Abstract
Objectives
Necroptosis, a programmed inflammatory cell death, is involved in the pathogenesis of acute pancreatitis (AP). We compared levels of interleukin (IL)-33 (released upon necroptosis), sST2 (soluble IL-33 receptor), MLKL, RIPK1 and RIPK3 (necroptosis executioner proteins), and proinflammatory cytokines IL-6, TNF and IL-1β at various severity categories and stages of AP.
Methods
Plasma from 20 patients with early mild AP (MAP) (symptom onset < 72 h), 7 with severe AP (SAP) without and 4 with persistent organ failure (OF) at sampling, 8 patients with late SAP and 20 healthy controls (HC) were studied by ELISAs.
Results
Early sST2 and IL-6 levels predicted the development of SAP and were higher in both MAP and early and late SAP than in HC. RIPK3 levels were higher than in HC in the patients who had or would later have SAP. MLKL levels were associated with the presence of OFs, particularly in the late phase, but were also higher in MAP than in HC.
Conclusions
sST2, RIPK3 and IL-6 levels may have prognostic value in AP. Elevated MLKL levels are associated with OF in AP. Better understanding of necroptosis in AP pathophysiology is needed to evaluate whether inhibiting and targeting necroptosis is a potential therapeutic option in AP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute pancreatitis (AP) is commonly caused by gallstones or excessive alcohol use. Pancreatic acinar cell death is the major pathophysiological change in the early phase of AP. About 20–30% of patients develop severe acute pancreatitis (SAP) with substantial necrosis of acinar cells, leading to profound local necroinflammation in the pancreas and potentially systemic inflammation and organ failure (OF) with high mortality [1, 2]. Early recognition of the development of SAP and lack of specific treatments are the main challenges in managing AP [3]. Infection of the pancreas and peripancreatic necrosis occur in about 29% of patients with SAP, exacerbating OF [4].
Programmed necrosis, necroptosis, is a caspase-independent, inflammatory cell death pathway triggered by binding of immune ligands such as tumor necrosis factor (TNF) to their cell-surface receptors. Subsequently, receptor-interacting protein kinase 1 (RIPK1) binds to RIPK3 in the cytosol to form the so-called necrosome, from which the signal is mediated to mixed lineage kinase domain-like protein (MLKL). MLKL translocate to the plasma membrane, inducing necroptosis. Membrane permeabilization and leakage of cytoplasmic contents result in release of danger-associated molecular patterns (DAMPs) that act as alarmins to induce inflammation, alert the immune system, and promote the initiation of healing processes [5].
Interestingly, results from animal models strongly suggest that necroptosis plays a significant role in the pathogenesis of AP. It is the predominant mode of acinar cell death, and RIPK3 or MLKL knockdown has been protective against SAP in cerulein-induced AP in mice [6,7,8]. Recently, it has also been observed that circulating levels of RIPKs and MLKL can reflect the activity or severity of diseases in which cells in the affected organ undergo necroptosis, e.g. coronary artery disease, liver failure in patients with hepatitis B, and nonalcoholic fatty liver disease [9,10,11]. Also, necroptosis is involved in the pathology of OF [12], and plasma RIPK3 levels are associated with mortality and OF in patients with sepsis and septic shock [13], and with acute kidney injury stage in critically ill patients after trauma [14]. Elevated serum MLKL concentrations have been described as an independent negative predictor of survival among patients in intensive care [15].
Interleukin-33 (IL-33) is expressed in normal pancreatic acinar cells [16]. It regulates genes for proinflammatory signaling [17] and is released during necrosis and necroptosis [5]. In animal models, IL-33 induces acute inflammation [18], but the binding to its cell-surface receptor (serum stimulation-2 [ST2]) also promotes survival and proliferation of cells with anti-inflammatory properties [5]. Soluble ST2 (sST2) levels have been found to be higher in patients who develop necrotizing pancreatitis than in those with edematous AP [19]. The definite role of the IL-33/sST2 axis in AP remains unclear.
