Abstract
Axicabtagene ciloleucel (axi-cel) and tisagenlecleucel (tisa-cel) are chimeric antigen receptor (CAR) T-cell therapies used to treat adult patients with relapsed or refractory follicular lymphoma (rrFL) after two or more lines of systemic therapy. In the absence of head-to-head clinical trials, this study aimed to compare the efficacy, safety, and cost of axi-cel and tisa-cel in the treatment of rrFL after at least two lines of treatment. Overall response rate (ORR) and safety signals were compared using reporting odds ratios (RORs) with 95% confidence intervals (CIs) at p < 0.05. Progression-free survival (PFS), duration of response (DoR), and overall survival (OS) were compared using the Kaplan?Meier method with a log-rank test. Cost and cost-minimization analyses of drug acquisition, drug administration, serious adverse events (AEs), and relapsed management were calculated. Costs were extracted from the IBM-Micromedex Red Book, Centers for Medicare and Medicaid Services, and existing literature. Statistical analyses were conducted using Microsoft Excel and R version 4.0.5. No statistically significant differences were observed between axi-cel and tisa-cel in terms of ORR, DoR, and OS (p > 0.05). PFS was significantly better with tisa-cel (p < 0.05). Axi-cel was significantly associated with higher incidences of CRS, neurologic events, and grade 3–4 AEs than tisa-cel (ROR > 1, p < 0.05). Axi-cel and tisa-cel cost $512,021 and $450,885 per patient, respectively, resulting in savings of US$61,136 with tisa-cel over axi-cel. Tisa-cel appears to have a better safety profile, fewer serious AEs, lower mortality rate, and lower cost than axi-cel.
Key points
Axicabtagene ciloleucel (axi-cel) and tisagenlecleucel (tisa-cel) are recently approved gene therapies for treatment of adult patients with relapsed or refractory follicular lymphoma after two or more lines of treatment. To date, no data were available to understand the differences in their efficacy, safety, and financial impact.
This study compared the two treatments based on pivotal clinical trials.
The results indicated that tisa-cel is a superior treatment over axi-cel, with better efficacy, fewer serious adverse events, and less economic burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Follicular lymphoma (FL) is the second most common lymphoma diagnosed in the United States (US) and Western Europe, accounting for approximately 35% of all non-Hodgkin lymphomas (NHLs) [1,2,3]. FL is the most common form of indolent lymphoma, with an estimated incidence rate of 6 new cases per 100,000 persons per year in the US [2, 4]. FL is most frequently diagnosed among people aged 55–64 years and rarely occurs in patients aged under 18 years [4, 5].
Patients with FL respond well to the available chemotherapeutic regimens, with survival rates of 15–18 years [6]. Nevertheless, FL is considered incurable, with approximately 20% of patients experiencing relapse or becoming refractory within 2 years of first-line therapy [7, 8]. Relapsed or refractory FL (rrFL) can be managed with rituximab or second-generation anti-CD20 antibodies, either as a single agent or in combination with chemotherapy, anti-CD20 maintenance therapy, and stem cell transplant [9]. However, successive treatment courses have shown decreased efficacy and durations of remission in most patients with FL [10, 11].
Axicabtagene ciloleucel (axi-cel) and tisagenlecleucel (tisa-cel) are autologous anti-CD19 chimeric antigen receptor (CAR) T-cell therapies, which were recently approved in the US for treatment of adult patients with rrFL after two or more lines of systemic therapy [12, 13]. Pivotal clinical trials—ZUMA-5 for axi-cel and ELARA for tisa-cel—showed high rates of durable responses with relatively manageable safety profiles in extensively pretreated rrFL, including in high-risk patients [14, 15]. ZUMA-5 (axi-cel) was a single-arm, multicenter, phase 2 trial with a median follow-up period of 17.5 months (interquartile range [IQR] 14.1–22.6). Overall response rate (ORR) was observed in 94% of the patients, with 79% having a complete response (CR). The most common grade 3 or worse adverse events (AEs) were neutropenia (61%), anemia (23%), and thrombocytopenia (23%). Grade 3 or higher cytokine release syndrome (CRS) occurred in 7% of the patients, and grade 3 or higher neurological events occurred in 15% of the patients [14]. ELARA (tisa-cel) was a multinational, phase 2 trial with a median follow-up period of 16.6 months (IQR 13.8–20.2). ORR was observed in 89% of the patients, and 74% had CR. Neutropenia (32%), anemia (13%), and decreased white blood cell count (12%) were the most common grade 3 or higher AEs. Grade 3 or higher CRS was not reported, and grade 3 or higher neurological events occurred in 3% of the patients [15]. CAR T-cell therapies are costly. Moreover, the long complicated administrative procedure, serious AEs, and relapse management lead to cost increases. Therefore, mean total healthcare expenditures between CAR T-cell therapies [16, 17].
