Abstract
Background
Sex hormones are strongly linked to the occurrence and development of diabetes, and influence glycated hemoglobin (HbA1c) levels in diabetic population; but, the relationship between sex hormones and HbA1c in non-diabetic population remains unknown. This study aimed to explore the extent of influence of sex hormones on HbA1c levels in non-diabetic population.
Methods
A total of 1409 non–diabetic subjects, including 601 men and 808 postmenopausal women were recruited from Shanghai community. HbA1c was detected using high performance liquid chromatography, and hemoglobin level was determined by sodium lauryl sulfate colorimetry. Serum estradiol (E2), total testosterone (TT), and sex hormone binding globulin (SHBG) were measured by chemiluminescent microparticle immunoassays.
Results
The level of HbA1c was 5.6 (5.4–5.9) % in all subjects, with 5.6 (5.4–5.8) % in men and 5.7 (5.5–5.9) % in postmenopausal women. After adjusting for age, body mass index (BMI), and hemoglobin, E2 was positively correlated with HbA1c in men (r = 0.122, P = .003), and SHBG was inversely correlated with HbA1c (r = − 0.125, P < .001) in women. Other hormones were not correlated with HbA1c (all P > .05). Multivariate linear regression analysis showed that, except for traditional factors, such as age, hemoglobin, and BMI, E2 was another determinant of HbA1c (standardized β = 0.137, P = .003) in men; besides, in women, SHBG was another determinant of HbA1c (standardized β = − 0.178, P < .001), except for age and systolic blood pressure.
Conclusion
After controlling for confounding factors, two sex hormones, as E2 and SHBG could influence HbA1c levels in non-diabetic population.
Similar content being viewed by others
Introduction
Sex hormones, including estrogen, progesterone, and androgens, are synthesized by the human gonads and adrenal cortex. Their main role is to promote development of the reproductive system and maintain secondary sexual characteristics. More than that, low circulating levels of testosterone and sex-hormone-binding globulin (SHBG) were reported to be associated with increased cardiovascular risk in men, possibly due to effects on insulin resistance and glycemia. Recent studies have found that men with low serum testosterone levels had increased risk of diabetes; however, it was in contrast to that in women [1,2,3]. Additionally, lower serum total testosterone and sex hormone binding globulin levels were found in patients living with diabetes [4, 5].
HbA1c has long been regarded as the gold standard for evaluating long-term blood glucose control in patients living with diabetes in clinical routines. In recent years, standardized detection of HbA1c has been constantly improved, leading to sufficient sensitivity and specificity for HbA1c as an indicator of diabetes diagnosis [6,7,8]. But relatively few data are available on the relationship between sex hormones and this marker of long-term glycaemia. One study found that serum testosterone level was positively correlated with that of HbA1c in men with type 2 diabetes mellitus [9]. The association between low SHBG and HbA1c was also found in postmenopausal women; further, low total testosterone (TT) and SHBG were reported to be associated with HbA1c even below the threshold for diabetes in middle-aged and older men [10,11,12], which suggested that sex hormones might be markers of pathological processes resulting in elevated glucose levels among populations without diabetes. However, there is no evidence to delineate the relationship between the levels of sex hormones and HbA1c in a non-diabetic population. Thus, this study recruited non-diabetic subjects from Shanghai communities to explore whether the association of sex hormones with HbA1c levels is similar in a non-diabetic population to in a diabetic population.
