Abstract
Air pollution and multimorbidity are two of the most important challenges for Public Health worldwide. Although there is a large body of evidence linking air pollution with the development of different single chronic conditions, the evidence about the relationship between air pollution and multimorbidity (the co-occurrence of multiple long-term conditions) is sparse. To obtain evidence about this relationship could be challenging and different aspects should be considered, such as its multifaceted and complex nature, the specific pollutants and their potential influence on health, their levels of exposure over time, or the data that could be used for its study. This evidence could be instrumental to inform the development of new recommendations and measures to reduce harmful levels of air pollutants, as means to prevent the development of multimorbidity and reduce its burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the World Health Organization (WHO) and the Organisation for Economic Co-operation and Development (OECD) [1, 2], the joint effects of indoor and ambient air pollution air pollution are the main environmental cause of premature death, contributing between 4 and 9 million premature deaths per year [3], and with an associated economic cost of 1.575 trillion US dollars [2]. In addition, the exposure to air pollution in form of particulate matter (PM) of different sizes (e.g., with an average diameter of 10 µm or less—PM10, or with an average diameter of 2.5 µm or less PM2.5), or in form of gases (e.g., nitrogen dioxide—NO2, or Sulphur dioxide—SO2), has been directly related to a substantial decrease in the quality of life and to a substantial increase in the burden of multiple acute and chronic diseases [1, 4]. Following the recent WHO revision of the annual PM2.5 guideline value to 5 µg (one-millionth of a gram) per cubic meter air [5], it is estimated that over 99% of the world population is exposed to unhealthy levels of pollutants, further reinforcing air pollution as one of the main public health priorities worldwide.
Although different studies point out the relationship between the exposure to air pollution and the development of different single chronic conditions [6,7,8,9,10,11,12,13], the evidence about the relationship between air pollution and multimorbidity (the co-existence of two or more long-term health conditions) is very limited [14,15,16,17]. However, the nature of this relationship is complex and different peculiarities must be considered cautiously for its study, such as the potential mechanisms and pathways underlying it, the possible differential effects over time of the exposure to different pollutants and different levels of them, and their influence on the development of different multimorbidity clusters.
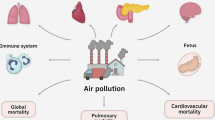
Impact of air pollution on health conditions
Considering the large body of evidence linking air pollution with single conditions (e.g., cardiorespiratory, or neurological disorders) [6], it is reasonable to expect that the exposure to unhealthy levels of air pollution could also be related to their accumulation, leading to multimorbidity [18]. While there is considerable heterogeneity in the way multimorbidity has been defined in research [18, 19], all the definitions agree that multimorbidity is considered to be the co-occurrence of two or more long-term communicable and/or non-communicable diseases (or at least health problems) in an individual [14, 18]. Additionally, although multimorbidity has been linked systematically to different factors, such as biological (e.g., ageing and inflammation) [20], lifestyle (e.g., physical inactivity) [21], and psychosocial determinants (e.g., socioeconomic status) [22], there is sparse evidence for the potential role of air pollution in its development. Furthermore, air pollution could play a relevant role on the development and evolution of syndemics related to multimorbidity i.e., on the potential synergistic effect of the multimorbidity epidemic with other epidemics such as COVID-19. Therefore, the contribution of air pollution to the accumulation of different health conditions could translate into significant additional health, societal and economic burdens, currently not represented in the WHO and OECD assessments [1, 2].
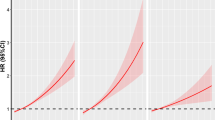
The impact of air pollution on health conditions is likely to vary over time. While the short-term exposure to air pollution has been associated with the development of mainly, albeit not exclusively acute pathologies [23], the larger burden of health effects is attributable to longer-term, potentially lifetime exposures [24]. Exposure to pollutants could both increase the incidence and the severity of multiple long-term conditions (e.g., through the development of chronic inflammatory profiles [17], aberrant tissue remodelling, accelerated ageing and senescence) [25], making it necessary to carry out studies with long follow-up periods to determine the nature of this relationship over time. Additionally, the effects of air pollution on health could vary over the life course, necessitating the study and identification of both age groups in which the exposure could have more detrimental effects on health [26], and of sensitive periods in which the exposure to pollutants might have a greater adverse impact on health, such as during early immune and organ development [27].
