Abstract
Pulmonary arterial hypertension (PAH) is a progressive disease primarily affecting the pulmonary vasculature and heart. PAH patients suffer from exercise intolerance and fatigue, negatively affecting their quality of life. This review summarizes current insights in the pathophysiological mechanisms underlying PAH. It zooms in on the potential involvement of nutritional status and micronutrient deficiencies on PAH exercise intolerance and fatigue, also summarizing the potential benefits of exercise and nutritional interventions. Pubmed/Medline, Scopus, and Web of Science were searched for publications on pathophysiological mechanisms of PAH negatively affecting physical activity potential and nutritional status, and for potential effects of interventions involving exercise or nutritional measures known to improve exercise intolerance. Pathophysiological processes that contribute to exercise intolerance and impaired quality of life of PAH patients include right ventricular dysfunction, inflammation, skeletal muscle alterations, and dysfunctional energy metabolism. PAH-related nutritional deficiencies and metabolic alterations have been linked to fatigue, exercise intolerance, and endothelial dysfunction. Available evidence suggests that exercise interventions can be effective in PAH patients to improve exercise tolerance and decrease fatigue. By contrast, knowledge on the prevalence of micronutrient deficiencies and the possible effects of nutritional interventions in PAH patients is limited. Although data on nutritional status and micronutrient deficiencies in PAH are scarce, the available knowledge, including that from adjacent fields, suggests that nutritional intervention to correct deficiencies and metabolic alterations may contribute to a reduction of disease burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary arterial hypertension (PAH) is a progressive disease affecting the arteries of the lungs. It is defined by a mean pulmonary artery pressure ≥ 25 mmHg at rest, an end-expiratory pulmonary artery wedge pressure (PAWP) ≤ 15 mmHg, and a pulmonary vascular resistance > 3 Wood units. There are different etiologies suggested for PAH, as the disease can (1) develop idiopathically (without a known cause); (2) be heritable (e.g., result from inherited mutations in genes coding for specific proteins like bone morphogenic protein receptor 2); (3) be associated with certain diseases like connective tissue disease, congenital heart disease, portal hypertension, or HIV; or (4) be induced by drugs or toxins [1]. The prevalence of all types of PAH in Europe is estimated to be in the range of 15–100 cases per million population. Prognosis of PAH is poor, with 1- and 3-year survival rates of 87 and 67%, respectively [1, 2]. The guidelines for the diagnosis and treatment of pulmonary hypertension from the European Society of Cardiology (ESC) and the European Respiratory Society (ERS) describe several risk stratification criteria for determination of prognosis of PAH patients (1-year mortality) [1]. Predictors of poor prognosis include advanced functional class, poor exercise capacity, and right ventricular dysfunction [1]. In heart failure (CHF) patients, right ventricular dysfunction and exercise intolerance are known to contribute to muscle wasting [3]. Many of the clinical characteristics of PAH such as heart failure, exercise intolerance, functional class, muscle wasting, and comorbidities are strongly associated with each other. These characteristics have also been taken along in the REVEAL score, which has been developed to predict disease progression and survival of PAH patients using prognostic criteria [4].
Malnutrition and muscle wasting are known clinical manifestations of cachexia, which is often seen in PAH as well [5]. Cachexia as such also contributes to a higher mortality risk and poorer quality of life [3, 6]. At the same time, there appears to be hardly any knowledge on the relevance of nutritional status in PAH. For those readers less familiar with some of the terminology used, Box 1 provides some formal definitions of cachexia, sarcopenia, and nutritional and micronutrient deficiency [7]. Interestingly, in case of CHF, which to some degree shows overlapping pathology with PAH, nutritional supplementation with fish oil, rich in n-3 fatty acids, has shown to improve disease progression. In addition, increased protein intake has proven to be effective in attenuating muscle wasting in CHF patients [8]. Specifically in PAH patients, iron deficiency is known to have a negative impact on exercise tolerance and fatigue [1, 9]. With this in mind, we hypothesize that nutrition impacts disease progression and quality of life in case of PAH as well. Furthermore, we envisage an opportunity to improve predictive modeling and quality of life for PAH by including nutritional status as a factor. Given the clinical manifestations of PAH, it is expected that effects resulting from optimizing nutritional status of PAH patients will at least include improved maintenance of muscle mass and function and ultimately quality of life.
The pathophysiology of PAH involves endothelial dysfunction in the pulmonary vasculature, metabolic shifts in vascular cells, hypertrophy and proliferation of smooth muscle cells, and unprogrammed growth of neointimal, medial, and adventitial layers, leading to thickening and occlusion of the small- and medium-sized pulmonary arteries [10]. Three known pathways involved in PAH are currently used as therapeutic targets. These are the endothelin pathway, the nitric oxide pathway, and the prostacyclin pathway [11]. Current therapies consist of endothelin receptor antagonists (ERAs), phosphodiesterase 5 (PDE5) inhibitors, a soluble guanylate cyclase (sGC) agonist, prostacyclin, prostacyclin analogues, and a selective IP receptor agonist [1]. These compounds aim to reduce pulmonary vascular resistance, provide relief of symptoms, enhance exercise capacity, and delay disease progression, but do not cure the disease once it has started. Therefore, additional treatment options for this incurable disease are clearly needed. Among these, treating muscle dysfunction, enhancing physical activity potential, and decreasing fatigue could be of great importance. Exercise programs, psycho-social support, and dietary consultation are offered to PAH patients depending on local availability, insurance coverage, and laws and regulations. However, there is little information about nutritional status or daily activity of PAH patients, or about possible strategies to increase the quality of life of patients by means of nutritional or lifestyle interventions. The ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension [1] contain very limited nutritional and lifestyle recommendations. Therefore, this review aims to gather the information on nutritional status, physical performance, and activity levels of PAH patients. In addition, clinical outcomes of previously investigated nutrition and lifestyle interventions are discussed.
Evidence-based nutrition and exercise interventions for PAH are limited, but established lifestyle interventions for CHF might be useful for PAH patients as well based on the similarities in pathophysiology. The 2016 Guidelines of the European Society of Cardiology (ESC) recommend regular aerobic exercise training in patients with heart failure and stable heart failure with reduced ejection fraction to improve functional capacity and reduce the risk of hospitalization (class I, level A recommendation) [12]. Nutritional advice for heart failure includes avoiding excessive salt intake (> 6 g/day) and fluid restriction in case of severe heart failure [8, 12]. Supplementation of omega-3 polyunsaturated fatty acids (N3 PUFA) has shown beneficial effects on mortality and hospitalization in patients with heart failure. Furthermore, high-caloric, protein-rich nutritional supplements or branched-chain amino acids can be beneficial in case of muscle wasting or cachexia [8]. Further research is needed to investigate whether these recommendations are also beneficial for PAH patients.
Methods
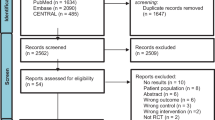
We used Pubmed/Medline, Scopus, and Web of Science to search for publications connecting the pathophysiological mechanisms of PAH to impaired physical activity, exercise intolerance, chronic fatigue, and nutritional deficiencies often observed in patients with PAH. We also searched for nutritional and exercise interventions to prevent or modulate these symptoms. For the literature search, we used specific combinations of the following search terms: pulmonary arterial hypertension, PAH, pathophysiology, symptoms, mechanism, right ventricular failure, skeletal muscle alterations, inflammation, hypoxia, dysfunctional energy metabolism, lipid accumulation, insulin resistance, satiety hormones, nutritional status, nutrition, deficiency, vitamin, mineral, protein, lipid, fatty acid, carbohydrate, iron, magnesium, calcium, vitamin D, omega 3 fatty acids, omega-3 PUFA, docosahexaenoic acid (DHA), eicasopentaenoic acid (EPA), alpha-linolenic acid (ALA), activity, daily activity, lifestyle, exercise tolerance, exercise capacity, exercise intervention, and quality of life.
