Abstract
The eye grows during childhood to position the retina at the correct distance behind the lens to enable focused vision, a process called emmetropization. Animal studies have demonstrated that this growth process is dependent upon visual stimuli, but dependent on genetic and environmental factors that affect the likelihood of developing myopia. The coupling between optical signal, growth, remodeling, and elastic response in the eye is particularly challenging to understand. To analyse this coupling, we develop a minimal morphoelastic model of an eye growing under intraocular pressure in response to visual stimuli. Distinct to existing three-dimensional finite-element models of the eye, we treat the sclera as a thin axisymmetric hyperelastic shell which undergoes local growth in response to external stimulus. This simplified analytic morphoelastic model provides a tractable framework in which we can evaluate various emmetropization hypotheses and understand different types of growth feedback. As an example, we demonstrate that local growth laws are sufficient to tune the global size and shape of the eye for focused vision across a wide range of parameter values.







Similar content being viewed by others
Code availability
The computer code used and generated in this work is freely available from https://gitlab.com/bjwalker/morphoelastic-eye.git
References
Morgan, I.G., Ohno-Matsui, K., Saw, S.M.: Myopia. Lancet 379(9827), 1739–1748 (2012)
Spillmann, L.: Stopping the rise of myopia in Asia. Graefe Arch. Clin. Exp. Ophthalmol. 258(5), 943–959 (2020)
Sherwin, J.C., Mackey, D.A.: Update on the epidemiology and genetics of myopic refractive error. Exp. Rev. Ophthalmol. 8(1), 63–87 (2013)
Dolgin, E.: The myopia boom. Nature 519(7543), 276–278 (2015)
Holden, B.A., Jong, M., Davis, S., Wilson, D., Fricke, T., Resnikoff, S.: Nearly 1 billion myopes at risk of myopia-related sight-threatening conditions by 2050 - time to act now. Clin. Exp. Optom. 98(6), 491–493 (2015)
Holden, B.A., Fricke, T.R., Wilson, D.A., Jong, M., Naidoo, K.S., Sankaridurg, P., Wong, T.Y., Naduvilath, T.J., Resnikoff, S.: Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123(5), 1036–1042 (2016)
Morgan, R., Speakman, J., Grimshaw, S.: Inuit myopia: an environmentally induced “epidemic”? Can. Med. Assoc. J. 112(5), 575 (1975)
Manjunath, V., Enyedi, L.: Pediatric myopic progression treatments: science, Sham, and promise. Curr. Ophthalmol. Rep. 2(4), 150–157 (2014)
Russo, A., Semeraro, F., Romano, M.R., Mastropasqua, R., Dell’Omo, R., Costagliola, C.: Myopia onset and progression: can it be prevented? Int. Ophthalmol. 34(3), 693–705 (2014)
Wu, P.C., Chuang, M.N., Choi, J., Chen, H., Wu, G., Ohno-Matsui, K., Jonas, J.B., Cheung, C.M.G.: Update in myopia and treatment strategy of atropine use in myopia control. Eye 33(1), 3–13 (2019)
Fatt, I., Weissman, B.: Physiology of the Eye: An Introduction to the Vegetative Functions, 2nd edn. Butterworths, London (1992)
Karimi, A., Razaghi, R., Navidbakhsh, M., Sera, T., Kudo, S.: Mechanical properties of the human sclera under various strain rates: elastic, hyperelastic, and viscoelastic models. J. Biomat. Tissue Eng. 7(8), 686–695 (2017)
Romano, M.R., Romano, V., Pandolfi, A., Costagliola, C., Angelillo, M.: On the use of uniaxial tests on the sclera to understand the difference between emmetropic and highly myopic eyes. Meccanica 52(3), 603–612 (2017)
Bryant, M.R., McDonnell, P.J.: Optical feedback-controlled scleral remodeling as a mechanism for myopic eye growth. J. Theor. Biol. 193(4), 613–622 (1998)
Grytz, R., Girkin, C.A., Libertiaux, V., Downs, J.C.: Perspectives on biomechanical growth and remodeling mechanisms in glaucoma. Mech. Res. Commun. 42, 92–106 (2012)
Grytz, R., Fazio, M.A., Girard, M.J., Libertiaux, V., Bruno, L., Gardiner, S., Girkin, C.A., Downs, J.C.: Material properties of the posterior human sclera. J. Mech. Behav. Biomed. 29, 602–617 (2013)
