Abstract
Unprecedented and chaotic growth of cities results in reducing open spaces and water bodies, worsening infrastructure facilities and changes in ecological morphology. This unregulated growth of the urban population led to uneven distribution of urban amenities, facilities and healthcare services. Considering this, the study aimed to draw attention to the existing spatial pattern of healthcare facility centres as well as to find out the possible sites for the provision of healthcare facility centres in the municipal ward (micro-scale) of Midnapore town. This prototype study was conducted using Analytical Hierarchy Process (AHP) and Ordinary Least Square (OLS) evaluation model based on various criteria through Arc GIS environment. The findings indicate that the spatial distribution patterns of existing public healthcare centres were significantly dispersed. Weights based on a set of criteria were calculated by AHP and OLS algorithm and generated suitability evaluation maps classified from 1 (poor suitable) to 4 (most suitable). According to the employed criteria in this study unveil those existing hospitals and primary healthcare centres have not been located in the appropriate locations. The model is found to be valid for the given study area and there is no significant difference between AHP and OLS results. Further, it can be used for preparing the suitability map for the other areas with similar geo-environmental conditions for the proviso of healthcare services as well as will be most effective in preventing disease progression and reducing healthcare inequality on a large scale.
Similar content being viewed by others
Introduction
Healthcare facilities are important criteria and/or indicators for social well being as well as socio-economic development (Alabi, 2011; Danjuma, 2015; Mansour, 2016; WHO, 2001, 2004) of any nation because ‘Health is wealth’ as stated in the 3rd Sustainable Development Goals (Lawal & Anyiam, 2019). We already experienced combat with the Coronavirus (COVID-19) and its spreading (Alexander et al., 2015) all over the world evoke (Lawal & Anyiam, 2019) the overall scenario of health care systems (Fiedler, 1981; Kroeger, 1983; Muller et al., 1998), especially in the developing nations. The rapid growth of urban population demands affordable healthcare facilities (Alabi, 2011; Danjuma, 2015; Lawal & Anyiam, 2019). The concentration of higher population in the small urban space does not maintain its carrying capacity, is a common feature in developing countries; we meant unplanned urban growth resulting in unplanned urban morphology in which uneven distribution (Alabi, 2011; Danjuma, 2015; Lawal & Anyiam, 2019) of healthcare centres not able to provide services to its catchment area (Murad, 2008). Evenly distribution and accessibility to healthcare centres (Ajala et al., 2017) and/or services provided to everyone can prevent unavoidable disability, illness and diseases i.e. ‘Health for All’ (Alma Ata conference, 1978; Langford & Higgs, 2006; Moisi et al., 2010; WHO, 1981). But continuous urban population explosion challenges the urban planners that how to maintain standard healthcare infrastructure and services (Lawal & Anyiam, 2019; Murad, 2008). The urban area with a large population size has a demand for improved accessibility of healthcare centres and services (Murad, 2008; McGrail & Humphreys, 2014; Mansour, 2016). Besides, urban healthcare centres also providing services to their rural counterpart as most of the urban areas acting as a district or block headquarter, particularly in developing countries (Christaller, 1966; Mansour, 2016; Sedenu et al., 2016). As a result, urban dwellers are neglected from healthcare facilities as to maintaining huge streams of the population flux from the urban–rural fringe areas (Danjuma, 2015; Dinda et al., 2018; Mansour, 2016). So, the urban area should have a distinctive healthcare infrastructure and facilities (Lawal & Anyiam, 2019).
India is urbanising gradually and the population growth rate is high in the small town than the metropolitan cities (Alabi, 2011; Danjuma, 2015; Lawal & Anyiam, 2019; Nath, 1986; Sharma, 2020). For the rapid expansion of the small town, there is a rational need to study the spatial association and distribution patterns of healthcare facilities to optimising their site selection and spatial allocation (Ajala et al., 2017; Alabi, 2011; Danjuma, 2015). The broad analytical results can be helpful for the assessment of the reasonability (Danjuma, 2015) of the distributions of existing urban healthcare facilities (HCF) (Geurs & Van Wee, 2004) and find the new suitable sites or the location of new healthcare centres. In this regard, the spatial analytic hierarchy process (SAHP) is a useful geospatial (Danjuma, 2015; Gorsevski et al., 2012; Guiqin et al., 2009) analysis technique that coalesces the AHP model (Ahmed et al., 2016; Cheng Ru Wu, 2005; Eldrandaly, 2014; Saaty, 1980; Zhou & Civco, 1996) with Geographical Information System (GIS) algorithm (Abbas et al., 2008; Ahmed et al., 2016; Malczewski, 2006; Mansour, 2016; Murad, 2008; Murseli, 2014; Rahimi et al., 2017; Senser et al., 2010; Wang et al., 2018; Yang et al., 2006; Youzi et al., 2017; Zarkesh, 2005) to determine the optimum site (Assad, 2019; Ghobadi et al., 2013; Guiqin et al., 2009; Lawal & Anyiam, 2019; Saeed et al., 2012; Siddiqui et al., 1996; Uyan, 2014; Yang et al., 2006; Youzi et al., 2017; Youzi et al., 2017; Zhou & Wu, 2012) for a new primary healthcare centres in the urban area and helpful to the public health administrators (Cheng-Ru Wu, 2007) for their enhance planning (Shukla et al., 2017; Sandipan et al., 2013) especially cost benefit analysis (Pyrialakou et al., 2016) and municipal planning (Nikolakaki, 2004). The present study emphasises the nature and distribution of primary healthcare facilities (PHCF) with their site situation as well as draws attention to the urban planners to regenerate healthcare facilities in the deficit HCF areas. The hypothesis was whether there is a significant difference between healthcare site selection and accessibility of healthcare facilities to the people from the existing healthcare centres or sufficient in providing services as a whole. Based on the chosen hypothesis, the objectives were set for this study as (1) to assess the distribution of public healthcare facilities in the study area (2) to find out the deficient areas of public healthcare facilities within the urban area (3) to propose new primary healthcare sites (PHS) in the deficient healthcare facility (HCF) areas.
Literature review
Numerous empirical findings have attempted to show that health care centres and facilities are inequitably distributed (Eyles, 1996; Yang et al., 2006) with measuring the accessibility to healthcare sites (Muller et al., 1998; Parry et al., 2018; McGrail and Humphreys, 2014; Ajala et.al., 2017; Khan, 1992),available modes of transportation (Lawal & Anyiam, 2019; Kim et al., 2018) and time consuming to healthcare services (Moisi et al., 2010; Okwarajiet al., 2012) in determining the quality of social life from the view of social equity (Kim et al., 2018) i.e. every person have an equal chance of accessibility (Ajala et al., 2017; Langford & Higgs, 2006) like Potential spatial accessibility to healthcare services with avoiding economic and geographical obstacles (McGrail and Humphreys, 2014; Lawal & Anyiam, 2019; Kim et al., 2018). Information about demand (Murad, 2008) of healthcare services and accessibility helps to urban authority for further improvement of the existing healthcare infrastructure, distribution of active labours, and development of public transportation along with alternative healthcare sites (Kim et al., 2018; Alabi, 2011; Danjuma, 2015) thereby reducing healthcare inequalities (Lawal & Anyiam, 2019). Poor people are to be more benefitted socially from the increasing access to healthcare services (Moisi et al., 2010) with the objectives of reducing mortality, morbidity and fertility.