Likewise, the efficacy, safety, and cost of CAR T-cell therapies vary. Currently, no head-to-head clinical trials have compared these therapies. Thus, this study aimed to compare axi-cel and tisa-cel in terms of efficacy, safety, and treatment cost for adult patients with rrFL after two or more lines of systemic therapy during the first 18–21 months of adoption.
Methods
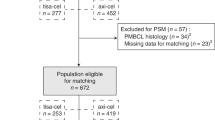
The analysis method was based on the pivotal clinical trials of axi-cel (NCT03105336) and tisa-cel (NCT03568461) for adults (≥ 18 years old) with FL, including grade 1–3a FL relapsed or refractory disease after two or more previous lines of therapy. Efficacy, safety, cost, and patient characteristics were compared between these interventions during the first 2 years of treatment.
Efficacy
Primary and secondary efficacy endpoints were assessed in this analysis. Primary endpoints included ORR, which involved either CR or partial response (PR), stable disease (SD), and progressive disease (PD). Secondary endpoints included progression-free survival (PFS), duration of response (DoR), and overall survival (OS). Efficacy outcomes had the same definition in both clinical trials. ORR was defined as the proportion of patients with the best overall disease response to CR or PR; no response indicated SD or PD in the case of consistent cancer progression [18]. PFS was the time from infusion to disease progression or death from any cause. DoR was the time from first objective response to disease progression or death from any cause. OS was the time from infusion to death from any cause.
In both ZUMA-5 and ELARA, evaluation of primary endpoints was based on reporting odds ratio (ROR) with a 95% confidence interval (CI) at p < 0.05. Kaplan-Meier curves were used to extract secondary endpoints—PFS, DoR, and OS—of the two treatments. Comparative efficacy was assessed using a log-rank test over 18–21 months. Statistical analyses were conducted using Microsoft Excel and R version 4.0.5.
Safety
RORs with 95% CIs were calculated to assess the disproportionality of grade 3–4 AEs, cytokine release syndrome (CRS), and neurologic events at p < 0.05. Grade 3–4 AEs included neutropenia, anemia, thrombocytopenia, pyrexia, infections, febrile neutropenia, and decreased white blood cell and lymphocyte counts. Statistical analyses were conducted using R version 4.0.5.
Cost
Treatment cost for each drug was calculated based on pivotal clinical trials. Cost was calculated from the perspective of US healthcare payers and included only direct healthcare costs. Total cost per patient included the cost of drug acquisition, administration, AE management, and retreatment with CAR T-cell therapy (relapsed patients). Wholesale acquisition costs (WACs) of one injection with axi-cel and tisa-cel were extracted from the IBM-Micromedex Red Book [19]. Administration costs of axi-cel and tisa-cel included apheresis, bridging therapy, conditioning chemotherapy (fludarabine 25–30 mg / m2 / day, and cyclophosphamide 250–500 mg / m2 / day), two IV injections (for conditioning chemotherapy and CAR T-cell therapy), and hospitalization, including in the intensive care unit (ICU). The Centers for Medicare and Medicaid Services (CMS) and previous literature were used to estimate administration costs associated with CAR T-cell therapy [11, 20,21,22,23].