Grytz, R., El Hamdaoui, M.: Multi-scale modeling of vision-guided remodeling and age-dependent growth of the tree shrew sclera during eye development and lens-induced myopia. J. Elast. 129(1–2), 171–195 (2017)
Simonini, I., Pandolfi, A.: Customized finite element modelling of the human cornea. PLoS ONE 10(6), e0130426 (2015)
Sánchez, P., Moutsouris, K., Pandolfi, A.: Biomechanical and optical behavior of human corneas before and after photorefractive keratectomy. J. Cataract Refract. Surg. 40(6), 905–917 (2014)
Montanino, A., Gizzi, A., Vasta, M., Angelillo, M., Pandolfi, A.: Modeling the biomechanics of the human cornea accounting for local variations of the collagen fibril architecture. J. Appl. Math. Mech./Z. Angew. Math. Mech. 98(12), 2122–2134 (2018)
Pandolfi, A., Gizzi, A., Vasta, M.: A microstructural model of cross-link interaction between collagen fibrils in the human cornea. Philos. Trans. R. Soc. A 377(2144), 20180079 (2019)
Pandolfi, A.: Cornea modelling. Eye Vis. 7(1), 1–15 (2020)
Humphrey, J.D.: Cardiovascular Solid Mechanics. Cells, Tissues, and Organs. Springer, New York (2002)
Cowin, S.C.: Tissue growth and remodeling. Annu. Rev. Biomed. Eng. 6, 77–107 (2004)
Kuhl, E., Maas, R., Himpel, G., Menzel, A.: Computational modeling of arterial wall growth. Biomech. Model. Mechanobiol. 6(5), 321–331 (2007)
Horvat, N., Virag, L., Holzapfel, G.A., Sorić, J., Karšaj, I.: A finite element implementation of a growth and remodeling model for soft biological tissues: verification and application to abdominal aortic aneurysms. Comput. Methods Appl. Mech. Eng. 352, 586–605 (2019)
Cyron, C.J., Humphrey, J.D.: Growth and remodeling of load-bearing biological soft tissues. Meccanica 52(3), 645–664 (2017)
Goriely, A., Vandiver, R.: On the mechanical stability of growing arteries. IMA J. Appl. Math. 75(4), 549–570 (2010)
Taber, L.A.: Biomechanics of growth, remodeling and morphogenesis. Appl. Mech. Rev. 48, 487–545 (1995)
Moulton, D.E., Goriely, A.: Possible role of differential growth in airway wall remodeling in asthma. J. Appl. Physiol. 110(4), 1003 (2011)
Budday, S., Steinmann, P., Goriely, A., Kuhl, E.: Size and curvature regulate pattern selection in the mammalian brain. Extreme Mech. Lett. 4, 193–198 (2015)
Ambrosi, D., Ben Amar, M., Cyron, C.J., DeSimone, A., Goriely, A., Humphrey, J.D., Kuhl, E.: Growth and remodelling of living tissues: perspectives, challenges and opportunities. J. R. Soc. Interface 16(157), 20190233 (2019)
Diether, S., Schaeffel, F.: Local changes in eye growth induced by imposed local refractive error despite active accommodation. Vis. Res. 37(6), 659–668 (1997)
Wallman, J., Gottlieb, M.D., Rajaram, V., Fugate-Wentzek, L.A.: Local retinal regions control local eye growth and myopia. Science 237(4810), 73–77 (1987)
Foulds, W.S., Barathi, V.A., Luu, C.D.: Progressive myopia or hyperopia can be induced in chicks and reversed by manipulation of the chromaticity of ambient light. Investig. Ophthalmol. Vis. Sci. 54(13), 8004–8012 (2013)
Kröger, R., Wagner, H.J.: The eye of the blue acara (aequidens pulcher, cichlidae) grows to compensate for defocus due to chromatic aberration. J. Comp. Physiol. A 179(6), 837–842 (1996)
Liu, R., Qian, Y.F., He, J.C., Hu, M., Zhou, X.T., Dai, J.H., Qu, X.M., Chu, R.Y.: Effects of different monochromatic lights on refractive development and eye growth in Guinea pigs. Exp. Eye Res. 92(6), 447–453 (2011)
Werblin, F., Roska, B.: The movies in our eyes. Sci. Am. 296(4), 72–79 (2007)
Oyster, C.W.: The Human Eye. Sinauer, Sunderland (1999)
Rodriguez, E.K., Hoger, A., McCulloch, A.D.: Stress-dependent finite growth in soft elastic tissues. J. Biomech. 27(4), 455–467 (1994)
Goriely, A., Ben Amar, M.: On the definition and modeling of incremental, cumulative, and continuous growth laws in morphoelasticity. Biomech. Model. Mechanobiol. 6(5), 289–296 (2007)