Provision of healthcare services varies across countries even at the grass-root level predominantly due to socio-economic conditions and government health policies (Mansour, 2016) as a whole promoting the general health and well being as well as socio-economic development. Healthcare services should be improved in the developing countries (Boulos et al., 2001) especially in India due to the large population with low GDP and limited distribution of hospitals, Primary health centres, equipment etc. (Assad, 2019). Migration to urban areas and gradual urban development has been global phenomena, especially in developing countries. In consequence, most of the small cities are rapidly changing into large cities. For the demand (Murad, 2008) of urban dwellers, the construction of primary healthcare centres with a rational allocation is looming and most significant. To the achievement of Millennium Development Goals, every government should have an affordable and proficient healthcare system that can easily be accessed by poor people (Malqvist et al., 2010; Lawal & Anyiam, 2019) link with poverty cycle for the sustainable urban development (Ajala et al., 2017) in the perspective of self-treatment and no treatment both are vulnerable to the long-term health problems.
W.H.O prescribed the meaning of Primary healthcare (PHCs) as indispensable healthcare aimed to promote health, prevent and cure diseases and rehabilitate i.e., usual lives after an illness and/or disability and which is accessible and available to all people at a rational cost by the motherland for their development at every stages. India have 3-tier hierarchical referral system i.e. primary, secondary and tertiary (M. Chokshi et al., 2016; Uzochukwu et al. 2016; Fiedler, 1981) public healthcare service facilities which are conceptualized as a basin healthcare service systems i.e. Sub-Health Centres (SHC) and Primary Health Centres (PHC) have been controlled by Community health centres (CHCs) and Sub-District Hospitals (SDH) are also controlled by District Hospitals (DH) and Medical Colleges (MC). The quality of services in the primary healthcare system would in due course reduce the strain on the Sub-District Hospitals and District Hospital (Muller et al., 1998). Primary Health Centre covering an area with a population of 20,000 in hilly, tribal, or difficult areas and 30,000 populations in plain areas with 6-surveillance beds. Each Primary Healthcare unit acts as a referral unit for 6 Sub-Centres and transfer chronic cases to Community Healthcare (30 bedded hospital) and hospitals at subdistrict and district levels. Therefore, Primary Healthcare centres are the primary or entry points in the healthcare system that provide basic services to the people and appropriate allocation shall be most useful in preventing disease progression (Guagliardo, 2004) on a large area. Hence, the local government ought to be provision of a healthcare infrastructure in compliance with the population and state and/or national health policy (Jordan et al., 2004). Indian government have initiated the National Urban Health Mission (NUHM) launched 1st May 2013 covering all state capitals, district headquarters and other cities or towns with a population of 50,000 and above (as per census 2011) with the goals of providing indispensable primary healthcare services and various scheme to the urban poor especially slum dwellers and reducing their expenses for treatment under the Ministries of Urban Development, Housing and Urban Poverty Alleviation, Human Resource Development and Women and Child Development. The healthcare system in India is progressively more in front of challenges of ensuring healthcare provision to the growing population, especially for the poor people and healthcare centres are unfairly distributed over space (Moisi et al., 2010; Danjuma, 2015). The facet of challenges is rapid population growth concentrated in existing towns and/or cities (Lawal & Anyiam, 2019), distance to the nearest health centre (Lawal &Anyiam, 2019; Wang & Luo, 2005; Shannon et al., 1969; Muller et al., 1998), lack of education and awareness, least efficient healthcare human resources and the inadequate financial support for the provision and management of health services (Danjuma, 2015). For instance, households distance farther away from the healthcare centres having a higher risk of growing death rates (Mansour, 2016; Shannon et al., 1969; Muller et al., 1998) of child and pregnant women. Apart from these important factors, an explicit government initiative has not been given for fairness in planning and allocation of health infrastructures over the years (Danjuma, 2015; Savigny and Wijeyaratne, 1994; Onokerhoraye, 1999) as we learn from the covid-19 virus spreading and infection over India.
Materials and methods
Location of the study area
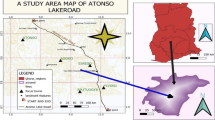
Midnapore town acting as headquarter of Paschim Medinipur district of West Bengal has a long urban history since the time of archaic. It was declared as a municipality on 1st April 1865, but now Midnapore is a class-I town (Fig. 1), located in the southwestern part of Paschim Medinipur district over the lateritic track. The study area is encircled by rural areas with open agricultural land, fallow land, vegetation, woodland and spreading of residential houses, commercial in addition to administrative offices and small-scale industries (Roy, 2016). The study area having a population of 1, 68,496 (Census of India, 2011) growing faster (Dinda et al., 2018; Dolui et al., 2014; Dutta et al., 2018) with 4-hospitals and 8-primary healthcare centres located in different parts of the town (Table 1) maintaining the standard of NUHM (National Urban Health Mission, India) i.e., 21,062 population per PHC.
Site characteristics
The study sites containing plain topography along the Kasai river with a slope < 1° to < 9° and elevation from mean sea level ranges between 23 and 60 m. Midnapore is one of the important administrative and educational towns in West Bengal as a whole. Its distance from Kharagpur town is 12 km and from Kolkata (capital of West Bengal) it around 120 km. This specific area is lies beside topologically well-connected roads and railway station, which mainly connected with most of the important towns in Paschim Medinipur. Administrative head offices, University and other important educational institutes and business centres are located in the heart of town. This is the most influencing factor behind the cross-culture ethnic agglomeration of the slum population. The slum settlements were mainly distributed all over the town predominantly grown up in the surrounding areas of the well-connected transport network. It has 25 municipal wards and near about 156-notified slums. According to the Census of India, 2011, the population of Midnapore town is 1,69,264; the male and female population is 84,977 and 84,287 respectively, sex ratio and child sex ratio is 992 and 985 respectively, literates persons are 88.99% whereas male literates 92.52% and female literates 85.44%. Besides, the Slum population is 50,943 which is almost 30.09% of the total population of the town.