Activity level and physical performance of PAH patients
A limited number of studies available underline the prevailing clinical idea that activity levels of patients decline with disease progression [2, 13, 14]. A study using accelerometry to estimate activity levels in 23 PAH and chronic thromboembolic pulmonary hypertension (CTEPH) patients found a relationship between activity and disease severity. Severely impaired patients (mean pulmonary arterial pressure (mPAP) 50 ± 7 mmHg) were inactive for longer periods during the night, and were less active during the day than modestly impaired patients (mPAP 33 ± 7 mmHg) [13]. Long nocturnal rest and reduced activity during the day were also reported to correlate with an overall poorer prognosis [13]. Another study showed that PAH patients spent significantly more time in sedentary activities than matched healthy controls and that this impacted all levels of physical activity [14]. A more recent paper of Alami et al. supports these findings, reporting that patients with PAH experience such an increase in symptoms like shortness of breath and fatigue that they have increased problems performing normal daily tasks such as body care, household chores, parenting, and leisure activities during progression of the disease [2]. There are currently more studies underway using activity tracking, such as the wearable wrist device Actigraph, which enables better recording of the activity pattern of PAH patients and the impact of treatment on activity levels (e.g., the TRACE study, clinicaltrials.gov identifier NCT03078907).
Nutritional status of PAH patients
PAH eventually leads to right heart failure, which is found to contribute to loss of skeletal muscle mass [3, 6]. Loss of skeletal muscle is a strong predictor of death in (left) heart failure patients [15]. Next, loss of skeletal muscle mass is often accompanied with loss of weight and fat mass [3, 6]. Muscle loss in general, diagnosed as sarcopenia or sometimes as cachexia, is related to a worsened prognosis and lower quality of life of chronically ill patients [8, 16]. The Society on Sarcopenia, Cachexia and Wasting Disorders (SCWD) defines cachexia as “a loss of lean tissue mass, involving a weight loss greater than 5% of body weight in 12 months or less in the presence of chronic illness or as a body mass index (BMI) lower than 20 kg/m2.” Often, three of the following five criteria are also required: decreased muscle strength, fatigue, anorexia, low fat-free mass index, an increase of inflammation markers, anemia, or low serum albumin [7]. Sarcopenia focuses on muscle loss and is defined as “loss of muscle mass and function, especially muscle strength and gait speed, associated with aging” [7] (see also Box 1). Improving nutritional status during the earliest stages of chronic diseases such as heart failure is an important factor in reducing the rate at which muscle wasting develops. Despite this, only few studies have investigated nutritional status in PAH.
In 2015, Kawamoto showed a close relationship between PAH with inferior vena cava (IVC) dilatation, poor nutritional status, and low BMI in a small prospective study with 8 PAH patients [3]. An older, cross-sectional study with 20 heart failure patients showed that these patients have an 18% higher resting metabolic rate and risk to develop sarcopenia than healthy age-matched controls [17]. Based on the similarities in pathophysiology, it could be hypothesized that PAH patients also have an increase in energy expenditure, although future studies will have to confirm this. Furthermore, drugs used to treat PAH, specifically epoprostenol, prostacyclin analogues, and other drugs that target the prostacyclin pathway, are known to induce side effects that may impact nutritional status and exercise tolerance: nausea, loss of appetite, vomiting, diarrhea, jaw pain, musculoskeletal pain, and fatigue [2].
Disease-related characteristics influencing daily activity or nutritional status
Right ventricular failure
In PAH patients, the pulmonary vascular system is obstructed and less elastic, which leads to an increased afterload of the right ventricle with decreased right ventricular cardiac output [18,19,20]. This, in turn, decreases the left ventricular preload which leads to a decreased left ventricular output. The decreased left ventricular output causes a reduced oxygen supply to the muscles both at rest and during exercise, contributing to exercise intolerance [21,22,23,24,25]. In addition to a reduced cardiac output, it has been suggested that PAH is associated with impaired chronotropic capacity [18, 26], which is associated with downregulation of β-adrenoreceptor activity in the right ventricle [27]. These effects prevent adequate adaptation of cardiac output and systemic blood pressure during exercise, which can further contribute to exercise intolerance. The pathological changes in the heart and other organs and their contribution to exercise intolerance are well described elsewhere [28], and include cardiac factors (right ventricular function), skeletal muscle dysfunction (decreased oxidative enzymes, reduced muscle fiber size), pulmonary factors (endothelial dysfunction, arterial stiffness), and other factors (e.g., inflammation and oxidative stress). Based on this, it is clear that right ventricular failure plays an important role in the exercise intolerance often found in PAH patients and that the responsible pathophysiological changes are relatively well studied.
Skeletal muscle alterations
Multiple causes of reduced daily activity of PAH patients have been proposed. In addition to shortness of breath and fatigue, skeletal and respiratory muscle alterations have also been described. These include a switch from type I fiber to type II fiber in skeletal muscle, increased muscle protein degradation, a reduced muscle capillary density, lower aerobic enzyme activity, mitochondrial abnormalities, and impaired calcium homeostasis [29,30,31,32]. The cross-sectional area and force-generating capacity of muscle cells from the left ventricle have been reported to be reduced by 30 and 25%, respectively [33]. Furthermore, forearm muscle weakness was found to correlate with respiratory muscle strength and exercise capacity, independent of hemodynamic severity in a prospective study with 24 idiopathic PAH (IPAH) patients (66% female) [34]. Pathological changes and reduced strength in the diaphragm muscle of PAH patients or in animal models of PH have been found by several authors [35,36,37]. The changes in the diaphragm muscle might be different from those in skeletal muscle. Instead of a type I to type II fiber switch as seen in skeletal muscle, a switch from type II fiber to type I fiber was observed in the diaphragm of animal models of heart failure [38, 39]. Alterations in the skeletal and respiratory muscles contribute to exercise intolerance in PAH patients. Whether changes in fiber type in skeletal and respiratory muscles in models of PAH are different (as was found in animal models of heart failure) remains to be studied. There is also a lack of studies into the potential effect of lifestyle interventions such as nutrition or exercise on skeletal muscle alterations in PAH.
Inflammation
Altered immune function and chronic inflammation are increasingly recognized features of PAH [10, 40,41,42]. In PAH patients, an accumulation of perivascular inflammatory cells including mast cells, macrophages, dendritic cells, and T and B lymphocytes has been found in the pulmonary vasculature and lung tissue [43]. In addition, chronically elevated serum levels of the proinflammatory cytokines IL-1b, IL-6, IL-8, IL-10, MCP-1, fractalkine, CCL5/RANTES, and TNF-α and chemokines have been reported [19, 42, 43]. Inflammatory conditions such as connective tissue diseases are associated with increased incidence of PAH, indicating that inflammation might play a significant role in the development and progression of PAH [19, 42]. This is supported by findings that in PAH patients, inflammation is associated with worse clinical outcome [43, 44].
Inflammatory cytokines such as IL-6 and TNF-α are known to impact nutritional status and to induce muscle wasting in other chronic diseases [45, 46]. Inflammation induces muscle protein breakdown via multiple mechanisms, such as via increased protein degradation through the ubiquitin-proteasome system (UPS), mitochondrial dysfunction, and autophagy [45,46,47]. The role of inflammation on mitochondrial dysfunction in chronic heart failure seems twofold: IL-6 has been shown to prevent mitochondrial dysfunction in cardiomyocytes, whereas TNF-α induces mitochondrial dysfunction in the same cell type [48]. It has been found that TNF-α worsens endothelial function in CHF, causing a decreased blood supply to other organs such as the skeletal muscle and the gut. As a consequence, less nutrients are absorbed from the gut and transported to other organs. At the same time, IL-6 induces the acute phase inflammatory response, which requires essential amino acids. Skeletal muscle is an important source of essential amino acids when delivery via the food is limited. Therefore, more skeletal muscle is broken down [47]. TNF-α, IL-6, and other inflammatory cytokines induce transcription of atrogenes, such as MuRF1 and MAFbx/Atrogin-1, via FOXO transcription factors. The E3-ubiquitin ligases MuRF-1 and MAFbx/Atrogin-1 are the main ligases in skeletal muscle that identify proteins for removal via the UPS. The UPS gets activated, which leads to increased protein degradation [45]. Proinflammatory cytokines such as TNF-α and IL-1 also inhibit food intake via an anorexigenic effect in the brain [49].
