demonstrated in HFpEF (Fig. 6) [60, 61]. Arterial stiffness is multifactorial, caused by factors such as endothelial dysfunction and reduced nitric oxide bioavailability, increased collagen deposition and accumulation of advanced glycation end products and matrix proteins [62, 63]. A number of imaging modalities have been employed to assess arterial stiffness in HFpEF, including high-frequency ultrasound and CMR [64]. CMR generates cross-sectional aortic cine imaging with high spatial resolution allowing accurate measurement of aortic distensibility [60, 65]. Furthermore, velocity-encoded flow mapping can accurately measure PWV, for which several methods are described (including transit-time, flow-area and cross-correlation methods) [66]. PWR are naturally occurring pressure waves reflected back to the LV at sites of high impedance such as arterial branches. Arterial stiffening leads to faster wave reflections, which arrive back at the LV earlier during systole, leading to increased LV loading in mid-to-late systole, which in turn results in increased systolic workload [61, 67]. Weber et al. [61] demonstrated increased PWR in HFpEF compared with non-HFpEF groups. Compared with hypertensive controls, Reddy et al. [68] showed similar resting PWR in patients with HFpEF; however, these became elevated during exercise. Chirinos et al. [69] showed significantly increased PWV (measured by applanation tonometry) in diabetic HFpEF patients compared to non-diabetic HFpEF patients. Arterial stiffness and increased systemic vascular resistance strongly correlate to exercise limitation and reduced peak oxygen consumption rate (VO2) in patients with HFpEF compared with age- and sex-matched healthy controls; however, population studies have failed to demonstrate an independent association between arterial stiffness and incident HFpEF [60, 64, 70, 71].
Cardiac magnetic resonance imaging (CMR) measures of arterial stiffness. a–d Pulse wave velocity (PWV) is calculated between the ascending and descending aorta by the transit-time method. A Aortic ‘candy-stick’ cine is used to plan a through-plane velocity flow map, demonstrated by the green line bisecting the pulmonary artery. The aortic distance between the two aortic locations is measured (∆x). b, c Through-plane flow and magnitude images generated from the aortic candy stick. The ascending aorta is contoured in Red and the descending aorta in Green. d Graph demonstrating flow in the ascending aorta (Red) and descending aorta (Green) during systole. Time to half the peak flow rate is measured and the difference calculated as the transit time (∆t). PWV is calculated by the equation PWV = ∆x/∆t. e, f Through-plane cine image of the ascending aorta. The maximal (e) and minimal (f) aortic areas through the cardiac cycle are calculated. Ascending aortic distensibility (AAD) is calculated by the equation AAD = ∆A / (Amin × PP), where ∆A represents the change in aortic area, Amin the minimal aortic area, and PP the pulse pressure
No change in aortic distensibility was found after 12 months of enalapril or 9 months of spironolactone, compared with placebo, in two randomised controlled trials of HFpEF [65, 72]. Sacubitril/valsartan, which combines anti-fibrotic, anti-inflammatory and vasodilatory effects, and thus may target multiple aspects of arterial dysfunction, could be hypothesised to be more efficacious.
Risk stratification
Cardiac imaging, in conjunction with clinical indices, has the potential to more precisely risk stratify patients. Shah et al. [24] identified three distinct HFpEF clinical phenotypes with markedly differing prognosis. The first group, which was relatively young (mean age 61 years) and had comparatively low natriuretic peptide levels (median brain natriuretic peptide (BNP) 72 pg/mL) and normal or only mildly abnormal diastolic function, had the best prognosis. The second group had features in keeping with what has previously been described as ‘metabolic HF’, or more recently, the ‘HFpEF obesity phenotype’, with a high prevalence of obesity, diabetes and obstructive sleep apnoea [3, 73]. Diastolic dysfunction (three-quarters had moderate or severe dysfunction), LA dilatation and LV hypertrophy were prominent and right atrial pressure was also relatively high, thought to reflect pericardial constraint, possibly by epicardial adipose tissue. The unadjusted HR for death in this group, in comparison with the first group, was 4.0 [confidence interval: 1.5–10.9]. After adjusting for BNP and the Meta-Analysis Global Group in Chronic Heart Failure (MAGGIC) risk score, the HR for death was 2.2 [confidence interval: 0.8–6.0], which was highest of all of the groups. The third group had the highest prevalence of hypertension and AF and demonstrated the largest LA volumes, highest LV mass, highest BNP levels and most severe diastolic dysfunction. Patients were also more likely to have pulmonary hypertension and right heart dysfunction. In comparison with the first group, the third group had an unadjusted HR for death of 6.5 [confidence interval: 2.5–16.6].
Discussion
The diagnosis of HFpEF is complex and inconsistent imaging measurements lead to greater ambiguity. Indices of diastolic function are very much in keeping with the ethos of ‘measuring what we can measure, rather than what we want to measure’. Indeed, no echocardiographic index is specific to any particular component of diastolic function, and all are confounded by factors unrelated to diastolic function [6]. The ‘gold-standard’ diagnostic parameter remains resting and exercise invasive LAP measurement. In the setting of normal resting echocardiographic indices and natriuretic peptide levels, exercise echocardiographic indices are useful for distinguishing patients that truly have dynamic LAP elevation; however, the technique is far from perfect and current measurements (e.g. E/eʹ) may generate a high rate of false-positive results. Assessment of diastolic dysfunction during exercise requires further refinement.