Field investigation, data and methodology
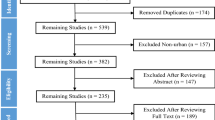
For the present study, a total of 156 slum areas were selected with their ward location and population. Data on public health facilities were obtained and analyzed within the GIS environment. Statistical data about the population and spatial data set of each ward were gathered from the Midnapore Municipality according to the 2011 census of India. The total number of governmental public healthcare centre is twelve within total area of approximately 20 km2, in which three hospitals and nine primary healthcare centres (Fig. 1) dispersely distributed across the town. The study used data containing the list of healthcare centres and their addresses in Midnapore Municipality and the administrative map of Midnapore Municipality was also sourced from the local government to serve as the base map. The GPS device was used to collect coordinate points of the healthcare centres in the municipality. Geospatial data were collected from Earth Explorer-USGS open website (https://earthexplorer.usgs.gov) and methodological development (Fig. 2) is highlighted as below:
Data analysis
This study integrated both the statistical operations of model building and handling of raster and vector datasets on a GIS and Remote sensing platform which necessitates processing the large dataset to an accurate output for the practical implication. The statistical calculations and algorithms of models were worked out and simulated using MS Excel v2016 (Microsoft Corporation) and SPSS v26.0 (IBM Analytics). The GIS operations and mapping were performed using the Arc GIS v10.4 and image processing was done by Erdas Imagine v9.2 software. Overall data analysis is divided into two folds- Spatial Analysis of Healthcare facilities (HCF) and Site Suitability for new Primary healthcare facilities (PHCF).
Spatial analysis of HCF
-
1.
Euclidean distance
Euclidean distance is calculated from the centre of the source point to the centre of each of the surrounding points based on a straight-line distance in meters or feet in a GIS platform to find the nearest point or cellsFootnote 1 (Mansour, 2016). The formula for this distance measuring between the point of X (X1, X2, etc.) and Y (Y1, Y2, etc.) is as follows:
The above formula was applying to the measure of distance between two points i.e., point sources, direction and proximity to the closest points. The Euclidean Distance tool is used in our study for finding the nearest accessible PHCs for an emergency i.e., how easy it is to reach within a certain distance from the PHCs and/or finding a suitable place to locate PHCs, varies across all municipal ward boundaries. Overall, the least accessible facilities were found in the marginal part of the ward boundary, especially the far west, south-east and north-east parts of the Midnapore municipality (Fig. 3). In contrast, the most accessible places were located in the middle and south-west direction with a high density of healthcare facilities due to location of maximum number of healthcare centres indicative that going away from the city centre, the distance to public health facility increases with decreasing accessibility to the healthcare facilities.
-
2.
Mean centre
The mean centre is a point of average x and y coordinate values for the input centroids feature with projected data accurately measure distances with the following mathematical formulaFootnote 2-
where xi and yi are the coordinates for features i and n equal to the number of features and \(\overline{X}\) and \(\overline{Y}\) defines the mean centre. Locating mean centres can be useful for pursuing changes in the distribution and/or to judge the distributions of different kinds of features (Sedenu et al., 2016) like health centres as well as possible points or locations of features in the GIS platform. Our analysis of the output map (Fig. 4) depicted the mean centre among the health facility centres in the study area which is acting as a geographic centre or point based on the most density area. But in the study area, the mean centre slightly deviated from most population density areas indicating primary healthcare facility centres were not properly distributed and need to be planning interventions.
-
3.
Central features
The central feature tool in GIS recognizes the most centrally sited point, line or polygon in the input database associated with the shortest accumulated distance to all other features are computed using the weighted mean centre (if weight is specified) in the dataset as well as used in distance computations by Euclidean or Manhattan distance (Sedenu et al., 2016). It is useful for finding the centre necessitate to minimize distance (Euclidean or Manhattan distance) for all features to the centre as to identify which part of the dataset is most accessible.Footnote 3 As shown in Fig. 4, Midnapore Medical College and Hospital considered the most centrally located healthcare facility centre among the existing centres, as both are most accessible from all directions in the study area. Midnapore Medical College and Hospital acting as a district hospital well connected by accessible roads with well equipped medical infrastructures identifying the most centrally located healthcare centre.
-
4.
Proximity or buffer analysis
In a GIS environment, a buffer is created around selected points, lines, or area features by using Euclidean distance in a two-dimensional Cartesian plane determining the area covered within a specific location or concentrated in a relatively small area e.g., distances from schools, public buildings or healthcare centres etc. Also, a separate buffer can be created around more than one feature at once.Footnote 4 Buffer analysis was used to explore the spatial distribution of healthcare units (Danjuma, 2015; Jamal, 2016;Mansour, 2016; Parry et al., 2018; Wong et al., 2010; Zhou & Civco, 1996; Zhou & Wu, 2012) as well as inspecting the proximity to public health facilities. Buffer analysis was applied for creating a buffer zone with a radius of 1 km around all public health centres within the study area (Mansour, 2016) (Fig. 5). The finding of this analysis is that most wards of western to north-western, south-east and north-east part of Midnapore municipality are located outside of the 1-km catchment area indicated to have lower public health accessibility. It is also clearly noticed that about 9 municipal wards (ward 3, 4, 5, 6, 17, 18 and 25) exhibit 20–50% unserved areas with a lack of access to near public health facilities within a 1 km buffer radius distance. Therefore, there is a need to be additional public health centres that adequately serve the facilities.
-
5.
Near
The Near analysis within the GIS algorithm was used to determine the distances from the input feature (slum point) to the nearest features (public health facilities) by using Euclidean distance through the calculation in the unit of meter or km within the same area with the specified distance or radii.Footnote 5 The limitation of the near tool is that it can only find the nearest feature in another dataset i.e. there is a one-to-one relationship in the output layerFootnote 6 (Assad, 2019; Danjuma, 2015; Kim, 2018; Wang & Luo, 2005; Wang, 2018;Zhou & Wu, 2012).
The output map (Fig. 6) of the near analysis signifies that 16.5% of slum neighbourhoods in the study area have resided within a 200 m distance from the nearest public health facility. About 77% of slum neighbourhoods are living further away from the nearest facility at a distance from 200 m to 1 km. Whereas, only 6.50% of slum neighbourhoods having further proximity to health facilities by a distance greater than 1 km.
-
6.
Standard distance
The standard distance is used to measures the magnitude to which features are concentrated or dispersed around the geographic mean centreFootnote 7 and estimate the compactness of distributed features around the centre on a map by a circle polygon with the radius equal to the standard distance (Sedenu et al., 2016) can be represented mathematically as:
where \(x_{i}\) and \(y_{i}\) are coordinates and \(\overline{X}\), \(\overline{Y}\) defines the mean centre which is not concentrated around mean centre. In Fig. 7, a standard distance polygon or circle has been developed to know the concentration of health centres around a mean health centre. The analysis indicates that there is a dispersed spatial pattern of health centres surrounding mean geographic health centres as standard distance encompasses only 50% of health centres which deviates from a standard normal distribution of 68%. Therefore, it is conceptualised that the spatial pattern of health centres within standard distance circle fails to provide proper services to its encircled area which needs to draw attention to the urban planners.
-
7.