Ambrosi, D., Ateshian, G., Arruda, E., Cowin, S., Dumais, J., Goriely, A., Holzapfel, G.A., Humphrey, J., Kemkemer, R., Kuhl, E., et al.: Perspectives on biological growth and remodeling. J. Mech. Phys. Solids 59(4), 863–883 (2011)
Goriely, A.: The Mathematics and Mechanics of Biological Growth. Interdisciplinary Applied Mathematics. Springer, New York (2017). https://books.google.co.uk/books?id=rgImDwAAQBAJ
Tongen, A., Goriely, A., Tabor, M.: Biomechanical model for appressorial design in magnaporthe grisea. J. Theor. Biol. 240(1), 1–8 (2006) [We note there is a sign error in equation (8) corrected in Woolley et al. (2014)]
Woolley, T.E., Gaffney, E.A., Oliver, J.M., Baker, R.E., Waters, S.L., Goriely, A.: Cellular blebs: pressure-driven, axisymmetric, membrane protrusions. Biomech. Model. Mechanobiol. 13(2), 463–476 (2014)
Shen, L., You, Q.S., Xu, X., Gao, F., Zhang, Z., Li, B., Jonas, J.B.: Scleral and choroidal volume in relation to axial length in infants with retinoblastoma versus adults with malignant melanomas or end-stage glaucoma. Graefe Arch. Clin. Exp. Ophthalmol. 254(9), 1779–1786 (2016)
Jonas, J.B., Holbach, L., Panda-Jonas, S.: Scleral cross section area and volume and axial length. PLoS ONE 9(3), 1–7 (2014)
Coulombre, A.J.: The role of intraocular pressure in the development of the chick eye. I. Control of eye size. J. Exp. Zool. 133(2), 211–225 (1956)
Maurice, D., Mushin, A.: Production of myopia in rabbits by raised body-temperature and increased intraocular pressure. Lancet 288(7474), 1160–1162 (1966)
Quinn, G.E., Berlin, J.A., Young, T.L., Ziylan, S., Stone, R.A.: Association of intraocular pressure and myopia in children. Ophthalmology 102(2), 180–185 (1995)
Girard, M.J., Dahlmann-Noor, A., Rayapureddi, S., Bechara, J.A., Bertin, B.M., Jones, H., Albon, J., Khaw, P.T., Ethier, C.R.: Quantitative mapping of scleral fiber orientation in normal rat eyes. Investig. Ophthalmol. Vis. Sci. 52(13), 9684–9693 (2011)
Jones, H., Girard, M., White, N., Fautsch, M.P., Morgan, J., Ethier, C., Albon, J.: Quantitative analysis of three-dimensional fibrillar collagen microstructure within the normal, aged and glaucomatous human optic nerve head. J. R. Soc. Interface 12(106), 20150066 (2015)
Gouget, C.L., Girard, M.J., Ethier, C.R.: A constrained von Mises distribution to describe fiber organization in thin soft tissues. Biomech. Model. Mechanobiol. 11(3–4), 475–482 (2012)
Coudrillier, B., Pijanka, J.K., Jefferys, J.L., Goel, A., Quigley, H.A., Boote, C., Nguyen, T.D.: Glaucoma-related changes in the mechanical properties and collagen micro-architecture of the human sclera. PLoS ONE 10(7), e0131396 (2015)
Melnik, A.V., Da Rocha, H.B., Goriely, A.: On the modeling of fiber dispersion in fiber-reinforced elastic materials. Int. J. Non-Linear Mech. 75 92–106 (2015)
Spencer, A.J.M.: Deformations of Fibre-Reinforced Materials. Clarendon, Oxford (1972)
Holzapfel, G.A., Ogden, R.W.: Constitutive modelling of arteries. Proc. R. Soc. A 466(2118), 1551–1597 (2010)
Melnik, A.V., Goriely, A.: Dynamic fiber reorientation in a fiber-reinforced hyperelastic material. Math. Mech. Solids 18(6), 634–648 (2013)
Zhang, L., Albon, J., Jones, H., Gouget, C.L., Ethier, C.R., Goh, J.C., Girard, M.J.: Collagen microstructural factors influencing optic nerve head biomechanicscollagen microstructural factors. Investig. Ophthalmol. Vis. Sci. 56(3), 2031–2042 (2015)
Green, A.E., Adkins, J.E.: Large Elastic Deformations. Oxford University Press, London (1970)
Holzapfel, G.A., Ogden, R.W.: Constitutive modelling of arteries. Proc. R. Soc. A 466(2118), 1551–1597 (2010)
Coudrillier, B., Boote, C., Quigley, H.A., Nguyen, T.D.: Scleral anisotropy and its effects on the mechanical response of the optic nerve head. Biomech. Model. Mechanobiol. 12(5), 941–963 (2013)