Novel associations and correlations between classical proinflammatory and necroptotic markers have been discovered recently. In AP, the proinflammatory TNF and IL-1β are key mediators in initiating acinar cell injury. They also induce the production of IL-6 in various cell types. IL-6, in turn, induces the synthesis of acute phase proteins, e.g., C-reactive protein, in the liver, thus crucially facilitating the development of systemic inflammation [20, 21]. sST2 production has been shown to be enhanced by IL-1β and TNF in human lung epithelial cells and cardiac myocytes and by IL-33 in mast cells [22]. Inhibition of necroptosis attenuated lung injury, decreased serum levels of IL-6 and IL-1β and improved survival in newborn mice with induced sepsis [23], and similar results were obtained by RIPK3 deficiency [24] suggesting that necroptosis participates in the systemic inflammatory response at least in sepsis. Furthermore, according to a mouse model, endothelial necroptosis may be an underlying mechanism for TNF-induced tissue damage in systemic inflammatory response syndrome [25].
Necroptosis may provide novel biomarkers for prognosis and monitoring of AP. Necroptosis is potentially reversible with the help of specific inhibitors [6, 26, 27], and the ability to regulate acinar cell necrosis may be a potentially effective measure to prevent the progression of AP [2]. Future treatment options for AP may include targeting necroptosis. This requires that the necroptotic phase in the course of AP can be identified.
The primary objective of this pilot study was to determine plasma concentrations of IL-33, sST2, RIPK1, RIPK3, and MLKL, which have seldom been analyzed in human studies, in parallel with the better-known inflammatory cytokines TNF, IL-1β and IL-6, to find associations with disease severity and development of OF in patients with AP.
Materials and Methods
Subjects
This pilot study includes patients with AP enrolled at the emergency department and the intensive care unit (ICU) at Helsinki University Hospital between December 2013 and February 2020. The study was approved by the Surgical Ethics Review Board (Joint Authority of the Helsinki and Uusimaa Hospital District). Informed consent was obtained from each patient or next of kin. All patients were 18 years or older.
AP was diagnosed and the severity of AP was assessed according to the revised Atlanta classification and fulfilled two out of three criteria: (1) symptoms typical to AP, (2) plasma amylase levels more than three times the normal upper limit, and (3) findings typical to AP in computed tomography. Patients with mild AP (MAP) had neither local nor systemic complications. Patients with SAP had persistent OF lasting over 48 h or complications [1]. The severity of OF was assessed using the Modified Marshall Score (MMS) [28]. Patients with chronic pancreatitis, known malignancy, or three or more previous AP episodes were excluded from the study.
Patient Groups
Plasma samples were available for 11 patients with SAP from our previous study [29]. The symptoms had started less than 48 h before admission, and samples were collected less than 72 h from symptom onset. These patients are referred to as the “early SAP” group. Four of the patients with SAP had OF already at the time of blood sampling, while 7 SAP patients were sampled prior to the occurrence of OF. The “early SAP” group is divided into the two subgroups of no OF at time of sampling (SAPOF−) and OF at time of sampling (SAPOF+).
In addition, eight patients with severe AP who were treated at the ICU for multiorgan failure were recruited. Blood samples were collected approximately 1 week after symptom onset, and this group is referred to as “late SAP” (LSAP).
For the purposes of this pilot study, we compared the 19 SAP patients available with 20 MAP patients and 20 healthy controls (HC). The samples were selected randomly from the 119 MAP patients and 32 HC in our previous study [29] using the corresponding function of the statistical program. Patients with moderately severe AP were deliberately omitted from this pilot study. The patient groups are visualized in Fig. 1.
Plasma Samples and Measurements
An 8-ml blood sample was obtained in an ACD (acid citric dextrose) tube by venipuncture, and plasma was separated by centrifugation within 2 h and frozen at – 80 °C until the marker determinations. Plasma levels of necroptosis markers and cytokines were detected using commercial ELISA kits as follows: LEGEND MAX™ for IL-33 from BioLegend (San Diego, CA, USA), OKAG00248 for sST2, OKCD00436 for RIPK1, OKCA02138 for RIPK3 and OKEH03401 for MLKL from Aviva Systems Biology (San Diego, CA, USA), and Quantikine DLB50 for IL-1β, D6050 for IL-6 from B&D systems (Minneapolis, MN, USA) and DTA00D for TNF from BioTechne (Dublin, Ireland). Any measurements falling below the lowest standard concentration (shown in Fig. 2) were analyzed as having half the lowest standard concentration. The intra-assay coefficients of variation reported by the manufacturers of the ELISA kits: IL-33 ≤ 5.6, sST2: ≤ 8.2, RIPK3: ≤ 8, RIPK1: < 10, MLKL: ≤ 4.8 and IL-6: ≤ 4.2.