Based on this information, it can be hypothesized that inflammation decreases the nutritional status of PAH patients and that it can induce muscle wasting or cachexia. This, in turn, supposedly augments the response to inflammation. In this way, a vicious cycle can develop that can only be interrupted when both inflammation and nutritional status are targeted at the same time [50,51,52]. Further research is needed to investigate to what extent alterations in immune function and inflammatory processes observed in PAH could affect nutritional status and whether nutritional supplementation might alter the inflammatory process in PAH.
Dysfunctional cellular energy metabolism
Oxygen is important for mitochondrial ATP production via oxidative phosphorylation. In PAH patients, abnormalities in energy production, heme synthesis, and mitochondrial function have been hypothesized to result from chronic hypoxia [9, 53].
A factor important for these impairments is hypoxia-inducible factor 1α (HIF-1α): a hypoxia-sensitive transcription factor. Under normoxic circumstances, HIF-1α is very unstable and rapidly degraded. Under chronic hypoxic conditions, as occurring in PAH patients, HIF-1α stabilizes and moves to the nucleus to induce expression of HIF target genes [54]. Expression of these genes promotes the delivery of oxygen to tissues and maintenance of ATP levels [55]. However, chronic activation of HIF also induces proteins that alter energy metabolism and cell proliferation and cause vascular remodeling, resulting in the development of pulmonary arterial remodeling and pulmonary hypertension [54]. HIF-1α activates glycolytic genes, increasing the production of lactate from pyruvate, and inactivates enzymes necessary for mitochondrial oxidative phosphorylation [56]. This process is known as aerobic glycolysis and often leads to an energy deficit [56, 57]. An increase in lactate levels might even suppress food intake, because lactate has an appetite-inhibiting effect [58]. The production of high amounts of lactate could also contribute to dysfunction of the right ventricle [59]. Due to the metabolic shift from oxidative to glycolytic metabolism, the mitochondrial membrane gets hyperpolarized, leading to proliferation of pulmonary artery smooth muscle cells (PASMC) and reduced apoptosis. This process may contribute to the development of pulmonary hypertension [56].
Other factors that could contribute to mitochondrial dysfunction in PAH are deficiencies in caveolin-1 and mutations in BMPRII. Mutated BMPRII shifts glucose metabolism of pulmonary arterial endothelial cells (PAECs) to anaerobic glycolysis, causing decreased ATP production, mitochondrial DNA damage, and apoptosis of endothelial cells [56]. A deficiency in caveolin-1 leads to activation of endothelial nitric oxide synthase (eNOS) and the development of ROS, also contributing to impaired mitochondrial functioning [56].
Both hypoxia and a decrease in cellular ATP can induce muscle breakdown and dysfunction which further reduces the exercise capacity of the patient [29].
In summary, due to chronic hypoxia present in PAH, there are changes in mitochondrial energy metabolism that lead to inefficient ATP production in the cells. Lactate, which occurs as a side product of aerobic glycolysis, might contribute to right ventricular dysfunction and potentially leads to a reduced dietary intake, thereby negatively influencing the clinical status of the patient. However, future studies have to test this hypothesis. A lower cellular ATP production might also induce muscle breakdown and dysfunction itself, although more studies to support this hypothesis are needed.
Lipid accumulation
In the healthy human heart, the major source of energy (60–90%) is provided by fatty acid oxidation (FAO). The other 10–40% mainly comes from glucose oxidation [59]. In PAH patients, due to the Warburg effect, glucose utilization in the heart increases, while FAO is reduced. Despite this, there is an increase in uptake of fatty acids by the fatty acid (FA) transporter CD36 [60, 61]. Lipid accumulation in cardiomyocytes and skeletal muscle cells is therefore a common feature in PAH patients [62]. Cytosolic accumulation of FA leads to a more abundant production of long-chain acyl-CoA in the cytoplasm, which can be converted into intracellular lipid intermediates, such as triglycerides, diacylglycerol, and ceramides, causing cardiac lipotoxicity. These intermediates induce insulin resistance due to multiple mechanisms, such as impairing pyruvate dehydrogenase (PDH), inhibiting insulin receptor substrate 1 (IRS-1) and glucose transporter type 4 (GLUT4) expression [60]. Next to insulin resistance, the lipid intermediates are also related to the development of cardiac dysfunction and right heart failure [60]. Insulin resistance is related to skeletal muscle weakness in CHF patients, although it is unclear whether this relationship is causal [63].
Cardiac dysfunction and right heart failure lead to fatigue and hypoxia, both of which contribute to exercise intolerance. This altogether leads to muscle protein breakdown. The combination of immobility and the inability to use fat can lead to a sarcopenic obesity phenotype (high BMI, low muscle mass), a malnourished phenotype that is also more and more encountered in cancer [64] and is associated with increased morbidity and mortality in this disease. Based on the above-described mechanisms and cause-effect relationships between lipid intermediates, insulin resistance, and skeletal muscle weakness, the prevalence of sarcopenic obesity in PAH patients needs further investigation.
Insulin resistance
A higher prevalence of insulin resistance has been reported in PAH patients than in the general population, and this may be a disease modifier or risk factor for PAH [65,66,67,68]. Insulin resistance is known to be a risk factor for cardiovascular disease (CVD) in general. It has been linked to diseases that share pathophysiological characteristics with PAH such as idiopathic cardiomyopathy or congestive heart failure [65]. Inflammatory cytokines, seen in the pathogenesis of PAH, are likely to contribute to insulin resistance [69]. Obesity in PAH patients may contribute to the development of insulin resistance if coupled with low daily activity levels [65], but insulin resistance has been found independently of obesity in PAH patients as well [66]. In general, insulin resistance induces energy deficit in the muscle, which triggers muscle protein breakdown. From this, it becomes clear that there are many observed associations between insulin resistance and PAH, but little is known about whether it is a symptom of, or a contributing factor to, the disease. More research is needed to show whether insulin or glucose levels play a role in the pathophysiology of PAH and whether it contributes to a loss of muscle mass in PAH patients.
Gut-derived satiety hormones
Deregulations in the expression of satiety hormones, such as increased levels of the anorexigenic hormone PYY after a meal, have been found in a small study with nine cardiac cachectic patients with primary PAH [5]. In addition to its systemic effects, PYY reduces the digestion rate by decreasing GI motility, gall bladder emptying, and gastric emptying, which further contributes to a reduction in food intake [70]. Larger trials should show whether an increase in the anorexigenic hormone PYY or changes in other gut-derived satiety hormones after a meal contribute to reduced food intake in PAH patients.
Disease-related nutritional deficiencies and intervention trials investigating their possible connection to quality of life
Iron deficiency
Iron deficiency is common in patients with idiopathic and heritable forms of PAH. The prevalence has been estimated to be between 30 and 65%, dependent on the type of PAH and status of the patient [1, 9, 71, 72]. Iron deficiency is defined by reduced serum iron (normal = 9.0–30.0 μmol/L), serum ferritin (normal = 3–400 μg/L (males), 30–150 μg/L (females)), and transferrin saturation (normal = 16–45%) [73]. In patients with IPAH, a low iron status has been related to a reduced exercise capacity, measured as the 6-min walk test, and to poorer survival [9, 74]. Iron deficiency was reported to be independent of the presence of anemia [9, 72, 75] and not associated with a worsened right ventricle function [76].