As a result of the limitations of current measurements of diastolic function, HF symptoms may be wrongly classed (or ‘dismissed’) as ‘non-cardiac’ [23, 24, 26, 28, 58]. Furthermore, mandating that particular structural abnormalities, such as LA dilatation and increased LV wall thickness, be present for a diagnosis of HFpEF, as is the case in recent and on-going trials, means that some patients with confirmed HFpEF are excluded from such trials [4, 23, 74, 75].
So, what for the future? Whilst, as discussed, a number of imaging measurements hold promise for more meaningful assessment of diastolic function, there is no non-invasive index on the horizon that seems likely to overcome the current limitations. But perhaps that is the wrong approach in any case. Having identified a patient with symptoms ± signs of HF, raised natriuretic peptide levels and a preserved LVEF, perhaps the next step in the diagnostic pathway should be to search for the underlying disease mechanism, for it is this that an intervention would aim to target, and it is this that will determine prognosis. Does the patient have fibrotic-HFpEF, do they have arterial dysfunction-HFpEF, do they have atrial dysfunction-HFpEF? We currently do not routinely investigate for the cause of HF in the context of a preserved EF, and as such, it is entirely unsurprising that we do not have a treatment. Indeed, as an analogy, we currently stop at ‘anaemia’, rather than going on to determine the cause of the anaemia and hence the underlying diagnosis. HFpEF is not a diagnosis.
Imaging can help. As described, contemporary imaging techniques can delve into the myocardium and identify those patients with myocardial fibrosis, with cellular hypertrophy, with impaired energetics, and assess the wider cardiovascular system to identify those patients with atrial dysfunction and with arterial dysfunction. Myocardial fibrotic-HFpEF is a good example. Myocardial fibrosis can be measured non-invasively with CMR and myocardial fibrosis is strongly associated with prognosis in HFpEF. If we routinely assessed for myocardial fibrosis, we could potentially target those patients displaying it with antifibrotic interventions, as is under investigation in the ongoing PIROUETTE trial (NCT02932566) [42].
Reclassifying the complexity of HFpEF into more appropriate diagnoses that take into account underlying disease mechanisms and clinical factors is likely to require techniques such as machine learning, as used by Shah et al. and others. Such techniques allow “agnostic’ variable selection, in which optimal groups of variables are chosen through iterative statistical modelling, rather through human endeavour [76]. Grouping together pathophysiologically similar individuals would provide the basis for developing and evaluating tailored therapy, provide patients with more appropriate diagnoses, allow personalised risk stratification and better guide patient care.
References
Shah SJ, Kitzman DW, Borlaug BA, van Heerebeek L, Zile MR, Kass DA, Paulus WJ (2016) Phenotype-specific treatment of heart failure with preserved ejection fraction: A multiorgan roadmap. Circulation 134(1):73–90. https://doi.org/10.1161/CIRCULATIONAHA.116.021884
Lewis GA, Schelbert EB, Williams SG, Cunnington C, Ahmed F, McDonagh TA, Miller CA (2017) Biological phenotypes of heart failure with preserved ejection fraction. J Am Coll Cardiol 70(17):2186–2200. https://doi.org/10.1016/j.jacc.2017.09.006
Obokata M, Reddy YNV, Pislaru SV, Melenovsky V, Borlaug BA (2017) Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation 136(1):6–19. https://doi.org/10.1161/CIRCULATIONAHA.116.026807
Anand IS, Claggett B, Liu J, Shah AM, Rector TS, Shah SJ, Desai AS, O’Meara E, Fleg JL, Pfeffer MA, Pitt B, Solomon SD (2017) Interaction between spironolactone and natriuretic peptides in patients with heart failure and preserved ejection fraction: from the TOPCAT Trial. JACC Heart Fail 5(4):241–252. https://doi.org/10.1016/j.jchf.2016.11.015
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29(4):277–314. https://doi.org/10.1016/j.echo.2016.01.011
Kosmala W, Rojek A, Przewlocka-Kosmala M, Mysiak A, Karolko B, Marwick TH (2016) Contributions of nondiastolic factors to exercise intolerance in heart failure with preserved ejection fraction. J Am Coll Cardiol 67(6):659–670. https://doi.org/10.1016/j.jacc.2015.10.096