Dealing with complexity
It should be noted that the biological pathways underlying the relationship between the exposure to toxic air pollutants and the development of different types of multimorbidity needs further research [21, 28]. Since specific air pollutants are differentially related to the development of chronic health conditions [6], a wide range of air pollutants (such as NO2, SO2 and PM) and their pathways for the development of health problems must be considered over time. As highlighted by previous studies [29, 30], exposure to air pollutants in certain combinations could have different effects on the development of co-existing disorders and it remains unclear how they could impact multimorbidity via potential pathways, such as metabolic and neuroendocrine alterations, or systemic inflammation and oxidative stress [6, 25]. Furthermore, air pollutants are often co-occurring and collinear with each other and other socio-economic and environmental exposures, making it difficult to disentangle specific effects because they are intrinsically intertwined in a complex, dynamic network. To address the challenge of causality and collinearity, the exposome paradigm provides a framework that may advance the study of environment with the integration of omic markers in multimorbidity related epidemiological studies [31].
Due to the multifaceted and complex nature of the relationship between air pollution and multimorbidity, obtaining data to study it could be challenging. A suitable and promising option to study this relationship over time is the use of real-world data with existing or novel linkages with air pollution metrics [32]. Different types of real-world data from all over the world could be used to study this relationship, such as data population-based birth cohort studies, such as the National Survey of Health and Development (NSHD) in the UK [33], and the Danish National Birth Cohort (DNBC) in Denmark [34], or data from large-scale biomedical databases containing in-depth genetic and health information such as the UK Biobank in the UK [35], the “All of Us” Research Program in the US [36], or the Biobank for health research (Lifelines) in the Netherlands [37]. Furthermore, another promising option to be used for the study of the impact of air pollution on multimorbidity, are clinical data from electronic health records, such as the Clinical Practice Research Datalink (CPRD) [38].
Despite the opportunity offered by real-world data, it is worth mentioning that these data also have limitations [32]. In some cases, these data include a limited number of records or participants, and/or do not include variables potentially relevant to account for the complex relationship between air pollution and multimorbidity, as for example health records with a clinical focus in which could be limited the availability of non-clinical variables (e.g., sociodemographic, or environmental factors). Additionally, collecting relevant data about multi-morbidity and air pollution could be challenging in surveys or cohort studies. To account for them, these types of studies need to include data about a wide spectrum of physical and mental disorders, and about the exposure to air pollution over time (ideally on a continuous basis), or at least, proxy measures from which could be possible determine this exposure, such as the postcode of participants and possible changes on it [39]. To overcome these limitations and challenges, one possible solution is the use of pooled and/or linked real-world data from different sources. Different examples of real-world data pooling and linkage could be the European Study of Cohorts for Air Pollution Effects project (ESCAPE) that uses pooled data from more than 30 cohort studies with different variables of interest about the exposure to air pollution (determined using the postcode of cohort members), and about long-term conditions[39, 40], or a recent study aimed to study the influence of the exposure to air pollution on the development of different patterns of chronic diseases, that uses linked data from the UK Biobank and the Hospital Episodes Statistics database [16]. Therefore, data pooling and linkage could be a useful resource to enhance the richness, robustness and power of the data collected in individual studies to detect relevant relationships between air pollution and multimorbidity over the life course.