Costs of grade 3–4 AEs, which appeared in at least 5% of the patients, and costs of CRS and neurologic events were extracted from the literature and inflated to 2022 USD using the medical care component of the Consumer Price Index from the US Bureau of Labor Statistics [23,24,25,26,27]. Grade 3–4 AEs included neutropenia, anemia, thrombocytopenia, hypoxia, pyrexia, decreased white blood cell count, infections, and febrile neutropenia. AE costs were calculated by multiplying their annual cost by the incidence rate. Eleven patients (8.9%) required a second dose of axi-cel therapy; they were assumed to follow the same treatment regimen as the first dose of axi-cel. No relapse was reported with tisa-cel.
Cost-minimization analyses were performed by calculating incremental costs as percentages between the two drugs. Microsoft Excel was used for all analyses.
Patient characteristics
Patient characteristics were compared to determine whether these clinical trials were comparable. The patient characteristics were as follows: age (< 65 vs. ≥ 65 years), gender (male vs. female), Eastern Cooperative Oncology Group (ECOG) performance status (0 vs. ≥ 1), disease stage (I/II vs. III/IV), follicular lymphoma international prognostic index (0–2 vs. ≥ 3), high tumor bulk, and previous lines of therapy (phosphoinositide 3-kinase inhibitors [PI3K inhibitor], anti-CD20 monoclonal antibodies [mAb], alkylating agent, lenalidomide, and stem-cell transplantation). The chi-square test (p < 0.05) was used to examine differences between these categorical variables. Statistical analyses were conducted using R version 4.0.5.
Results
Efficacy
For the primary endpoints, ORR was slightly higher with axi-cel (94%) than with tisa-cel (89%; Table 1), as CR was slightly higher with axi-cel (79%) than with tisa-cel (74%). PR was the same in both treatments (15%). Nevertheless, RORs showed no significant differences (p > 0.05%) for ORR, CR, and PR. SD appeared to be the same in axi-cel and tisa-cel clinical trials with only 3%, indicating that ROR was insignificant (p = 1). In addition, 8% had PD with the use of the tisa-cel regimen; however, axi-cel showed no PD. Approximately 2% of patients in the axi-cel clinical trial had unknown primary efficacy endpoints, and none of the participants had unknown outcomes in the tisa-cel clinical trial. ROR of PD was significant (p = 0). However, as one clinical trial had zero, the ROR result was indeterminate and could not be interpreted.
For the secondary efficacy endpoints, the log-rank test showed that PFS was insignificant between the two treatments for month 1–11 (Table 1 and S1). From the 12th month, PFS became significant with better outcomes for tisa-cel. The difference continued to be significant until the end of the data available (18 months). The log-rank test for DoR appeared to be insignificant at the end of the data available (21 months). The difference in DoR was insignificant for month 1–15; however, a significant difference was observed at months 16 and 17 (Table S2). Subsequently, the difference became insignificant until the end of the 21st month. The difference in OS was insignificant between axi-cel and tisa-cel throughout (month by month) and at the end of the 18-month period (Table S3).
Safety
Disproportionality analyses for anemia, decreased white blood cell lymphocyte counts, and grade 1 and 2 neurologic events showed insignificant results between axi-cel and tisa-cel (Fig. 1). Axi-cel was significantly associated with a lower incidence of febrile neutropenia than tisa-cel (RORs < 1, p < 0.05). Conversely, axi-cel was significantly associated with a higher incidence of neutropenia, thrombocytopenia, pyrexia, infections, grade 1 and 2 CRS, and grade 3 or higher neurologic events than tisa-cel (RORs > 1, p < 0.05). Grade 3 or higher CRS was not associated with tisa-cel. Therefore, ROR was infinite.
RORs for the CRS, neurologic events, and grade 3–4 AEs associated with CAR T cell therapies used for the treatment of relapsed or refractory follicular lymphoma. CAR T: chimeric antigen receptor-engineered T; Axi-cel: axicabtagene ciloleucel; tisa-cel, tisagenlecleucel; Ref, reference; AE, adverse event; ROR: Reporting Odds Ratio; CI, confidence interval; CRS, cytokine release syndrome
Cost
Acquisition costs for one injection of axi-cel and tisa-cel were US$424,000 and US$399,110, respectively (Table 2) [19]. Each patient in the ELARA (tisa-cel) clinical trial needed one injection only. Conversely, in the ZUMA-5 (axi-cel) clinical trial, 8.9% of the patients required a second dose.