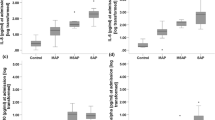
Plasma levels of necroptosis markers A sST2, B IL-33, C RIPK1, D RIPK3, and E MLKL, and proinflammatory cytokines, F IL-1 beta, G IL-6, and H TNF in control subjects (controls, n = 20), and patients with mild acute pancreatitis (MAP, n = 20). Severe acute pancreatitis was sampled prior to the occurrence of organ failure [(SAPOF−), n = 7] or after manifested organ failure [(SAPOF+), n = 4], or late severe acute pancreatitis [(SAPL), n = 8)]. Groups were compared by Kruskal–Wallis test, and statistically significant post hoc p-values by Mann–Whitney test are shown. Circles denote results of individual subjects, boxes denote 25th to 75th percentiles of groups, and horizontal bars inside boxes denote group medians. The lowest standard concentration is shown as a dashed line, and measured values below that are set to half of the lowest standard concentration. Note logarithmic scales in panels A, C and E–H
Statistics
The results are shown as medians with interquartile ranges. Continuous variables were compared between groups using Kruskal–Wallis test with post hoc p-values calculated using Mann–Whitney U test. Spearman correlation coefficients were computed with bootstrapped 95% confidence intervals. p-values of less than 0.05 were considered significant; two-tailed tests were used. No correction was made for multiple testing. Statistical analysis was carried out using SPSS, version 27 (IBM, Armonk, NY, USA).
Results
The characteristics of the patients are shown in Table 1.
Plasma Markers and AP Severity
sST2
Plasma levels of sST2 were significantly higher in early SAP than in early MAP, and the highest levels were seen in SAPOF+, as shown in Fig. 2A. sST2 levels in LSAP did not significantly differ from those in MAP or early SAP. sST2 levels in HC were significantly lower than in any of the patient groups.
IL-33
IL-33 levels did not significantly differ between any of the groups, as shown in Fig. 2B.
RIPK1 and RIPK3
RIPK1 levels in most samples were below the lowest standard concentration of the ELISA kit (0.156 ng/ml) and did not significantly differ between any of the groups, as shown in Fig. 2C.
RIPK3 levels were significantly higher in SAPs than in HC, as shown in Fig. 2D. The levels in MAP did not significantly differ from HC or SAPs.
MLKL
MLKL levels in LSAP were higher than in SAPOF− or in MAP, whereas the levels between SAPOF+ and LSAP did not show a statistically significant difference, as seen in Fig. 2E. The MLKL levels of HC were lower than in MAP and SAPs.
IL-1β
IL-1β levels in SAPOF− were higher than in HC or in MAP, and levels in LSAP were higher than in HC, as seen in Fig. 2F. All HC and all but one MAP samples had concentrations below the lowest standard concentration, as did several SAP samples.
IL-6
IL-6 levels in all AP patient groups were higher than in HC, where all samples were below the lowest standard concentration, as shown in Fig. 2G. Both early SAP groups were also higher than MAP.
TNF
TNF levels were mostly below the lowest standard concentration and did not significantly differ between any of the groups, as shown in Fig. 2H.
Correlations with Disease Severity Scores, Routine Laboratory Measurements and Cytokine Levels
The levels of all plasma necroptosis markers positively correlated with APACHEII and/or SOFA score evaluated at the time of blood sampling, as shown in Fig. 3. These correlations were statistically significant, except for the correlation between RIPK3 and APACHEII. RIPK3 had a positive correlation with CRP and leukocyte count, as shown in Table 2.