Implications and conclusions
Mechanisms and challenges aside, if air pollution exposure affects multimorbidity risk, it presents an unusual opportunity for multimorbidity prevention: the possibility of integrating environmental policy and regulation into patient and healthcare policies aimed at addressing the multimorbidity epidemic [9, 10, 41,42,43,44]. This environmental perspective and population-wide approach could complement the individual perspective used in clinical settings [45], such as for the management of chronic diseases Furthermore, obtain evidence about the influence of air pollution on the development of multimorbidity, could be also helpful to determine the risk attributable to the exposure to different pollutants, and to identify high risk population groups. This evidence could be instrumental to inform the development of new environmental recommendations and preventive measures to reduce harmful levels of air pollutants, and to improve the outcomes of prevention strategies currently in use. Hence, obtain this evidence could suppose a step forward for cutting down substantial costs for healthcare systems, and for the prevention of the development of multiple co-occurring conditions [28].
Tackling multimorbidity represents one of the greatest challenges for health systems worldwide, and a deeper and more comprehensive understanding of its determinants is urgently needed. Therefore, given the lack of evidence, the study of the long-term influence of air pollution on the accumulation of chronic diseases would be key to inform preventive measures and, ultimately, reduce the burden of multimorbidity.
References
World Health Organization. Burden of disease from the joint effects of household and ambient Air pollution for 2016. Summary of results. World Health Organization. 2018;2.
OECD. The Cost of Air Pollution. OECD; 2014.
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020 Oct 17;396(10258):1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2
Burnett RT, Pope CA 3rd, Ezzati M, Olives C, et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ Health Perspect. 2014 Apr;122(4):397-403. https://doi.org/10.1289/ehp.1307049. Epub 2014 Feb 11. Erratum in: Environ Health Perspect. 2014 Sep;122(9):A235.
World Health Organization. WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Regional Office for Europe. 2021. https://apps.who.int/iris/handle/10665/345334.
Kampa M, Castanas E. Human health effects of air pollution. Environ Pollut. 2008;151:362–7.
Schikowski T, Mills IC, Anderson HR, Cohen A, Hansell A, Kauffmann F, et al. Ambient air pollution: a cause of COPD. Eur Respir J. 2014;43(1):250–63. https://doi.org/10.1183/09031936.00100112
Block ML, Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32:506.
Manisalidis I, Stavropoulou E, Stavropoulos A, Bezirtzoglou E. Environmental and health impacts of air pollution: a review. Front Public Health. Front Med SA. 2020;8:14.
Landrigan PJ. Air pollution and health. Lancet Public Health [Internet]. Elsevier; 2017 [cited 2021 Dec 8];2:e4–5. http://www.thelancet.com/article/S2468266716300238/fulltext
Newbury JB, Stewart R, Fisher HL, Beevers S, Dajnak D, Broadbent M, et al. Association between air pollution exposure and mental health service use among individuals with first presentations of psychotic and mood disorders: retrospective cohort study. Br J Psychiatry. 2021;219(6):678–85. https://doi.org/10.1192/bjp.2021.119.
Bakolis I, Hammoud R, Stewart R, Beevers S, Dajnak D, MacCrimmon S, et al. Mental health consequences of urban air pollution: prospective population-based longitudinal survey. Soc Psychiatry Psychiatr Epidemiol. 2021;56(9):1587–99. https://doi.org/10.1007/s00127-020-01966-x.
COMEAP report (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1090376/COMEAP-dementia-report-2022.pdf).
Johnston MC, Crilly M, Black C, Prescott GJ, Mercer SW. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health. 2019;29(1):182–9. https://doi.org/10.1093/eurpub/cky098
Hu K, Keenan K, Hale JM, Liu Y, Kulu H. A longitudinal analysis of PM2.5 exposure and multimorbidity clusters and accumulation among adults aged 45–85 in China. PLOS Glob Public Health. 2022;2:e0000520.
Ronaldson A, Arias de la Torre J, Ashworth M, Hansell AL, Hotopf M, Mudway I, et al. Associations between air pollution and multimorbidity in the UK Biobank: a cross-sectional study. Front Public Health. 2022;10:1035415. https://doi.org/10.3389/fpubh.2022.1035415.