Directional distribution
Directional distribution is measuring the trend of a set of points or areas through the calculation of the standard distance separately in the x and y directions define the axes of an ellipse i.e. standard deviational elliptical polygon represents the distribution of features in a particular orientation, mathematically expressed as:
where \(x_{i}\) and \(y_{i}\) are coordinates, \(\overline{X}\) and \(\overline{Y}\) define the mean centre and \(n\) is equal to the total number of features. Directional distribution in the GIS platform helps to understand the dispersion or spread of data covering a normal distribution and may be useful in setting up mitigation strategies.Footnote 8 The output map (Fig. 8) of analysis in the GIS platform reveals that the development of healthcare centres in the study area in an SW to NE direction following geographic mean centre. Moreover, along the direction around the mean centre, the density of healthcare centres is higher than the other parts of the study area. As a result, inequalities of healthcare services persist in the study area, which needs to be organized from the perspectives of public interest.
-
8.
Average nearest neighbour
The Average Nearest Neighbour (ANN) tool in the GIS platform is the Euclidean distance between each feature centroid (mean centre) and its nearest neighbour’s centroid location (public health facilities) and averages all these nearest neighbour distances.Footnote 9 The average nearest neighbour ratio is designed as the observed average distance (\(\overline{D}_{0}\)) divided by the expected average distance (\(\overline{D}_{E}\)) (based on the same number of features covering the total area).
In the above equations, \({\text{d}}_{i}\) equals to the distance between feature i and its nearest neighbouring feature, \(n\) corresponds to the total number of features, and \(A\) is the area of a minimum enclosing rectangle around all features, or it’s a user-specified area valueFootnote 10 (Danjuma, 2015; Mansour, 2016; Sedenu et al., 2016) is 0.0175264. The average nearest neighbour z-score for the statistics is calculated as:
For the analysis of the spatial pattern of distances among public health centres, the Average Nearest Neighbour tool explores the value of Nearest Neighbour Ratio (NNR) is 1.52 (p < 0.0001) and the Z-score was 3.43 (p < 0.0001). The value indicates that public health facilities over the study area were spatially dispersed (Fig. 9), as a result, the null hypothesis is acceptedFootnote 11 that there is a spatial pattern among public health centres in the study area is accepted. In general, the spatial pattern of public health centres was concentrated in the middle part of the city and dispersed towards its periphery. Hence, the identified spatial pattern in this analysis reveals dispersed spatial patterns along with riotous and bungling distribution of public health centres across the city. For instance, the south, southeast, north and northwest part of the city has the least number of public health centres (Fig. 8). Similarly, the complete absence of health centres was identified in the southeast and eastern parts of the city, most probably, are subjected to urban expansion and new housing construction.
-
9.
Population density
Density analysis in GIS environment obtains by known quantities e.g. population and spread over terrain based on the quantity i.e. area, which measured at each location with the spatial relationship. The Density tool distributes a measured quantity of an input point layer throughout the landscape to produce a continuous surface.Footnote 12 The Density tool calculates the density map within an area of interest based on single input of point or line features only. It may be calculated by a count field i.e. a numerical field that specifies the number of incidents at each location. For calculating the population density, cities could use a count field that will provide the output densities in Square Miles or Square KilometersFootnote 13 depending on the user units setting. We calculate population density using population (As per Census of India, 2011) for each ward is divided by the area (km2) of each ward to get an estimated population density (Sedenu et al., 2016) for each ward (Fig. 10). The formula used for estimated population density is given as here will be population density equation:
-
10.
Health facility ratio
In the twenty-first century, providing a pertinent number of public healthcare facilities at each administrative urban unit in all states is the main concern of Govt. of India (Department of Health & Family Welfare, India, 2013) aiming of analyzing the health facility to population ratio and to determine how best to meet the basic needs of the health services to the urban population. Allocation of health resources depends on the geographic aspects of the healthcare delivery system. Therefore, healthcare service points should be geographically proficiently distributed following population concentration and density (Mansour, 2016). According to WHO (2010), the health facility ratio is the facility distribution per10, 000 populations as a useful standardized indicator that measuring the levels of health services accessibility by population and identification of gaps in health service coverage within a particular geographical administrative unit.
The output of the analysis is demonstrating (Fig. 11) that most of the municipal wards exhibited zero ratios and/or less than one facility per 10,000 populations. The core of the city has a high population density maintain advanced health facilities due to the provision of govt. hospitals and private healthcare centres. Correspondingly, some municipal wards in the northern, eastern and south-west parts displayed moderate health facilities due to the presence of 24 h primary healthcare facilities. In contrast, most of the peripheral wards of the city are not well served by public health facilities or exhibit limited (mostly zero) provision of public health facilities conceivably due to the municipal wards being relatively low population size and newly constructed roads. Therefore, the pattern of the spatial distribution of health facilities per population varies considerably throughout the city is a sign of the unevenness of healthcare facilities and not properly achieved the ultimate equity in public health coverage.
-
11.
Service area
A service area is allied with a local network dataset or a network service in a GIS (Network Analyst extension) environment as a region that encompasses all accessible streets evaluating accessibility from a pointFootnote 14 that identify how many people or how much of anything else can be reached within the neighbourhood or region with specified area or distanceFootnote 15,Footnote 16 and travel time, expressed as-
The service area maps were created to show the total travel time from the points of a neighbourhood to the nearest healthcare facilities (Sedenu et al., 2016) within a given time of 3, 5, 7, and 9 minutes considering a constant speed of 40 km/h for identifying the most efficient routes or roads for the accessibility of healthcare services. Also, it indicates the shortest or least-cost routes to the nearest healthcare centre (Fig. 9). The Network tools were also found the total area served by the health facilities in the study area is 12.28 km2 showing green colour in Fig. 12 and households outside the green colour were underserved or unserved is 7.72 km2. The map demonstrates that 5-municipal wards to be short of access to near public health facilities having 90% of the area is unserved and in 4-municipal wards, more than 30–50% area has not enclosed with public health services. Similarly, over 3-wards exhibit 20% unserved areas while only 8-wards are served entirely with public health centres with shortest routes (Fig. 13). Therefore, it is recommended to the provision of additional healthcare centres in the unserved area for the healthy allocation of healthcare services.
-
12.
Multidimensional Poverty Index (MPI)
Multidimensional Poverty Indices (MPI) was designed to state the inclusive picture of people living in poverty and allowing comparisons both across countries, regions as well as the world and within countries by targeted socio-cultural groups, urban or rural key households and communities over time.
MPIs as analytical tools are most useful in identifying poverty patterns and vulnerable households (Alkire et al., 2015) with the help of accessible indicators, suitable weighted values, cut-offs and thresholds. Multidimensional Poverty Indices typically uses microdata from household surveys and their unit of analysis to identify multiple deprivations at the individual level in health, education and standard of living etc. (Alkire et al., 2015; Cavapozzi et al., 2015; Das et al., 2020; Ravallion, 2011). A household is deprived if they fail to satisfy a given ' poverty cut off 'determined by weighted deprivation score i.e. aggregate score for each household (Ci) as-
The weighted deprivation score (Ci) is calculated by multiplying the deprivation matrix (\(gij\)) and weighted value (equal) assigned for each indicator or dimension (\(wj\)). If the household deprivation score goes beyond a given threshold (e.g. 1/3) then a household is considered to be 'multiple deprived', or simply 'poor' (Alkire et al., 2015; Das et al., 2020).