Peverill RE (2015) “Left ventricular filling pressure(s)” - ambiguous and misleading terminology, best abandoned. Int J Cardiol 191:110–113. https://doi.org/10.1016/j.ijcard.2015.04.254
Nishimura RA, Tajik AJ (1997) Evaluation of diastolic filling of left ventricle in health and disease: Doppler echocardiography is the clinician’s Rosetta Stone. J Am Coll Cardiol 30(1):8–18
Mirsky I (1984) Assessment of diastolic function: Suggested methods and future considerations. Circulation 69(4):836–841
Brutsaert DL, Rademakers FE, Sys SU (1984) Triple control of relaxation: Implications in cardiac disease. Circulation 69(1):190–196
Wang J, Khoury DS, Thohan V, Torre-Amione G, Nagueh SF (2007) Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressures. Circulation 115(11):1376–1383. https://doi.org/10.1161/CIRCULATIONAHA.106.662882
Yotti R, Bermejo J, Benito Y, Antoranz JC, Desco MM, Rodriguez-Perez D, Cortina C, Mombiela T, Barrio A, Elizaga J, Fernandez-Aviles F (2011) Noninvasive estimation of the rate of relaxation by the analysis of intraventricular pressure gradients. Circ Cardiovasc Imaging 4(2):94–104. https://doi.org/10.1161/CIRCIMAGING.110.960369
Garcia MJ, Palac RT, Malenka DJ, Terrell P, Plehn JF (1999) Color M-mode Doppler flow propagation velocity is a relatively preload-independent index of left ventricular filling. J Am Soc Echocardiogr 12(2):129–137. https://doi.org/10.1016/s0894-7317(99)70125-2
Dong SJ, Hees PS, Siu CO, Weiss JL, Shapiro EP (2001) MRI assessment of LV relaxation by untwisting rate: A new isovolumic phase measure of tau. Am J Physiol Heart Circ Physiol 281(5):H2002-2009. https://doi.org/10.1152/ajpheart.2001.281.5.H2002
Notomi Y, Popovic ZB, Yamada H, Wallick DW, Martin MG, Oryszak SJ, Shiota T, Greenberg NL, Thomas JD (2008) Ventricular untwisting: A temporal link between left ventricular relaxation and suction. Am J Physiol Heart Circ Physiol 294(1):H505-513. https://doi.org/10.1152/ajpheart.00975.2007
Lam CS, Roger VL, Rodeheffer RJ, Bursi F, Borlaug BA, Ommen SR, Kass DA, Redfield MM (2007) Cardiac structure and ventricular-vascular function in persons with heart failure and preserved ejection fraction from Olmsted County. Minnesota Circulation 115(15):1982–1990. https://doi.org/10.1161/CIRCULATIONAHA.106.659763
Burke MA, Katz DH, Beussink L, Selvaraj S, Gupta DK, Fox J, Chakrabarti S, Sauer AJ, Rich JD, Freed BH, Shah SJ (2014) Prognostic importance of pathophysiologic markers in patients with heart failure and preserved ejection fraction. Circ Heart Fail 7(2):288–299. https://doi.org/10.1161/CIRCHEARTFAILURE.113.000854
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: A comparative simultaneous doppler-catheterization study. Circulation 102(15):1788–1794
Yamamoto K, Nishimura RA, Redfield MM (1996) Assessment of mean left atrial pressure from the left ventricular pressure tracing in patients with cardiomyopathies. Am J Cardiol 78(1):107–110. https://doi.org/10.1016/s0002-9149(96)00238-x
Nishimura RA, Appleton CP, Redfield MM, Ilstrup DM, Holmes DR Jr, Tajik AJ (1996) Noninvasive Doppler echocardiographic evaluation of left ventricular filling pressures in patients with cardiomyopathies: A simultaneous Doppler echocardiographic and cardiac catheterization study. J Am Coll Cardiol 28(5):1226–1233. https://doi.org/10.1016/S0735-1097(96)00315-4
Zile MR, Gottdiener JS, Hetzel SJ, McMurray JJ, Komajda M, McKelvie R, Baicu CF, Massie BM, Carson PE, Investigators IP (2011) Prevalence and significance of alterations in cardiac structure and function in patients with heart failure and a preserved ejection fraction. Circulation 124(23):2491–2501. https://doi.org/10.1161/CIRCULATIONAHA.110.011031
Shah AM, Shah SJ, Anand IS, Sweitzer NK, O’Meara E, Heitner JF, Sopko G, Li G, Assmann SF, McKinlay SM, Pitt B, Pfeffer MA, Solomon SD, Investigators T (2014) Cardiac structure and function in heart failure with preserved ejection fraction: Baseline findings from the echocardiographic study of the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist trial. Circ Heart Fail 7(1):104–115. https://doi.org/10.1161/CIRCHEARTFAILURE.113.000887
Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM (2010) Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail 3(5):588–595. https://doi.org/10.1161/CIRCHEARTFAILURE.109.930701
Shah SJ, Katz DH, Selvaraj S, Burke MA, Yancy CW, Gheorghiade M, Bonow RO, Huang CC, Deo RC (2015) Phenomapping for novel classification of heart failure with preserved ejection fraction. Circulation 131(3):269–279. https://doi.org/10.1161/CIRCULATIONAHA.114.010637