Materials and methods
Study population
We recruited the subjects aged 40 years and over who volunteered to participate and were able to provide required information in Shanghai communities between October 2015 and July 2016. Patients living with diabetes were excluded according to prior medical diagnoses or receiving hypoglycemic therapy, or meeting the diagnostic criteria of the 2010 ADA, which states that diabetes is defined by fasting plasma glucose (FPG) ≥ 7.0 mmol/L and/or 2-h plasma glucose (2hPG) ≥ 11.1 mmol/L and/or HbA1c ≥ 6.5% [6]. Other exclusion criteria included a known history of cardiovascular and cerebrovascular diseases, malignant tumors, severe liver or kidney dysfunction, thyroid dysfunction, severe anemia, treatment with steroids or thyroxine or estrogen or androgen, using oral drugs to treat metabolic syndrome and hyperinsulinemia, cystic fibrosis, and nonmenopausal women. Menopause is defined as 12 consecutive months of amenorrhea without other medical behaviors [13]. This study was approved by the Ethics Committee of the Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University. All subjects signed an informed consent form before participation. All non-diabetic subjects received standardized questionnaires, including previous and present illness and treatment, physical examinations, and biochemical determinations.
Anthropometric and biochemical measurements
Height, weight and blood pressure were measured using the previously standardized method [14]. Body mass index (BMI) = weight (kg) / height (m2). Venous blood samples were collected after a 10 h overnight fast to detect fasting blood glucose (FPG), HbA1c, fasting insulin (FINS), blood lipids [total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-c), and low-density lipoprotein cholesterol (LDL-c)], and C-reactive protein (CRP). Additionally, all the non-diabetic subjects were tested for hemoglobin, and blood samples were collected after 75 g oral glucose tolerance test to determine the 2-h blood glucose (2hPG). All laboratory indicators were measured using the standard methods. The homeostasis model assessment of insulin resistance (HOMA-IR) was as follows: HOMA-IR = FINS (mU/L) × FPG (mmol/L)/22.5 [15].
HbA1c level was measured by high performance liquid chromatography (Variant II hemoglobin analyzer; Bio–Rad, Hercules, CA, USA), and hemoglobin level was measured by sodium lauryl sulfate colorimetry (Sysmex XE–2100 hematology analyzer, Sysmex Corporation, Kobe, Japan). The intra-assay and inter-assay coefficients of variation for HbA1c were < 2.60% and < 3.40%, respectively. Serum insulin levels were measured with an electrochemiluminescence immunoassay on a Cobas e411 analyzer (Roche Diagnostics GmbH, Mannheim, Germany) with intra- and interassay coefficients of variation of 1.7 and 2.5%, respectively. Serum estradiol (E2), TT, and SHBG were detected on Abbott Architect i2000SR analyzer by chemiluminescence microparticle immunoassay (kits from Abbott GmbH & Co. KG, Wiesbaden, Germany). Bioactive testosterone (BT) = N × [FT]; Kt = 1 × 109 L/mol, N = Ka × Ca + 1, where Ka = 3.6 × 104 L/mol; and Ca is Alb level. The sensitivity of E2, TT, and SHBG estimation was < 2.5 pg/mL, < 0.1 ng/mL, and < 0.3 mmol/L, respectively. The intra-assay and inter-assay coefficients of variation for E2 were < 2.40% and < 2.70%, respectively; the intra-assay and inter-assay coefficients of variation for TT were < 2.16% and < 2.23%, respectively. The intra-assay and inter-assay coefficients of variation for SHBG were < 2.80% and < 4.30%, respectively.
Statistical analyses
The research data was analyzed using SPSS, version 20.0 (SPSS Inc., Chicago, IL, USA). All variables were tested for normality. Normally distributed variables are presented as mean ± standard deviation, and non–normally distributed variables are presented as median and interquartile range. Student’s t-test was used to compare two groups with normal distribution, whereas Wilcoxon rank sum test was used for skewed distribution between two groups. Partial correlation analysis was conducted to analyze the potential correlation between the levels of HbA1c and sex hormones. A multivariate linear regression was performed to examine this correlation in men and women, respectively. All P values were two-tailed, and P < .05 was considered statistically significant.