Girard, M., Downs, J.C., Bottlang, M., Burgoyne, C.F., Suh, J.F.: Peripapillary and posterior scleral mechanics, part II-experimental and inverse finite element characterization. J. Biomech. Eng. 131(5), 051012 (2009)
Destrade, M., Mac Donald, B., Murphy, J., Saccomandi, G.: At least three invariants are necessary to model the mechanical response of incompressible, transversely isotropic materials. Comput. Mech. 52(4), 959–969 (2013)
Gizzi, A., Pandolfi, A., Vasta, M.: A generalized statistical approach for modeling fiber-reinforced materials. J. Eng. Math. 109(1), 211–226 (2018)
Kalhöfer-Köchling, M., Bodenschatz, E., Wang, Y.: Structure tensors for dispersed fibers in soft materials. Phys. Rev. Appl. 13, 064039 (2020)
Wang, Y., Bensaid, N., Tiruveedhula, P., Ma, J., Ravikumar, S., Roorda, A.: Human foveal cone photoreceptor topography and its dependence on eye length. eLife 8, e47148 (2019)
Haughton, D.: In: Elastic Membranes. London Mathematical Society Lecture Note Series, pp. 233–267 (2001)
Atchison, D.A.: Optical models for human myopic eyes. Vis. Res. 46(14), 2236–2250 (2006)
Adkins, J.E., Rivlin, R.S.: Large elastic deformations of isotropic materials. IX. The deformation of thin shells. Philos. Trans. R. Soc. A 244(888), 505–531 (1952)
Gordon, R.A., Donzis, P.B.: Refractive development of the human eye. AMA Arch. Ophthalmol. 103(6), 785–789 (1985)
Howell, P., Kozyreff, G., Ockendon, J.: Applied Solid Mechanics. Cambridge University Press, Cambridge (2009)
Acknowledgements
The research leading to these results has received funding from the European Union Seventh Framework Programme (FP7/2007-2013) under grant agreement no. 309962 (HydroZONES). BJW is supported by the UK Engineering and Physical Sciences Research Council (EPSRC), Grant No. EP/N509711/1. AG acknowledges the support by the Engineering and Physical Sciences Research Council of Great Britain under research grants EP/R020205/1.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A: Shell Stresses
We briefly discuss the standard rationale for the functional form of the stresses specified by Eqns. (17a) and (17b). In a fully three-dimensional elastic body, the Cauchy stress, \(\mathbf{\sigma }\), is
where \(\mathbf{F}\) is the deformation gradient, \(\mathbf{C}=\mathbf{F}^{T}\mathbf{F}\) is the right Cauchy-Green tensor, \(p\) is the hydrostatic contribution to the stress associated with enforcing incompressibility, and \(W\) is the strain-energy function. For a detailed account, we direct the interested reader to, for example, the work of [61]. If we suppose that \(W=W(I_{1},I_{4},I_{6})\) where
so that \(I_{4}\) and \(I_{6}\) represent the stretch of fibres that lie in the directions \(\mathbf{a}\) and \(\mathbf{b}\), then
Furthermore, if we select the basis used for our scleral model so that \(\mathbf{F}\) is diagonal with entries \(\alpha _{s},\alpha _{\phi },\alpha _{n}\), define the fibre directions as in Eqns. (12a), (12b) and (13), so that \(I_{4}=I_{6}\), and finally require \(W(I_{1},I_{4},I_{6})=W(I_{1},I_{6},I_{4})\), then the off-diagonal terms in \(\mathbf{a}\otimes \mathbf{a}\) and \(\mathbf{b}\otimes \mathbf{b}\) cancel. Thus, the only non-zero components in Eq. (29) are
The shell’s thin geometry can be exploited as discussed in the context of membranes in [68]. We apply the key results in our shell model by working with resultant stresses of the form
and setting \(\sigma _{nn}=0\), often termed the ‘membrane assumption’. This is akin to noting that the curved shell is so thin that load across the surface due to the intraocular pressure is supported by in-shell tension, as opposed to stress across the shell thickness. The membrane assumption enables the elimination of the hydrostatic pressure, \(p\), and our incompressibility assumption, \(\alpha _{n} = 1/\alpha _{s}\alpha _{\phi }\), gives principal in-shell stress resultants of the form Eq. (14a), (14b).