Availability of iron influences the pulmonary vasoconstrictor response to hypoxia and the basal pulmonary artery pressure [77, 78]. Iron status influences modulation of the pulmonary circulation, but also myocardial and skeletal muscle function. Iron is essential for oxygen transport and functions as a cofactor in several mitochondrial oxidative enzymes and the respiratory chain. Inhibition of dietary iron uptake by the negative regulator of plasma iron levels, hepcidin, might form a mechanism behind the iron deficiency. The main iron transporter of the intestine (ferroportin) is inhibited by hepcidin, resulting in a decreased intestinal absorption of iron. Hepcidin levels are higher in patients with PAH. Moreover, a low intestinal absorption of iron is supported by reports that the response to oral iron supplementation is low in PAH patients [71, 74]. High hepcidin levels might be due to dysfunctional BMPRII signaling and/or the presence of chronic inflammation. Normally, high hepatic iron levels induce bone morphogenic protein 6 (BMP6) expression, which stimulates hepcidin transcription via BMP response elements 1 and 2 (BMP-RE1 and BMP-RE2) on the hepcidin gene. Inflammatory cytokines such as IL-1beta and IL-6 stimulate hepcidin transcription via different mechanisms, leading to excessive hepcidin production. IL-1beta might even provide the onset signal, as it induces the transcription of IL-6. This excessive hepcidin production also happens when there are no high hepatic iron levels present and thereby leads to inflammation-induced anemia [79].
In summary, iron deficiency is common in PAH patients and contributes to the disease itself and to exercise intolerance by influencing the pulmonary circulation, myocardial and skeletal muscle function, and oxidative energy metabolism. High levels of hepcidin, induced by inflammatory cytokines and/or dysfunctional BMPRII signaling, lead to inhibition of dietary iron uptake.
Iron supplementation
The response to oral iron supplementation in PAH patients is low, which is likely due to inhibition of iron uptake by hepcidin in the digestive tract [71, 74]. Therefore, more recent studies investigated the effect of intravenous infusion of iron in the form of ferric carboxymaltose. For example, Viethen et al. and Ruiter et al. studied the effect of a single dose of 1000 mg ferric carboxymaltose. They used observation periods of 8 and 12 weeks in 20 and 15 PAH patients, respectively [73, 74]. Both studies found improvement of serum iron status and quality of life, as measured by the patient-reported Short Form 36 (SF-36) questionnaire, and showed minimal side effects. The study of Viethen et al. also found an improvement in the 6-min walk distance (6MWD), whereas Ruiter and colleagues did not, although they did find improved endurance exercise capacity and mitochondrial oxidative capacity [73, 74]. A larger study into the effects of parenteral iron replacement in at least 60 patients with IPAH is underway (The “Supplementation of Iron in Pulmonary Hypertension” (SIPHON) Phase II clinical trial) [80]. More randomized controlled trials are needed to show whether parenteral iron replacement is more successful in treating iron deficiency than oral iron supplementation and if this leads to a better quality of life of PAH patients.
Vitamin D
Vitamin D deficiency is linked to musculoskeletal, metabolic, and cardiopulmonary diseases and to disorders of the immune system [81, 82]. It has been suggested that vitamin D influences smooth muscle cell proliferation and endothelial function, which are both affected in PAH [81, 83, 84]. Pulmonary hypertension was associated with vitamin D3 deficiency in a group of 40 systemic sclerosis patients [84]. In a small prospective uncontrolled longitudinal study, weekly supplementation of 50,000 IU cholecalciferol (vitamin D3) plus a daily dose of 200 mg magnesium, 8 mg zinc, and 400 IU vitamin D for a 3-month period has been found to significantly increase the serum vitamin D level and 6MWD in 22 patients with pulmonary hypertension and vitamin D deficiency. It also led to improvements in right ventricle size and function [81]. While the evidence from this single study is limited, it does show an interesting potential of correcting vitamin D deficiencies to improve the quality of life of PAH patients. Further rigorously conducted randomized trials into the effect of vitamin D supplementation should confirm potential effects on the right ventricle, exercise tolerance, and quality of life.
Exercise interventions
In the past, exercise training was not recommended in patients with PAH. It was thought that exercise could be a major risk due to increased blood flow, a drop in cardiac output that may worsen right ventricular function or risk of arrhythmia and hypoxia [85,86,87]. However, more and more studies now show that exercise training can actually be safe and beneficial for exercise capacity, peak oxygen capacity, systemic pulmonary artery pressure, heart rate, and quality of life of patients with various forms of pulmonary hypertension [88,89,90,91,92].
There are different kinds of exercise training that are used in cardiac and pulmonary diseases: (1) aerobic exercise training, like cycling or walking; (2) strength training; and (3) respiratory exercise training [88]. Respiratory training often consists of body perception, yoga, and respiratory muscle strengthening exercises [85]. Although yoga and meditative breathing have been mentioned as possible interventions, studies exclusively examining these interventions were so small that no conclusions can be drawn from them [93].
Studies on exercise training in PAH patients were almost exclusively done in medically stable patients. González-Saiz and colleagues found that aerobic, inspiratory, and muscle resistance training during a short intervention period of 8 weeks can improve muscle power and strength in PAH patients. Also, peak VO2 was improved by this exercise intervention [94].
Others found that the combination of aerobic exercise and education can improve fatigue and daily activity, while this effect was not found when giving education only [95].
Different reviews have been published that summarize the effect of exercise interventions combining aerobic exercise, resistance exercise, and/or respiratory training during periods of 3–15 weeks. Sessions were often performed between 2 and 5 times per week. Among others, improvements have been found in 6MWD, fatigue, peak VO2, QoL, increased amount of capillaries per muscle fiber, mean pulmonary blood volume, lower resting heart rate, and increased strength of different muscles (including the respiratory muscles) [86,87,88, 96,97,98].
Researchers also reported mild exercise-related adverse events, like dizziness, desaturation, progressive fatigue towards the end of the training period, (pre-)syncope, and supraventricular tachycardia in about 5% of the participants [96, 97]. It has been found that fainting during exercise could be triggered in PAH patients when doing isometric exercise training. Therefore, these authors recommended not to imply isometric exercise in training schedules [87].
According to the Pulmonary Hypertension Association (PHA), PAH patients should seek advice regarding safe exercise training from their doctor before starting to exercise. The PHA recommendations for exercise in patients with PAH state that patients should not overexercise to the point of dizziness, chest pain, or severe shortness of breath. Recommended forms of exercise are light resistance training of small muscle groups (without heavy lifting) and light to moderate aerobic activity, such as walking or swimming. For symptomatic PAH patients, it is not advised to exercise the upper and lower body at the same time. Patients with severe exercise intolerance or those with a history of fainting or dizziness are not advised to continue or start a regular exercise program. Lastly, exercise is better avoided during extreme weather circumstances such as very hot or cold temperatures [99].
Discussion and conclusion
Nutritional status is likely to be impaired in patients with PAH due to an increased energetic demand, increased protein catabolism, and congestion of the splanchnic organs [2, 3, 17]. The effect and potential side effects of exercise interventions in PAH patients are relatively well studied. Although the pathophysiology of PAH involves many mechanisms that may influence nutritional status and may induce muscle wasting (see Fig. 1), potentially limiting the effect of exercise interventions, there is only little scientific knowledge about the nutritional status of PAH patients and the way this may impact physical activity.
We found no data on the general nutritional status and only limited data on the daily activity of PAH patients. Although deficiencies in micronutrients such as vitamin D, vitamin B12, iron, or magnesium might influence symptoms of fatigue and quality of life, there are only few studies into the prevalence of such nutritional deficiencies in PAH patients. Next to micronutrient deficiencies, the presence of insulin resistance is a sign of metabolic change and can also contribute to feelings of fatigue. All of these nutritional deficiencies and metabolic changes can be monitored and treated.