Cuspidi C, Rescaldani M, Sala C (2013) Prevalence of echocardiographic left-atrial enlargement in hypertension: A systematic review of recent clinical studies. Am J Hypertens 26(4):456–464. https://doi.org/10.1093/ajh/hpt001
Obokata M, Kane GC, Reddy YN, Olson TP, Melenovsky V, Borlaug BA (2017) Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction: A simultaneous invasive-echocardiographic study. Circulation 135(9):825–838. https://doi.org/10.1161/CIRCULATIONAHA.116.024822
Talreja DR, Nishimura RA, Oh JK (2007) Estimation of left ventricular filling pressure with exercise by Doppler echocardiography in patients with normal systolic function: A simultaneous echocardiographic-cardiac catheterization study. J Am Soc Echocardiogr 20(5):477–479. https://doi.org/10.1016/j.echo.2006.10.005
Telles F, Nanayakkara S, Evans S, Patel HC, Mariani JA, Vizi D, William J, Marwick TH, Kaye DM (2019) Impaired left atrial strain predicts abnormal exercise haemodynamics in heart failure with preserved ejection fraction. Eur J Heart Fail. https://doi.org/10.1002/ejhf.1399
Kanagala P, Cheng ASH, Singh A, McAdam J, Marsh AM, Arnold JR, Squire IB, Ng LL, McCann GP (2018) Diagnostic and prognostic utility of cardiovascular magnetic resonance imaging in heart failure with preserved ejection fraction - implications for clinical trials. J Cardiovasc Magn Reson 20(1):4. https://doi.org/10.1186/s12968-017-0424-9
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, Martinez F, Packer M, Pfeffer MA, Pieske B, Redfield MM, Rouleau JL, van Veldhuisen DJ, Zannad F, Zile MR, Desai AS, Claggett B, Jhund PS, Boytsov SA, Comin-Colet J, Cleland J, Dungen HD, Goncalvesova E, Katova T, Kerr Saraiva JF, Lelonek M, Merkely B, Senni M, Shah SJ, Zhou J, Rizkala AR, Gong J, Shi VC, Lefkowitz MP, Investigators P-H, Committees, (2019) Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med 381(17):1609–1620. https://doi.org/10.1056/NEJMoa1908655
Borbely A, van der Velden J, Papp Z, Bronzwaer JG, Edes I, Stienen GJ, Paulus WJ (2005) Cardiomyocyte stiffness in diastolic heart failure. Circulation 111(6):774–781. https://doi.org/10.1161/01.CIR.0000155257.33485.6D
Zile MR, Baicu CF, Ikonomidis JS, Stroud RE, Nietert PJ, Bradshaw AD, Slater R, Palmer BM, Van Buren P, Meyer M, Redfield MM, Bull DA, Granzier HL, LeWinter MM (2015) Myocardial stiffness in patients with heart failure and a preserved ejection fraction: contributions of collagen and titin. Circulation 131(14):1247–1259. https://doi.org/10.1161/CIRCULATIONAHA.114.013215
Miller CA, Naish JH, Bishop P, Coutts G, Clark D, Zhao S, Ray SG, Yonan N, Williams SG, Flett AS, Moon JC, Greiser A, Parker GJ, Schmitt M (2013) Comprehensive validation of cardiovascular magnetic resonance techniques for the assessment of myocardial extracellular volume. Circ Cardiovasc Imaging 6(3):373–383. https://doi.org/10.1161/CIRCIMAGING.112.000192
Schelbert EB, Fridman Y, Wong TC, Abu Daya H, Piehler KM, Kadakkal A, Miller CA, Ugander M, Maanja M, Kellman P, Shah DJ, Abebe KZ, Simon MA, Quarta G, Senni M, Butler J, Diez J, Redfield MM, Gheorghiade M (2017) Temporal relation between myocardial fibrosis and heart failure with preserved ejection fraction: Association with baseline disease severity and subsequent outcome. JAMA Cardiol 2(9):995–1006. https://doi.org/10.1001/jamacardio.2017.2511
Mordi IR, Singh S, Rudd A, Srinivasan J, Frenneaux M, Tzemos N, Dawson DK (2018) Comprehensive echocardiographic and cardiac magnetic resonance evaluation differentiates among heart failure with preserved ejection fraction patients, hypertensive patients, and healthy control subjects. JACC Cardiovasc Imaging 11(4):577–585. https://doi.org/10.1016/j.jcmg.2017.05.022
Rommel KP, von Roeder M, Latuscynski K, Oberueck C, Blazek S, Fengler K, Besler C, Sandri M, Lucke C, Gutberlet M, Linke A, Schuler G, Lurz P (2016) Extracellular volume fraction for characterization of patients with heart failure and preserved ejection fraction. J Am Coll Cardiol 67(15):1815–1825. https://doi.org/10.1016/j.jacc.2016.02.018
Hunter WG, Kelly JP, McGarrah RW, 3rd, Khouri MG, Craig D, Haynes C, Ilkayeva O, Stevens RD, Bain JR, Muehlbauer MJ, Newgard CB, Felker GM, Hernandez AF, Velazquez EJ, Kraus WE, Shah SH (2016) Metabolomic Profiling Identifies Novel Circulating Biomarkers of Mitochondrial Dysfunction Differentially Elevated in Heart Failure With Preserved Versus Reduced Ejection Fraction: Evidence for Shared Metabolic Impairments in Clinical Heart Failure. J Am Heart Assoc 5 (8). https://doi.org/10.1161/JAHA.115.003190