Appendix B: Intrinsic Growth Capacity
In Eq. (19), we posed a phenomenological functional form for the intrinsic growth capacity \(g_{c}\), which we restate here as
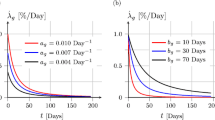
Via the parameters \(\Gamma \) and \(\delta \), this functional form allows for significant variation in the intrinsic growth capacity. This is illustrated in Fig. 8, from which increasing \(\Gamma \) can be seen to extend the region of high growth capacity, whilst \(\delta \) governs the sharpness of the interface between regions of high and low growth capacity.
The intrinsic growth capacity, \(g_{c}(\Sigma )\), and its dependence on its parameters \(\Gamma \) and \(\delta \). Increasing \(\Gamma \) can be seen to extend the region of high growth capacity away from the posterior sclera, whilst increasing \(\delta \) serves to smooth out the interface between high and low growth regions. Here, we have sampled \(\Gamma \in \{4,8,12\}\) and \(\delta \in \{2,6\}\), each with units of millimetres as in Fig. 6. The parameter \(\eta _{0}\) determines the maximum growth capacity
Appendix C: Optical Calculations
The optical components of the anterior eye, the cornea, anterior chamber, lens and vitreous chamber, focus the light wavefronts that are incident on the eye on a fictitious curved surface near the retina, which we term the best-focus surface. The position and shape of this surface are dependent on the wavelength of the incident light due to chromatic aberrations in the light focusing components. Modeling the geometrical and optical properties of the anterior eye as in [69], a raytracing algorithm was employed in order to compute the individual surfaces of best focus for red and blue incident light wavefronts, exemplified in Fig. 9. Dense arrays of parallel coherent rays were traced through the anterior optics, with the phase of the wavefront emerging on the posterior surface of the lens fitted to Zernike polynomial functions. These are propagated via a Kirchhoff integral and the Strehl ratio is computed on various test surfaces perpendicular to the central ray. The surface corresponding to the maximum Strehl ratio represents the best-focus surface, which is constructed for incident angles between 0 and 40 degrees, appealing to assumed axisymmetry. This approach may be readily extended to include the effects of additional or non-uniform lenses, enabling the modeling of corrective lenses and their effects on ocular development, for example.
Computing the best-focus surfaces. A dense array of parallel, coherent rays (thin lines) is traced through the anterior optics (cornea, pupil, lens – medium lines) and the phase of the wavefront emerging through the posterior surface of the lens is fitted to Zernike polynomial functions. Bottom – Left: Example of a lens-emerging waveform. A Kirchhoff integral is applied to further propagate the wavefront and compute its modulation transfer function (MTF) on small surfaces perpendicular to the central ray. Bottom – Right: Example MTFs along probed surfaces. Surface C maximizes the Strehl ratio and hence corresponds to the best-focus surface for this wavelength. Computing the best-focus distance for a range of incidence angles (0-40 degrees), assuming axial symmetry, we reconstruct the best-focus surfaces for two wavelengths: 400 nm (blue) and 600 nm (red)
Appendix D: Initial and Boundary Conditions
When considering a non-uniform scleral thickness, following [11] we prescribe
as shown in Fig. 10 alongside the initial fibre orientation, prescribed as
following the observations of [16, 51].
