Abstract
Both clear cell renal carcinoma (ccRCC) and clear cell carcinoma of the ovary (CCOC) have a clear cytoplasmic morphological feature, hence it is difficult to identify metastatic ccRCC and CCOC by morphology alone. At present, there are no effective immunohistochemical markers to distinguish between these two tumors. Studies have shown that the clear cytoplasm of ccRCC is mainly caused by cholesterol-rich lipids in the cytoplasm, while that of CCOC is due to the accumulation of cytoplasmic glycogen. Objective: to hypothesize that the scavenger receptor class B-type 1 (SR-B1) protein responsible for HDL cholesterol uptake may be differentially expressed in ccRCC and CCOC, and high CD10 expression in the renal tubular epithelium may assist in distinguishing between ccRCC and CCOC. Methods: effective immunohistochemical markers were applied in 90 cases of renal clear cell carcinoma and 31 cases of ovarian cancer to distinguish between the two types of tumors.Result: SR-B1 and CD10 expression is significantly higher in ccRCC than CCOC. Both SR-B1 and CD10 exhibited focal weak-medium intensity staining in CCOC, and their staining extent and intensity were significantly lower than ccRCC. The sensitivity and specificity of SR-B1 for identifying ccRCC were 74.4% and 83.9%, respectively. The sensitivity and specificity of CD10 for identifying CCOC were 93.3% and 80.6%, respectively. The combined SR-B1( +) CD10( +) immunoprofile supports the diagnosis of ccRCC with a specificity of 93.5%. The combined SR-B1(-) CD10(-) immunoprofile supports the diagnosis of CCOC with a specificity of 93.3%. Conclusions: our findings demonstrate that the combination of SR-B1 and CD10 immunoprofiling is a valuable tool for differential diagnosis of ccRCC and CCOC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clear cell renal cell carcinoma (ccRCC) is the most common malignant tumor of the renal parenchyma. The incidence of ccRCC is increasing every year with an average annual rate of 2%, and approximately 20% to 30% of patients with ccRCC have recurrence or metastasis within 3 years after surgery (NCCN Guidelines® 2019). Clear cell carcinoma of the ovary (CCOC) is characterized by resistance to conventional chemotherapy, early recurrence, and a poor prognosis (Gulec et al. 2015; Sugiyama et al. 2000) CCOC and ccRCC share morphological similarities such as a clear cytoplasm, and tubular, flaky or papillary structures. Moreover both tumors express PAX8, a transcription factor normally expressed by cells of the nephric, thyroid, and Mullerian duct lineage (Köbel et al. 2016) Consequently, distinguishing between CCOC and metastatic ccRCC to the ovary based on histomorphology alone is challenging. Thus far, there is a lack of effective immunohistochemical markers for differentiating these two tumors. Recent studies have shown that CCOC and ccRCC show different metabolism characteristics. The cytoplasmic transparency of ccRCC is mainly due to the large amount of cytoplasmic cholesterol ester (Gebhard et al. 1987; Tosi et al. 2004), while the clear cytoplasm of CCOC is more likely due to the accumulation of cytoplasmic glycogen (Tavassoli and Devilee 2003), suggesting that different energy metabolism characteristics may assist in a differential diagnosis.
Scavenger receptor class B type 1 (SR-B1), also known as HDL receptor, is a glycoprotein located on the surface of cell membranes, and the only molecule that acts on the selective absorption of HDL cholesterol ester. Our previous studies have found that SR-B1 is highly expressed in ccRCC and promotes tumor proliferation and invasion; however, the expression of SR-B1 in CCOC has not been examined. In addition, CD10, a marker of the renal tubular epithelium is highly expressed in ccRCC (Fletcher et al. 2013), but the expression of CD10 in CCOC has not been determined. We hypothesize that the SR-B1 protein is differentially expressed in ccRCC and CCOC, and a combined immunoprofiling of SR-B1 and CD10 will assist in the differential diagnosis of these two cancers.