Sabbah HN, Sharov VG, Lesch M, Goldstein S (1995) Progression of heart failure: A role for interstitial fibrosis. Mol Cell Biochem 147(1–2):29–34
Hudsmith LE, Neubauer S (2009) Magnetic resonance spectroscopy in myocardial disease. JACC Cardiovasc Imaging 2(1):87–96. https://doi.org/10.1016/j.jcmg.2008.08.005
Phan TT, Abozguia K, Nallur Shivu G, Mahadevan G, Ahmed I, Williams L, Dwivedi G, Patel K, Steendijk P, Ashrafian H, Henning A, Frenneaux M (2009) Heart failure with preserved ejection fraction is characterized by dynamic impairment of active relaxation and contraction of the left ventricle on exercise and associated with myocardial energy deficiency. J Am Coll Cardiol 54(5):402–409. https://doi.org/10.1016/j.jacc.2009.05.012
Mahmod M, Pal N, Rayner J, Holloway C, Raman B, Dass S, Levelt E, Ariga R, Ferreira V, Banerjee R, Schneider JE, Rodgers C, Francis JM, Karamitsos TD, Frenneaux M, Ashrafian H, Neubauer S, Rider O (2018) The interplay between metabolic alterations, diastolic strain rate and exercise capacity in mild heart failure with preserved ejection fraction: A cardiovascular magnetic resonance study. J Cardiovasc Magn Reson 20(1):88. https://doi.org/10.1186/s12968-018-0511-6
Lewis GA, Schelbert EB, Naish JH, Bedson E, Dodd S, Eccleson H, Clayton D, Jimenez BD, McDonagh T, Williams SG, Cooper A, Cunnington C, Ahmed FZ, Viswesvaraiah R, Russell S, Neubauer S, Williamson PR, Miller CA (2019) Pirfenidone in heart failure with preserved ejection fraction-rationale and design of the PIROUETTE Trial. Cardiovasc Drugs Ther 33(4):461–470. https://doi.org/10.1007/s10557-019-06876-y
van Empel VP, Mariani J, Borlaug BA, Kaye DM (2014) Impaired myocardial oxygen availability contributes to abnormal exercise hemodynamics in heart failure with preserved ejection fraction. J Am Heart Assoc 3(6):e001293. https://doi.org/10.1161/JAHA.114.001293
Paulus WJ, Tschope C (2013) A novel paradigm for heart failure with preserved ejection fraction: Comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol 62(4):263–271. https://doi.org/10.1016/j.jacc.2013.02.092
Srivaratharajah K, Coutinho T, deKemp R, Liu P, Haddad H, Stadnick E, Davies RA, Chih S, Dwivedi G, Guo A, Wells GA, Bernick J, Beanlands R, Mielniczuk LM (2016) Reduced Myocardial Flow in Heart Failure Patients With Preserved Ejection Fraction. Circ Heart Fail 9 (7). https://doi.org/10.1161/CIRCHEARTFAILURE.115.002562
Kato S, Saito N, Kirigaya H, Gyotoku D, Iinuma N, Kusakawa Y, Iguchi K, Nakachi T, Fukui K, Futaki M, Iwasawa T, Kimura K, Umemura S (2016) Impairment of Coronary Flow Reserve Evaluated by Phase Contrast Cine-Magnetic Resonance Imaging in Patients With Heart Failure With Preserved Ejection Fraction. J Am Heart Assoc 5 (2). https://doi.org/10.1161/JAHA.115.002649
Taqueti VR, Solomon SD, Shah AM, Desai AS, Groarke JD, Osborne MT, Hainer J, Bibbo CF, Dorbala S, Blankstein R, Di Carli MF (2018) Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J 39(10):840–849. https://doi.org/10.1093/eurheartj/ehx721
Shah SJ, Lam CSP, Svedlund S, Saraste A, Hage C, Tan RS, Beussink-Nelson L, Fermer ML, Broberg MA, Gan LM, Lund LH (2018) Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J 39(37):3439–3450. https://doi.org/10.1093/eurheartj/ehy531
Olsen RH, Pedersen LR, Snoer M, Christensen TE, Ghotbi AA, Hasbak P, Kjaer A, Haugaard SB, Prescott E (2016) Coronary flow velocity reserve by echocardiography: Feasibility, reproducibility and agreement with PET in overweight and obese patients with stable and revascularized coronary artery disease. Cardiovasc Ultrasound 14(1):22. https://doi.org/10.1186/s12947-016-0066-3
Borlaug BA, Lam CS, Roger VL, Rodeheffer RJ, Redfield MM (2009) Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction. J Am Coll Cardiol 54(5):410–418. https://doi.org/10.1016/j.jacc.2009.05.013
Schwartzenberg S, Redfield MM, From AM, Sorajja P, Nishimura RA, Borlaug BA (2012) Effects of vasodilation in heart failure with preserved or reduced ejection fraction implications of distinct pathophysiologies on response to therapy. J Am Coll Cardiol 59(5):442–451. https://doi.org/10.1016/j.jacc.2011.09.062
Kraigher-Krainer E, Shah AM, Gupta DK, Santos A, Claggett B, Pieske B, Zile MR, Voors AA, Lefkowitz MP, Packer M, McMurray JJ, Solomon SD, Investigators P (2014) Impaired systolic function by strain imaging in heart failure with preserved ejection fraction. J Am Coll Cardiol 63(5):447–456. https://doi.org/10.1016/j.jacc.2013.09.052
