Abstract
Introduction
Cost-effectiveness data on chimeric antigen receptor (CAR) T cell therapies for relapsed/refractory large B cell lymphoma (R/R LBCL), accounting for inpatient/outpatient site of care (site), are sparse.
Methods
This payer model compares lifetime costs/benefits for CAR T cell-treated (axicabtagene ciloleucel [axi-cel], lisocabtagene maraleucel [liso-cel], tisagenlecleucel [tisa-cel]) patients with R/R LBCL in the USA. Three-month post-infusion costs were derived from unit costs and real-world all-payer (RW) site-specific utilization data for 1175 patients with diffuse R/R LBCL (CAR T cell therapy October 2017–September 2020). Therapy- and site-specific grade 3+ cytokine release syndrome (CRS) and neurologic event (NE) incidences were imputed from published trials. Lifetime quality-adjusted life-years (QALYs) and long-term costs were calculated from therapy-specific overall and progression-free survival data, adjusted for differences in trial populations. The base case used 17% outpatient site (RW) for all therapies. ZUMA-1 trial cohorts 1/2 informed other axi-cel base case inputs; ZUMA-1 cohorts 4/6 data (updated safety management) supported scenario analyses.
Results
Base case total costs for axi-cel exceeded liso-cel ($637 K versus $621 K) and tisa-cel ($631 K versus $577 K) costs. Three-month post-infusion costs were $57 K to $59 K across all therapies. Total QALYs for axi-cel also exceeded those for liso-cel (7.7 versus 5.9) and tisa-cel (7.2 versus 5.0) with incremental costs per QALY gained of $9 K versus liso-cel and $25 K versus tisa-cel. Base case incremental net monetary benefit was $255 K (95% confidence interval (CI) $181–326 K) for axi-cel versus liso-cel, and $280 K (95% CI $200–353 K) versus tisa-cel. Longer survival with axi-cel conferred higher lifetime costs. In all scenarios (e.g., varied outpatient proportions, CRS/NE incidence), axi-cel was cost-effective versus both comparators at a maximum willingness-to-pay of under $26 K/QALY as a result of axi-cel’s higher incremental survival gains and quality-of-life.
Conclusions
Axi-cel is a cost-effective CAR T cell therapy for patients with R/R LBCL compared to tisa-cel and liso-cel. Site of care does not impact the cost-effectiveness of CAR T cell therapy.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Why carry out this study? |
Chimeric antigen receptor (CAR) T cell therapies have changed the treatment paradigm for patients with relapsed or refractory large B cell lymphoma (R/R LBCL). |
There are three anti-CD19 CAR T cell therapies approved for R/R LBCL by the US Food and Drug Administration, but the relative cost-effectiveness of these therapies, accounting for site of care (i.e., inpatient/outpatient infusion), has not yet been well evaluated. |
To address this knowledge gap, we constructed a payer perspective model to compare lifetime costs/benefits for CAR T cell-treated (axicabtagene ciloleucel [axi-cel], lisocabtagene maraleucel [liso-cel], tisagenlecleucel [tisa-cel]) patients with R/R LBCL in the USA. |
What has been learned from this study? |
For patients with R/R LBCL, axi-cel confers a greater survival benefit than other approved CAR T therapies and is also cost-effective compared to those therapies (i.e., tisa-cel and liso-cel). |
Site of care does not impact the cost-effectiveness of CAR T cell therapy. |
Introduction
Cellular immunotherapy using chimeric antigen receptor (CAR) transduced T cells has changed the treatment paradigm for patients with relapsed or refractory large B cell lymphoma (R/R LBCL). There are currently three anti-CD19 CAR T cell therapies approved by the US Food and Drug Administration (FDA) for the treatment of adult patients with R/R LBCL after two or more lines of systemic therapy: axicabtagene ciloleucel (axi-cel; YESCARTA® [1]), lisocabtagene maraleucel (liso-cel; BREYANZI® [2]), and tisagenlecleucel (tisa-cel; KYMRIAH® [3]) [4]. The approvals were made on the basis of the results of the ZUMA-1 trial for axi-cel [5], TRANSCEND trial for liso-cel [6], and JULIET trial for tisa-cel [7].
The overall response rates reported in trials of these CAR T cell therapies has ranged from 52% (tisa-cel) to 82% (axi-cel) [5,6,7] However, CAR T cell therapies are also associated with two potentially serious adverse events (AEs): cytokine release syndrome (CRS) and neurologic event (NE). In the ZUMA-1 trial of axi-cel, grade 3+ CRS and NE occurred in 13% and 28%, respectively, of patients in pivotal cohorts 1 and 2 [5]. Corresponding numbers are 22% and 12% from the JULIET trial for tisa-cel [7], and 2% and 10% from the TRANSCEND trial for liso-cel [6]. Onset of CRS and NE are typically 2–3 days and 4–10 days after CAR T cell infusion, with durations of 7–8 days and 14–17 days, respectively [8]. Disease burden, lymphodepletion regimen, and CAR T cell dose can impact the severity of CRS and NE [9]. Treatment for CRS includes anti-IL-6 therapy (e.g., tocilizumab) and corticosteroids, while treatment for NE is mainly corticosteroids with additional supportive care [8].