Although it is being recognized that oral iron supplementation in iron-deficient PAH patients is ineffective, there is limited insight in alternative treatments. There are only few studies on the effect of intravenous iron substitution in PAH patients to reduce iron deficiency. Current studies are relatively small with a sample size of 15–20 subjects. Data of a larger study that is currently being performed have not been published yet. Studies on the effect of micronutrients such as vitamin D supplementation in PAH patients are rare and small in size, and study designs can be improved. Chronic inflammation is an important feature in the pathophysiology of PAH, but the effect of nutritional intervention on the inflammation status of these patients is unknown. High-quality papers on the effect of treatments to reduce adverse effects of medication that impact nutritional status are lacking. It should also not be forgotten that physical inactivity itself induces skeletal muscle atrophy [100], so prevention of becoming inactive in the first place should receive extra clinical attention.
In conclusion, larger and well-designed studies into the nutritional status of PAH patients, the prevalence of micronutrient deficiencies, and the effect of supplementation strategies to reduce these deficiencies and improve the quality of life of PAH patients are needed.
References
Galiè N, Humbert M, Vachiéry J-L, Gibbs S, Lang I, Torbicki A et al (2015) 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 37:67–119. https://doi.org/10.1093/eurheartj/ehv317
Alami S, Cottin V, Mouthon L, Desjeux D, Quessette E, Poiraudeau S, Sitbon O (2016) Patients’, relatives’, and practitioners’ views of pulmonary arterial hypertension: a qualitative study. Presse Med 45:e11–e27. https://doi.org/10.1016/j.lpm.2015.06.017
Kawamoto A, Kato T, Minamino-Muta E, Okano Y, Shioi T, Kimura T (2015) Relationships between nutritional status and markers of congestion in patients with pulmonary arterial hypertension. Int J Cardiol 187:27–28. https://doi.org/10.1016/j.ijcard.2015.03.354
Benza RL, Gomberg-Maitland M, Miller DP, Frost A, Frantz RP, Foreman AJ, Badesch DB, McGoon MD (2012) The REVEAL registry risk score calculator in patients newly diagnosed with pulmonary arterial hypertension. Chest 141:354–362. https://doi.org/10.1378/chest.11-0676
Le Roux CW, Ghatei MA, Gibbs JSR, Bloom SR (2005) The putative satiety hormone PYY is raised in cardiac cachexia associated with primary pulmonary hypertension. Heart 91:241–242. https://doi.org/10.1136/hrt.2003.026880
Valentova M, Von Haehling S, Krause C, Ebner N, Steinbeck L, Cramer L, Doehner W, Murin J, Anker SD, Sandek A (2013) Cardiac cachexia is associated with right ventricular failure and liver dysfunction. Int J Cardiol 169:219–224. https://doi.org/10.1016/j.ijcard.2013.08.134
Society on Sarcopenia Cachexia and Wasting Disorders (2018) Definition of cachexia and sarcopenia. http://society-scwd.org/cachexia-definition/. Accessed 15 May 2018
von Haehling S, Ebner N, dos Santos MR, Springer J, Anker SD (2017) Muscle wasting and cachexia in heart failure: mechanisms and therapies. Nat Rev Cardiol 14:323–341. https://doi.org/10.1038/nrcardio.2017.51
Ruiter G, Lankhorst S, Boonstra A, Postmus PE, Zweegman S, Westerhof N, Van Der Laarse WJ, Vonk-Noordegraaf A (2011) Iron deficiency is common in idiopathic pulmonary arterial hypertension. Eur Respir J 37:1386–1391. https://doi.org/10.1183/09031936.00100510
de Jesus Perez VA (2016) Molecular pathogenesis and current pathology of pulmonary hypertension. Heart Fail Rev 21:239–257. https://doi.org/10.1007/s10741-015-9519-2
Humbert M, Lau EM, Montani D, Jaïs X, Sitbon OSG (2014) Advances in therapeutic interventions for patients with pulmonary arterial hypertension. Circulation 130:2189–2208. https://doi.org/10.1161/CIRCULATIONAHA.114.006974
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 37:2129–2200m . doi: https://doi.org/10.1093/eurheartj/ehw128, 2200
Ulrich S, Fischler M, Speich R, Bloch KE (2013) Wrist actigraphy predicts outcome in patients with pulmonary hypertension. Respiration 86:45–51. https://doi.org/10.1159/000342351
Pugh ME, Buchowski MS, Robbins IM, Newman JH, Hemnes AR (2012) Physical activity limitation as measured by accelerometry in pulmonary arterial hypertension. Chest 142:1391–1398. https://doi.org/10.1378/chest.12-0150
Anker SD, Ponikowski P, Varney S, Chua TP, Clark AL, Webb-Peploe KM, Harrington D, Kox WJ, Poole-Wilson PA, Coats AJ (1997) Wasting as independent risk factor for mortality in chronic heart failure. Lancet (London, England) 349:1050–1053. https://doi.org/10.1016/S0140-6736(96)07015-8
Loncar G, Springer J, Anker M, Doehner W, Lainscak M (2016) Cardiac cachexia: hic et nunc. J Cachexia Sarcopenia Muscle 7:246–260. https://doi.org/10.1002/jcsm.12118
Poehlman ET (1994) Increased resting metabolic rate in patients with congestive heart failure. Ann Intern Med 121:860–862. https://doi.org/10.7326/0003-4819-121-11-199412010-00006
Provencher S, Chemla D, Hervé P, Sitbon O, Humbert M, Simonneau G (2006) Heart rate responses during the 6-minute walk test in pulmonary arterial hypertension. Eur Respir J Off J Eur Soc Clin Respir Physiol 27:114–120. https://doi.org/10.1183/09031936.06.00042705
Humbert M, Morrell NW, Archer SL, Stenmark KR, MacLean MR, Lang IM, Christman BW, Weir EK, Eickelberg O, Voelkel NF, Rabinovitch M (2004) Cellular and molecular pathobiology of pulmonary arterial hypertension. J Am Coll Cardiol 43:S13–S24. https://doi.org/10.1016/j.jacc.2004.02.029
Sutendra G, Michelakis ED (2014) The metabolic basis of pulmonary arterial hypertension. Cell Metab 19:558–573. https://doi.org/10.1016/j.cmet.2014.01.004
Holverda S, Gan CT-J, Marcus JT, Postmus PE, Boonstra A, Vonk-Noordegraaf A (2006) Impaired stroke volume response to exercise in pulmonary arterial hypertension. J Am Coll Cardiol 47:1732–1733. https://doi.org/10.1016/j.jacc.2006.01.048
Laskey WK, Ferrari VA, Palevsky HI, Kussmaul WG (1993) Pulmonary artery hemodynamics in primary pulmonary hypertension. J Am Coll Cardiol 21:406–412. https://doi.org/10.1016/0735-1097(93)90682-Q
Nootens M, Wolfkiel CJ, Chomka EV, Rich S (1995) Understanding right and left ventricular systolic function and interactions at rest and with exercise in primary pulmonary hypertension. Am J Cardiol 75:374–377. https://doi.org/10.1016/S0002-9149(99)80557-8
Xing-Guo Sun MD, James E, Hansen MD, Ronald J, Oudiz MD, Karlman Wasserman MDP (2001) Exercise pathophysiology in patients with primary pulmonary hypertension. Circulation 104:429–435