Shah AM, Claggett B, Sweitzer NK, Shah SJ, Anand IS, Liu L, Pitt B, Pfeffer MA, Solomon SD (2015) Prognostic importance of impaired systolic function in heart failure with preserved ejection fraction and the impact of spironolactone. Circulation 132(5):402–414. https://doi.org/10.1161/CIRCULATIONAHA.115.015884
Tan YT, Wenzelburger F, Lee E, Heatlie G, Leyva F, Patel K, Frenneaux M, Sanderson JE (2009) The pathophysiology of heart failure with normal ejection fraction: Exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. J Am Coll Cardiol 54(1):36–46. https://doi.org/10.1016/j.jacc.2009.03.037
Wang J, Khoury DS, Yue Y, Torre-Amione G, Nagueh SF (2008) Preserved left ventricular twist and circumferential deformation, but depressed longitudinal and radial deformation in patients with diastolic heart failure. Eur Heart J 29(10):1283–1289. https://doi.org/10.1093/eurheartj/ehn141
Bianco CM, Farjo PD, Ghaffar YA, Sengupta PP (2020) Myocardial Mechanics in patients with normal LVEF and diastolic dysfunction. JACC Cardiovasc Imaging 13(1 Pt 2):258–271. https://doi.org/10.1016/j.jcmg.2018.12.035
Freed BH, Daruwalla V, Cheng JY, Aguilar FG, Beussink L, Choi A, Klein DA, Dixon D, Baldridge A, Rasmussen-Torvik LJ, Maganti K, Shah SJ (2016) Prognostic Utility and Clinical Significance of Cardiac Mechanics in Heart Failure With Preserved Ejection Fraction: Importance of Left Atrial Strain. Circ Cardiovasc Imaging 9 (3). https://doi.org/10.1161/CIRCIMAGING.115.003754
Kurt M, Wang J, Torre-Amione G, Nagueh SF (2009) Left atrial function in diastolic heart failure. Circ Cardiovasc Imaging 2(1):10–15. https://doi.org/10.1161/CIRCIMAGING.108.813071
Cameli M, Lisi M, Righini FM, Massoni A, Natali BM, Focardi M, Tacchini D, Geyer A, Curci V, Di Tommaso C, Lisi G, Maccherini M, Chiavarelli M, Massetti M, Tanganelli P, Mondillo S (2013) Usefulness of atrial deformation analysis to predict left atrial fibrosis and endocardial thickness in patients undergoing mitral valve operations for severe mitral regurgitation secondary to mitral valve prolapse. Am J Cardiol 111(4):595–601. https://doi.org/10.1016/j.amjcard.2012.10.049
Hundley WG, Kitzman DW, Morgan TM, Hamilton CA, Darty SN, Stewart KP, Herrington DM, Link KM, Little WC (2001) Cardiac cycle-dependent changes in aortic area and distensibility are reduced in older patients with isolated diastolic heart failure and correlate with exercise intolerance. J Am Coll Cardiol 38(3):796–802
Weber T, Wassertheurer S, O’Rourke MF, Haiden A, Zweiker R, Rammer M, Hametner B, Eber B (2013) Pulsatile hemodynamics in patients with exertional dyspnea: Potentially of value in the diagnostic evaluation of suspected heart failure with preserved ejection fraction. J Am Coll Cardiol 61(18):1874–1883. https://doi.org/10.1016/j.jacc.2013.02.013
Wilkinson IB, Franklin SS, Cockcroft JR (2004) Nitric oxide and the regulation of large artery stiffness: From physiology to pharmacology. Hypertension 44(2):112–116. https://doi.org/10.1161/01.HYP.0000138068.03893.40
DeVallance E, Fournier S, Lemaster K, Moore C, Asano S, Bonner D, Donley D, Olfert IM, Chantler PD (2016) The effects of resistance exercise training on arterial stiffness in metabolic syndrome. Eur J Appl Physiol 116(5):899–910. https://doi.org/10.1007/s00421-016-3348-4
Kitzman DW, Herrington DM, Brubaker PH, Moore JB, Eggebeen J, Haykowsky MJ (2013) Carotid arterial stiffness and its relationship to exercise intolerance in older patients with heart failure and preserved ejection fraction. Hypertension 61(1):112–119. https://doi.org/10.1161/HYPERTENSIONAHA.111.00163
Kitzman DW, Hundley WG, Brubaker PH, Morgan TM, Moore JB, Stewart KP, Little WC (2010) A randomized double-blind trial of enalapril in older patients with heart failure and preserved ejection fraction: Effects on exercise tolerance and arterial distensibility. Circ Heart Fail 3(4):477–485. https://doi.org/10.1161/CIRCHEARTFAILURE.109.898916
el Ibrahim SH, Johnson KR, Miller AB, Shaffer JM, White RD (2010) Measuring aortic pulse wave velocity using high-field cardiovascular magnetic resonance: Comparison of techniques. J Cardiovasc Magn Reson 12:26. https://doi.org/10.1186/1532-429X-12-26
Chirinos JA (2017) Deep Phenotyping of systemic arterial hemodynamics in HFpEF (part 1): Physiologic and technical considerations. J Cardiovasc Transl Res 10(3):245–259. https://doi.org/10.1007/s12265-017-9735-3