Correlations of plasma levels of necroptosis markers sST2, IL-33, RIPK3, and MLKL with APACHEII and SOFA scores in all patients with acute pancreatitis (n = 39). Spearman correlation coefficients with 95% confidence intervals (CIs) and associated p-values are shown within figure panels. Fit lines are shown with 95% CI denoted by dotted line
sST2 had a positive correlation with IL-1β and IL-6, as shown in Table 2. APACHE II score had a positive correlation with TNF (r = 0.35, 95% CI 0.015 to 0.62; p = 0.031), and SOFA score had a positive correlation with IL-1β (r = 0.55, 95% CI 0.32 to 0.71; p < 0.001), IL-6 (r = 0.59, 95% CI 0.37 to 0.76; p < 0.001), and TNF (r = 0.43, 95% CI 0.13 to 0.68; p = 0.007).
Discussion
We studied the necroptosis-related plasma markers MLKL, RIPK1, RIPK3, IL-33, and sST2 and the proinflammatory cytokines IL-6, TNF, and IL-1β with respect to the severity of acute pancreatitis (AP) in the early and late phase of the disease (< 72 h and 1 week from onset of symptoms, respectively). The results show that early sST2 and IL-6 levels predicted the development of severe AP (SAP) and were higher in both mild AP (MAP) and early and late severe AP (SAP) than in healthy controls (HC). RIPK3 levels were higher than in HC in the patients who had or would later have SAP. Further, MLKL levels were associated with the presence of organ failure (OF), particularly in the late phase, but were also higher in MAP than in HC. MLKL, RIPK3, IL-33, sST2, IL-6, TNF, and IL-1β levels were associated with at least one of the severity scores studied (APACHEII and SOFA).
sST2 and IL-33
Our finding that the levels of the IL-33 decoy receptor sST2 are associated with the development of SAP is in agreement with previously described associations between sST2 and diseases with a marked tissue damage component such as sepsis and heart failure [17, 30, 31]. In our results, sST2 levels also correlated with both disease severity scores determined, and furthermore, with hemoglobin and hematocrit, which may suggest a failure in vascular permeability. Apparently, one crucial mechanism behind the disadvantageous effects of sST2 is that by binding to IL-33 it prevents the effects mediated via the cell-surface IL-33 receptor ST2, e.g., survival and proliferation of basophils, mast cells, Tregs, and Th2 cells and secretion of Th2 cytokines (IL-4, IL-5, IL-10, IL-13). When the release of anti-inflammatory cytokines is reduced, the response is modulated in the direction of Th1 activation, including release of proinflammatory cytokines [5].
In one of the few studies conducted on sST2 in AP, the levels of sST2 were increased early during AP, correlated with parameters of severity, and decreased to near-normal range 30 days after the acute episode [19]. This seems to be in line with our current findings regarding the kinetics, as the sST2 levels were somewhat lower in late SAP than in early SAP, although not (yet) reaching the levels of HC. Interestingly, the sST2 levels of patients with early MAP were lower than in those with early SAP with persistent OF but also lower than in those who developed persistent OF only after sampling. Hence, sST2 appears to be a candidate for an early predictor of AP severity.
IL-33 levels showed broad variation among both AP patients and HC, and the levels of the patients did not significantly differ from those of HC. Considering that IL-33 is mainly produced in cells exposed to the environment, such as epithelial and endothelial cells, the possibility remains that it is continuously released by minimal surface damage, low-level inflammation, or low-level necroptosis/necrosis for various reasons also in healthy individuals. Moreover, it is noteworthy that IL-33 has been reported to be upregulated in the tumor microenvironment of pancreatic adenocarcinoma and lesions from chronic pancreatitis [32, 33]. Hence, systemic IL-33 levels in these diseases may also be more prominent than in AP.
Proinflammatory Cytokines
Interestingly, IL-6 and sST2 showed a similar pattern according to AP severity so that plasma level of either of these, determined < 72 h of symptom onset, was significantly lower in HC and MAP than in early SAP even when OF developed after blood sampling in patients with SAP. The potential of IL-6 as an early predictor of OF is well known, but the IL-6 assay has been considered expensive and complex for routine clinical practice [20]. However, nowadays an automated, rapid assay is available and has been studied for predicting complications in AP [34]. Our results also show that both IL-6 and sST2 peak in early SAP and tend to decrease towards late SAP, further emphasizing the potential of these markers in the early phase of AP. Further research aiming at developing more fluent clinical use of IL-6 and sST2 determination in the early phase of AP seems to be a rational approach for managing the disease.
