Abstract
Research has indicated that sex hormone-binding globulin (SHBG) is associated with glucose homeostasis and may play a role in the etiology of type 2 diabetes (T2D). While it is unclear whether SHBG may mediate sex differences in glucose control and subsequently, incidence of T2D. We used observational data from the German population-based KORA F4 study (n = 1937, mean age: 54 years, 41% women) and its follow-up examination KORA FF4 (median follow-up 6.5 years, n = 1387). T2D was initially assessed by self-report and validated by contacting the physicians and/ or reviewing the medical charts. Mediation analyses were performed to assess the role of SHBG in mediating the association between sex (women vs. men) and glucose- and insulin-related traits (cross-sectional analysis) and incidence of T2D (longitudinal analysis). After adjustment for confounders, (model 1: adjusted for age; model 2: model 1 + smoking + alcohol consumption + physical activity), women had lower fasting glucose levels compared to men (β = -4.94 (mg/dl), 95% CI: -5.77, -4.11). SHBG levels were significantly higher in women than in men (β = 0.47 (nmol/l), 95% CI:0.42, 0.51). Serum SHBG may mediate the association between sex and fasting glucose levels with a proportion mediated (PM) of 30% (CI: 22–41%). Also, a potential mediatory role of SHBG was observed for sex differences in incidence of T2D (PM = 95% and 63% in models 1 and 2, respectively). Our novel findings suggest that SHBG may partially explain sex-differences in glucose control and T2D incidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ample evidence indicates that the alarming rise in obesity will continue to drive a devastating increase in the prevalence and burden of type 2 diabetes (T2D) over the next decades [1]. The prevalence and incidence of T2D and the associated risk factors such as obesity, glucose and insulin impairments differ according to the sex [2]. In general, prevalence of diabetes is higher in men than women while aging reduces this difference [3]. There is a growing body of evidence that sex differences exist in diabetes outcomes and related complications, highlighting the need for further sex-specific research [4].
Certainly, some of these sex differences are determined by genetics, socio-cultural and most largely by biological factors [5]. Sex hormones and sex hormone binding globulin (SHBG) have been suggested as potential determinants of these sex differences [6]. The association of sex hormones (testosterone, estradiol, etc.) with T2D have been widely addressed [7], however, the independent role of SHBG is still a topic of debate. While SHBG has traditionally been viewed as a passively binding protein that simply regulates the levels of free sex hormones, in recent years its independent biological properties have been highlighted [5]. Emerging evidence suggests that SHBG may directly influence various physiological processes and disease states, offering a promising avenue for further investigation and potential therapeutic development [8]. Typically, men have lower levels of SHBG compared to women [5]. In adult men, SHBG levels are stable for many years but tend to increase with age [9] while SHBG progressively decreases in adult women between the ages of 20 and 60 and then begins to increase [10].
Findings from a large systematic review and meta-analysis of observational studies indicated that lower levels of SHBG are associated with insulin resistance and higher risk of T2D, with stronger associations seen in women compared to men [7]. Mendelian randomization studies have supported a causal role of SHBG in T2D, although the causal effects have been shown to be weaker than the estimates observed in observational studies [11, 12]. However, there is limited evidence on sex-specific mendelian randomization studies on causal role of SHBG in T2D [13]. Therefore, our study lays the groundwork for future research to explore the potentially distinct causal pathways in men and women.
We hypothesized that SHBG levels may explain sex differences for glucose homeostasis and incidence of T2D. To test this hypothesis, we aimed to (i) investigate the association of sex with glucose- and insulin-related traits and incidence of T2D; (ii) to investigate the associations of sex with SHBG and SHBG with glucose- and insulin-related traits and incidence of T2D; and (iii) to assess the potential mediating role of SHBG and its extent in the association of sex with incidence of T2D in a population-based setting of middle-aged and elderly adults. Particularly, we also focused to identify and quantify SHBG’s potential mediating role in broader aspects of glucose homeostasis, such as glucose- and insulin-related traits, an area that has received less attention.
Methods
Setting and study population
This study was conducted among participants of the prospective population-based Cooperative Health Research in the Region of Augsburg (KORA) study, selected from population registries in the city of Augsburg (Germany) and two surrounding counties. A total of 4261 middle-aged and older adults, aged 25–74 years, were included at baseline between 1999 and 2001 (KORA S4). Follow-up examinations were performed after 7 years, between 2006 and 2008 (KORA F4) and after 14 years, between 2013 and 2014 (KORA FF4). The KORA F4 study enrolled 3080 participants of whom 2161 were followed up in KORA FF4. All study participants have provided written informed consent. The study was approved by the Ethics Committees of the Bavarian Chamber of Physicians (Ethical Approval Number 06068) adhering to the declaration of Helsinki. Details of the study population and data collection have been reported elsewhere [14].