Reddy YNV, Andersen MJ, Obokata M, Koepp KE, Kane GC, Melenovsky V, Olson TP, Borlaug BA (2017) Arterial stiffening with exercise in patients with heart failure and preserved ejection fraction. J Am Coll Cardiol 70(2):136–148. https://doi.org/10.1016/j.jacc.2017.05.029
Chirinos JA, Bhattacharya P, Kumar A, Proto E, Konda P, Segers P, Akers SR, Townsend RR, Zamani P (2019) Impact of diabetes mellitus on ventricular structure, arterial stiffness, and pulsatile hemodynamics in heart failure with preserved ejection fraction. J Am Heart Assoc 8(4):e011457. https://doi.org/10.1161/JAHA.118.011457
Maeder MT, Thompson BR, Brunner-La Rocca HP, Kaye DM (2010) Hemodynamic basis of exercise limitation in patients with heart failure and normal ejection fraction. J Am Coll Cardiol 56(11):855–863. https://doi.org/10.1016/j.jacc.2010.04.040
Tsao CW, Lyass A, Larson MG, Levy D, Hamburg NM, Vita JA, Benjamin EJ, Mitchell GF, Vasan RS (2015) Relation of Central Arterial Stiffness to Incident Heart Failure in the Community. J Am Heart Assoc 4 (11). https://doi.org/10.1161/JAHA.115.002189
Upadhya B, Hundley WG, Brubaker PH, Morgan TM, Stewart KP, Kitzman DW (2017) Effect of spironolactone on exercise tolerance and arterial function in older adults with heart failure with preserved ejection fraction. J Am Geriatr Soc 65(11):2374–2382. https://doi.org/10.1111/jgs.14940
Jumean MF, Konstam MA (2015) Heart failure with preserved ejection fraction: What is in a name? Cardiol Rev 23(4):161–167. https://doi.org/10.1097/CRD.0000000000000057
Solomon SD, Rizkala AR, Gong J, Wang W, Anand IS, Ge J, Lam CSP, Maggioni AP, Martinez F, Packer M, Pfeffer MA, Pieske B, Redfield MM, Rouleau JL, Van Veldhuisen DJ, Zannad F, Zile MR, Desai AS, Shi VC, Lefkowitz MP, McMurray JJV (2017) Angiotensin receptor neprilysin inhibition in heart failure with preserved ejection fraction: Rationale and design of the PARAGON-HF trial. JACC Heart Fail 5(7):471–482. https://doi.org/10.1016/j.jchf.2017.04.013
Anker SD, Butler J, Filippatos GS, Jamal W, Salsali A, Schnee J, Kimura K, Zeller C, George J, Brueckmann M, Zannad F, Packer M, Committees EM-PT, Investigators, (2019) Evaluation of the effects of sodium-glucose co-transporter 2 inhibition with empagliflozin on morbidity and mortality in patients with chronic heart failure and a preserved ejection fraction: Rationale for and design of the EMPEROR-Preserved Trial. Eur J Heart Fail 21(10):1279–1287. https://doi.org/10.1002/ejhf.1596
Gottdiener JS, Fohner AE (2020) Risk prediction in heart failure: New methods. Old Problems JACC Heart Fail 8(1):22–24. https://doi.org/10.1016/j.jchf.2019.08.015
Garcia MJ, Ares MA, Asher C, Rodriguez L, Vandervoort P, Thomas JD (1997) An index of early left ventricular filling that combined with pulsed Doppler peak E velocity may estimate capillary wedge pressure. J Am Coll Cardiol 29(2):448–454. https://doi.org/10.1016/s0735-1097(96)00496-2
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA (1997) Doppler tissue imaging: A noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30(6):1527–1533
Firstenberg MS, Levine BD, Garcia MJ, Greenberg NL, Cardon L, Morehead AJ, Zuckerman J, Thomas JD (2000) Relationship of echocardiographic indices to pulmonary capillary wedge pressures in healthy volunteers. J Am Coll Cardiol 36(5):1664–1669. https://doi.org/10.1016/s0735-1097(00)00909-8
Nagueh SF, Mikati I, Kopelen HA, Middleton KJ, Quinones MA, Zoghbi WA (1998) Doppler estimation of left ventricular filling pressure in sinus tachycardia A new application of tissue doppler imaging. Circulation 98(16):1644–1650. https://doi.org/10.1161/01.cir.98.16.1644
Oki T, Tabata T, Yamada H, Wakatsuki T, Shinohara H, Nishikado A, Iuchi A, Fukuda N, Ito S (1997) Clinical application of pulsed Doppler tissue imaging for assessing abnormal left ventricular relaxation. Am J Cardiol 79(7):921–928. https://doi.org/10.1016/s0002-9149(97)00015-5
Schwammenthal E, Popescu BA, Popescu AC, Di Segni E, Kaplinsky E, Rabinowitz B, Guetta V, Rath S, Feinberg MS (2000) Noninvasive assessment of left ventricular end-diastolic pressure by the response of the transmitral a-wave velocity to a standardized Valsalva maneuver. Am J Cardiol 86(2):169–174. https://doi.org/10.1016/s0002-9149(00)00855-9