Autenrieth C, Hampel R, Wolf K, Cyrys J, Döring A, Pershagen G, et al. Long-term exposure to air pollution and risk of systemic inflammation-induced multimorbidity among the elderly: results from the population-based kora-age study. Circulation. 2013;2013:127.
Ho IS-S, Azcoaga-Lorenzo A, Akbari A, Black C, Davies J, Hodgins P, et al. Examining variation in the measurement of multimorbidity in research: a systematic review of 566 studies. Lancet Public Health. 2021;6:e587–97.
Ronaldson A, Arias de la Torre J, Prina M, Armstrong D, Das-Munshi J, Hatch S, et al. Associations between physical multimorbidity patterns and common mental health disorders in middle-aged adults: a prospective analysis using data from the UK Biobank. The Lancet Regional Health Europe. 2021;8.
Arias-de la Torre J, Ronaldson A, Prina M, Matcham F, Hatch SL, Pickles A, et al. Depressive symptoms during early adulthood and the development of physical multimorbidity in the UK: an observational cohort study. Lancet Healthy Longev. 2021;2:801–10.
The Academy of Medical Sciences. Multimorbidity: a priority for global health research. https://acmedsci.ac.uk/policy/policy-projects/multiple-morbidities-as-a-global-health-challenge. 2015.
Sinnott C, Mc Hugh S, Fitzgerald AP, Bradley CP, Kearney PM. Psychosocial complexity in multimorbidity: the legacy of adverse childhood experiences. Fam Pract. 2015;32(3):269–75. https://doi.org/10.1093/fampra/cmv016.
Wei Y, Wang Y, Di Q, Choirat C, Wang Y, Koutrakis P, et al. Short term exposure to fine particulate matter and hospital admission risks and costs in the medicare population: time stratified, case crossover study. BMJ. 2019;2019:367.
Strak M, Weinmayr G, Rodopoulou S, Chen J, de Hoogh K, Andersen ZJ, et al. Long term exposure to low level air pollution and mortality in eight European cohorts within the ELAPSE project: pooled analysis. BMJ. 2021;374:n1904. https://doi.org/10.1136/bmj.n1904
Chuang KJ, Chan CC, Su TC, Lee CT, Tang CS. The effect of urban air pollution on inflammation, oxidative stress, coagulation, and autonomic dysfunction in young adults. Am J Respir Crit Care Med. 2012;176:370–6. https://doi.org/10.1164/rccm200611-1627OC.
Russ TC, Cherrie MPC, Dibben C, Tomlinson S, Reis S, Dragosits U, et al. Life course air pollution exposure and cognitive decline: modelled historical air pollution data and the Lothian birth cohort 1936 the Creative Commons Attribution-NonCommercial License (CC BY-NC 4.0). J Alzheimer’s Dis. 2021;79:1063–74.
Herr CE, Dostal M, Ghosh R, Ashwood P, Lipsett M, Pinkerton KE, et al. Air pollution exposure during critical time periods in gestation and alterations in cord blood lymphocyte distribution: a cohort of livebirths. Environ Health. 2010;9:46. https://doi.org/10.1186/1476-069X-9-46.
Whitty CJM, MacEwen C, Goddard A, Alderson D, Marshall M, Calderwood C, et al. Rising to the challenge of multimorbidity. BMJ. 2020;368:l6964.
Urman R, McConnell R, Islam T, Avol EL, Lurmann FW, Vora H, et al. Associations of children’s lung function with ambient air pollution: joint effects of regional and near-roadway pollutants. Thorax. 2014;69(6):540-7. https://doi.org/10.1136/thoraxjnl-2012-203159.
Wang M, Zhou T, Song Y, Li X, Ma H, Hu Y, et al. Joint exposure to various ambient air pollutants and incident heart failure: a prospective analysis in UK Biobank. Eur Heart J. 2021;2021:42.
Vineis P, Robinson O, Chadeau-Hyam M, Dehghan A, Mudway I, Dagnino S. What is new in the exposome? Environ Int. 2020;143:105887. https://doi.org/10.1016/j.envint.2020.105887.