Levels of sST2 were strongly correlated to those of IL-6 and IL-1β. Correlation between sST2 and IL-6 levels has been described recently in metabolic syndrome, and high circulating sST2 levels can be seen to mirror high inflammatory burden [35]. In different cell types, sST2 has been observed to enhance the secretion of IL-6 and IL-1β [36] but also to be produced in response to these [22]. Unfortunately, owing to the generally low levels of IL-1β and especially TNF in the current study, interpretation of the results concerning them is dubious.
RIPK1 and RIPK3
We observed that, as compared with HC, plasma RIPK3 levels were higher in late and early SAP also in those patients with early SAP who did not yet have persistent OF at blood sampling. The levels in MAP were a bit lower than in SAP, but the difference did not reach statistical significance. Hence, whether a significant difference between RIPK3 levels in early MAP and early SAP would emerge in larger studies, i.e., whether RIPK3 levels possess prognostic value in AP, remains to be elucidated. Recently, summarized results from several cohorts showed that RIPK3 levels in the plasma of patients admitted to intensive care for sepsis or septic shock are associated with in-hospital mortality and OF [13]. RIPK3 concentrations have also been found to be associated with the stage of acute kidney injury among critically ill trauma patients [14]. Furthermore, transcriptome analysis of leukocytes of patients with community-acquired pneumonia in intensive care revealed that higher mortality was associated with a subgroup of patients with high expression of RIPK3 (and other genes) [37]. These findings agree with our RIPK3 results, allowing us to conclude that high systemic RIPK3 levels represent a nonspecific sign of disease severity in several critical illnesses.
RIPK1 levels fell below the smallest standard concentration in almost all samples studied. Unfortunately, and for reasons unknown to us, the manufacturer changed the range of the RIPK1 ELISA kit from 15.6–1000 pg/ml (comparable to that of RIPK3 kit) to 0.156–10 ng/ml after our order was already placed. Therefore, it is not possible to make conclusions about the biomarker potential of plasma RIPK1 based on the current study, and reassessment with a more sensitive assay remains a topic for further research.
MLKL
Plasma MLKL levels were associated with the presence of OF and were at their highest in late SAP. The result is parallel to the finding that serum MLKL correlates with surrogate markers of OF such as serum lactate levels [15]. Our results also reinforce the view obtained from an animal model that OF, or multiple organ dysfunction syndrome, is characterized by necroptosis rather than apoptosis [12]. As the MLKL levels in MAP and early SAP before the development of persistent OF were very similar in our results, it seems unlikely that MLKL could serve as a marker predicting AP severity. It is also noteworthy that MLKL levels in early MAP were slightly but nevertheless significantly higher than in HC, which may reflect ongoing necroptosis in the pancreas also in the mild disease form.
To interpret the differences between the results concerning RIPK3 and MLKL, it should be noted that RIPK3 acts on other pathways besides necroptosis. RIPK3 can promote caspase-8-dependent apoptosis independent of its kinase function. Also, RIPK3 is a cell type-specific NF-κB activator, and it functions in mitochondrial production of reactive oxygen species, inflammasome activation, and subsequent release of IL-1β [38]. Hence, it can be expected that high systemic RIPK3 levels reflect a vigorous proinflammatory phase of systemic inflammation, whereas MLKL, as the terminal mediator of necroptosis, confirms the occurrence of necroptosis.