Weighted deprivation score is varying between 0 (Non-deprived) and 1 (Deprived) where Xij > Zj. The Deprivation matrix (\(gij\)) is established by order of achievement matrix (n × d) denoted as Xij and deprivation cut off (Zj) standard value which judges whether the households are deprived or not. If the weighted deprivation score (Ci) is greater than the poverty cut off (Ci > Pk), then the households are considered as Multidimensionally poor (q). HeadCount Ratio (HCR) is calculated as
The average number of multidimensionally poor households (A) indicates the intensity of the multidimensionally poor condition. Finally, Multidimensional Poverty Index (MPI) designed (Alkire et al., 2015; Das et al., 2020) as
We used micro-level household data of slum communities with their standard of living, expenditure, income per head, education level etc.in every municipal ward and results are evaluated using MPIs shown in Fig. 14.
Results and discussion
Site suitability analysis for new PHCF
The demand for developing new healthcare centres in the urban area for upgrading the social wellbeing and living standard is a crucial topic in planning decision processes. Minimizing the diseconomies and determinants of new health risk factors, more in deep, require rational site selection of new healthcare centres and/or facilities which plays a vital role in urban social potentials (Oppio et al., 2016). Primary healthcare site selection may also an important task for hospital construction and management in the urban poor area of India. Appropriate healthcare site selection will help to optimize the provision, allocation and accessibility of healthcare facilities to meet the social and economic demands bring together with the development of urban health services. In perspectives of cost–benefit analysis, a rational site selection strategy is thought to be an effective means to trim down cost and time of rescue in urban poor areas satisfying people’s medical needs as well as enhance the quality of life with attaining high reimbursement in municipal planning (Wang et al., 2018; Zhou & Wu, 2012). Geospatial site selection (GSS) is a framework that helps urban decision-makers for the selection of sites according to space availability and suitability (Abujayyab et al., 2016) to some extent either suitable or unsuitable for the actions being planned through sophisticated analysis with the deliberation of significant issues such as technical, environmental, physical, social and many others (Parry et al., 2018). In this regard, Remote Sensing, GIS, GPS, AHP and statistical models and tools play a vital role in the identification and multi-criterion decision analyzing site selection with planning and management (Parry et al., 2018; Sandipan et al., 2013; Shukla et al., 2017) concern with urban development. In the study area, different sites suffer from a shortage and dreadful distribution of healthcare services which needs consideration of the multiple alternative solutions and evaluation factors. We developed Multi-Criteria Decision Support System (MCDSS) (Ahmed et al., 2016) processes that combine Geographical Information System (GIS) analysis, Ordinary Least Square (OLS) statistical tool with Analytical Hierarchy Process (AHP) model. And through using these geospatial techniques, we have found the optimum sites for new Primary Healthcare centres (PHCs) in the study area. Based on the spatial analysis, a set of criteria (Fig. 15) involving geophysical and socioeconomic variables as:
-
a.
Distance to slum areas
-
b.
Distance to poverty affected areas
-
c.
Distance to population density areas
-
d.
Distance to existing HCF
-
e.
Distance to major road
Elimination of constraint area
Constraint areas are those areas (lands) within the city preoccupied with developmental activities and not available for the construction of any kind of developmental project (Abdullahi et al., 2013) subject to transmission constraints by the competent authority. In Arc GIS (vs.10.4) the erase tool helps users to remove the overlapping areas or portions (polygon) of a featureFootnote 17 which are not allowed for any kind of development programme. This tool will use a tiling process to handle very large datasets for better performance and scalability.Footnote 18 In our study, we have identified constraint areas that were not available for the construction of primary healthcare centres (Fig. 16) due to already possesses of any developmental units. These areas were removed from the whole study area and do not take into account the final decision making. Generally, major administrative areas like central and state government offices, police headquarter area, universities and colleges, industries and recreational parks etc. are to be considered as constraint areas where the built-up of PHCs is insignificant.
Weight calculation based on OLS technique
Based on the linear regression (simple or multiple) model assumptions, coefficient estimation is on the intercept and slope that minimize the sum of squared residuals (SSR) by the principle of least squares (smaller the differences, better the model fits with data) for finding the relationships among the variables (Observed dependent variable and predicted variable by the linear function) of interest in the given dataset called the Ordinary Least Squared (OLS) estimatesFootnote 19 with explanatory variables (p) articulated as:
where Y is the dependent variable, β0 is the intercept of the model, X j corresponds to the j-th explanatory variable of the model (j = 1 to p), and ε is the random error with expectation 0 and variance σ2. Besides, the estimation of the value of the predicted dependent variable (Y) for the i-th observation is given byFootnote 20 the equation:
The OLS method corresponds to minimizing the sum of square differences between the observed and predicted values. This minimization leads to the following estimators of the parameters of the model:Footnote 21
where β is the vector of the estimators of the βi parameters, X is the matrix of the explanatory variables preceded by a vector of 1s, y is the vector of the n observed values of the dependent variable, p* is the number of explanatory variables to which added 1 if the intercept is not fixed, wi is the weight of the i-th observation, and W is the sum of the wi weights, and D is a matrix with the wi weights on its diagonal. Also, the vector of the predicted values can be written as follows:Footnote 22
Ordinary least square is useful when a large number of explanatory variables in comparison to the number of observations for estimating the unknown parameters. OLS provides minimum-variance mean-unbiased estimation when the errors (Assume normally distributed) have finite variances as a maximum likelihood estimator.18 We used Ordinary least square to investigate the relationship between existing healthcare centres with other criteria, such as Distance to slum areas, Distance to poverty areas, Distance to population density areas, Distance to major roads and Distance to existing HCF (Table 2). By using this method, the effects of various criteria on existing healthcare centres were estimated by determining coefficients for each criterion. These coefficients were calculated based on the average distance between each healthcare centre to other healthcare centres (Table 3) (Abdullahi & Pradhan, 2012).