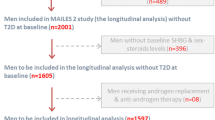
The present analysis includes data from the KORA F4 at baseline and KORA FF4 at follow-up. We excluded participants who withdrew consent (n = 3), non-fasting participants and participants with missing information on fasting status (n = 21), participants with T2D (n = 217) and type 1 diabetes (n = 7), participants with unclear diabetes diagnosis (n = 75), participants newly diagnosed with diabetes by oral glucose tolerance test (OGTT) (n = 115), participants diagnosed with medication induced diabetes (n = 1), participants with missing information on diabetic medications (n = 2), participants taking external hormone therapy (including estrogen and/or progestin, anti-estrogens) (n = 240), participants with surgeries (including hysterectomy, oophorectomy) (n = 232), participants with missing information on surgeries (n = 1), and participants with missing information on SHBG, sex hormones and glucose- and insulin-related traits (fasting glucose levels, insulin levels, 2 h-glucose levels, homeostatic model assessment for insulin resistance (HOMA-IR)) (n = 229). Thus, 1937 individuals were included in the cross-sectional analysis, while 1387 participants were included for the longitudinal analysis. (Fig. 1).
Sexual hormone-binding globulin, glucose homeostasis and T2D assessments
SHBG was measured in serum that was stored at -80 °C, until being assayed. Measurements of SHBG in serum were performed using the ARCHITECT SHBG assay, a chemiluminescent microparticle immunoassay (CMIA) for absolute quantification of SHBG (Abbott Diagnostics) (measuring range SHBG: 0-250 nmol/L, with intra-assay coefficient of variation: 4.29% and inter-assay coefficient of variation range: 6.39–10.3%). Known T2D was self-reported, validated by a physician or medical record review, or self-reported current use of glucose-lowering medications. Participants without known T2D were given a standard 75 g OGTT. Among those receiving an OGTT, newly diagnosed diabetes was defined according to the 1999 World Health Organization diagnostic criteria (i.e. fasting glucose > 6.9 mmol/L and/or 2 h-glucose > 11.0 mmol/L) [15]. Incident diabetes at follow-up was a combination of diabetes clinically diagnosed during the follow-up period plus those who had newly diagnosed diabetes based on OGTT data at FF4 among those who did not have diabetes at baseline. Fasting glucose was measured in fresh serum using hexokinase-G6PD (GLUFlex; Dade Behring, USA). Fasting insulin was measured in thawed serum by an elctrochemiluminescence immunoassay (Cobas e602 Immunoassay Analyser; Roche Diagnostics GmbH, Germany).
Assessment of covariates
Information on age, sex, medication use (antihypertensive medications and lipid-lowering medications (yes/ no)), hypertension (yes/no), smoking status (regular smoker, irregular smoker, ex-smoker, never-smoker), alcohol consumption (g/day), physical activity (inactive/ active) was collected by trained medical staff using a standardized interview [16]. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Waist circumference (cm) was measured at the level midway between the lower rib margin and the iliac crest while the participants breathed out gently. High C-reactive protein was quantified in plasma using a high-sensitivity latex-enhanced nephelometric assay (BN II Analyzer, Dade Behring). Thyroid-stimulating hormone was measured using electrochemiluminescent methods (Dimension Vista Systems; Siemens, Germany). Total cholesterol was measured in fresh serum by enzymatic methods (CHOL Flex).
Statistical analyses
Continuous data are presented as mean ± SD or as median (inter quartile range (IQR)) when the variables are non-normally distributed. Categorical data are shown as percentages. We log-transformed non-normally distributed variables prior to further regression and subsequently mediation analysis. Differences in baseline characteristics of men and women were assessed with independent-sample t-test or Mann-Whitney U-test for continuous variables and the chi-squared test for categorical variables.