Importantly, in a rodent model of SAP, inhibition of necroptosis with the RIPK1-specific inhibitor necrostatin-1 (Nec-1) could reduce disease severity even when administrated after the establishment of SAP, thus making necroptosis a potential therapeutic target in AP [6]. Also, inhibition of necroptosis using the MLKL inhibitor necrosulfonamide (NSA) has been reported to alleviate, for instance, lung ischemia–reperfusion injury in mice [27]. In view of necrotizing pancreatitis being associated with increased sST2 levels [19] and infection of necrotized pancreas being quite common [4], it is also notable that IL-33 promotes neutrophil migration to the infectious site, which is crucial for host defence. For example, septic mice that were given an IL-33 injection showed significantly reduced mortality [30]. However, chronic pancreatitis has recently been described as an IL-33-dependent inflammation [33]. Hence, it is dubious whether targeting the IL-33/sST2 axis could be as promising as necroptosis inhibition as a future treatment option for AP.
Intravenous fluid resuscitation is the cornerstone of therapy strategies for SAP, but it is probable that aggressive fluid resuscitation (AFR) will aggravate other organ injuries while rapidly correcting the shock state. Interestingly, a recent study on rats showed that Nec-1, when administered before AFR, could reduce iatrogenic gut injuries, suggesting that necroptosis is an important mechanism in AFR-related intestinal barrier injury [39]. NSA was also able to protect against damage of intestinal epithelial cells in a mouse model [26]. Based on these results, it is conceivable that inhibiting necroptosis would be advantageous not only for reducing AP severity but also for counteracting treatment-associated damage.
Limitations of the Study
The present study was designed as a pilot study to test the feasibility of measuring circulating necroptosis markers in AP. Thus, the number of samples studied was relatively low in order to limit cost. Also, patients with severe AP are overrepresented as only a random sample of mild AP patients was included and those with moderately severe AP were totally omitted. Thus, the results should be considered preliminary as they are hampered by low sample size and distribution of AP severity not completely representing the clinical setting. The findings need to be validated in a larger cohort of AP patients. This would also allow analysis of necroptosis markers with respect to a more diverse array of clinical outcomes, such as mortality, pancreatic necrosis, and other complications.
Another limitation is that the levels of TNF and IL-1β turned out to be very low in the majority of samples making their interpretation difficult. This, however, emphasizes that as these crucial proinflammatory mediators are unsteady and purged rapidly from the circulation, novel and more suitable prognostic biomarkers are needed. Also, among limitations is that the study setting did not allow tracing the origin of the necroptosis-related plasma markers. However, in a mouse model of AP, dramatic increase in MLKL expression was observed specifically in the pancreas [7]. Furthermore, accumulating evidence suggest that RIPK and MLKL levels in the blood reflect the severity or activity of diseases in which pathogenetic necroptosis takes place in the affected organ [9,10,11]. As yet another limitation, we recognize that drawing direct conclusions about necroptosis inhibition as a near-future treatment option in AP and the related OF is premature. Instead, much research is required for defining the ultimate cell type- and tissue-specific effects and outcomes associated with necroptosis inhibitors, as well as effective and safe dosage and timing of inhibitor administration.
Conclusions
To conclude, the results of this pilot study show that plasma levels of sST2, the soluble receptor of the necroptotic alarmin IL-33, and the inflammatory cytokine IL-6, are able to predict the development of SAP. Levels of RIPK3, a kinase with necroptotic and non-necroptotic inflammatory functions, appear to be associated with SAP. Elevated levels of the necroptosis executor MLKL are seen in MAP patients and even more prominently in patients with persistent OF. While still requiring more research, the results support the idea that reversing necroptosis may be an appealing option to optimize AP treatment.
Data availability
No datasets were generated or analyzed during the current study.
References
Banks PA, Bollen TL, Dervenis C et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. https://doi.org/10.1136/gutjnl-2012-302779.
Wang G, Qu FZ, Li L, Lv JC, Sun B. Necroptosis: a potential, promising target and switch in acute pancreatitis. Apoptosis. 2016;21:121–129. https://doi.org/10.1007/s10495-015-1192-3.
Kylänpää ML, Repo H, Puolakkainen PA. Inflammation and immunosuppression in severe acute pancreatitis. World J Gastroenterol. 2010;16:2867–2872. https://doi.org/10.3748/wjg.v16.i23.2867.
Husu HL, Valkonen MM, Leppäniemi AK, Mentula PJ. Occurrence and Risk Factors of Infected Pancreatic Necrosis in Intensive Care Unit-Treated Patients with Necrotizing Severe Acute Pancreatitis. J Gastrointest Surg. 2021;25:2289–2298. https://doi.org/10.1007/s11605-021-05033-x.