To mitigate the risks of CRS and NE, healthcare facilities that dispense and administer CAR T cell therapy must be enrolled in and comply with the Risk Evaluation and Mitigation Strategies requirements [4]. As such, CAR T cell therapies are currently administered at authorized treatment centers and are primarily delivered in the inpatient setting.
Interest in outpatient administration is growing over time as safety management improves. Indeed, 26% of patients in the JULIET trial received tisa-cel in outpatient sites of care [7]. As use of CAR T cell therapies continues to evolve, especially with regard to site of care, it is important to understand the cost-effectiveness (CE) and value of these therapies. This study addresses payer costs and health benefits of CAR T cell therapy for patients with R/R LBCL who previously received at least two lines of systemic therapy, while accounting for site of CAR T cell infusion. The analysis estimates CE results for specific CAR T cell therapies (i.e., axi-cel, tisa-cel, and liso-cel) over time horizons ranging from 3 months to patient lifetime, with health benefits captured in the form of quality-adjusted life-years (QALYs). Real-world data on short-term healthcare resource use post CAR T cell infusion, stratified by CAR T cell site of care and CRS and NE status, informed cost estimates.
Methods
Structure
A decision-tree model compared lifetime direct healthcare costs and benefits between axi-cel and each of two other CAR T cell therapies marketed in the USA: tisa-cel and liso-cel (Fig. 1). The costs included in the model span the pre-infusion period through patients’ expected lifetimes (Fig. S1 in the supplementary material). Cost calculations accounted for the proportion of patients infused with CAR T cells in inpatient versus outpatient sites of care and site-specific CRS and NE incidence for each treatment. Partitioned survival models based on Liu et al. [10] and Oluwole et al. [11] formed the basis of post-infusion cost and QALY estimates (Fig. S2a, b in the supplementary material).
Data
For all CAR T cell therapies, safety and efficacy input values were derived from clinical trial data and utilization input values came from claims data. Ninety-day post-infusion costs apart from those associated with stem cell transplant (SCT) and use of intravenous immune globulin (IVIG) were derived from real-world resource use estimates. Anlitiks All-Payor Claims (AAPC) data were analyzed to assess average per patient inpatient days (intensive care unit (ICU) and non-ICU), emergency department (ED) visits, and outpatient/other visits in the 91-day period beginning on the day of CAR T cell infusion, stratified by CAR T cell site of care and CRS and NE status. The AAPC data comprise linked pharmacy and medical claims from a nationally representative sample of patients with Commercial, Medicaid, Medicare Fee-for-Service, or Medicare Advantage healthcare coverage.
The AAPC analysis included data from 1175 adult patients with R/R diffuse LBCL who had at least 6 months of continuous health plan enrollment prior to receiving CAR T cell therapy between October 2017 and September 2020. In this sample, average rates of healthcare resource utilization as described above were evaluated separately in six subgroups defined by CAR T cell site of care (inpatient or outpatient) and AE status (CRS, NE, or neither) and used to estimate short-term healthcare resource use among modeled patients (S3 and Table S4 in the supplementary material).
The percentage of patients infused with CAR T cells in an inpatient versus outpatient setting was also derived from AAPC data. In the base case,Footnote 1 the same proportion of outpatient use, equal to the overall rate observed in the full sample of patients identified in the AAPC data, was used for all three CAR T cell therapies studied. However, rates were varied for each CAR T cell treatment independently in sensitivity analyses (Table 1, and Table S5 in the supplementary material).
Cost Estimation
The model estimates average per patient lifetime costs (2020 US dollars) as the sum of five categories of costs (Fig. S1 in the supplementary material):
-
1.
CAR T cell-related and other relevant pre-infusion costs (t ≤ 0), including costs of apheresis, bridging therapy, lymphodepletion chemotherapy, and CAR T cell acquisition and administration
-
2.
Near-term post-infusion costs (0 ≤ t ≤ 90 days), including ICU, non-ICU inpatient, ED, and outpatient/other costs
-
3.
Distant post-infusion costs (t > 90 days), including costs associated with pre-progression and post-progression routine care applied to surviving patients
-
4.
End of life costs (t > 3 days), including costs of palliative and other end of life care applied monthly to the newly deceased share of patients
-
5.