Multivariable linear regression models were used to investigate the association of sex (women vs. men) with SHBG (exposure-mediator) and glucose- and insulin-related traits (fasting glucose levels, 2 h-glucose levels, fasting insulin levels, and HOMA-IR) (exposure-outcome), as well as SHBG with glucose- and insulin-related traits (mediator-outcome). In addition, the association of sex and SHBG with incidence of T2D was assessed using multivariable logistic regression analysis. In model 1, all analyses were adjusted for age and additionally for physical activity, alcohol consumption and smoking in model 2. These models were selected based on potential confounders according to the published literature and the second one was considered as the main model in the mediation analysis.
We performed the mediation analysis to determine whether SHBG is a potential mediator in the association of sex (women vs. men) with glucose- and insulin-related traits and incidence of T2D and if so to what extent. The hypothesized causal structure of the association between sex (the exposure) and the outcome (glucose- and insulin-related traits / incidence of T2D) with SHBG as a mediator are shown as a Directed Acyclic Graph (DAG) in Supplementary Figs. 1–3.
-
1)
We performed several sensitivity analyses to investigate the robustness of our results. 1) We defined a third model with additional adjustments for waist circumference, systolic blood pressure, total cholesterol, high C-reactive protein, thyroid-stimulating hormone, antihypertensive medications and lipid lowering medications. We did not consider model 3 as one of our main models since the covariates in this model are more likely to play an intermediate role in the pathways of investigated associations, rather than being confounders. Thus, the findings of the third model should be interpreted with caution as stated by VanderWeele [17, 18] - the confounding assumptions for mediation analysis are extremely important and violations in these assumptions can give rise to misleading results.
-
2)
To investigate the effect of age, we divided the participants into two groups based on the median age of 53 and repeated the analyses. 3) To account for the effect of weight, we repeated the mediation analysis for subset of individuals with normal weight (BMI < 25) and with overweight and obesity (BMI ≥ 25). 4) To investigate the independent role of SHBG from testosterone, we added testosterone to the main models and repeated the mediation analysis. This sensitivity analysis was run only for fasting glucose levels as an outcome, and we were not able to rerun the analyses for incidence of T2D as the incidence of T2D in the subsamples was limited.
The direct effect (DE), indirect effect (IE), total effect (TE) and proportion mediated (PM) were estimated using regression based approach in a counterfactual framework developed by Valeri and VanderWeele [19]. Non-parametric bootstrapping (200 times) was used to estimate 95% CI and P values. The proportion mediated (%) was estimated as (ORDirect × (ORIndirect – 1)/(ORDirect × ORIndirect – 1) ×100 in the case of a binary outcome (odds ratio(OR)) or as (βIndirect/βTotal)×100 in the case of a continuous outcome (β coefficient (β)) [18]. The DE can be conceived of as the exposure effect on the outcome at a fixed level of the mediator variable, which is different from the TE, the latter representing the overall effect of exposure on the outcome. The IE can be conceived of as the effect on the outcome resulting from the changes of the exposure due to different mediator levels (SHBG). Of note, DE and IE should operate in the same direction in order for the PM to provide meaningful summary [20].
Multiple imputations were done to handle missing values on covariates. Statistical analyses were performed using R statistical software, version 4.2.2 with CMAverse package [21]. All results were considered statistically significant at a p-value < 0.05.
Results
Baseline characteristics of the overall population and stratified by sex are shown in Table 1. Overall, in the cross-sectional analysis 1937 men (n = 1130) and women (n = 807) with a mean age of 54.0 ± 12.8 years and median BMI of 26.5 kg/m2 (IQR: 24.2, 29.6) were included. The overall mean and SD of fasting glucose and 2 h-glucose were 94.2 ± 9.4 and 106.7 ± 30.1 mg/dl, respectively. Fasting glucose levels, 2 h-glucose levels, fasting insulin levels, and HOMA-IR were significantly higher in women compared to men (p < 0.001). No significant difference was observed in the level of physical activity between men and women. Alcohol consumption and intake of medications were higher in men and a sex difference was observed in smoking status (p < 0.001). Over a median follow-up of 6.5 years, 99 incident T2D cases (70 men, 29 women) were recorded.
Sex, SHBG, glucose- and insulin-related traits and T2D
Supplementary Table 1 presents the association of sex (women vs. men) with SHBG and glucose- and insulin-related traits. SHBG levels were significantly higher in women than in men. Women had lower fasting glucose, fasting insulin and HOMA-IR levels in both model 1 and 2. No significant sex differences were observed for 2 h-glucose levels.