Shlomovitz I, Erlich Z, Speir M et al. Necroptosis directly induces the release of full-length biologically active IL-33 in vitro and in an inflammatory disease model. Febs j. 2019;286:507–522. https://doi.org/10.1111/febs.14738.
Louhimo J, Steer ML, Perides G. Necroptosis Is an Important Severity Determinant and Potential Therapeutic Target in Experimental Severe Pancreatitis. Cell Mol Gastroenterol Hepatol. 2016;2:519–535. https://doi.org/10.1016/j.jcmgh.2016.04.002.
He S, Wang L, Miao L et al. Receptor interacting protein kinase-3 determines cellular necrotic response to TNF-alpha. Cell. 2009;137:110011. https://doi.org/10.1016/j.cell.2009.05.021.
Wu J, Huang Z, Ren J et al. Mlkl knockout mice demonstrate the indispensable role of Mlkl in necroptosis. Cell Res. 2013;23:994–1006. https://doi.org/10.1038/cr.2013.91.
Hu XM, Chen X, Pang HY et al. Plasma levels of receptor interacing protein kinase-3 correlated with coronary artery disease. Chin Med J. 2019;132:1400–1405. https://doi.org/10.1097/CN9.0000000000000225.
Chen L, Cao Z, Yan L et al. Cisrculating receptor-intercting protein kinase 3 are increased in HBV patients with acute-on-chronic liver failure and are associated with clinical outcome. Front Physiol. 2020;11:526. https://doi.org/10.3389/fphys.2020.00526.
Majdi A, Aoudjehane L, Ratziu V et al. Inhibition of receptor-interacting protein kinase 1 improves experimental non-alcoholic fatty liver disease. J Hepatol. 2020;72:627–635. https://doi.org/10.1016/j.jhep.2019.11.008s.
Cui YL, Qiu LH, Zhou SY et al. Necroptosis as a potential therapeutic target in multiple organ dysfunction syndrome. Oncotarget. 2017;8:56980–56990. https://doi.org/10.18632/oncotarget.18252.
Ma KC, Schenck EJ, Siempos II et al. Circulating RIPK3 levels are associated with mortality and organ failure during critical illness. JCI Insight. 2018. https://doi.org/10.1172/jci.insight.99692.
Shashaty MG, Reilly JP, Sims CA et al. Plasma Levels of Receptor Interacting Protein Kinase-3 (RIP3), an Essential Mediator of Necroptosis, are Associated with Acute Kidney Injury in Critically Ill Trauma Patients. Shock. 2016;46:139–143. https://doi.org/10.1097/shk.0000000000000596.
Vucur M, Roderburg C, Kaiser L et al. Elevated Serum Levels of Mixed Lineage Kinase Domain-Like Protein Predict Survival of Patients during Intensive Care Unit Treatment. Dis Markers. 2018;2018:1983421. https://doi.org/10.1155/2018/1983421.
Masamune A, Watanabe T, Kikuta K, Satoh K, Kanno A, Shimosegawa T. Nuclear expression of interleukin-33 in pancreatic stellate cells. Am J Physiol Gastrointest Liver Physiol. 2010;299:G821–G832. https://doi.org/10.1152/ajpgi.00178.2010.
Homsak E, Gruson D. Soluble ST2: A complex and diverse role in several diseases. Clin Chim Acta. 2020;507:75–87. https://doi.org/10.1016/j.cca.2020.04.011.
Kempuraj D, Twait EC, Williard DE, Yuan Z, Meyerholz DK, Samuel I. The novel cytokine interleukin-33 activates acinar cell proinflammatory pathways and induces acute pancreatic inflammation in mice. PLoS One. 2013;8:e56866. https://doi.org/10.1371/journal.pone.0056866.
Ouziel R, Gustot T, Moreno C et al. The ST2 pathway is involved in acute pancreatitis: a translational study in humans and mice. Am J Pathol. 2012;180:2330–2339. https://doi.org/10.1016/j.ajpath.2012.03.009.