Estimation of weights using Analytical Hierarchy Process (AHP) model
The Analytical Hierarchy Process is a pair-wise comparison technique developed by Thomas Saaty. In the late 1970s, Saaty has developed the framework of Multi-Criteria Decision Making (MCDM) by assigning various weights and scores representing the relative importance of pairs criteria (Saaty, 1994) (Table 4) based on his scale (Abdullahi et al., 2013; Saaty, 1980). The application of AHP is rare in medical geography and the field of healthcare site selection or has not been fully explored (Soltani & Marandi, 2010). Siddiqui et al. (1996) were the first used to combine the GIS and AHP model to solve the site selection problems (Ahmed et al., 2016). AHP model is most applicable in the salvation of complex problems and set priorities in decision making for capturing both subjective and objective aspects of a decision. The AHP breed a score or weight for each evaluation criterion and each option according to the decision maker’s pairwise comparisons of the criteria (Tables 5, 6) with a combination of producing global score and the weighted sum of the scores concerning all criteria. Moreover, AHP can integrate the inspection of the reliability of the decision maker’s evaluations and reducing the bias in the decision-making process (Ahmed et al., 2016; Hao & Dai, 2013; Korpela & Tuominen, 1996; Wang et al., 2018). This evaluation process is done by set up the pairwise comparison matrix through the selection of different criteria with the help of GIS, SPSS and Microsoft Excel. The relative score and weights provided by the authors are aggregated by the measurement scale of Satty (Abdullahi et al., 2013). We present a case study that employed spatial information technologies (GIS), OLS and MCDM (AHP) in assessing and selecting the suitable Primary healthcare optimal and backup sites. We also incorporated factors from environmental, economic and urban context which is applicable in rapidly developing cities of the developing countries providing references in the future healthcare planning (Ahmed et al., 2016). A classification scheme was applied for the criteria weighted by pairwise comparison. The coefficients of each parameter were calculated based on the OLS technique and expert’s knowledge with normalization and converted to Satty’s scale as an input for spatial mapping. Then areas of sites from two techniques that have the same suitability class were computed. The result shows that there has a similarity in the areas as well as the spatial distribution of each suitable class in the study area (Fig. 17). Analytical Hierarchy Process (AHP) and ordinary least square (OLS) is breeding the weight setting on factor criteria with the requisite test were applied to their weight change (Ahmed et al., 2016). Spatial analysis in GIS was used to generate factors maps with overlay and suitability evaluation maps. All maps are classified from 1 (very poor-S1) to 4 (Most suitable-S4) using this model (Fig. 17). It was found that the most suitable area (S4) is about 2–3% and the suitable area (S3) is about 27% as well as the unsuitable area (S1) is about 6%. Furthermore, about 65% area is considered as not important (S2) due to the sphere of influence of the existing healthcare centres. As well, according to the employed criteria in this study, existing hospitals and PHCs has not been located in the appropriate locations. A careful examination of the suitability map generated by two models revealed that the Northeastern and southeastern part shows a belt of high suitability (S4) and a narrow belt of the middle and northeastern part of the municipality incorporating moderately suitable (S3) for establishing PHCs and there was no significant difference of between AHP and OLS results (Table 7; Fig. 18).
Concluding remarks
Every city has a specific urban morphology and essentially determined by natural settings and demographic factors. The settlement areas in the study area are gradually increasing since 1991 in different directions. Dinda et al. (2018) estimated the built-up area of Midnapore municipality in 1991 was 15.29 km2 which increased in 2001 to 20.10 km2 with a growth rate of 31.48%, though it was high in the period between 2001 and 2017 about 35.39%. The residential areas also developed along outside the administrative boundary and gradually expanding which is an indication of dependency on healthcare services from the municipal healthcare centres. Continuous rural to urban migration induced the development of slum and squatter settlements to occupy illegally most of the vacant land and unplanned urban development therein reduces the scope of proper healthcare facilities. A predictive map, displaying the potential areas of primary healthcare sites, will help in designing inclusive policies for scientific urban land use and area-specific planning. Furthermore, the suitability map may be used as a base map for framing urban morphology and smart city development context with harmonizing the characteristics of an area with the attributes which are most appropriate for health services. Also, it may provide an appropriate methodology and predictive tools to support location choice and land suitability appraisal (Ahmed et al., 2016). Moreover, this can offer as decision support to the rational allocation of funds to different micro-level administrative units especially blocks or panchayat levels for the schemes related to the development of new healthcare centres and infrastructure, free and mobile health services and others facility to the poor section. This study also may put forward a technique that would be suitable for site-specific pilot-scale research and does attempt to assess the suitability over larger areas.
Spatial analyses with various GIS tools were applied to findings the inequalities in public health service across the study area. These analyses serve as a base for addressing spatial variation of equity in access to public health facilities, directional distribution and pattern, time-distance context, facility ratio, service area etc. at the small administrative units following population size and geographic distances. However, equity of health access and provision within urban areas has indispensable to assess numerous factors, such as availability, quality, travel time, and distance from provider to population (Mansour, 2016). The findings of this study revealed that there was a dispersed pattern of public health facility distribution along with a lower healthcare facility ratio. Most of the marginal parts were identified as underserved within a 1 km distance from public health facilities. Therefore, this study will be extensively contributed to the further understanding of the provision and distribution of healthcare facilities, inequalities of service accessibility and its effectiveness in the delivery system (Danjuma, 2015; Mansour, 2016). Spatial analysis was also contributed to finding the major five basic variables for suitability analysis and mapping, such as (a) Distance to slum areas (b) Distance to poverty affected areas (c) Distance to population density areas (d) Distance to existing HCF (e) Distance to the major road. The result with the model can be benefitted to the local authorities, planners, professionals, decision-makers and researchers for further research (Ahmed et al., 2016) on small and large scale terrain for integrated health management planning. It also seeks relatively less time consuming, simple, economically practicable and trustworthy analytical tools for the formulation of national rural–urban health development policies in India, as well as the other developing countries where the economy is dominated by the agro-based economy and urbanisation rate, is high requires predictive maps for identifying the areas with different constraints to healthcare facilities.
Recently in a pandemic situation, healthcare planning is a challenging issue that requires spatial data such as location and characteristics of health centres demand, utilization rates, patients' perspectives and socio-economic components (Danjuma, 2015). This study was limited by the absence of attribute data and statistics, for instance, the number of beds, physicians and nurses per healthcare centre, service quality, available facilities, people’s satisfaction level and other criteria to be considered for future research. Therefore, further refinement of the data structure and the employment of more spatially significant variables in compliance with enhanced by geospatial approaches (Ahmed et al., 2016) may append high exactitude to the demarcation of suitability zones, as well as provide meaningful insights in addressing the nature of healthcare distributions over a spatial frame.
Notes
https://desktop.arcgis.com/en/arcmap/10.3/tools/analysis toolbox/near.htm#: ~ :text = A%20near%20angle%20measures%20direction,90%C2%B0%20to%20the%20south.
Ibid 9.
Ibid 9.
Ibid 19.
Ibid 19.
References
Abdullahi, S., & Pradhan, B. (2012). Spatial modelling of site suitability assessment for hospitals using geographical information system-based multicriteria approach at Qazvin city, Iran. Geocarto International. https://doi.org/10.1080/10106049.2012.752531
Abujayyab, S., et al. (2016). GIS modelling for new landfill sites: Critical review of employed criteria and method of selection criteria. IOP Conference Series Earth and Environmental Science, 5(2), 101–118. https://doi.org/10.1088/1755-1315/37/1/012053
Ahmed, A. H., Mahmoud, H., & Aly, A. M. M. (2016). Site suitability evaluation for sustainable distribution of hospital using spatial information technologies and AHP: A case study of Upper Egypt, Aswan City. Journal of Geographic Information System. https://doi.org/10.4236/jgis.2016.85048
Ajala, O. A., Sanni, L., & Adeyinka, S. A. (2017). Accessibility to health care facilities: A panacea for sustainable rural development in Osun State Southwestern, Nigeria. Journal of Human Ecology. https://doi.org/10.1080/09709274.2005.11905819
Alabi, M. O. (2011). Towards a sustainable distribution of health centres using GIS. American Journals of Tropical Medicine and Public Health, 1, 130–136.