Riley MS, Pórszász J, Engelen MPKJ, Brundage BH, Wasserman K (2000) Gas exchange responses to continuous incremental cycle ergometry exercise in primary pulmonary hypertension in humans. Eur J Appl Physiol 83:63–70. https://doi.org/10.1007/s004210000240
Deboeck G, Niset G, Lamotte M, Vachiery JL, Naeije R, Vachie J (2004) Exercise testing in pulmonary arterial hypertension and in chronic heart failure. Eur Respir J 23:747–751. https://doi.org/10.1183/09031936.04.00111904
Bristow MR, Minobe W, Rasmussen R, Larrabee P, Skerl L, Klein JW, Anderson FL, Murray J, Mestroni L, Karwande SV, Fowler M, Ginsburg R (1992) β-Adrenergic neuroeffector abnormalities in the failing human heart are produced by local rather than systemic mechanisms. J Clin Invest 89:803–815. https://doi.org/10.1172/JCI115659
Tran DL, Lau EMT, Celermajer DS, Davis GM, Cordina R (2018) Pathophysiology of exercise intolerance in pulmonary arterial hypertension. Respirology 23:148–159. https://doi.org/10.1111/resp.13141
Marra AM, Arcopinto M, Bossone E, Ehlken N, Cittadini A, Grünig E (2015) Pulmonary arterial hypertension-related myopathy: an overview of current data and future perspectives. Nutr Metab Cardiovasc Dis 25:131–139. https://doi.org/10.1016/j.numecd.2014.10.005
Tonelli AR, Plana JC, Heresi GA, Dweik RA (2012) Prevalence and prognostic value of left ventricular diastolic dysfunction in idiopathic and heritable pulmonary arterial hypertension. Chest 141:1457–1465. https://doi.org/10.1378/chest.11-1903
Malenfant S, Potus F, Mainguy V, Leblanc E, Malenfant M, FRna R, Saey D, Maltais F, Bonnet S, Provencher S (2015) Impaired skeletal muscle oxygenation and exercise tolerance in pulmonary hypertension. Med Sci Sports Exerc 47:2273–2282. https://doi.org/10.1249/MSS.0000000000000696
Mainguy V, Maltais F, Saey D, Gagnon P, Martel S, Simon M, Provencher S (2010) Peripheral muscle dysfunction in idiopathic pulmonary arterial hypertension. Thorax 65:113–117. https://doi.org/10.1136/thx.2009.117168
Manders E, Bogaard H-J, Handoko ML, van de Veerdonk MC, Keogh A, Westerhof N, Stienen GJM, Dos Remedios CG, Humbert M, Dorfmüller P, Fadel E, Guignabert C, van der Velden J, Vonk-Noordegraaf A, de Man FS, Ottenheijm CAC (2014) Contractile dysfunction of left ventricular cardiomyocytes in patients with pulmonary arterial hypertension. J Am Coll Cardiol 64:28–37. https://doi.org/10.1016/j.jacc.2014.04.031
Bauer R, Dehnert C, Schoene P, Filusch A, Bärtsch P, Borst MM, Katus HA, Joachim Meyer F (2007) Skeletal muscle dysfunction in patients with idiopathic pulmonary arterial hypertension. Respir Med 101:2366–2369. https://doi.org/10.1016/j.rmed.2007.06.014
Meyer FJ, Lossnitzer D, Kristen AV, Schoene AM, Kübler W, Katus HA, Borst MM (2005) Respiratory muscle dysfunction in idiopathic pulmonary arterial hypertension. Eur Respir J 25:125–130. https://doi.org/10.1183/09031936.04.00095804
de Man FS, van Hees HWH, Handoko ML, Niessen HW, Schalij I, Humbert M, Dorfmüller P, Mercier O, Bogaard H-J, Postmus PE, Westerhof N, Stienen GJM, van der Laarse WJ, Vonk-Noordegraaf A, Ottenheijm CAC (2011) Diaphragm muscle fiber weakness in pulmonary hypertension. Am J Respir Crit Care Med 183:1411–1418. https://doi.org/10.1164/rccm.201003-0354OC
Manders E, Bonta PI, Kloek JJ, Symersky P, Bogaard H-J, Hooijman PE, Jasper JR, Malik FI, Stienen GJM, Vonk-Noordegraaf A, de Man FS, Ottenheijm CAC (2016) Reduced force of diaphragm muscle fibers in patients with chronic thromboembolic pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 311:L20–L28. https://doi.org/10.1152/ajplung.00113.2016
Bowen TS, Brauer D, Rolim NPL, Bækkerud FH, Kricke A, Ormbostad Berre AM, Fischer T, Linke A, da Silva GJ, Wisloff U, Adams V (2017) Exercise training reveals inflexibility of the diaphragm in an animal model of patients with obesity-driven heart failure with a preserved ejection fraction. J Am Heart Assoc 6:e006416. https://doi.org/10.1161/JAHA.117.006416
Mangner N, Weikert B, Scott Bowen T, Sandri M, Höllriegel R, Erbs S, Hambrecht R, Schuler G, Linke A, Gielen S, Adams V (2015) Skeletal muscle alterations in chronic heart failure: differential effects on quadriceps and diaphragm. J Cachexia Sarcopenia Muscle 6:381–390. https://doi.org/10.1002/jcsm.12034
Cracowski J-L, Chabot F, Labarère J, Faure P, Degano B, Schwebel C, Chaouat A, Reynaud-Gaubert M, Cracowski C, Sitbon O, Yaici A, Simonneau G, Humbert M (2014) Proinflammatory cytokine levels are linked to death in pulmonary arterial hypertension. Eur Respir J 43:915–917. https://doi.org/10.1183/09031936.00151313
Hassoun PM (2014) Inflammation in pulmonary arterial hypertension: is it time to quell the fire? Eur Respir J 43:685–688. https://doi.org/10.1183/09031936.00006014
Price LC, Wort SJ, Perros F, Dorfmüller P, Huertas A, Montani D, Cohen-Kaminsky S, Humbert M (2012) Inflammation in pulmonary arterial hypertension. Chest 141:210–221. https://doi.org/10.1378/chest.11-0793
Rabinovitch M, Guignabert C, Humbert M, Nicolls MR (2014) Inflammation and immunity in the pathogenesis of pulmonary arterial hypertension. Circ Res 115:165–175. https://doi.org/10.1161/CIRCRESAHA.113.301141
Krause L, Becker MO, Brueckner CS, Bellinghausen C-J, Becker C, Schneider U, Haeupl T, Hanke K, Hensel-Wiegel K, Ebert H, Ziemer S, Ladner U-M, Pirlich M, Burmester GR, Riemekasten G (2010) Nutritional status as marker for disease activity and severity predicting mortality in patients with systemic sclerosis. Ann Rheum Dis 69:1951–1957. https://doi.org/10.1136/ard.2009.123273
Bowen TS, Schuler G, Adams V (2015) Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J Cachexia Sarcopenia Muscle 6:197–207. https://doi.org/10.1002/jcsm.12043
von Haehling S, Lainscak M, Springer J, Anker SD (2009) Cardiac cachexia: a systematic overview. Pharmacol Ther 121:227–252. https://doi.org/10.1016/j.pharmthera.2008.09.009
von Haehling S, Doehner W, Anker SD (2007) Nutrition, metabolism, and the complex pathophysiology of cachexia in chronic heart failure. Cardiovasc Res 73:298–309. https://doi.org/10.1016/j.cardiores.2006.08.018
Rosca MG, Hoppel CL (2013) Mitochondrial dysfunction in heart failure. Heart Fail Rev 18:607–622. https://doi.org/10.1007/s10741-012-9340-0
Langhans W, Hrupka B (1999) Interleukins and tumor necrosis factor as inhibitors of food intake. Neuropeptides 33:415–424
Don BR, Kaysen G (2004) Serum albumin: relationship to inflammation and nutrition. Semin Dial 17:432–437
McMillan DC (2009) Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care 12:223–226. https://doi.org/10.1097/MCO.0b013e32832a7902