Materials and methods
Tumor specimens
The 90 cases of ccRCC (collected from 1974 to 2013) used in this study were provided by the Department of Pathology, the First Affiliated Hospital of Shihezi University School of Medicine. The 31 cases of CCOC were provided by the Department of Pathology, Beijing Chao Yang Hospital of Capital Medical University. All patients had complete medical history and clinical pathological data and all cases were confirmed by surgery and pathology.
Immunohistochemistry
Paraffin blocks and corresponding hematoxylin and eosin (HE) stained sections were collected, and the HE sections were evaluated by two senior pathologists (HZ and FL). Biopsy specimens were fixed in 10% neutral-buffered formalin and routinely processed. Paraffin-embedded blocks were sectioned (5-μm thick), stained with HE and observed by microscopy (Olympus, CX23). The two-step immunohistochemical envision method was applied. To confirm the specificity of the immunoreaction, known positive and negative tissues were used as controls. The intensity of staining was evaluated for each marker and assigned an incremental score of 0, 1 + , 2 + , and 3 + . The extent of staining was categorized as focal (< 25%), multifocal (25% to 75%), or diffuse (> 75%).
Statistical analysis
The sensitivity and specificity of each marker and the diagnostic positive predictive values of their combination were subsequently determined in both types of tumor. The difference between the two groups was compared by the chi-square test.
All statistical analyses was performed using the SPSS version 17.0, and p-values < 0.05 were considered significant. The sensitivity, specificity, and positive predictive values were calculated by evaluation of the screening and diagnostic tests.
Results
Clinical features
The average age of the 90 patients with ccRCC was 58.5 (28 to 77) years old, including 63 males and 27 females with an average age of 60.1 (39 to 76) years. All 31 patients with CCOC were female patients with an average age of 52.3 (32 to 75) years.
Pathological findings
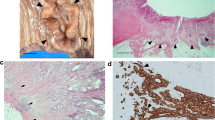
In all 90 cases of ccRCC, nest-sheet and acinar cells were mainly arranged (Fig. 1a), and some were microencapsulated, papillary, papillary-tubular and glandular-tubular. Most of the tumor cells exhibited a clear cytoplasm, with a few eosinophils and abundant blood vessels in the stroma. Cell morphology included round, multilateral, or cubic. The cytoplasm was transparent and eosinophilic. The cells of the 31 CCOC cases were solid, papillary, nested, and transparent. Sixteen of the 31 (51.6%) cases had typical spike-like cells (Fig. 1b).
Both ccRCC (a) and CCOC (b) exhibit a clear cytoplasmic morphological feature, × 200 magnification. SR-B1 in ccRCC show a strong positive expression in the cytoplasm and membrane (c) but is negatively or weakly expressed in CCOC (d). CD10 expression is strongly positive in the cytoplasm and membrane (e) in ccRCC but is negatively or weakly expressed in CCOC (f), × 200 magnification
Immunohistochemistry
Of the 90 ccRCC cases, 67 (74.4%) demonstrated membranous and cytoplasmic SR-B1 positivity that was diffuse in 24 cases and multifocal in 43 cases. The staining intensity scores ranged from 2 + to 3 + . The staining intensity of SR-B1 was higher in nuclear high-grade ccRCC (Fig. 1c). Only 5 (16.1%) of the 31 CCOC cases were SR-B1 focal positive (Fig. 1d) with a staining intensity score of 1 + . Eighty four (93.3%) of the 90 ccRCC cases exhibited membranous CD10 positivity (Fig. 1e) that was diffuse in 53 cases and multifocal in 31 cases. The intensity of staining ranged from 2 + to 3 + (Table 1). Membranous CD10 expression was present in 6 of 31 (19.4%) evaluable CCOC cases (Fig. 1f), and the intensity of staining was 1 + . Sixty-seven ccRCC cases were positive for both SR-B1 and CD10. Two cases of CCOC were positive for both SR-B1 and CD10. Five cases of SR-B1 positivity and 4 cases of CD10 positivity in CCOC showed shoe-nail-like cells. Two cases of CD10 positivity in CCOC were clear cells. The remaining cases that lacked typical nail-like cells and were clear were negative for both SR-B1 and CD10 (Table 2).