Alkire, S., et al. (2015). Multidimensional poverty measurement. Oxford University Press.
Boulos, M. N. K., Roudsari, A. V., & Carson, E. R. (2001). Health geomatics: An enabling suite of technologies in health and healthcare. Journal of Biomedical Informatics, 34, 195–219. https://doi.org/10.1006/jbin.2001.1015
Cavapozzi, D., Han, W., & Miniach, R. (2015). Alternative weighting structures for multidimensional poverty assessment. Journal of Economic Inequality, 13(3), 425–447.
Chokshi, M., et al. (2016). Health system in India. Journal of Perinatology, 36, S9–S12. https://doi.org/10.1038/jp.2016.184
Christaller, W. (1966). Central places in Southern Germany. Prentice-Hall.
Danjuma, I. (2015). Locational analysis of healthcare facilities in Keffi Local Government Area of Nasarawa State, Nigeria. PhD Thesis. Retrieved from http://kubanni.abu.edu.ng/jspui/bitstream.
Das, P., Paria, B., & Firdaush, S. (2020). Consumption poverty and multidimensional poverty: A study in Indian context, social indicators research. Social Indicators Research. https://doi.org/10.1007/s11205-020-02519-0
Dinda, S., Das, K., Chatterjee, N. D., & Ghosh, S. (2018). Integration of GIS and statistical approach in mapping of urban sprawl and predicting future growth in Midnapore town. Modeling Earth Systems and Environment, 5, 331–352.
Dolui, G., Das, S., & Satpathy, S. (2014). An application of remote sensing and GIS to analyze urban expansion and land use land cover change of Midnapore Municipality, WB, India. International Research Journal of Earth Sciences, 2(5), 8–20.
Dutta, B., Roy, U., & Maity, I. (2018). Evaluating coping mechanism of slum dwellers in Midnapore municipal area, West Bengal. Asian Journal of Multidimensional Research, 7(8), 150–163.
Eldrandaly, K. A. (2014). Developing a GIS-based MCE site selection tool in ArcGIS using COM technology. May 2013.
Eyles, J. D. (1996). Poverty as inequality: A case study. Progress in Human Geography, 6, 55–64.
Fiedler, J. L. (1981). A review of the literature in access and utilization of medical care with special emphasis on rural primary care. Social Science & Medicine Part c: Medical Economics, 15, 129–142.
Geurs, K. T., & Wee, B. V. (2004). Accessibility evaluation of land-use and transport strategies: Review and research directions. Journal of Transport Geography, 12(2), 127–140. https://doi.org/10.1016/j.jtrangeo.2003.10.005
Ghobadi, M., et al. (2013). Siting MSW landfills by combining AHP with GIS in Hamedan province, western Iran. Environmental Earth Sciences, 70, 1823–1840.
Gorsevski, P. V., et al. (2012). Integrating multi-criteria evaluation techniques with geographic information systems for landfill site selection: A case study using ordered weighted average. Waste Management, 32, 287–296.
Guagliardo, M. F. (2004). Spatial accessibility of primary care: Concepts, methods and challenges. International Journal of Health Geographics, 13, 1–13.
Guiqin, W., et al. (2009). Landfill site selection using spatial information technologies and AHP: A case study in Beijing, China. Journal of Environmental Management, 90, 2414–2421.
Hao, Q. L., & Dai, R. (2013). Dalian LNG terminal port site selection based on fuzzy evaluation. Journal of Dalian Maritime University, 39(103–106), 111.
Jordan, H., Roderick, P., Martin, D., & Barnett, S. (2004). Distance, rurality, and the need for care: access to health services in South West England. International Journal of Health Geographics, 3(21), 1–9.
Hu, R., Dong, S., Zhao, Y., Hu, H., & Li, Z. (2013). Assessing potential spatial accessibility of health services in rural China: A case study of Donghai county. International Journal for Equity in Health, 12, 1–11.
Jamal, I. A. (2016). Multi-criteria GIS analysis for school site selection in Gorno-Badakhshan Autonomous Oblast, Tajikistan. 55.
Jones, S. G., Ashby, A. J., Momin, S. R., & Naidoo, A. (2009). Spatial implications associated with using Euclidean distance measurements and geographic centroid imputation in health care research. Health Services Research, 45, 316–327. https://doi.org/10.1111/j.1475-6773.2009.01044.x
Khan, A. A. (1992). An integrated approach to measuring potential spatial access to health care services. Socioeconomic Planning Sciences, 26(4), 275–287. https://doi.org/10.1016/0038-0121(92)90004-O
Kim, Y., Byon, Y., & Yeo, H. (2018). Enhancing healthcare accessibility measurements using GIS: A case study in Seoul, Korea. PLoS ONE, 13, 1–19.
Korpela, J., & Tuominen, M. (1996). A decision aid in warehouse site selection. International Journal of Production Economics, 45, 169–180.
Langford, M., & Higgs, G. (2006). Measuring potential access to primary healthcare services: The influence of alternative spatial representations of population. The Professional Geographer, 58, 294–306.
Lawal, O., & Anyiam, F. E. (2019). Modelling geographic accessibility to Primary Health Care Facilities: Combining open data and geospatial analysis. Geo-Spatial Information Science, 22(3), 174–184. https://doi.org/10.1080/10095020.2019.1645508
Luo, W. (2004). Using a GIS-based floating catchment method to assess areas with shortage of physicians. Health & Place, 10, 1–11. https://doi.org/10.1016/S1353-8292(02)00067-9
Malczewski, J. (2006). GIS based multi-criteria decision analysis: A survey of the literature. International Journal of Geographical Information Science, 20(7), 703–726.
Mansour, S. (2016). Spatial analysis of public health facilities in Riyadh Governorate, Saudi Arabia: A GIS-based study to assess geographic variations of service provision and accessibility. Geo-Spatial Information Science, 5020, 1–13. https://doi.org/10.1080/10095020.2016.1151205
McGrail, M. R., & Humphreys, J. S. (2014). Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Applied Geography, 54, 182–188. https://doi.org/10.1016/j.apgeog.2014.08.005
Moisi, J. C., et al. (2010). Geographic access to care is not a determinant of child mortality in a rural Kenyan setting with high health facility density. BMC Public Health, 10, 1–9. https://doi.org/10.1186/1471-2458-10-142
Muller, I., Smith, T., Mellor, S., & Genton, B. (1998). The effect of distance from home on attendance at a small rural health centre in Papua New Guinea. International Journal of Epidemiology, 27, 878–884.