Appleton CP, Hatle LK, Popp RL (1988) Relation of transmitral flow velocity patterns to left ventricular diastolic function: New insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol 12(2):426–440. https://doi.org/10.1016/0735-1097(88)90416-0
Kasner M, Westermann D, Steendijk P, Gaub R, Wilkenshoff U, Weitmann K, Hoffmann W, Poller W, Schultheiss HP, Pauschinger M, Tschope C (2007) Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: A comparative Doppler-conductance catheterization study. Circulation 116(6):637–647. https://doi.org/10.1161/CIRCULATIONAHA.106.661983
Garcia MJ, Firstenberg MS, Greenberg NL, Smedira N, Rodriguez L, Prior D, Thomas JD (2001) Estimation of left ventricular operating stiffness from Doppler early filling deceleration time in humans. Am J Physiol Heart Circ Physiol 280(2):H554-561. https://doi.org/10.1152/ajpheart.2001.280.2.H554
Kim YJ, Sohn DW (2000) Mitral annulus velocity in the estimation of left ventricular filling pressure: Prospective study in 200 patients. J Am Soc Echocardiogr 13(11):980–985. https://doi.org/10.1067/mje.2000.107156
Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, Lee MM, Park YB, Choi YS, Seo JD, Lee YW (1997) Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 30(2):474–480
Sohn DW, Song JM, Zo JH, Chai IH, Kim HS, Chun HG, Kim HC (1999) Mitral annulus velocity in the evaluation of left ventricular diastolic function in atrial fibrillation. J Am Soc Echocardiogr 12(11):927–931
Kasner M, Sinning D, Burkhoff D, Tschope C (2015) Diastolic pressure-volume quotient (DPVQ) as a novel echocardiographic index for estimation of LV stiffness in HFpEF. Clin Res Cardiol 104(11):955–963. https://doi.org/10.1007/s00392-015-0863-y
Bouchard JL, Aurigemma GP, Hill JC, Ennis CA, Tighe DA (2008) Usefulness of the pulmonary arterial systolic pressure to predict pulmonary arterial wedge pressure in patients with normal left ventricular systolic function. Am J Cardiol 101(11):1673–1676. https://doi.org/10.1016/j.amjcard.2008.01.054
McQuillan BM, Picard MH, Leavitt M, Weyman AE (2001) Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation 104(23):2797–2802. https://doi.org/10.1161/hc4801.100076
Galie N, Torbicki A, Barst R, Dartevelle P, Haworth S, Higenbottam T, Olschewski H, Peacock A, Pietra G, Rubin LJ, Simonneau G, Priori SG, Garcia MA, Blanc JJ, Budaj A, Cowie M, Dean V, Deckers J, Burgos EF, Lekakis J, Lindahl B, Mazzotta G, McGregor K, Morais J, Oto A, Smiseth OA, Barbera JA, Gibbs S, Hoeper M, HumbertNaeije MR, Pepke-Zaba J, Task F (2004) Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J 25(24):2243–2278. https://doi.org/10.1016/j.ehj.2004.09.014
Tsang TS, Barnes ME, Gersh BJ, Bailey KR, Seward JB (2002) Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol 90(12):1284–1289. https://doi.org/10.1016/s0002-9149(02)02864-3
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing G, American Society of Echocardiography’s G, Standards E European Association of C (2005) Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18(12):1440–1463. https://doi.org/10.1016/j.echo.2005.10.005
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22(2):107–133. https://doi.org/10.1016/j.echo.2008.11.023
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28 (1):1–39 e14. https://doi.org/10.1016/j.echo.2014.10.003
Raff GL, Glantz SA (1981) Volume loading slows left ventricular isovolumic relaxation rate. Evidence of load-dependent relaxation in the intact dog heart. Circ Res 48(6):813–824. https://doi.org/10.1161/01.res.48.6.813
Weiss JL, Frederiksen JW, Weisfeldt ML (1976) Hemodynamic determinants of the time-course of fall in canine left ventricular pressure. J Clin Invest 58(3):751–760. https://doi.org/10.1172/JCI108522
Funding
Dr Lewis is funded by a fellowship grant from the National Institute for Health Research. Dr Miller is funded by a Clinician Scientist Award (CS-2015-15-003) from the National Institute for Health Research. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Author information
Authors and Affiliations
Contributions
GAL wrote the manuscript with CAM. KP, SGW, EBS and AM provided critical review. All authors approved the final manuscript.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lewis, G.A., Pearce, K., Williams, S.G. et al. The utility of cardiovascular imaging in heart failure with preserved ejection fraction: diagnosis, biological classification and risk stratification. Heart Fail Rev 26, 661–678 (2021). https://doi.org/10.1007/s10741-020-10047-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-020-10047-9