SR-B1 and CD10 in CCOC were focal positive with a significantly lower staining extent and intensity than ccRCC. SR-B1 and CD10 expression was significantly higher in ccRCC than CCOC (p < 0.01). SR-B1 positivity supported the diagnosis of ccRCC with a sensitivity of 74.4% and a specificity of 83.9%. CD10 positivity supported the diagnosis of CCOC with a sensitivity of 93.3% and a specificity of 80.6% (Table 3). Combined SR-B1 and CD10 immunopositivity supported the diagnosis of ccRCC with a sensitivity of 74.8%, specificity of 93.5%, and positive predictive value of 97.1%. Combined SR-B1 and CD10 immunonegativity supported the diagnosis of CCOC with a sensitivity of 71.0%, specificity of 93.3%, and positive predictive value of 78.6% (Table 4).
Discussion
In addition to ccRCC and CCOC, other common cytoplasmic tumors include Perivascular epithelioid cell tumor (PEComa), MiT family translocation renal cell carcinoma, fetal adenocarcinoma of the lung, hemangioblastoma, clear cell malignant mesothelioma, and serous carcinoma of the ovary. A differential diagnosis is needed when metastasis occurs, but the latter has relatively specific immunohistochemical markers to assist in diagnosis (Fig. 2), such as melanin labeling S-100 and HMB45 positivity in PEComa (Fletcher et al. 2013), TFE3 or TFEB positivity in MiT family translocation renal cell carcinoma (Moch et al. 2016), TTF-1 and NapsinA positivity in fetal adenocarcinoma of the lung (Huang and Chen 2016), Inhibin A positivity and PAX8/PAX2 negativity in hemangioblastoma (Carney et al. 2011), D2-40, CK5/6, Calretinin and WT-1 positivity in malignant mesothelioma (Travis et al. 2015), and PAX8 and WT-1 positivity in serous carcinoma of the ovary (Kuhn and Ayhan 2018). In ccRCC and CCOC, PAX-8 positivity is difficult to differentiate if metastasis occurs. In addition, ccRCC is well known for the tendency to metastasize to organs including the lung, bone, and ovary. In this study, only about 50% of CCOC have characteristic shoe-nail-like clear cells. The other common structures are nested, aciniform, microcapsule, papillary, nipple-tubular, and glandular cells, which are similar to the morphology and structure of ccRCC. Since ccRCC and CCOC have different prognosis and treatment schemes, immunohistochemistry is particularly important as a diagnostic supplement when histological morphology alone cannot differentiate between the two carcinomas. Therefore, it is necessary to find immunohistochemical markers with high sensitivity and specificity for diagnosing ccRCC and CCOC.
The difficulty in identifying the primary site is a major problem in diagnosing female reproductive system tumors, and highlights the need to improve the diagnosis rate of primary CCOC. PAX8 (Köbel et al. 2016) is emerging as the most specific marker for distinguishing between primary and metastatic ovarian tumors. However, PAX8 can be expressed in both ccRCC and CCOC, which makes it difficult to determine the primary site of the tumor by PAX8 positivity. Some studies have found that HNF-1β, WT-1, and NapsinA are highly expressed in CCOC, but lack specificity or sensitivity. These markers can also be expressed in varying degrees in ccRCC (Ji et al. 2018), which makes their application a challenge. Recently a few studies have reported on the expression of CD10 in CCOC and its value in distinguishing between ccRCC and CCOC. The present study, based on the perspective of tumor metabolism, found that expression of the SR-B1 protein and CD10 was significantly higher in ccRCC than CCOC. SR-B1 and CD10 exhibited focal weak-medium intensity staining in CCOC with a staining range and intensity that is significantly lower than ccRCC. The specificity of SR-B1 for ccRCC diagnosis was 83.9% and the specificity of CD10 for CCOC diagnosis was 80.6%. When SR-B1 and CD10 immunopositivity were combined, specificity of the ccRCC diagnosis was increased to 93.5%. When both SR-B1 and CD10 were negative, the specificity of the CCOC diagnosis was increased to 93.3%. Taken together, our results show that SR-B1 and CD10 immunoreactivity have higher sensitivity and specificity for ccRCC diagnosis, and can improve specificity when combined, even for identifying tumors with clear cell morphology (Fig. 3).