Other post-infusion costs (0 < t ≤ 365 days), including post-infusion SCT costs applied in months 2–3 to the share of (living) patients undergoing SCT post CAR T cell infusion, and IVIG costs incurred during the first model year post infusion
Benefit Estimation
Benefits were determined for each CAR T cell treatment, regardless of the CAR T cell site of care, on the basis of prior partitioned survival models developed using matching-adjusted indirect comparison (MAIC) survival curves from the clinical trials of each CAR T cell treatment, along with health utility multipliers accounting for time since CAR T cell infusion and progression status.
MAIC-adjusted overall survival (OS) and progression-free survival (PFS) curves for axi-cel, tisa-cel, and liso-cel from Liu et al. [10] and Oluwole et al. [11] were used to model long-term costs, QALYs, life years, and NMB associated with each therapy. The MAICs matched axi-cel individual patient data to the baseline characteristics of each other CAR T cell trial (i.e., JULIET and TRANSCEND) separately. The axi-cel-matched to liso-cel results are only used when comparing axi-cel to liso-cel; similarly, the axi-cel matched to tisa-cel results are only used when comparing axi-cel to tisa-cel. Accordingly, there are two sets of input data for axi-cel and two corresponding sets of results in this analysis. The researchers did not have access to individual patient data for liso-cel matched to tisa-cel or vice versa, so direct comparisons between liso-cel and tisa-cel were not made.
CAR T Cell Inputs
All patients were assumed to receive CAR T cell therapy. CAR T cell wholesale acquisition costs came from Red Book (Table 2, and Table S6 in the supplementary material) [12]. Costs per patient receiving lymphodepleting chemotherapy (bendamustine, cyclophosphamide-fludarabine) were calculated separately for each CAR T cell therapy on the basis of the body surface area-based dosing schedule(s) followed in the relevant FDA-approved labels [1,2,3] assuming no vial sharing across patients and a mean per patient body surface area of 78.7 m2 [13]. In the base case, estimated costs of lymphodepletion were approximately $9 K per patient receiving bendamustine and between $2 and $3 K per patient receiving cyclophosphamide-fludarabine for all CAR T cell therapies.
Percentages of patients receiving bridging therapy, lymphodepleting chemotherapy, SCT after CAR T cell therapy, and post-infusion IVIG, as well as incidence rates of grade 3+ CRS and NEs (CRS only, NE only, and comorbid CRS and NE) were based on the ZUMA-1 trial program for axi-cel [5, 14], the TRANSCEND trial program for liso-cel [6, 15], and the JULIET trial program for tisa-cel [7, 16, 17]. In the base case, where possible, matching-adjusted estimates based on prior published indirect comparisons to liso-cel and tisa-cel were used for inputs specific to axi-cel. CRS and NE were assumed to present within 90 days following CAR T cell infusion for all therapies. The ratio of CRS and NE incidence between inpatient and outpatient CAR T cell sites of care was estimated from data published on the TRANSCEND and OUTREACH liso-cel trials [18]. As a result of lack of product-specific data, the same ratio was used for axi-cel and tisa-cel but ratios were varied for each therapy independently in sensitivity analyses.
As discussed above, OS and PFS were derived from the relevant survival curves previously generated using partitioned survival mixture-cure models based on the results of MAIC of axi-cel to each of tisa-cel [10] and liso-cel [11] (Fig. S2a, b in the supplementary material).
General Model Inputs
General inputs applied to all CAR T cell therapies included unit costs unrelated to CAR T cell acquisition; select patient characteristics; and health utility multipliers (Table 1, and Table S5 in the supplementary material). All patients were assumed to undergo apheresis and to receive CAR T cell therapy; the same unit costs of CAR T cell administration and apheresis from the 2021 Centers for Medicare and Medicaid Services (CMS) Physician Fee Schedule [19] were applied to all patients for all CAR T cell therapies. Supportive care therapy costs were also the same across CAR T cell therapies in terms of the cost per pack of bendamustine, cyclophosphamide, fludarabine, and IVIG based on Red Book® WAC prices from 2021 [12]. SCT and bridging therapy costs included costs for the entire episode of care and were based on estimates from published literature [20, 21].
Costs associated with inpatient hospitalization in the 91 days following and including the day of CAR T cell infusion were based on unit costs and quantities of ICU days, non-ICU days, ED visits, and outpatient and other facility visits. Unit costs came from Gershengorn et al. [22], the 2021 HCUP National inpatient sample [23], and the 2021 CMS Physician Fee Schedule [19]. Numbers of visits and days were derived from aforementioned analyses of real-world data.
Costs incurred more than 90 days post CAR T cell infusion were based on progression status (pre versus post progression) and represent bundled costs associated with routine care. Consistent with Liu et al. [10], the average monthly cost of routine care per progression-free patient was assumed to decrease after 5 years post CAR T cell infusion. Both pre- and post-progression unit costs, as well as end-of-life care costs, were derived from Liu et al. [10].