The association of SHBG and glucose- and insulin-related traits are shown in Supplementary Table 2. Inverse associations of SHBG with fasting and 2 h-glucose levels, fasting insulin, and HOMA-IR were observed in both model 1 and 2.
Sex differences were observed for the incidence of T2D based on our model 2 (OR: 0.56, CI: 0.34, 0.92) (Supplementary Table 3). An inverse association was seen between SHBG and T2D in model 1 (OR: 0.38, CI: 0.23, 0.62) and model 2 (OR: 0.37, CI: 0.22, 0.60) (Supplementary Table 3).
Mediation analysis
Mediation analysis was performed to assess whether, and to what extent, the sex differences (women vs. men) in glucose- and insulin-related traits and incidence of T2D were mediated by serum SHBG levels.
The results of the mediation analysis on glucose- and insulin-related traits are shown in Table 2. The findings of the mediation analysis showed a significant mediatory effect of SHBG on the association between sex and fasting glucose levels in both DE and IE. DE were (β= -3.68, 95% CI: -4.53, -2.86) in model 1 and (β= -3.42, 95% CI: -4.42, -2.61) in model 2. IE were (β= -1.56, 95% CI: -1.99, -1.18) and (β= -1.51, 95% CI: -1.93, -1.13) in model 1 and 2, respectively. In both models, serum SHBG was estimated to mediate up to PM 30% (CI: 22–41%) of the association.
The DE and IE were in opposite directions for mediation analysis of SHBG on the association between sex and 2 h-glucose levels, fasting insulin levels and HOMA-IR (known as inconsistent mediation). In the second model, IE of SHBG for 2 h-glucose levels, fasting insulin levels and HOMA-IR were (β= -5.17, 95% CI: -6.84, -3.89), (β= -0.16, 95% CI: -0.19, -0.14) and (β= -0.18, 95% CI: -0.21, -0.15), respectively.
The mediation analysis of SHBG on the association between sex and incidence of T2D is presented in Table 3. The DE of this association was not statistically significant in neither model 1 (OR: 0.98, 95% CI: 0.61, 1.60) nor model 2 (OR: 0.82, 95% CI: 0.49, 1.28), while the IE was statistically significant in both models 1 (OR: 0.63, 95% CI: 0.50, 0.80) and model 2 (OR: 0.63, 95% CI: 0.50, 0.83), showing the mediatory effect of SHBG on this association. PM was estimated to be 95% in model 1 and 63% in model 2. The results of all sensitivity analyses are provided in Supplementary information 1.
Discussion
To our best knowledge, the current study is the first investigation examining the mediatory role of SHBG, an important biological factor, in explaining sex differences in glucose metabolism and incidence of T2D. Our results indicated a greater level of SHBG in women than in men, which may explain sex differences in glucose levels and incidence of T2D. We observed a high estimated PM by SHBG in the association between sex (women vs. men) and fasting glucose levels (30%) and incidence of T2D (63%).
Our findings on sex differences for SHBG, glucose homeostasis and T2D are in line with previous studies, showing in general higher SHBG levels [22], lower glucose levels [23], lower insulin resistance [23] and lower incidence of T2D [24] in women compared to men.
Our results reinforce previous evidence on the association between SHBG, glucose biomarkers and T2D incidence. The results of a large systematic review and meta-analysis of observational studies on endogenous sex hormones and risk of T2D showed an inverse association of SHBG and risk of T2D in both sexes, although the findings were stronger in women than in men [7]; the same inverse association of SHBG with T2D was found in another systematic review and meta-analysis performed exclusively on women [25]. In support of observational evidence, mendelian randomization studies have also found a causal role of SHBG on T2D [12, 13]. Above all, our study underscores the necessity of developing sex-specific mendelian randomization studies.
A novel finding of our study is the potential mediating role of SHBG on glucose homeostasis. To our knowledge, the current study is the first study that identified SHBG as a potential mediator in the association between sex and glucose hemostasis. We found the mediating effect of SHBG, which was independent of confounding factor and some of potential intermediate factors including age and obesity. Findings of a recent study based on a large population-based cohort on aging, cardiovascular risk and SHBG, found a clear sex-specific pattern of SHBG levels with age. These novel findings highlighted the importance of considering the age-related changes in SHBG levels to avoid controversial results [22]. Thus, we tried to perform the analysis for different subsets of individuals based on median age. Of note, the potentially mediatory role of SHBG on sex differences in glucose levels was observed in participants < 53 years of age and > = 53 years, with a lower PM in those aged 53 and over. The median (IQR) of SHBG levels for individuals aged < 53 were 40.8 (29.6–55.2) and 81.9 (61.4-105.5) and for those > = 53 years were 54.3 (40.2–71.2) and 69.7 (50-97.3) for men and women, respectively. The SHBG levels in men increased with aging, while they decreased in women, resulting in the narrower variation of SHBG levels between men and women in adults aged 53 years and over. This has resulted in lower PM (19–22%) in older individuals compared to higher PM (29–30%) in younger adults.