Laveneziana P, Palange P (2012) Physical activity, nutritional status and systemic inflammation in COPD. Eur Respir J 40:522–529
Archer SL, Fang Y-H, Ryan JJ, Piao L (2013) Metabolism and bioenergetics in the right ventricle and pulmonary vasculature in pulmonary hypertension. Pulm Circ 3:144–152. https://doi.org/10.4103/2045-8932.109960
Veith C, Schermuly RT, Brandes RP, Weissmann N (2016) Molecular mechanisms of hypoxia-inducible factor-induced pulmonary arterial smooth muscle cell alterations in pulmonary hypertension. J Physiol 594:1167–1177. https://doi.org/10.1113/JP270689
Mateo J, García-Lecea M, Cadenas S, Hernández C, Moncada S (2003) Regulation of hypoxia-inducible factor-1alpha by nitric oxide through mitochondria-dependent and -independent pathways. Biochem J 376:537–544. https://doi.org/10.1042/BJ20031155
Peng H, Xiao Y, Deng X, Luo J, Hong C, Qin X (2016) The Warburg effect: a new story in pulmonary arterial hypertension. Clin Chim Acta 461:53–58. https://doi.org/10.1016/j.cca.2016.07.017
Liu N, Parry S, Xiao Y, Zhou S, Liu Q (2017) Molecular targets of the Warburg effect and inflammatory cytokines in the pathogenesis of pulmonary artery hypertension. Clin Chim Acta 466:98–104. https://doi.org/10.1016/j.cca.2017.01.015
Bray GA (2000) Afferent signals regulating food intake. Proc Nutr Soc 59:373–384. https://doi.org/10.1017/S0029665100000422
Ryan JJ, Archer SL (2014) The right ventricle in pulmonary arterial hypertension: disorders of metabolism, angiogenesis and adrenergic signaling in right ventricular failure. Circ Res 115:176–188. https://doi.org/10.1161/CIRCRESAHA.113.301129
Talati M, Hemnes A (2015) Fatty acid metabolism in pulmonary arterial hypertension: role in right ventricular dysfunction and hypertrophy. Pulm Circ 5:269–278. https://doi.org/10.1086/681227.Pulmonary
Talati MH, Brittain EL, Fessel JP, Penner N, Atkinson J, Funke M, Grueter C, Jerome WG, Freeman M, Newman JH, West J, Hemnes AR (2016) Mechanisms of lipid accumulation in the bone morphogenetic protein receptor type 2 mutant right ventricle. Am J Respir Crit Care Med 194:719–728. https://doi.org/10.1164/rccm.201507-1444OC
Brittain EL, Talati M, Fessel JP, Zhu H, Penner N, Calcutt MW, West JD, Funke M, Lewis GD, Gerszten RE, Hamid R, Pugh ME, Austin ED, Newman JH, Hemnes AR (2016) Fatty acid metabolic defects and right ventricular lipotoxicity in human pulmonary arterial hypertension. Circulation 133:1936–1944. https://doi.org/10.1161/CIRCULATIONAHA.115.019351
Doehner W, Turhan G, Leyva F, Rauchhaus M, Sandek A, Jankowska EA, Von HS, Anker SD (2015) Skeletal muscle weakness is related to insulin resistance in patients with chronic heart failure. ESC Hear Fail 2:85–89. https://doi.org/10.1002/ehf2.12035
Carneiro IP, Mazurak VC, Prado CM (2016) Clinical implications of sarcopenic obesity in cancer. Curr Oncol Rep 18(62):62. https://doi.org/10.1007/s11912-016-0546-5
Zamanian RT, Hansmann G, Snook S, Lilienfeld D, Rappaport M, Reaven GM, Rabinovitch M, Doyle RL (2010) Insulin resistance in pulmonary arterial hypertension. Eur Respir J 33:318–324. https://doi.org/10.1183/09031936.00000508.Insulin
Pugh ME, Robbins IM, Rice TW, West J, Newman JH, Hemnes AR (2011) Unrecognized glucose intolerance is common in pulmonary arterial hypertension. J Hear Lung Transplant 30:904–911. https://doi.org/10.1016/j.healun.2011.02.016
Naderi N, Boobejame P, Bakhshandeh H, Amin A, Taghavi S, Maleki M (2014) Insulin resistance in pulmonary arterial hypertension, is it a novel disease modifier? Res Cardiovasc Med 3:e19710. https://doi.org/10.5812/cardiovascmed.19710
Hansmann G, Wagner RA, Schellong S, Perez VADJ, Urashima T, Wang L, Sheikh AY, Suen RS, Stewart DJ, Rabinovitch M (2007) Pulmonary arterial hypertension is linked to insulin resistance and reversed by peroxisome proliferator-activated receptor-gamma activation. Circulation 115:1275–1284. https://doi.org/10.1161/CIRCULATIONAHA.106.663120
Paulin R, Michelakis ED (2014) The metabolic theory of pulmonary arterial hypertension. Circ Res 115:148–164. https://doi.org/10.1161/CIRCRESAHA.115.301130
Luttikhold J, De Ruijter FM, Van Norren K, Diamant M, Witkamp RF, Van Leeuwen PAM, Vermeulen MAR (2013) Review article: the role of gastrointestinal hormones in the treatment of delayed gastric emptying in critically ill patients. Aliment Pharmacol Ther 38:573–583. https://doi.org/10.1111/apt.12421
Rhodes CJ, Wharton J, Howard L, Gibbs JSR, Vonk-Noordegraaf A, Wilkins MR (2011) Iron deficiency in pulmonary arterial hypertension: a potential therapeutic target. Eur Respir J 38:1453–1460. https://doi.org/10.1183/09031936.00037711
Soon E, Treacy CM, Toshner MR, MacKenzie-Ross R, Manglam V, Busbridge M, Sinclair-McGarvie M, Arnold J, Sheares KK, Morrell NW, Pepke-Zaba J (2011) Unexplained iron deficiency in idiopathic and heritable pulmonary arterial hypertension. Thorax 66:326–332. https://doi.org/10.1136/thx.2010.147272
Viethen T, Gerhardt F, Dumitrescu D, Knoop-Busch S, Ten Freyhaus H, Rudolph TK, Baldus S, Rosenkranz S (2014) Ferric carboxymaltose improves exercise capacity and quality of life in patients with pulmonary arterial hypertension and iron deficiency: a pilot study. Int J Cardiol 175:233–239. https://doi.org/10.1016/j.ijcard.2014.04.233
Ruiter G, Manders E, Happé CM, Schalij I, Groepenhoff H, Howard LS, Wilkins MR, Bogaard HJ, Westerhof N, van der Laarse WJ, de Man FS, Vonk-Noordegraaf A (2015) Intravenous iron therapy in patients with idiopathic pulmonary arterial hypertension and iron deficiency. Pulm Circ 5:466–472. https://doi.org/10.1086/682217
Robinson JC, Graham BB, Rouault TC, Tuder RM (2014) The crossroads of iron with hypoxia and cellular metabolism: implications in the pathobiology of pulmonary hypertension. Am J Respir Cell Mol Biol 51:721–729. https://doi.org/10.1165/rcmb.2014-0021TR
Van Empel VPM, Lee J, Williams TJ, Kaye DM (2014) Iron deficiency in patients with idiopathic pulmonary arterial hypertension. Hear Lung Circ 23:287–292. https://doi.org/10.1016/j.hlc.2013.08.007
Smith TG, Balanos GM, Croft QPP, Talbot NP, Dorrington KL, Ratcliffe PJ, Robbins PA (2008) The increase in pulmonary arterial pressure caused by hypoxia depends on iron status. J Physiol 586:5999–6005. https://doi.org/10.1113/jphysiol.2008.160960
Balanos GM, Dorrington KL, Robbins PA (2002) Desferrioxamine elevates pulmonary vascular resistance in humans: potential for involvement of HIF-1. J Appl Physiol 92:2501–2507. https://doi.org/10.1152/japplphysiol.00965.2001