All costs were inflation-adjusted to 2020 USD based on the medical care component of the Consumer Price Index (CPI) [24].
Health utilities, a commonly used measure of both life span and quality-of-life [25], were sourced from the literature and based on both time since CAR T cell infusion and progression status [26]. A single utility value was applied to surviving patients in the first 30 days following CAR T cell infusion regardless of progression status [27]. After that, health utility was assumed to increase at day 30 and again at the end of the fifth year following CAR T cell infusion among progression-free patients [27]. The lowest utility value was applied to all patients in post progression irrespective of time since CAR T cell infusion [26].
Results Presentation
Payer costs and health benefits (both discounted at 3% annually) were used to estimate NMB for each therapy, as well as incremental net monetary benefit (INMB) and incremental cost-effectiveness ratios (ICERs) for axi-cel versus tisa-cel and axi-cel versus liso-cel under the assumption that a QALY gained is worth $150,000 [28]. Also referred to as incremental costs per QALY gained, ICERs are commonly used to determine whether the added benefits associated with use of one therapy versus another justify a parallel increase in costs. In other words, they speak to the relative value to a payer or other stakeholder of one therapy compared to another. To make this determination, ICERs are typically evaluated against conventional thresholds ($150,000 per QALY in this case) representing stakeholders’ maximum willingness-to-pay per unit of added benefit. In general, the lower the ICER, the greater the value. ICERs and INMBs are calculated for axi-cel through direct comparisons with liso-cel and tisa-cel owing to the use of MAIC-matched input values which are specific to pair-wise comparisons [29]. Deterministic sensitivity analyses (DSA) were conducted for uncertain parameters and results are presented in tornado diagrams for the 20 parameters with the greatest impact on INMB. Probabilistic sensitivity analyses (PSA) were performed to account for uncertainty in model parameters simultaneously, using 5000 second-order Monte Carlo simulations. PSA parameter values and distributions appear in Tables S5 and S6 in the supplementary material.
Scenario Analysis
In the base case, relevant axi-cel input values were based on ZUMA-1 cohorts 1 and 2. To examine the effect of alternative safety protocols adopted for more recent ZUMA-1 cohorts, scenario analyses were conducted using ZUMA-1 cohort 4 [30] and ZUMA-1 cohort 6 [31] to inform relevant axi-cel input values (Table S7 in the supplementary material). ZUMA-1 cohort 4 patients received earlier corticosteroids and/or tocilizumab in response to CRS and NE, while cohort 6 patients received prophylactic and earlier corticosteroids and/or tocilizumab for prevention/treatment of CRS and NE. A scenario analysis using unadjusted AE incidence rates from ZUMA-1 cohorts 1 and 2 was also conducted.
Two additional scenario analyses were conducted to evaluate the effect of simultaneous changes in the proportions of patients infused in an inpatient site of care for all CAR T cell therapies. In the first, all patients were assumed to receive CAR T cell therapy in an inpatient site of care. In the second, approximately 34% were assumed to receive CAR T cell therapy in an outpatient site of care.
Ethics Compliance
This study is based on published data and data derived from retrospective analysis of an existing HIPAA-compliant database and does not contain any individual patient data.
Results
Tisa-cel had the lowest total healthcare cost followed by liso-cel and axi-cel in the base case (Table 3). CAR T cell acquisition costs contributed the largest proportion of these costs and explained most of the total cost differences between therapies. Post-infusion SCT costs were also lower for tisa-cel than for liso-cel or axi-cel. IVIG costs were lowest for liso-cel. Inpatient costs, including ICU and non-ICU days, and outpatient and ED costs were similar across CAR T cell therapies. Long-term (more than 90 days after CAR T cell administration) costs formed the majority of total costs unrelated to CAR T cell acquisition, and were lowest for tisa-cel and highest for axi-cel.
Life years, including pre-progression and post-progression life-years, were highest for axi-cel. In turn, QALYs were also the highest for axi-cel in both comparisons with the greatest differences between therapies occurring in the pre-progression period, which was longest for axi-cel. Because only living patients receive routine care, the additional life years associated with axi-cel also explain why long-term costs of routine care are highest for axi-cel.
When considering monetary benefit, axi-cel had the highest NMB despite its higher total direct costs: $518,624 versus liso-cel and $454,719 versus tisa-cel, followed by liso-cel at $263,711 and tisa-cel at $174,246. As a result, INMB (95% CI) was $255 K ($181–326 K) for axi-cel versus liso-cel and $280 K ($200–353 K) for axi-cel versus tisa-cel. Differences in NMB are attributable to axi-cel’s greater accumulation of lifetime QALYs. Because the incremental costs associated with axi-cel are relatively small compared to the QALYs gained by its patients, ICERs for axi-cel versus its comparators were substantially lower than the $150 K per QALY threshold used to evaluate axi-cel’s relative cost-effectiveness ($8946 versus liso-cel and $24,506 versus tisa-cel).