The administration procedure started with the apheresis process to harvest peripheral blood mononuclear cells at a target dose of 2 × 106 CAR positive T-cells per kg for axi-cel and (0.6-6) × 108 CAR positive-T cells for tisa-cel. The cost of apheresis was approximately $110.39 according to the Physician Fee Schedule Final Rule [20]. Patients were allowed to receive bridging therapy consistent with their symptoms. A total of 3.2% and 45.4% of the patients received bridging therapy for axi-cel and tisa-cel, respectively. Costs of bridging therapy were estimated based on previous findings of US$3,638.74 for patients undergoing CAR T-cell therapy infusion in the US in 2022 [21]. Bridging therapy was US$117.38 for axi-cel and US$1,650.56 for tisa-cel. Conditioning chemotherapy was conducted one week before infusion of CAR T-cell therapy. Each patient received an intravenous infusion of fludarabine (25–30 mg per m2 of body-surface area per day) and cyclophosphamide (250–500 mg per m2 per day) on the 5th, 4th, and 3rd days prior to CAR T-cell therapy infusion [22]. The total cost was US$605.49 for axi-cel and US$473.95 for tisa-cel. Hospitalization was the most expensive administrative procedure, costing US$2,868.29 per day [23]. All patients in the ZUMA-5 clinical trial (axi-cel) required hospitalization for a median of 7 days, with a total cost of US$20,087.45 per patient. Approximately 82% of the patients received tisa-cel injections while they were in the hospital, and the rest were outpatients. However, 65% of outpatients required hospitalization after CAR T-cell infusion. The total hospitalization cost was US$37,982 for tisa-cel [11]. Two IV injections were required to administer the conditioning chemotherapy and CAR T-cell therapy, each costing US$140.16 [20]. The total administration cost was US$21,192 for axi-cel and US$40,497 for tisa-cel.
Except for CRS and neurologic events, only grade 3–4 AEs, which occurred in at least 5% of the patients, were included in the analysis. CRS, neurological events, and serious AEs, except for febrile neutropenia, were more intense with axi-cel than with tisa-cel. The total cost of AEs was calculated by multiplying the AE incidence rate by the unit cost for one patient. The total AE cost per patient was US$25,109 for axi-cel and US$11,278 for tisa-cel [23,24,25,26]. The mortality rates reported in pivotal clinical trials were 12.1% for axi-cel and 7.2% for tisa-cel.
The total treatment cost was US$470,301 per patient for axi-cel. However, as there was approximately 8.9% relapse with axi-cel, this increased the treatment cost up to US$512,021. Tisa-cel was less costly, with a total cost of US$450,885 per patient. As no relapse was reported with tisa-cel, the treatment cost was lower than that of axi-cel.
The cost-minimization analysis demonstrated that drug acquisition and AE management of axi-cel were associated with US$24,890 and US$13,831 increase in cost, respectively (Table 3), indicating cost increases of 6% and 55%, respectively, with axi-cel over tisa-cel. Administration cost was US$19,305 (91%) lower with axi-cel. Incremental total cost per patient indicated that US$19,416 (4%) would be saved with tisa-cel if there was no relapse, and US$61,136 (12%) with relapse.
Patient characteristics
The chi-square test showed no statistically significant differences by age (< 65 vs. ≥ 65 years), gender (male vs. female), ECOG performance status (0 vs. ≥ 1), disease stage (I/II vs. III/IV), high tumor bulk, and previous lines of therapy (Table 4). Only the follicular lymphoma international prognostic index showed a statistically significant difference between axi-cel and tisa-cel (p < 0.05). This difference was in favor of axi-cel; 44% of the patients in the axi-cel group had a higher risk than that in the tisa-cel group (59.8%).