We also stratified the mediation analysis by BMI categories, given the robust evidence linking overweight and obesity to altered SHBG levels [26]. Interestingly, while the mediation effect of SHBG on sex-differences in glucose levels was strongest in individuals with normal weight, it remained significant across both BMI subsets. The lower PM observed in overweight and obese individuals could be attributed to the well-established reduction in SHBG levels associated with increased adiposity [27, 28].
Various mechanisms have been proposed regarding sex differences in risk of T2D, with steroid hormones being the important ones. Research has indicated that SHBG may interfere with the pathogenesis and development of T2D by regulating the biologic effects of sex hormones (testosterone and estrogen) on peripheral tissues (e.g. muscle, fat and liver).
Increased risk of T2D with low SHBG levels may represent the stronger effects and possible interactions of more bioavailable testosterone and estradiol, and thus, explaining the sex-dependent associations of SHBG. Some studies have proposed a sex-dependent association of SHBG with risk of T2D. For instance, the study done by Haffner et al. indicated that SHBG levels, independent of insulin levels, predict the development of T2D in women but not in men [29]. Another observational study found that SHBG was associated with higher risk of T2D in women rather than men [30]. The findings of a recent mediation analysis on the Masstricht study, investigating the mediatory role of SHBG on the association between intrahepatic lipid content (IHL) and T2D showed greater mediatory role of SHBG in women compared to men, with a PM of 17.2% and 50.9% of SHBG on the association of IHL and T2D for men and women, respectively [31].
Rather than interaction with other sex hormones, there is also a strong evidence supporting independent effect of SHBG on T2D [32]. Studies have found several polymorphisms in the SHBG gene to be associated with insulin resistance and T2D, showing that altered SHBG physiology may trigger the pathogenesis of T2D [11,12,13]. Additionally, it has been shown that SHBG may mediate cell-surface signaling, cellular delivery, and biological action of sex hormones via activation of a specific plasma receptor directly [12, 33]. To test this hypothesis, we repeated the mediation analysis additionally adjusting for testosterone levels in model 1 and 2 and found that the mediatory role of SHBG was still significant and large for sex differences in glucose levels and T2D. In support of some previous literature, our findings suggest that SHBG may play a more significant role in T2D risk rather than previously recognized mechanisms linked to androgens, which warrants further investigations. However, it’s important to exercise caution when interpreting these results, as our mediation analysis model was adjusted for testosterone, a potential mediator, compromising as such the mediation analysis assumptions [17, 18].
Other novel findings of the current study are the inconsistent mediatory role of SHBG on fasting insulin levels, 2 h-glucose levels and HOMA-IR. While we found no significant associations for the DE of sex on these traits, the IE for the above-mentioned outcomes were significant and considerable, which is sometimes called inconsistent mediation [20].
Our findings could provide more insights to implement randomized clinical trials targeting SHBG in women suffering from low levels of SHBG. Although a large number of clinical trials have been investigating the effect of different interventions like dietary interventions [34], medications [35] and hormonal therapy [36] on SHBG levels, to our knowledge, no clinical trial has investigated the effect of SHBG administration on health outcomes.
This current study has several strengths and limitations. This was the first study to report the mediatory role of SHBG on sex differences in glucose metabolism and incidence of T2D. By using data from the KORA study, we were able to investigate the mediatory role of SHBG on the association of sex and glucose homeostasis in a large cohort of individuals both cross-sectionally and longitudinally with a limited proportion of missing values for confounders. OGTT were performed at both baseline and follow-up which helped us to explore the development of clinically diagnosed T2D and also newly OGTT-diagnosed T2D. Having detailed data on menopausal status (e.g. experiencing oophorectomy or hysterectomy) and on hormonal therapy (e.g. anti-estrogens, estrogens, progestin, hormone replacement therapy, androgens, antiandrogens, enzyme inhibitors, gonadotropin releasing hormones, and anabolic steroids) was helpful to account for these important confounding factors which may not be well-collected in other cohort studies. As a limitation, we were not able to repeat the sensitivity analysis stratified by age and BMI categories for T2D due to the limited number of incident cases. Lack of replication and not considering the non-alcoholic fatty liver disease in our statistical models are other limitations of our study. In addition, we could not perform other preferable modeling such as Cox regression analysis, due to the lack of exact time to event data. Finally, this study was conducted among a German population, which limits the generalizability of our findings to other ethnicities.