In both comparisons, one-way sensitivity analyses indicated that the health benefit discount rate, CAR T cell acquisition costs, and utility for the pre-progression period of the partitioned survival curves have the greatest leverage over INMB (Fig. 2a, b). However, in no case does the change in one parameter cause the results to decrease below $0; INMB indicated that axi-cel is more cost-effective than the other CAR T cell therapies in all one-way sensitivity analyses. Notably, CAR T cell site of care appears to have little impact on NMB of CAR T cell therapy.
a Axi-cel matched to liso-cel deterministic sensitivity analysis results. Top 20 input parameters with greatest impact on INMB for axi-cel versus liso-cel. b Axi-cel matched to tisa-cel deterministic sensitivity analysis results. Top 20 input parameters with greatest impact on INMB for axi-cel versus tisa-cel. Black square, low parameter value. Purple square, high parameter value. CAR chimeric antigen receptor, CRS cytokine release syndrome, ICU intensive care unit, inpt inpatient, IVIG intravenous immune globulin, NE neurologic event, prog. progression, pt patient, SCT stem cell transplant, t time since CAR T cell infusion
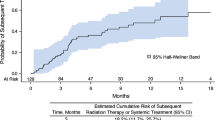
The PSA indicates that results are robust to QALYs having a value substantially lower than the $150,000 used in the base case (Fig. 3a, b). Results would favor liso-cel if a QALY were valued at $8750 or less; results would favor tisa-cel if a QALY were valued at $24,500 or less. Results would also favor tisa-cel but not liso-cel if the time horizon were limited to 1 year.
a Axi-cel matched to liso-cel probabilistic sensitivity analysis results. Cost-effectiveness acceptability curves, axi-cel versus liso-cel. b Axi-cel matched to tisa-cel probabilistic sensitivity analysis results. Cost-effectiveness acceptability curves, axi-cel versus tisa-cel. QALY quality-adjusted life-year, WTP willingness-to-pay
Scenario analyses examining the effects of using unadjusted CRS and NE rates and alternative ZUMA-1 cohort(s) to inform relevant input values for axi-cel generated similar results (Table S8a, b in the supplementary material). Comparing to liso-cel, INMB was lowest when relevant input values for axi-cel, including (unadjusted) CRS and NE rates, were sourced from ZUMA-1 cohort 4 ($252,505). While CRS and NE rates were lower for cohort 4 relative to cohorts 1 and 2 (both MAIC-adjusted and unadjusted), more than two-thirds of patients in cohort 4 received bridging therapy compared to none in cohorts 1 and 2. As a result, lifetime costs for axi-cel were slightly higher under this scenario as compared to the base case. The largest change in INMB occurred when input values for axi-cel were instead based on ZUMA-1 cohort 6 for which no grade 3 or higher CRS events were observed and for which NE incidence was less than half the MAIC-adjusted base-case rate derived from cohorts 1 and 2. Here, cost savings associated with the substantial decreases in CRS and NE incidence and post-infusion SCT rates more than offset the cost increases arising from the use of bridging therapy in more than half of patients, leading to an INMB of $269,336. These trends persisted in the comparison of axi-cel to tisa-cel, with INMB bottoming at $278,097 (cohort 4 scenario) and peaking at $294,892 (cohort 6 scenario).
Two final scenario analyses showed that results were similarly robust to simultaneous changes across all CAR T cell therapies to the proportions of patients infused in an inpatient site of care. Both when assuming 100% of patients are infused in an inpatient site of care and when assuming 34% are infused in an outpatient site of care, INMB for axi-cel versus each comparator deviated from the corresponding base-case INMB by less than 1%.
Discussion
Our data suggest that axi-cel is a cost-effective CAR T cell option for patients with R/R LBCL compared to tisa-cel and liso-cel, regardless of setting of infusion. Axi-cel’s value was largely determined by the health benefits associated with the increases in overall and pre-progression survival time relative to the other CAR T cell therapies. Results were not sensitive to changes in the ZUMA-1 cohort(s) used to inform relevant inputs for axi-cel or to the proportion of patients infused in an inpatient site of care when applied to all CAR T cell therapies simultaneously. Axi-cel input values in the base case were based on the older ZUMA-1 cohorts 1 and 2, with ZUMA-1 cohort 4 and cohort 6 being tested in scenario analyses to assess the effects of updated safety protocols reflecting earlier and prophylactic treatment with corticosteroids and/or tocilizumab for CRS and NE risk management.