Discussion
FL is one of the most difficult diseases to treat and is generally considered incurable. Although patients respond well to initial treatment, they tend to relapse or become refractory multiple times during their lifetime [28, 29]. There is no consensus on the best treatment option for patients with rrFL [30]. Advanced treatment strategies, such as PI3K inhibitors, stem cell transplantation, radiotherapy, and chemotherapy followed by rituximab maintenance therapy, have been shown to improve outcomes, such as OS, PFS, and quality of life (QoL), in rrFL patients [31, 32]. Nevertheless, the majority of patients relapse or become refractory and require multiple lines of treatment [33]. Therefore, new therapeutics are required to achieve control with minimal drug-related toxicity. The introduction of axi-cel and tisa-cel CAR T-cell therapy in rrFL patients has shown promising outcomes with manageable safety profiles. In the absence of a head-to-head clinical trial, this analysis compared the efficacy, safety, cost, and patient characteristics of axi-cel and tisa-cel for treatment of adult patients with rrFL after two or more lines of systemic therapy.
The analysis showed no statistically significant differences between the two treatment regimens in terms of ORR, CR, PR, or SD (p > 0.05). The median PFS, DoR, and OS were not reached in either clinical trial. Patients in the ELARA (tisa-cel) trial showed a statistically better PFS than those in the ZUMA-5 (axi-cel) trial starting from the 12th month. DoR was not significant after 21 months of follow-up. However, there was a significant difference between the 16th and 17th months, indicating that short-term follow-up is insufficient. Long term follow-up throughout the treatment course is required to understand and compare efficacy endpoints. OS was insignificant over 18 months follow-up. There is currently no efficacy analysis comparing axi-cel and tisa-cel in rrFL; however, Bachy et al. found that axi-cel was significantly associated with better ORR, PFS, and OS than tisa-cel for relapsed or refractory diffuse large B-cell lymphoma after two or more previous lines of treatment [34]. The same study demonstrated no statistically significant differences in terms of DoR. This difference could be justified, as the two diseases are subtypes of NHL with different characteristics and clinical aggressiveness (i.e., indolent, aggressive, and highly aggressive) [35, 36]. The two diseases are usually managed using different protocols, suggesting that a direct comparison between them might not be accurate even if the same drugs are used [37].
Except for febrile neutropenia, axi-cel was significantly associated with a higher incidence of serious AEs. These findings are consistent with previous studies [34, 38, 39]. Therefore, axi-cel might not be the best option for severely ill or elderly patients.
This analysis demonstrated that using tisa-cel over axi-cel for rrFL could provide a comparable efficacy profile at lower costs. Previous cost-effectiveness analysis models found that axi-cel was superior to tisa-cel for relapsed or refractory diffuse large B-cell lymphoma at a lower or minimally higher cost [17, 40]. Although this study did not use a cost-effectiveness analysis model, it measured the short-term value-cost relationship. Comparison of different diseases could be one of the reasons for the difference in outcomes. Moreover, the cost-effectiveness analysis model was conducted when the costs of axi-cel and tisa-cel were the same at US$373,000, whereas axi-cel costs increased, with incremental cost of US$24,890 over tisa-cel, in the present study [17].
Patient characteristics were compared between ZUMA-5 and ELARA clinical trials to identify statistically significant differences that could affect study outcomes. The results revealed that only the follicular lymphoma international prognostic index was statistically significant. Approximately 59.8% of the patients had ≥ 3 (high risk) in the ELARA trial compared to 44% in the ZUMA-5 trial. The follicular lymphoma international prognostic index was used to predict FL survival rates in patients receiving chemotherapy [41,42,43]. Consequently, patients in the ELARA study had lower odds of better outcomes than those in the ZUMA-5 study. In addition, all characteristics were comparable between the two trials.
This analysis indicated that using tisa-cel over axi-cel for rrFL after two or more lines of systemic therapy could provide a comparable efficacy profile for ORR, DoR, and OS, a better efficacy profile for PFS, lower mortality rate, lower incidence of serious AEs, and US$61,136 savings over the first 18 months after adoption. However, further long-term research with a larger sample size is required to confirm these findings.
Limitations
This study was based on data derived from two separate clinical trials with different populations and inclusion and exclusion criteria. The main limitation of this analysis was the absence of a head-to-head clinical trial. WAC was used to represent acquisition costs of axi-cel and tisa-cel, which did not include rebates, co-payments, or discounts. Moreover, this analysis only estimated direct healthcare costs and did not include indirect costs.