In conclusion, in a large-scale population-based study we showed that serum SHBG is a potential mediator in the association between sex and glucose levels as well as incident T2D. Whether SHBG could be a target therapy for reducing sex differences in diabetes needs larger and well-designed clinical studies.
Data availability
All available data are provided within the manuscript and supplementary files.
References
Sun H, Saeedi P, Karuranga S et al. IDF diabetes atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes research and clinical practice. 2021:109119.
Huebschmann AG, Huxley RR, Kohrt WM, Zeitler P, Regensteiner JG, Reusch JE. Sex differences in the burden of type 2 diabetes and cardiovascular risk across the life course. Diabetologia. 2019;62(10):1761–72.
Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157:107843.
Arnetz L, Ekberg NR, Alvarsson M. Sex differences in type 2 diabetes: focus on disease course and outcomes. Diabetes, metabolic syndrome and obesity: targets and therapy. 2014:409 – 20.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev. 2016;37(3):278–316.
Arnold AP, Cassis LA, Eghbali M, Reue K, Sandberg K. Sex hormones and sex chromosomes cause sex differences in the development of cardiovascular diseases. Arterioscler Thromb Vasc Biol. 2017;37(5):746–56.
Ding EL, Song Y, Malik VS, Liu S. Sex differences of endogenous sex hormones and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2006;295(11):1288–99.
Arathimos R, Millard LA, Bell JA, Relton CL, Suderman M. Impact of sex hormone-binding globulin on the human phenome. Hum Mol Genet. 2020;29(11):1824–32.
Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. J Clin Endocrinol Metabolism. 2001;86(2):724–31.
Maggio M, Lauretani F, Basaria S, et al. Sex hormone binding globulin levels across the adult lifespan in women—the role of body mass index and fasting insulin. J Endocrinol Investig. 2008;31:597–601.
Wang Q, Kangas AJ, Soininen P, et al. Sex hormone-binding globulin associations with circulating lipids and metabolites and the risk for type 2 diabetes: observational and causal effect estimates. Int J Epidemiol. 2015;44(2):623–37.
Perry JR, Weedon MN, Langenberg C, et al. Genetic evidence that raised sex hormone binding globulin (SHBG) levels reduce the risk of type 2 diabetes. Hum Mol Genet. 2010;19(3):535–44.
Ding EL, Song Y, Manson JE, et al. Sex hormone–binding globulin and risk of type 2 diabetes in women and men. N Engl J Med. 2009;361(12):1152–63.
Holle R, Happich M, Löwel H, Wichmann H-E, Group nftMKS. KORA-a research platform for population based health research. Das Gesundheitswesen. 2005;67(S 01):19–25.
Organization WH. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus: World health organization1999.
Lau LHY, Nano J, Cecil A, et al. Cross-sectional and prospective relationships of endogenous progestogens and estrogens with glucose metabolism in men and women: a KORA F4/FF4 study. BMJ Open Diabetes Res Care. 2021;9(1):e001951.
VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34:211–9.
VanderWeele TJ. Mediation analysis: a practitioner’s guide. Annu Rev Public Health. 2016;37:17–32.
Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137.
VanderWeele T. Explanation in causal inference: methods for mediation and interaction. Oxford University Press; 2015.
Shi B, Choirat C, Coull BA, VanderWeele TJ, Valeri L. CMAverse: a suite of functions for reproducible causal mediation analyses. Epidemiology. 2021;32(5):e20–2.
Aribas E, Kavousi M, Laven JS, Ikram MA, Roeters van Lennep JE. Aging, cardiovascular risk, and SHBG levels in men and women from the general population. J Clin Endocrinol Metabolism. 2021;106(10):2890–900.
Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009;6:60–75.
Mauvais-Jarvis F. Gender differences in glucose homeostasis and diabetes. Physiol Behav. 2018;187:20–3.