Our model addresses a similar research question as the one raised in Lyman et al. [32], which sought to identify whether inpatient or outpatient provision of CAR T cell therapy was less costly over a 1-month window from treatment initiation. In contrast to that earlier work, our model is empirical and reduces the number of assumptions for key model inputs, including for the cost of CRS and NE management. Our model estimates that long-term routine care represents the costliest category of post-infusion care, while short-term care in the 90 days immediately following CAR T cell infusion is second. The management of CRS and NE plays a key role in shaping these short-term costs. The short-term cost estimates used in our model, obtained through an analysis of real-world data from a large, nationally representative database covering the major public and commercial payers, are likely substantially more reliable than assumptions that are not tied to direct experience as in that earlier analysis.
A key finding from Lyman et al. is that administering CAR T cell therapy in non-academic or academic specialty oncology networks saves approximately $33,000 per patient over the 30-day period after receipt of CAR T cell infusion [32]. This result may not be surprising given that inpatient care is more expensive than outpatient care over short periods of time, and care at academic centers is more expensive than care in community facilities [33]. Independent of the limitation of using cost assumptions that are unanchored to real-world data as noted above, the short time window upon which this conclusion is based also raises concern. In general, a longer perspective, such as the lifetime horizon used in our model, provides a more realistic and complete picture of the true benefits and cost-effectiveness of a therapy, especially in a disease where patients may live for a substantial number of years after the therapy is provided. Depending on the expected course of the disease being evaluated, a 30-day follow-up may be unlikely to reveal critical between-therapy differences, including the impact of differential efficacy, and this therapy differentiation may only be apparent when a longer time horizon is used. Our study, for example, highlights the fact that estimated morbidity, mortality, and costs incurred more than 30 days post infusion differ substantially between patients treated with axi-cel and those treated with either tisa-cel or liso-cel, and these differences are important to patients, payers, physicians, hospitals, and other stakeholders who are interested in understanding treatment benefit within a more relevant context.
To the best of our knowledge, this model uses the largest real-world data set, supplemented by trial data, for CAR T cell patients with R/R LBLC to address which CAR T cell therapy is most cost-effective. Safety and efficacy input values were derived from clinical trial data, where they can be expected to have been measured with low measurement error, while most utilization input values came from claims data, where resources were included from all sites of care, at transaction prices, for a large and likely more representative patient population, with the expectation of greater external validity. Nevertheless, certain limitations need to be considered. First, claims data may not be the ideal source for identifying adverse events, because severity grade is not directly specified on claims, and an algorithm developed with expert clinical input was applied to approximate grade in the AAPC analysis. The fact that most claims did not specify the CAR T cell therapy used precluded stratifying by therapy. Data limitations meant that the relationship between CRS and NE incidence and site of care had to be derived from the data rather than obtained directly. Survival data for each CAR T cell therapy were derived from different sources. While MAIC was used to mitigate underlying differences in patient samples across the source trial data, meaningful differences in measured or unmeasured characteristics may remain. However, the MAICs ensured that key prognostic factors were balanced. In general, lack of real-world data necessitated reliance on clinical trial data for many model input values, including PFS, OS, CRS and NE rates, and shares of patients receiving bridging therapy following apheresis but before CAR T cell administration. Trial data may lack external validity in some contexts. The actual experiences of patients when receiving treatment outside the trial setting may be different than the trial-based input values, but real-world data are not yet available that could explore such a difference. In addition, the OS and PFS model inputs reflect expectations for the average patient, using data from the overall samples in the underlying studies. The model is not a microsimulation, wherein individual patient characteristics could affect expected OS and PFS outcomes. Rather, the goal of the project was to compare CAR T cell therapies on average in the population for which they are indicated, as in most cost-effectiveness analyses. Finally, standard of care has evolved since the trials were conducted, and bendamustine may now be less frequently given for lymphodeletion.
Conclusion
This model showed that axi-cel was more cost-effective for patients with R/R LBCL compared to liso-cel and tisa-cel. These results held regardless of site of care for the initial CAR T cell therapy. This model provides important new evidence on the health benefits and costs of approved CAR T cell therapies over expected lifetimes of patients with LBCL.
Notes
“Base case” refers to the set of input values used in model calculations which collectively return the expected value(s) of model outcome measures for the target population of interest. It is distinguished from “scenarios” and “sensitivity analyses” which use alternative values for one or more model input parameters for the purpose of evaluating uncertainty in model results, exploring the effects of potential changes in treatment protocols, and/or studying particular subgroups of the overall target population.
References
YESCARTA® (axicabtagene ciloleucel) [package insert on the Internet]. Kite Pharma, Inc. U.S. Food and Drug Administration website. https://www.accessdata.fda.gov/spl/data/45e1bf54-5158-4fe4-b999-151539f23ed3/45e1bf54-5158-4fe4-b999-151539f23ed3.xml. Accessed 7 Mar 2022.