Results
Clinical characteristics of study subjects
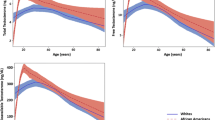
A total of 1409 cases with an average age of 60.4 ± 6.2 years were enrolled in this study, including 601 men, and 808 postmenopausal women with a median menopause duration of 10 (6–15) years. HbA1c level was 5.6 (5.4–5.9) % in all the subjects, with 5.6 (5.4–5.8) % in men and 5.7 (5.5–5.9) % in postmenopausal women. Men had a median E2 level of 99.1 (84.4–121.1) pmol/L, median TT of 20.12 (15.5–24.9) nmol/L, median BT of 12.5 (10.0–15.9) nmol/L, and median SHBG of 40.7 (30.4–52.8) nmol/L. Postmenopausal women had a median E2 level of 36.7 (18.4–47.7) pmol/L, median TT of 0.9 (0.8–1.2) nmol/L, median BT of is 0.3 (0.2–0.3) nmol/L, and median SHBG of 53.7 (38.8–72.8) nmol/L (Table 1). Levels of E2, TT, and BT were significantly higher while those of SHBG were lower in men than in women (all P < .001) (Fig. 1). Additionally, the levels of BMI, SBP, DBP, and TG were higher in men than in women (all P < .05); whereas, women tended to have higher HbA1c, HOMA-IR, TC, HDL-c, and LDL-c levels than that in men (all P < .05).
Associations between sex hormone levels and HbA1c
Figure 2 showed the correlation of E2 with HbA1c in men and SHBG with HbA1c in women. Partial correlation analysis after adjusting for age, BMI, and hemoglobin levels showed that only E2 was positively correlated with HbA1c in men (r = 0.122, P = .003); BT was marginally correlated with HbA1c (r = 0.080, P = .05). TT and SHBG were not correlated to HbA1c (P = .238; P = .318). In women, only SHBG was negatively correlated with HbA1c (r = − 0.125, P < .001), while other hormones were not correlated with HbA1c (all P > .05) (Table 2).
Analysis of sex hormones affecting HbA1c
A multivariate linear regression model was constructed with data from men and postmenopausal women to analyze the association of sex hormones with HbA1c. In men, age, BMI, SBP, DBP, FPG, 2hPG, HOMA-IR, TC, TG, HDL-c, LDL-c, CRP, hemoglobin, and E2 were independent variables, and HbA1c was the dependent variable. We found that except for hemoglobin and BMI, E2 was a positive factor for HbA1c (standardized β = 0.137, P = .003) (Table 3). Further, in postmenopausal women, age, BMI, SBP, DBP, FPG, 2hPG, HOMA-IR, TC, TG, HDL-c, LDL-c, CRP, hemoglobin, and SHBG were independent variables, and HbA1c was the dependent variable. Except for age and SBP, SHBG was a negative factor for HbA1c (standardized β = − 0.178, P < .001).
Discussion
To our knowledge, the present study was the first to assess the association between a relatively complete set of sex hormones and HbA1c, and was conducted in both men and postmenopausal women. We found that E2 was a positive factor for HbA1c in men while SHBG was a negative factor for HbA1c in postmenopausal women.
At a cellular level, testosterone increases the expression of insulin receptor β subunit, insulin receptor substrate-1, protein kinase B and glucose transporter type 4 in adipose tissue and adenosine 5′-monophosphate-activated protein kinase expression and activity in skeletal muscle [16, 17]. Hence, it was reported that testosterone enhances insulin sensitivity in obese men with hypogonadism by decreasing fat mass, increasing lean mass, decreasing free fatty acids and suppressing inflammation [18]. In addition, androgen therapy increases hemoglobin concentration and stimulates erythropoiesis [19]. Some studies suggest that low BT can compromise erythropoiesis, thus causing anemia, and may be an under-recognized anemia-related factor. Therefore, low BT may lead to a decrease in hemoglobin and HbA1c levels [20].