Conclusions
The use of axi-cel and tisa-cel CAR T-cell therapies for rrFL after two or more lines of treatment appeared to be effective with manageable safety profiles. Axi-cel was associated with a comparable efficacy profile, more serious AEs, and higher cost than tisa-cel. However, further research with head-to-head clinical trials and patient follow-up over the treatment course is required to understand and compare efficacy and safety profiles, as well as to assess the economic impact of these CAR T-cell therapies.
References
Freedman A, Jacobsen E (2020) Follicular lymphoma: 2020 update on diagnosis and management. Am J Hematol 95(3):316–327. https://doi.org/10.1002/ajh.25696
Kaseb H, Ali MA, Koshy NV (2022) Follicular lymphoma. StatPearls. Treasure Island (FL), vol 27. StatPearls Publishing
Dreyling M, Ghielmini M, Rule S et al (2021) Newly diagnosed and relapsed follicular lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 32(3):298–308. https://doi.org/10.1016/j.annonc.2020.11.008
Dada R (2019) Diagnosis and management of follicular lymphoma: a comprehensive review. Eur J Haematol 103(3):152–163. https://doi.org/10.1111/ejh.13271
National Cancer Institute (NIH). Cancer Stat Facts: NHL — Follicular Lymphoma. https://seer.cancer.gov/statfacts/html/follicular.html. Accessed December 19 2022
Apostolidis J, Mokhtar N, Al Omari R, Darweesh M, Al Hashmi H (2020) Follicular lymphoma: update on management and emerging therapies at the dawn of the new decade. Hematol Oncol 38(3):213–222. https://doi.org/10.1002/hon.2711
Casulo C, Byrtek M, Dawson KL et al (2015) Early Relapse of Follicular Lymphoma after Rituximab Plus Cyclophosphamide, Doxorubicin, Vincristine, and Prednisone defines patients at high risk for death: an analysis from the National LymphoCare Study [published correction appears in J Clin Oncol. 2016;34(12):1430] [published correction appears in J Clin Oncol. 2016;34(12):1430]. J Clin Oncol 33:2516–2522. https://doi.org/10.1200/JCO.2014.59.7534
Cheah CY, Fowler NH (2018) Novel agents for relapsed and refractory follicular lymphoma. Best Pract Res Clin Haematol 31(1):41–48. https://doi.org/10.1016/j.beha.2017.11.003
Erblich T, Montoto S (2018) Treating relapsed follicular lymphoma. Expert Rev Hematol 11(5):403–410. https://doi.org/10.1080/17474086.2018.1453801
Becnel MR, Nastoupil LJ (2018) Follicular Lymphoma: Past, Present, and Future. Curr Treat Options Oncol. ;19(7):32. Published 2018 May 24. https://doi.org/10.1007/s11864-018-0550-0
Fowler NH, Dickinson M, Ghosh M et al (2022) Assessment of Healthcare Resource utilization and hospitalization costs in patients with relapsed or refractory follicular lymphoma undergoing CAR-T cell therapy with Tisagenlecleucel: results from the ELARA Study [published online ahead of print, 2022 sep 28]. Transpl Cell Ther S2666–6367(22):01660–01668. https://doi.org/10.1016/j.jtct.2022.09.022
U.S. Food and Drug Administration (FDA) FDA grants accelerated approval of axicabtagene ciloleucel for relapsed or refractory follicular lymphoma. Accessed December 12, (2022) https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-axicabtagene-ciloleucel-relapsed-or-refractory-follicular-lymphoma. Accessed December 12, 2022
U.S. Food and Drug Administration. KYMRIAH (tisagenlecleucel). Accessed December 12, (2022) https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/kymriah-tisagenlecleucel
Jacobson CA, Chavez JC, Sehgal AR et al (2022) Axicabtagene ciloleucel in relapsed or refractory indolent non-hodgkin lymphoma (ZUMA-5): a single-arm, multicentre, phase 2 trial. Lancet Oncol 23(1):91–103. https://doi.org/10.1016/S1470-2045(21)00591-X
Fowler NH, Dickinson M, Dreyling M et al (2022) Tisagenlecleucel in adult relapsed or refractory follicular lymphoma: the phase 2 ELARA trial. Nat Med 28(2):325–332. https://doi.org/10.1038/s41591-021-01622-0