BREYANZI® (lisocabtagene maraleucel) [package insert on the Internet]. Juno Therapeutics, Inc. U.S. Food and Drug Administration website. https://www.accessdata.fda.gov/spl/data/a8e3c3f1-900a-488c-91a2-aa67e76e825f/a8e3c3f1-900a-488c-91a2-aa67e76e825f.xml. Accessed 22 Mar 2021.
KYMRIAH® (tisagenlecleucel) [package insert on the Internet]. Novartis Pharmaceuticals Corporation. U.S. Food and Drug Administration website. https://www.accessdata.fda.gov/spl/data/998538b0-e70b-4a9c-9e31-3ecd1cac27a2/998538b0-e70b-4a9c-9e31-3ecd1cac27a2.xml. Accessed 7 Mar 2022.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: B-Cell Lymphomas. 3.2021 ed2021.
Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377(26):2531–44.
Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254):839–52.
Schuster SJ, Bishop MR, Tam CS, et al. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2019;380(1):45–56.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Management of Immunotherapy-Related Toxicities. 1.2021 ed2021.
Hirayama AV, Turtle CJ. Toxicities of CD19 CAR-T cell immunotherapy. Am J Hematol. 2019;94(S1):S42–9.
Liu R, Oluwole OO, Diakite I, Botteman MF, Snider JT, Locke FL. Cost effectiveness of axicabtagene ciloleucel versus tisagenlecleucel for adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy in the United States. J Med Econ. 2021;24(1):458–68.
Oluwole OO, Liu R, Diakite I, et al. Cost-effectiveness of axicabtagene ciloleucel versus lisocabtagene maraleucel for adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy in the US. J Med Econ. 2022;25(1):541–51.
Micromedex Red Book Online Search. Truven Health Analytics. 2021. http://www.micromedexsolutions.com. Accessed 16 Nov 2021.
Tisagenlecleucel for diffuse large B-cell lymphoma: economic review report. Ottawa: CADTH; 2019;8(3e):1–68.
Locke FL, Ghobadi A, Jacobson CA, et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1–2 trial. Lancet Oncol. 2019;20(1):31–42.
Abramson JS, Siddiqi T, Garcia J, et al. Cytokine release syndrome and neurological event costs in lisocabtagene maraleucel-treated patients in the TRANSCEND NHL 001 trial. Blood Adv. 2021;5(6):1695–705.
Maziarz RT, Schuster SJ, Romanov VV, et al. Grading of neurotoxicity in patients with relapsed or refractory diffuse large B-cell lymphoma (r/r DLBCL) receiving tisagenlecleucel treatment in the JULIET study. Blood. 2018;132(Supplement 1):4183.
Schuster SJ, Maziarz RT, Ericson SG, et al. Consensus grading of cytokine release syndrome (CRS) in adult patients with relapsed or refractory diffuse large B-cell lymphoma (r/r DLBCL) treated with tisagenlecleucel on the JULIET Study. Blood. 2018;132(Supplement 1):4190.
Palomba ML, Jun MP, Lymp J, et al. Postinfusion monitoring costs by site of care for patients with relapsed/refractory large B-cell lymphoma receiving third- or later-line treatment with lisocabtagene maraleucel in the TRANSCEND NHL 001 and OUTREACH trials. Leuk Lymphoma. 2021;62(9):2169–76.
Centers for Medicare & Medicaid Services. CY 2021 Physician Fee Schedule Final Rule. Physician Fee Schedule. 2021.
Broder MS, Quock TP, Chang E, et al. The cost of hematopoietic stem-cell transplantation in the United States. Am Health Drug Benefits. 2017;10(7):366–74.
Lin JK, Muffly LS, Spinner MA, Barnes JI, Owens DK, Goldhaber-Fiebert JD. Cost effectiveness of chimeric antigen receptor T-cell therapy in multiply relapsed or refractory adult large B-cell lymphoma. J Clin Oncol. 2019;37(24):2105–19.
Gershengorn HB, Garland A, Gong MN. Patterns of daily costs differ for medical and surgical intensive care unit patients. Ann Am Thorac Soc. 2015;12(12):1831–6.
Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS). Rockville, MD: Agency for Healthcare Research and Quality; 2021. HCUP Fast Stats National Trends in Inpatient Stays, 1994–2018. http://hcupnet.ahrq.gov. Accessed 24 Nov 2021.
United States Bureau of Labor Statistics. Consumer Price Index for All Urban Consumers: Medical Care (CUSR0000SAM). United States Bureau of Labor Statistics; 2021. https://www.bls.gov/data/. Accessed 21 June 2021.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
Chen Q, Staton AD, Ayer T, Goldstein DA, Koff JL, Flowers CR. Exploring the potential cost-effectiveness of precision medicine treatment strategies for diffuse large B-cell lymphoma. Leuk Lymphoma. 2018;59(7):1700–9.