Previous studies showed that serum BT was positively correlated with HbA1c in men with type 2 diabetes [10], but this population had been treated with hypoglycemic drugs. One study also found that obese men with type 2 diabetes had lower testosterone levels than those with normal glucose tolerance [21]. Here, we selected the non-diabetic population to investigate whether sex hormones, including BT, were associated with HbA1c levels in these individuals. We found that serum BT and HbA1c were marginally correlated in men; while after adjusting for other factors, BT was correlated with other sex hormones, but no correlation was found between BT and HbA1c. Additionally, we found that E2 was positively correlated with HbA1c in men. Mean age of men included in this study was 60.3 years old. Moreover, testosterone levels gradually decrease with age [19], while the activity of aromatase increases, which activates the conversion of testosterone to estradiol [22, 23]. Thus, the above results may be related to the ability of aromatase to convert testosterone into estradiol.
We also found that SHBG was negatively correlated with HbA1c in postmenopausal women. Previous study showed a significantly negative correlation between SHBG and HbA1c in non-diabetic postmenopausal women (n = 200) after adjusting for age and BMI [3]. In this study, data of a large number of postmenopausal women was further adjusted for other metabolic factors. SHBG is synthesized and secreted by the liver cells to primarily combine with sex hormones and regulate their physiological effects [24]. Testosterone stimulates erythropoiesis, and while its levels are significantly reduced in postmenopausal women, the change in SHBG is not obvious [25]. The affinity of SHBG for androgens is much greater than that for estrogen, and while circulating, SHBG concentration is easily affected by the activity of peripheral androgens. It is regarded as one of the biological effects of androgens [26]. This may explain why SHBG is related to HbA1c. Additionally, we found that hemoglobin was a negative factor, while BMI was a positive factor for HbA1c in men. Age was a positive factor for HbA1c, in both men and postmenopausal women, consistent with results of previous studies [27, 28].
This study has some limitations. First, the study population only included middle-aged and elderly individuals, and hence, the results may not be generalized to entire community. Second, the cross–sectional study design could not determine the causal relationship between changes in sex hormone and HbA1c levels. Therefore, prospective studies with a larger sample size and different age groups are needed to validate these findings.
In summary, sex hormones influence HbA1c levels in non-diabetic population. Moreover, levels of E2 were independently and positively correlated with HbA1c in men, and those of SHBG were independently and inversely correlated with HbA1c in postmenopausal women.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
References
Karakas M, Schäfer S, Appelbaum S, et al. Testosterone levels and type 2 diabetes-no correlation with age, differential predictive value in men and women. Biomolecules. 2018;8(3):76.
Ramachandran S, Hackett GI, Strange RC. Sex hormone binding globulin: a review of its interactions with testosterone and age, and its impact on mortality in men with type 2 diabetes. Sex Med Rev. 2019;7(7):669–78.
Ding EL, Song Y, Manson JE, et al. Plasma sex steroid hormones and risk of developing type 2 diabetes in women: a prospective study. Diabetologia. 2007;50(10):2076–84.
Arthur R, Rohrmann S, Møller H, et al. Pre-diabetes and serum sex steroid hormones among US men. Andrology. 2017;5(1):49–57.
Hu J, Zhang A, Yang S, et al. Combined effects of sex hormone-binding globulin and sex hormones on risk of incident type 2 diabetes. J Diabetes. 2016;8(4):508–15.
American Diabetes A. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl 11):S11–61.
World Health Orgnization. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. In: Abbreviated report of a WHO consultation; 2011. EB/OL. 2011-01-13 http://who.int/diabetes/publications/report-hbalc-2011.Pdf.
Bao Y, Ma X, Li H, et al. Glycated haemoglobin A1c for diagnosing diabetes in Chinese population: cross sectional epidemiological survey. BMJ. 2010;340:c2249.
Fukui M, Tanaka M, Hasegawa G, Yoshikawa T, et al. Association between serum bioavailable testosterone concentration and the ratio of glycated albumin to glycated hemoglobin in men with type 2 diabetes. Diabetes Care. 2008;31(3):397–401.
Zhu H, Wang N, Han B, et al. Low sex hormone-binding globulin levels associate with prediabetes in Chinese men independent of Total testosterone. Plos One. 2016;11(5):e0162004.