At the anterior point of the sclera, we match the scleral displacement to the inflation of a thin, spherically symmetric, non-growing shell of uniform thickness with no fibres, minimally modeling the cornea. Firstly, for this simple shell, we see that \(\alpha _{s}^{c}=\alpha _{\phi }^{c}\), so for notational convenience we denote the stretch simply by \(\alpha \), where the superscript on all other variables denotes that we are considering the cornea. Since the corneal reference configuration is spherical, we have
for \(\Sigma ^{c}\in [0,\pi R_{0}^{c}]\), where \(R_{0}^{c}\) is the radius of the sphere. The position of a point on the inflated sphere is thus given by
where \(B\) is a constant of integration. The constraint of spherical symmetry ensures there is no normal shear force, \(Q^{c}=0\), so that the shell deforms as a membrane. The solution to this problem is presented in [70], where it is shown that
where \(C^{c}\) is the neo-Hookean constant, \(H^{c}\) is the undeformed thickness and \(R_{0}^{c}\) is the undeformed radius of the shell. We take \(C^{c}\), \(H^{c}\) and \(R_{0}^{c}\) to have values based on the mechanics of the cornea and we calculate \(\alpha \) for the required pressure difference numerically, restricting \(\alpha \in (1,7^{(1/6)})\) due to the non-injective relation between \(\alpha \) and \(\Delta P\). In particular, the upper limit here is the \(\alpha \) value corresponding to the maximum of \(1/\alpha -1/\alpha ^{7}\) for \(\alpha >1\), it placing a bound on the maximum pressure difference that we can consider, though we don’t vary the intraocular pressure in this work. Finally, evaluating the shape of the cornea at the point of attachment to the sclera, we find the boundary conditions for the scleral shell to be
Appendix E: Implementation
The governing equations presented in Sect. 2.6 have a singularity when \(r=0\), so we solve the system numerically on the truncated domain \(\sigma \in [\sigma (\varepsilon ,t),\sigma (L,t)]\) for \(0<\varepsilon \ll 1\). By expanding the variables \(r\), \(\theta \), \(\alpha _{s}\), \(\kappa _{s}\) and \(Q\) around \(\sigma =0\) and evaluating at \(\sigma =\sigma (\varepsilon ,t)\), following [45], then substituting the expansions into (21a), (21c), (21d), (21e) and Eq. (22) subject to Eq. (24), it becomes clear that the singularity is removable for compatible initial fibre directions. Indeed, isotropy is required as \(\sigma \rightarrow 0\) because any preferred direction is undefined at the pole, and if we do not require \(\psi \rightarrow \pi /4\) as \(\sigma \rightarrow 0\) then there is a singularity in the stress as \(\sigma \rightarrow 0\) in the fibre-reinforced shells. Intuitively, this is due to the preferred fibre orientation needing to change direction increasingly quickly as we approach the pole. In order to circumvent this in all the fibre-reinforced simulations in this work, we ensure that \(\psi \rightarrow \pi /4\) as \(\sigma \rightarrow 0\), subject to which the stress is finite and the boundary conditions on \(r\) and \(\theta \) can be replaced by the notationally cumbersome
where we have suppressed the \(t\)-dependence of all quantities here for brevity. Now considering \(Q\), we further manipulate Eq. (21a), (21b), (21c) (21d), (21e) and (21f) to admit the first integral
where \(A\) is a constant. Since we require solutions that pass through \(r=0\) with \(\theta =\pi /2\), we find \(A=0\). Thus, evaluating Eq. (40) at \(\sigma =\sigma (\varepsilon ,t)\) provides the analogous truncated boundary condition for \(Q\). Note that whilst it is possible to use Eq. (40) to eliminate \(Q\) from Eqns. (21a), (21c) to (21e) and (22), preliminary numerical simulations suggest that it is easier to solve the five ordinary differential equations than the reduced system. Hence, we retain \(Q\) in the governing equations and use Eq. (40) as a check on the numerical solutions.
We utilise MATLAB’s inbuilt adaptive boundary problem solver bvp4c to solve equations Eqns. (21a), (21c) to (21e) and (22) subject to the boundary conditions truncated boundary conditions. The initial conditions are provided on a regular grid for \(\Sigma \in [0,L]\) and growth is approximated with an explicit Euler scheme for Eqns. (9) and (10). For each simulation, we ensure that the solution has converged with respect to our choices of grid size, timestep, truncation point and error tolerances in the solver. For example, the simulations in Fig. 3 were rerun on a refined spatial grid, with a smaller timestep, with a lower error tolerance in the bvp4c solver, and with a reduced truncation value \(\varepsilon \). The largest relative errors in the variables \(\kappa _{s}\), \(\alpha _{s}\), \(r\) and \(\theta \) at \(t=1\) in this refined simulation are \(1.7\times 10^{-3}\), \(2.1\times 10^{-5}\), \(9.4\times 10^{-4}\) and \(7.4\times 10^{-4}\) respectively, well below practical tolerance. Typical parameter values for the simulations in this work are given in Table 1. Typical simulation runtime on modest hardware (Intel® Core™ i7-6920HQ CPU) is, without significant optimisation of the implementation, approximately two minutes.
Rights and permissions
About this article
Cite this article
Kimpton, L.S., Walker, B.J., Hall, C.L. et al. A Morphoelastic Shell Model of the Eye. J Elast 145, 5–29 (2021). https://doi.org/10.1007/s10659-020-09812-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10659-020-09812-6