Muka T, Nano J, Jaspers L, et al. Associations of steroid sex hormones and sex hormone–binding globulin with the risk of type 2 diabetes in women: a population-based cohort study and meta-analysis. Diabetes. 2017;66(3):577–86.
Cooper LA, Page ST, Amory JK, Anawalt BD, Matsumoto AM. The association of obesity with sex hormone-binding globulin is stronger than the association with ageing–implications for the interpretation of total testosterone measurements. Clin Endocrinol. 2015;83(6):828–33.
Tchernof A, Toth MJ, Poehlman ET. Sex hormone-binding globulin levels in middle-aged premenopausal women. Associations with visceral obesity and metabolic profile. Diabetes Care. 1999;22(11):1875–81.
Tchernof A, Després J-P. Sex steroid hormones, sex hormone-binding globulin, and obesity in men and women. Horm Metab Res. 2000;32(11/12):526–36.
Haffner SM, Valdez RA, Morales PA, Hazuda HP, Stern MP. Decreased sex hormone-binding globulin predicts noninsulin-dependent diabetes mellitus in women but not in men. J Clin Endocrinol Metabolism. 1993;77(1):56–60.
O’Reilly MW, Glisic M, Kumarendran B, et al. Serum testosterone, sex hormone-binding globulin and sex‐specific risk of incident type 2 diabetes in a retrospective primary care cohort. Clin Endocrinol. 2019;90(1):145–54.
Simons PI, Valkenburg O, van de Waarenburg MP et al. Serum sex hormone-binding globulin is a mediator of the association between intrahepatic lipid content and type 2 diabetes: the Maastricht Study. Diabetologia. 2022:1–10.
Lakshman KM, Bhasin S, Araujo AB. Sex hormone–binding globulin as an independent predictor of incident type 2 diabetes mellitus in men. Journals Gerontol Ser A: Biomedical Sci Med Sci. 2010;65(5):503–9.
Fortunati N, Catalano MG, Boccuzzi G, Frairia R. Sex hormone-binding globulin (SHBG), estradiol and breast cancer. Mol Cell Endocrinol. 2010;316(1):86–92.
Morisset A-S, Blouin K, Tchernof A. Impact of diet and adiposity on circulating levels of sex hormone-binding globulin and androgens. Nutr Rev. 2008;66(9):506–16.
Crave J-C, Fimbel S, Lejeune H, Cugnardey N, Dechaud H, Pugeat M. Effects of diet and metformin administration on sex hormone-binding globulin, androgens, and insulin in hirsute and obese women. J Clin Endocrinol Metabolism. 1995;80(7):2057–62.
Ropponen A, Aittomaki K, Vihma V, Tikkanen MJ, Ylikorkala O. Effects of oral and transdermal estradiol administration on levels of sex hormone-binding globulin in postmenopausal women with and without a history of intrahepatic cholestasis of pregnancy. J Clin Endocrinol Metabolism. 2005;90(6):3431–4.
Acknowledgements
We thank all participants for their long-term commitment to the KORA study, the staff for data collection and research data management and the members of the KORA Study Group (https://www.helmholtz-munich.de/en/epi/cohort/kora) who are responsible for the design and conduct of the study.
Funding
The KORA study was initiated and financed by the Helmholtz Zentrum München – German Research Center for Environmental Health, which is funded by the German Federal Ministry of Education and Research (BMBF) and by the State of Bavaria. Data collection in the KORA study is done in cooperation with the University Hospital of Augsburg. HR-D has received funding for his PhD studies by the Swiss National Science Foundation under the “Spirit grant” (SNSF IZSTZ0_190277). The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
HR-D, TM and JN contributed to the study design and conception. HR-D and MA performed the statistical analysis. HR-D wrote the first draft of the manuscript. All authors helped to interpret the data and critically revised the manuscript for important intellectual content. JN had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors have read and approved the final manuscript and the authorship list.
Corresponding authors
Ethics declarations
Ethical approval
All study participants have provided written informed consent. The study was approved by the Ethics Committees of the Bavarian Chamber of Physicians (Ethical Approval Number 06068) adhering to the declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Consent to publish is not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Raeisi-Dehkordi, H., Amiri, M., Rathmann, W. et al. Sex hormone-binding globulin may explain sex differences for glucose homeostasis and incidence of type 2 diabetes: the KORA study. Eur J Epidemiol (2024). https://doi.org/10.1007/s10654-024-01136-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10654-024-01136-2