Brand JS, Wareham NJ, Dowsett M, et al. Associations of endogenous testosterone and SHBG with glycated haemoglobin in middle-aged and older men. Clin Endocrinol. 2011;74(10):572–8.
Page-Wilson G, Goulart AC, Rexrode KM. Interrelation between sex hormones and plasma sex hormone-binding globulin and hemoglobin A1c in healthy postmenopausal women. Metab Syndr Relat Disord. 2009;7(3):249–54.
Burger HG. The menopause: when it is all over or is it? Aust N Z J Obstet Gynaecol. 1994;34(3):293–5.
Xu Y, Ma X, Shen Y, et al. Influence of sex hormones on the relationship between body fat and glycated albumin levels. J Sex Med. 2020;17(5):903–10.
Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Ghanim H, Dhindsa S, Batra M, et al. Testosterone increases the expression and phosphorylation of AMP kinase α in men with hypogonadism and type 2 diabetes. J Clin Endocrinol Metab. 2020;105(4):1169–75.
Day EA, Ford RJ, Steinberg GR. AMPK as a therapeutic target for treating metabolic diseases. Trends Endocrinol Metab. 2017;28(8):545–60.
Dandona P, Dhindsa S, Ghanim H, et al. Mechanisms underlying the metabolic actions of testosterone in humans: a narrative review. Diabetes Obes Metab. 2021;23(1):18–28.
Roy CN, Snyder PJ, Stephens-Shields AJ, et al. Association of Testosterone Levels with Anemia in older men: a controlled clinical trial. JAMA Intern Med. 2017;177(4):480–90.
Solomon LR, Hendler ED. Androgen therapy in haemodialysis patients. II Effects on red cell metabolism. Br J Haematol. 1987;65:223–30.
Souteiro P, Belo S, Oliveira SC, et al. Insulin resistance and sex hormone-binding globulin are independently correlated with low free testosterone levels in obese males. Andrologia. 2018;50(7):e13035.
Harman SM, Metter EJ, Tobin JD, et al. Baltimore longitudinal study of aging. Longitudinal effects of aging on serum total and free testosterone levels in healthy men Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab. 2001;86:724–31.
Vermeulen A, Kaufman JM, Goemaere S, et al. Estradiol in elderly men. Aging Male. 2002;5(2):98–102.
Cumming DC, Cumming DC WSR, Wall SR. Non-sex hormone-binding globulin-bound testosterone as a marker for hyperandrogenism. J Clin Endocrinol Metab. 1985;61(5):873–6.
Hammond GL. Diverse roles for sex hormone-binding globulin in reproduction. Biol Reprod. 2011;85:431–41.
Schneider G, Kirschner MA, Berkowitz R, Ertel NH. Increased estrogen production in obese men. J Clin Endocrinol Metab. 1979;48:633–8.
Wang D, Wang Y, Madhu S, et al. Total hemoglobin count has significant impact on A1C - Data from National Health and nutrition examination survey 1999-2014. Prim Care Diabetes. 2019;13(4):316–23.
Nagarathna R, Kaur N, Anand A, et al. Distribution of glycated haemoglobin and its determinants in Indian young adults. Diabetes Res Clin Pract. 2020;159:107982.
Acknowledgements
Not applicable.
Funding
This work was funded by the National Key R&D Program of China (2016YFA0502003).
Author information
Authors and Affiliations
Contributions
XJM and YQB conceived the work. YTX performed the statistical analyses. YTX, YS, JLT, YFX, and XJM contributed to data collection. YTX and WJC contributed to drafting the article. XJM and YQB revised the manuscript. All authors gave final approval for the published version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the World Medical Association Declaration of Helsinki and approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. All subjects signed an informed consent form before participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, Y., Cao, W., Shen, Y. et al. The relationship between sex hormones and glycated hemoglobin in a non-diabetic middle-aged and elderly population. BMC Endocr Disord 22, 91 (2022). https://doi.org/10.1186/s12902-022-01002-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01002-w