In conclusion, our study confirms that SR-B1 and CD10 are highly expressed in ccRCC but only weakly expressed or not expressed at all in CCOC. The combination of SR-B1 and CD10 can be used as new markers in the differential diagnosis of ccRCC and CCOC. This will help clinicians and pathologists identify the primary lesions of tumors and adopt appropriate treatments to avoid misdiagnosis and mistreatment.
References
Carney EM, Banerjee P, Ellis CL et al (2011) PAX2(-)/PAX8(-)/inhibin A(+) immunoprofile in hemangioblastoma: A helpful combination in the differential diagnosis with metastatic clear cell renal cell carcinoma to the central nervous system. Am J Surg Pathol 35(2):262–267
Fletcher CDM, Bridge JA, Hogendoorn PCW (2013) WHO classification of tumours of soft tissue and bone [M]. IARC Press, Lyon
Gebhard RL, Clayman RV, Prigge WF et al (1987) Abnormal cholesterol metabolism in renal clear cell carcinoma. J Lipid Res 28:1177–1184
Gulec UK, Paydas S, Guzel AB, Vardar MA, Khatib G, Gumurdulu D (2015) The clinical characteristics and outcomes of cases with pure ovarian clear cell, mixed type and high-grade serous adenocarcinoma. Arch Gynecol Obstet 292(4):923–929
Huang HJ, Chen XY (2016) Fetal adenocarcinoma of the lung: a clinicopathologic analysis of six cases. Zhonghua Bing Li Xue Za Zhi (Chinese Journal of Pathology) 45(9): 617–621
Ji JX, Wang YK, Cochrane DR, Huntsman DG (2018) Clear cell carcinomas of the ovary and kidney: clarity through genomics. J Pathol 244(5):550–564
Köbel M, Rahimi K, Rambau PF et al (2016) An immunohistochemical algorithm for ovarian carcinoma typing. Int J Gynecol Pathol 35(5):430–441
Kuhn E, Ayhan A (2018) Diagnostic immunohistochemistry in gynaecological neoplasia: a brief survey of the most common scenarios. J Clin Pathol 71(2):98–109
Moch H, Humphrey PA, Ulright TM et al (2016) WHO classification of the urinary system and male genital organs [M]. IARC Press, Lyon
NCCN (2019) Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Kidney Cancer Version 3. February 6.
Sugiyama T, Kamura T, Kigawa J et al (2000) Clinical characteristics of clear cell carcinoma of the ovary - a distinct histologic type with poor prognosis and resistance to platinum-based chemotherapy. Cancer 88:2584–2589
Tavassoli FA, Devilee P (eds) (2003) Pathology and Genetics: Tumours of the Breast and Female Genital Organs. WHO Classification of Tumours series–IV. IARC Press, Lyon
Tosi MR, Rodriguez-Estrada MT, Lercker G et al (2004) Magnetic resonance spectroscopy and chromatographic methods identify altered lipid composition in human renal neoplasms. Int J Mol Med 14:93–100
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG (2015) WHO Classification of tumours of the lung, pleura, thymus and heart, 4th edn. IARC Press, Lyon
Acknowledgments
This work were supported by the National Natural Science Foundation of China [grant numbers 81460383, 81660411], the International Cooperation Project and the Key Areas Innovation Team Project of Xinjiang Production and Construction Corps of China [Grant Numbers 2019BC001, 2018CB002].
Funding
No funding or other benefits related to the subject of this article were received from any commercial entity.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, T., Diao, X., Ding, M. et al. SR-B1 and CD10 combined immunoprofile for differential diagnosis of metastatic clear cell renal cell carcinoma and clear cell carcinoma of the ovary. J Mol Histol 52, 539–544 (2021). https://doi.org/10.1007/s10735-021-09963-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10735-021-09963-3