Arias de la Torre J, Ronaldson A, Valderas JM, Vilagut G, Serrano-Blanco A, Hatch SL, et al. Diagnostic promiscuity: the use of real-world data to study multimorbidity in mental health. Br J Psychiatry. 2021;218:237–9.
Wadsworth M, Kuh D, Richards M, Hardy R. Cohort profile: The 1946 National Birth Cohort (MRC National Survey of Health and Development). Int J Epidemiol. 2006;35(1):49–54. https://doi.org/10.1093/ije/dyi201.
Ernst A, Brix N, Lauridsen LLB, Strandberg-Larsen K, Bech BH, Nohr EA, et al. Cohort profile: the puberty cohort in the Danish National Birth Cohort (DNBC). Int J Epidemiol. 2020;49(2):373-374g. https://doi.org/10.1093/ije/dyz222.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
The “All of Us” Research Program. N Engl J Med. 2019.
Sijtsma A, Rienks J, van der Harst P, Navis G, Rosmalen JGM, Dotinga A. Cohort profile update: lifelines, a three-generation cohort study and biobank. Int J Epidemiol. 2022;51(5):e295–e302. https://doi.org/10.1093/ije/dyab257.
Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, Staa T van, et al. Data resource profile: clinical practice research datalink (CPRD). Int J Epidemiol. 2015;44(3):827–36. https://doi.org/10.1093/ije/dyv098.
Beelen R, Raaschou-Nielsen O, Stafoggia M, Andersen ZJ, Weinmayr G, Hoffmann B, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet. 2014;383(9919):785–95. https://doi.org/10.1016/S0140-6736(13)62158-3.
Cyrys J, Eeftens M, Heinrich J, Ampe C, Armengaud A, Beelen R, et al. Variation of NO2 and NOx concentrations between and within 36 European study areas: results from the ESCAPE study. Atmos Environ. 2012;62:374–90. https://doi.org/10.1016/j.atmosenv.2012.07.080
Tainio M, Jovanovic Andersen Z, Nieuwenhuijsen MJ, Hu L, de Nazelle A, An R, et al. Air pollution, physical activity and health: a mapping review of the evidence. Environ Int. 2021.
Duque L, Relvas H, Silveira C, Ferreira J, Monteiro A, Gama C, et al. Evaluating strategies to reduce urban air pollution. Atmos Environ. 2016;127:196–204.
Seaton A, MacNee W, Donaldson K, Godden D. Particulate air pollution and acute health effects. Lancet. 1995;345(8943):176–8. https://doi.org/10.1016/s0140-6736(95)90173-6.
Loxham M, Davies DE, Holgate ST. The health effects of fine particulate air pollution. BMJ 2019;27(367):l6609. https://doi.org/10.1136/bmj.l6609.
Bergeson SC, Dean JD. A systems approach to patient-centered care. JAMA. 2006;296:2848–51.
Acknowledgements
This article represents independent research part funded also by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Funding
The present work is partially funded by the Medical Research Council (Grant No. MR/S028188/1) and by CIBER Epidemiology and Public Health (CIBERESP). IM was part funded by the National Institute for Health Research Health Protection Research Units (NIHR HPRU) in Environmental Exposures and Health and Chemical and Radiation Threats and Hazards at Imperial College in partnership with the UK Health Security Agency (UKHSA). IB is supported by the NIHR Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and by the National Institute of Health and Care Research (NIHR) Applied Research Collaboration (ARC) at King’s College Hospital NHS Foundation Trust, London.
Author information
Authors and Affiliations
Contributions
JAT, AR and IB drafted the first version of the manuscript. JAT and AR share the first authorship. All authors contributed to subsequent writing, revisions and agreed the final version submitted.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arias de la Torre, J., Ronaldson, A., Alonso, J. et al. The relationship between air pollution and multimorbidity: Can two birds be killed with the same stone?. Eur J Epidemiol 38, 349–353 (2023). https://doi.org/10.1007/s10654-022-00955-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-022-00955-5