Murad, A. A. (2008). Defining health catchment areas in Jeddah city, Saudi Arabia: An example demonstrating the utility of geographical information systems. Geospatial Health, 2(2), 151–160.
Murseli, R. (2014). Land suitability location analysis for housing development using GIS.
Nikolakaki, P. A. (2004). GIS site-selection process for habitat creation: Estimating connectivity of habitat patches. Landscape and Urban Planning, 68, 77–94.
Okwaraji, Y. B., Mulholland, K., Schellenberg, J. R. M. A., Andarge, G., Admassu, M., & Edmond, K. M. (2012). The association between travel time to health facilities and childhood vaccine coverage in rural Ethiopia. A community based cross sectional study. BMC Public Health, 12, 1–9.
Onokerhoraye, A. G. (1999). Access and utilization of modern health cares facilities in the petroleum-proucing region of Nigeria: The case study of Bayelsa State. Retrieved from http://www.hspl.harvard.edu/research/taken./file/rep162.pdfj.
Oppio, A., Buffoli, M., Ovo, M. D., & Capolongo, S. (2016). Addressing decisions about new hospitals’ siting: A multidimensional evaluation approach. Annali Dell’istituto Superiore Di Sanita, 52(1), 78–87. https://doi.org/10.4415/ANN
Parry, J. A., Ganaie, S. A., & Bhat, M. S. (2018). GIS based land suitability analysis using AHP model for urban services planning in Srinagar and Jammu urban centers of J&K, India. Journal of Urban Management, 7(2), 46–56. https://doi.org/10.1016/j.jum.2018.05.002
Pyrialakou, V. D., Gkritza, K., & Fricker, J. D. (2016). Accessibility, mobility, and realized travel behavior: Assessing transport disadvantage from a policy perspective. Journal of Transport Geography, 51, 252–269. https://doi.org/10.1016/j.jtrangeo.2016.02.001
Rahimi, F., Goli, A., & Rezaee, R. (2017). Hospital location-allocation in Shiraz using Geographical Information System (GIS). Shiraz E-Medical Journal. https://doi.org/10.5812/semj.57572.Research
Ravallion, M. (2011). On multidimensional indices of poverty. The Journal of Economic Inequality, 9(2), 235–248. https://doi.org/10.1007/s10888-011-9173-4.hdl:10986/3346
Roy, U. (2016). Causative factors of social inequality and its impact on community health: A neighbourhood level study in Midnapore municipal area, West Bengal, India. The International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences. https://doi.org/10.5194/isprs-archives-XLI-B8-1417-2016
Saaty, T. (1980). The analytical hierarchy process (pp. 20–25). McGraw-Hill.
Saaty, T. (1994). Highlights and critical points in the theory and application of the analytic hierarchy process. European Journal of Operational Research, 74(3), 426–447.
Saeed, M. O., et al. (2012). An integrated AHP-GIS technique for landfill siting: A case study in Malaysia. Kuwait Journal of Science and Engineering, 39, 23–46.
Sandipan, D., Anirban, B., & Sagar, M. (2013). Study on urban land suitability assessment using remote sensing and GIS: A case study of Khairagarh, Chhattisgarh. International Journal of Computer Applications, 74(10), 20–26.
Sedenu, A. H., et al. (2016). Spatial analysis of the distribution pattern of primary healthcare facilities in Ile-Ife metropolis using geographic information system. Journal of Scientific Research and Reports. https://doi.org/10.9734/JSRR/2016/22339
Shannon, G. W., Bashshur, R. L., & Metzner, C. (1969). The concept of distance as a factor in accessibility and utilization of health care. Medical Care Research and Review, 26, 143–161.
Sharma. N. C. (2020). Why smaller cities in India witnessing faster growth?
Shukla, A., Kumar, V., & Jain, K. (2017). Site suitability evaluation for urban development using remote sensing, GIS and analytic hierarchy process (AHP). Proceedings of International Conference on Computer Vision and Image Processing. https://doi.org/10.1007/978-981-10-2107-7_34
Siddiqui, M. Z., Everett, J. W., & Vieux, B. E. (1996). Landfill siting using geographic information systems: A demonstration. Journal of Environmental Engineering, 122(6), 515–523.
Soltani, A., & Marandi, E. (2010). Hospital site selection using two-stage fuzzy multicriteriadecision making process. Journal of Urban and Environmental Engineering, 5(1), 32–43.
Uyan, M. (2014). MSW landfill site selection by combining AHP with GIS for Konya, Turkey. Environmental Earth Sciences, 71, 1629–1639.
Uzochukwu, B., Onwujekwe, O., Mbachu, C., Okwuosa, C., Etiaba, E., Nyström, M. E., & Gilson, L. (2016). The challenge of bridging the gap between researchers and policy makers: Experiences of a health policy research group in engaging policy makers to support evidence informed policy making in Nigeria. Globalization and Health, 12(1), 67. https://doi.org/10.1186/s12992-016-0209-1
Wang, F., & Luo, W. (2005). Assessing spatial and nonspatial factors for healthcare access: Towards an integrated approach to defining health professional shortage areas. Health & Place, 11, 131–146. https://doi.org/10.1016/j.healthplace.2004.02.003
Wang, L., Fan, H., & Wang, Y. (2018). Site selection of retail shops based on spatial accessibility and hybrid BP neural network. ISPRS International Journal of Geo-Information. https://doi.org/10.3390/ijgi7060202
Wong, N. S., Lee, S. S., & Lin, H. (2010). Assessing the spatial distribution of methadone clinic clients and their access to treatment. Harm Reduction Journal, 7, 1–6.
Yang, D. H., et al. (2006). Comparing GIS-based methods of measuring spatial accessibility to health services. Journal of Medical Systems, 30(1), 23–32. https://doi.org/10.1007/s10916-006-7400-5
Youzi, H., Nemati, G., & Emamgholi, S. (2017). The optimized location of hospital using an integrated approach GIS and analytic hierarchy process: A case study of Kohdasht City. International Journal of Economics, 7(1), 1–6. https://doi.org/10.4172/2162-6359.1000500
Zarkesh, M. K. (2005). Decision support system for floodwater spreading site selection in Iran. ITC.
Zhou, L., & Wu, J. (2012). GIS-based multi-criteria analysis for hospital site selection in Haidian district of Beijing.
Acknowledgements
The authors are grateful to Midnapore Municipality for providing the base map of the study area. The authors also would like to thank to all researcher for their competent research, encouragement, and valuable suggestion for undertaking this study.
Funding
This research did not receive any specific grant or financial support from funding agencies.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
There is no potential conflict of interest was reported by the authors.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dutta, B., Das, M., Roy, U. et al. Spatial analysis and modelling for primary healthcare site selection in Midnapore town, West Bengal. GeoJournal 87, 4807–4836 (2022). https://doi.org/10.1007/s10708-021-10528-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10708-021-10528-w