Ghanem B, Shi L (2022) The Economic Burden of CAR T Cell Therapies Ciltacabtagene Autoleucel and Idecabtagene Vicleucel for the treatment of adult patients with relapsed or refractory multiple myeloma in the US. BioDrugs 36(6):773–780. https://doi.org/10.1007/s40259-022-00557-3
Liu R, Oluwole OO, Diakite I, Botteman MF, Snider JT, Locke FL (2021) Cost effectiveness of axicabtagene ciloleucel versus tisagenlecleucel for adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy in the United States. J Med Econ 24(1):458–468. https://doi.org/10.1080/13696998.2021.1901721
Cheson BD, Fisher RI, Barrington SF et al (2014) Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-hodgkin lymphoma: the Lugano classification. J Clin Oncol 32(27):3059–3068. https://doi.org/10.1200/JCO.2013.54.8800
IBM Watson, Micromedex IBM (2022) RED BOOK Online. [Database]. http://www. micro medex solut ions. com. Accessed 16 November 2022
Centers for Medicare & Medicaid Services (2022) Physician Fee Schedule Final Rule. https://www.cms.gov/Medicare/ Medic are- Fee- for-Servi ce- Payme nt/ Physi cianF eeSch ed. Published Accessed Novermver 16 2022
Simons CL, Malone D, Wang M et al (2021) Cost-effectiveness for KTE-X19 CAR T therapy for adult patients with relapsed/refractory mantle cell lymphoma in the United States. J Med Econ 24(1):421–431. https://doi.org/10.1080/13696998.2021.1894158
Centers for Medicare and Medicaid Services (2022) ASP Drug Pricing Files. 2022. https://www.cms.gov/medicare/ medic arepart-b- drug- avera ge- sales- price/ 2022- asp- drug- prici ng- files. Accessed November 16 2022. (HCPCS J9185)
Potnis KC, Di M, Isufi I et al (2022) Cost-Effectiveness of Chimeric Antigen Receptor T-Cell Therapy in Adults with Relapsed or Refractory Follicular Lymphoma [published online ahead of print, 2022 Nov 7]. Blood Adv. ;bloodadvances.2022008097. https://doi.org/10.1182/bloodadvances.2022008097
Guzauskas GF, Masaquel A, Reyes C, Bernaards C, Krivasi T, Veenstra DL (2018) Cost-effectiveness of obinutuzumab plus bendamustine followed by obinutuzumab monotherapy for the treatment of follicular lymphoma patients who relapse after or are refractory to a rituximab-containing regimen in the US. J Med Econ 21(10):960–967. https://doi.org/10.1080/13696998.2018.1489254
Eichten C, Ma Q, Delea TE et al (2021) Lifetime costs for treated follicular lymphoma patients in the US. PharmacoEconomics 39(10):1163–1183. https://doi.org/10.1007/s40273-021-01052-3
Badaracco J, Gitlin M, Keating SJ (2022) A model to Estimate Cytokine Release Syndrome and neurological event management costs Associated with CAR T-Cell therapy [published online ahead of print, 2022 Oct 19]. Transpl Cell Ther S2666–6367(22):01704–01703. https://doi.org/10.1016/j.jtct.2022.10.009
U.S. Bureau of Labor Statistics. Consumer price index. Accessed November 16 (2022) https://www.bls.gov/cpi
Batlevi CL, Sha F, Alperovich A et al (2020) Follicular lymphoma in the modern era: survival, treatment outcomes, and identification of high-risk subgroups. Blood Cancer J 10(7):74 Published 2020 Jul 17. https://doi.org/10.1038/s41408-020-00340-z
Izutsu K (2014) Treatment of follicular lymphoma. J Clin Exp Hematop 54(1):31–37. https://doi.org/10.3960/jslrt.54.31
Luminari S, Trotman J, Federico M (2020) Advances in treatment of follicular lymphoma. Cancer J 26(3):231–240. https://doi.org/10.1097/PPO.0000000000000444
Matasar MJ, Luminari S, Barr PM et al (2019) Follicular lymphoma: recent and emerging therapies, treatment strategies, and remaining unmet needs. Oncologist 24(11):e1236–e1250. https://doi.org/10.1634/theoncologist.2019-0138