Kanamori Y, Murakami M, Sugiyama M, Hashimoto O, Matsui T, Funaba M (2017) Interleukin-1β (IL-1β) transcriptionally activates hepcidin by inducing CCAAT enhancer-binding protein δ (C/EBPδ) expression in hepatocytes. J Biol Chem 292:10275–10287. https://doi.org/10.1074/jbc.M116.770974
Howard LSGE, Watson GMJ, Wharton J, Rhodes CJ, Chan K, Khengar R, Robbins PA, Kiely DG, Condliffe R, Elliott CA, Pepke-Zaba J, Sheares K, Morrell NW, Davies R, Ashby D, Gibbs JSR, Wilkins MR (2013) Supplementation of iron in pulmonary hypertension: rationale and design of a phase II clinical trial in idiopathic pulmonary arterial hypertension. Pulm Circ 3:100–107. https://doi.org/10.4103/2045-8932.109923
Mirdamadi A, Moshkdar P (2016) Benefits from the correction of vitamin D deficiency in patients with pulmonary hypertension. Casp J Intern Med 7:253–259
Zittermann A (2003) Vitamin D in preventive medicine: are we ignoring the evidence? Br J Nutr 89:552–572. https://doi.org/10.1079/BJN2003837
Demir M, Uyan U, Keçeoçlu S, Demir C (2013) The relationship between vitamin D deficiency and pulmonary hypertension. Prague Med Rep 114:154–161. https://doi.org/10.14712/23362936.2014.17
Atteritano M, Santoro D, Corallo G, Visalli E, Buemi M, Catalano A, Lasco A, Bitto A, Squadrito F (2016) Skin involvement and pulmonary hypertension are associated with vitamin D insufficiency in scleroderma. Int J Mol Sci 17:1–8. https://doi.org/10.3390/ijms17122103
Madonna R, De Caterina R, Geng Y-J (2016) Aerobic exercise-related attenuation of arterial pulmonary hypertension: a right arrow targets the disease? Vasc Pharmacol 87:6–9. https://doi.org/10.1016/j.vph.2016.10.002
Arena R, Cahalin LP, Borghi-Silva A, Myers J (2015) The effect of exercise training on the pulmonary arterial system in patients with pulmonary hypertension. Prog Cardiovasc Dis 57:480–488. https://doi.org/10.1016/j.pcad.2014.03.008
Zafrir B (2013) Exercise training and rehabilitation in pulmonary arterial hypertension. J Cardiopulm Rehabil Prev 33:263–273. https://doi.org/10.1097/HCR.0b013e3182a0299a
Chia KSW, Wong PKK, Faux SG, McLachlan CS, Kotlyar E (2017) The benefit of exercise training in pulmonary hypertension: a clinical review. Intern Med J 47:361–369. https://doi.org/10.1111/imj.13159
Becker-Grünig T, Klose H, Ehlken N, Lichtblau M, Nagel C, Fischer C, Gorenflo M, Tiede H, Schranz D, Hager A, Kaemmerer H, Miera O, Ulrich S, Speich R, Uiker S, Grünig E (2013) Efficacy of exercise training in pulmonary arterial hypertension associated with congenital heart disease. Int J Cardiol 168:375–381. https://doi.org/10.1016/j.ijcard.2012.09.036
Grünig E, Lichtblau M, Ehlken N, Ghofrani HA, Reichenberger F, Staehler G, Halank M, Fischer C, Seyfarth HJ, Klose H, Meyer A, Sorichter S, Wilkens H, Rosenkranz S, Opitz C, Leuchte H, Karger G, Speich R, Nagel C (2012) Safety and efficacy of exercise training in various forms of pulmonary hypertension. Eur Respir J 40:84–92. https://doi.org/10.1183/09031936.00123711
Grünig E, Maier F, Ehlken N, Fischer C, Lichtblau M, Blank N, Fiehn C, Stöckl F, Prange F, Staehler G, Reichenberger F, Tiede H, Halank M, Seyfarth H-J, Wagner S, Nagel C (2012) Exercise training in pulmonary arterial hypertension associated with connective tissue diseases. Arthritis Res Ther 14:R148. https://doi.org/10.1186/ar3883
Grünig E, Ehlken N, Ghofrani A, Staehler G, Meyer FJ, Juenger J, Opitz CF, Klose H, Wilkens H, Rosenkranz S, Olschewski H, Halank M (2011) Effect of exercise and respiratory training on clinical progression and survival in patients with severe chronic pulmonary hypertension. Respiration 81:394–401. https://doi.org/10.1159/000322475
Awdish R, Small B, Cajigas H (2015) Development of a modified yoga program for pulmonary hypertension: a case series. Altern Ther Health Med 21:48–52
González-Saiz L, Fiuza-Luces C, Sanchis-Gomar F, Santos-Lozano A, Quezada-Loaiza CA, Flox-Camacho A, Munguía-Izquierdo D, Ara I, Santalla A, Morán M, Sanz-Ayan P, Escribano-Subías P, Lucia A (2017) Benefits of skeletal-muscle exercise training in pulmonary arterial hypertension: the WHOLEi+12 trial. Int J Cardiol 231:277–283. https://doi.org/10.1016/j.ijcard.2016.12.026
Weinstein AA, Chin LMK, Keyser RE, Kennedy M, Nathan SD, Woolstenhulme JG, Connors G, Chan L (2013) Effect of aerobic exercise training on fatigue and physical activity in patients with pulmonary arterial hypertension. Respir Med 107:778–784. https://doi.org/10.1016/j.rmed.2013.02.006
Babu AS, Padmakumar R, Maiya AG, Mohapatra AK, Kamath RL (2016) Effects of exercise training on exercise capacity in pulmonary arterial hypertension: a systematic review of clinical trials. Hear Lung Circ 25:333–341. https://doi.org/10.1016/j.hlc.2015.10.015
Pandey A, Garg S, Khunger M, Garg S, Kumbhani DJ, Chin KM, Berry JD (2015) Efficacy and safety of exercise training in chronic pulmonary hypertension: systematic review and meta-analysis. Circ Hear Fail 8:1032–1043. https://doi.org/10.1161/CIRCHEARTFAILURE.115.002130
Buys R, Avila A, Cornelissen VA (2015) Exercise training improves physical fitness in patients with pulmonary arterial hypertension: a systematic review and meta-analysis of controlled trials. BMC Pulm Med 15:40. https://doi.org/10.1186/s12890-015-0031-1
Pulmonary Hypertension Association (2008) Recommendations for exercise in patients with PAH. In: Recomm. Exerc. Patients with PAH. https://phassociation.org/medicalprofessionals/consensusstatements/exercise/. Accessed 15 May 2018
D’Antona G, Pellegrino MA, Adami R, Rossi R, Carlizzi CN, Canepari M, Saltin B, Bottinelli R (2003) The effect of ageing and immobilization on structure and function of human skeletal muscle fibres. J Physiol 552:499–511. https://doi.org/10.1113/jphysiol.2003.046276
Acknowledgements
We thank Shani Sela and Roos Verstegen for their assistance in the literature search for this review and Marianne Geleijnse and T. Scott Bowen for their critical comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Paulien Vinke, MSc, received financial support from Actelion Pharmaceuticals BV The Netherlands to perform the literature study and write the manuscript for this paper. Dr. Suzanne M. Jansen is an employee of Actelion Pharmaceuticals BV The Netherlands. Dr. Klaske van Norren and Prof. Dr. Renger F. Witkamp have no conflicts of interest or financial ties to disclose.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Vinke, P., Jansen, S.M., Witkamp, R.F. et al. Increasing quality of life in pulmonary arterial hypertension: is there a role for nutrition?. Heart Fail Rev 23, 711–722 (2018). https://doi.org/10.1007/s10741-018-9717-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-018-9717-9