Lin VW JY, Chuang LH, Navale L, Cheng P, Purdum A. Health utilities for patients with relapsed or refractory large B-cell lymphoma (R/R-LBCL): ad hoc analysis from an Axicabtagene Ciloleucel (Axi-cel) Safety Management Study. Poster session presented at The 44th Annual Meeting of the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant. 2019;53(1):878–87.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness–the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–7.
Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making. 1998;18(2 Suppl):S68-80.
Topp MS, van Meerten T, Houot R, et al. Earlier corticosteroid use for adverse event management in patients receiving axicabtagene ciloleucel for large B-cell lymphoma. Br J Haematol. 2021;195(3):388–98.
Oluwole OO, Bouabdallah K, Muñoz J, et al. Prophylactic corticosteroid use in patients receiving axicabtagene ciloleucel for large B-cell lymphoma. Br J Haematol. 2021;194(4):690–700.
Lyman GH, Nguyen A, Snyder S, Gitlin M, Chung KC. Economic evaluation of chimeric antigen receptor T-cell therapy by site of care among patients with relapsed or refractory large B-cell lymphoma. JAMA Netw Open. 2020;3(4): e202072.
Sloan FA. Quality and cost of care by hospital teaching status: what are the differences? Milbank Q. 2021;99(1):273–327.
Oluwole O, Chen J, Chan K, et al. Poster: ABCL-289: matching-adjusted indirect comparison (MAIC) of axicabtagene ciloleucel (Axi-Cel) and lisocabtagene maraleucel (Liso-Cel) in relapsed or refractory (R/R) large B-cell lymphoma (LBCL) after two or more prior lines of therapy. Clin Lymphoma Myeloma Leuk. 2021;21:S241.
Oluwole OO, Jansen JP, Lin VW, et al. Comparing efficacy, safety, and preinfusion period of axicabtagene ciloleucel versus tisagenlecleucel in relapsed/refractory large B cell lymphoma. Biol Blood Marrow Transplant. 2020;26(9):1581–8.
Parker C, Liu FF, Deger K, et al. Cost-Effectiveness of lisocabtagene maraleucel (liso-cel) versus axicabtagene ciloleucel (axi-cel) for treatment of relapsed or refractory (R/R) large B-cell lymphoma (LBCL). Blood. 2021;138:3003.
Westin JR, Kersten MJ, Salles G, et al. Efficacy and safety of CD19-directed CAR-T cell therapies in patients with relapsed/refractory aggressive B-cell lymphomas: observations from the JULIET, ZUMA-1, and TRANSCEND trials. Am J Hematol. 2021;96(10):1295–312.
Lee DW, Gardner R, Porter DL, et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124(2):188–95.
Acknowledgements
Funding
This study and the journal's Rapid Service and Open Access Fees were funded by Kite, A Gilead Company, Santa Monica, California, USA.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. The working model was constructed and tested by Alice Kate Cummings Joyner, Si-Tien Wang, Marric Buessing, and Scott Johnson. Usama Gergis provided expert clinical guidance. The first draft of the manuscript was written by Scott Johnson and Alice Kate Cummings Joyner, and all authors commented on versions of the manuscript prior to the final one. All authors read and approved the final manuscript.
Previous Presentation
Results of this study have not been previously presented. However, a subset was presented in a poster presentation at ISPOR 2022 in Washington, DC, USA, May 15–18, 2022.
Disclosures
Alice Kate Cummings Joyner, Si-Tien Wang, Marric Buessing, and Scott Johnson are all employees of Medicus Economics which received funding from Kite to conduct this study. Julia Thornton Snider is an employee of Kite, a Gilead company and holds Gilead stock. Sally West Wade is a partner in Wade Outcomes Research and Consulting and has received consulting fees from Abbvie, Amgen, Johnson & Johnson, and Kite, a Gilead Company. Usama Gergis is employed by Thomas Jefferson University and has received consulting fees from Jazz, Gamida, Mesoblast, Incyte, and Kite, a Gilead Company. He also has participated in the Speakers’ Bureau for Jazz, Astellas, Incyte, and Kite, and holds stock in Iovance, Pfizer, Moderna, and Gamida.
Compliance with Ethics Guidelines
This study is based on published data and data derived from retrospective analysis of an existing HIPAA-compliant database and does not contain any individual patient data.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or directly analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cummings Joyner, A.K., Snider, J.T., Wade, S.W. et al. Cost-Effectiveness of Chimeric Antigen Receptor T Cell Therapy in Patients with Relapsed or Refractory Large B Cell Lymphoma: No Impact of Site of Care. Adv Ther 39, 3560–3577 (2022). https://doi.org/10.1007/s12325-022-02188-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02188-0