Bargetzi M, Baumann R, Cogliatti S et al (2018) Diagnosis and treatment of follicular lymphoma: an update. Swiss Med Wkly 148:w14635. https://doi.org/10.4414/smw.2018.14635. Published 2018 Jul 24
Casulo C, Larson MC, Lunde JJ et al (2022) Treatment patterns and outcomes of patients with relapsed or refractory follicular lymphoma receiving three or more lines of systemic therapy (LEO CReWE): a multicentre cohort study. Lancet Haematol 9(4):e289–e300. https://doi.org/10.1016/S2352-3026(22)00033-3
Bachy E, Le Gouill S, Di Blasi R et al (2022) A real-world comparison of tisagenlecleucel and axicabtagene ciloleucel CAR T cells in relapsed or refractory diffuse large B cell lymphoma. Nat Med 28(10):2145–2154. https://doi.org/10.1038/s41591-022-01969-y
Koff JL, Chihara D, Phan A, Nastoupil LJ, Williams JN, Flowers CR (2015) To each its own: linking the Biology and Epidemiology of NHL subtypes. Curr Hematol Malig Rep 10(3):244–255. https://doi.org/10.1007/s11899-015-0267-0
Harris NL, Jaffe ES, Diebold J et al (1999) World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the clinical Advisory Committee meeting-Airlie House, Virginia, November 1997. J Clin Oncol 17(12):3835–3849. https://doi.org/10.1200/JCO.1999.17.12.3835
Ghielmini M, Vitolo U, Kimby E et al (2013) ESMO Guidelines consensus conference on malignant lymphoma 2011 part 1: diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL) and chronic lymphocytic leukemia (CLL). Ann Oncol. ;24(3):561–576. https://doi.org/10.1093/annonc/mds517
Fusaroli M, Isgrò V, Cutroneo PM et al (2022) Post-marketing Surveillance of CAR-T-Cell Therapies: analysis of the FDA adverse event reporting system (FAERS) database. Drug Saf 45(8):891–908. https://doi.org/10.1007/s40264-022-01194-z
Bonaldo G, Montanaro N, AlbertoVaccheri, Motola D (2021) Safety profile of chimeric antigen receptor T-cell immunotherapies (CAR-T) in clinical practice. Eur J Clin Pharmacol 77(8):1225–1234. https://doi.org/10.1007/s00228-021-03106-z
Cummings Joyner AK, Snider JT, Wade SW et al (2022) Cost-effectiveness of chimeric Antigen receptor T cell therapy in patients with relapsed or refractory large B cell lymphoma: no impact of site of Care. Adv Ther 39(8):3560–3577. https://doi.org/10.1007/s12325-022-02188-0
Nooka AK, Nabhan C, Zhou X et al (2013) Examination of the follicular lymphoma international prognostic index (FLIPI) in the National LymphoCare study (NLCS): a prospective US patient cohort treated predominantly in community practices. Ann Oncol 24(2):441–448. https://doi.org/10.1093/annonc/mds429
Yang G, Mills M, Kim Y et al (2019) Enhancement of the follicular Lymphoma International Prognostic Index (FLIPI) with lymphopenia (FLIPI-L): a predictor for overall survival and histologic transformation. Blood Cancer J 9:104. https://doi.org/10.1038/s41408-019-0269-6
Solal-Céligny P, Roy P, Colombat P et al (2004) Follicular lymphoma international prognostic index. Blood 104(5):1258–1265. https://doi.org/10.1182/blood-2003-12-4434
Funding
The author received no financial support for this research.
Open access funding provided by SCELC, Statewide California Electronic Library Consortium
Author information
Authors and Affiliations
Contributions
Author ContributionsButhainah Ghanem: Concept and design, acquisition of data, analysis and interpretation of data, and drafting of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Author declares no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ghanem, B. Efficacy, safety, and cost-minimization analysis of axicabtagene ciloleucel and tisagenlecleucel CAR T-Cell therapies for treatment of relapsed or refractory follicular lymphoma. Invest New Drugs 41, 710–718 (2023). https://doi.org/10.1007/s10637-023-01389-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-023-01389-w