Meher S, Mishra TS, Sasmal PK et al. Role of biomarkers in diagnosis and prognostic evaluation of acuta pancreatitis. J Biomark. 2015;2015:519534. https://doi.org/10.1155/2015/519534.
Leser HG, Gross V, Scheibenbogen C et al. Elevation of serum interleukin-6 concentration precedes acute-phase response and reflects severity in acute pancreatitis. Gastroenterology. 1991;101:782–785. https://doi.org/10.1016/0016-5085(91)90539-w.
Griesenauer B, Paczesny S. The ST2/IL-33 axis in immune cels during inflammatory diseases. Front Immunol. 2017;8:475. https://doi.org/10.3389/fimmu.2017.00475.
Bolognese AC, Yang WL, Hansen LW et al. Inhibition of necroptosis attenuates injury and improves survival in neonatal sepsis. Surgery. 2018;S0039–6060:30096–30105. https://doi.org/10.1016/j.surg.2018.02.017.
Hansen LW, Jacob A, Yang WL et al. Deficiency of receptor-interacting protein kinase 3 (RIPK3) attenuates inflammation and organ injury in neonatal sepsis. J Pediatr Surg. 2018;53:1699–1705. https://doi.org/10.1016/jpedsurg.2017.11.054.
Zelic M, Roderick JE, O’Donnell JA et al. RIP kinase 1-dependent endothelial necroptosis underlies systemic inflammatory response syndrome. J Clin Invest. 2018;128:2064–2075. https://doi.org/10.1172/JCI96147.
Dong W, Zhang M, Zhu Y et al. Protective effect of NSA on intestinal epithelial cells in a necroptosis model. Oncotarget. 2017;8:86726–86735. https://doi.org/10.18632/oncotarget.21418.
Ueda S, Chen-Yoshikawa TF, Tanaka S et al. Protective effect of necrosulfonamide on rat pulmonary ischemia-reperfusion injury via inhibition of necroptosis. J Thorac Cardiovasc Surg. 2022;163:e113–e122. https://doi.org/10.1016/j.jtcvs.2021.01.037.
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638–1652. https://doi.org/10.1097/00003246-199510000-00007.
Turunen A, Kuuliala A, Mustonen H, Puolakkainen P, Kylänpää L, Kuuliala K. Blood Leukocyte Signaling Pathways as Predictors of Severity of Acute Pancreatitis. Pancreas 2021;50:710–718. https://doi.org/10.1097/mpa.0000000000001832.
Alves-Filho JC, Sônego F, Souto FO et al. Interleukin-33 attenuates sepsis by enhancing neutrophil influx to the site of infection. Nat Med. 2010;16:708–712. https://doi.org/10.1038/nm.2156.
Bayés-Genís A, Núñez J, Lupón J. Soluble ST2 for Prognosis and Monitoring in Heart Failure: The New Gold Standard? J Am Coll Cardiol. 2017;70:2389–2392. https://doi.org/10.1016/j.jacc.2017.09.031.
Schmieder A, Multhoff G, Radons J. Interleukin-33 acts as a pro-inflammatory cytokine and modulates its receptor gene expression in highly metastatic human pancreatic carcinoma cells. Cytokine. 2012;60:514–521. https://doi.org/10.1016/j.cyto.2012.06.286.
Watanabe T, Sadakane Y, Yagama N et al. Nucleotide-binding oligomerization domain 1 acts in concert with the cholecystokinin receptor agonist, cerulein, to induce IL-33-dependent chronic pancreatitis. Mucosal Immunol. 2016;9:1234–1249. https://doi.org/10.1038/mi.2015.144.
Kolber W, Dumnicka P, Maraj M et al. Doe s the automatic measurement of interleukin 6 allow for prediction of complications during the first 48 h of acute pancreatitis? Int J Mol Sci. 2018;19:1820. https://doi.org/10.3390/ijms19061820.
Roy I, Jover E, Matilla L et al. Soluble ST2 as a new oxidative stress and inflammation marker in metabolic syndrome. Int J Environ Res Public Health. 2023;20:2579. https://doi.org/10.3390/ijerph20032579.
Matilla L, Ibarrola J, Arrieta V et al. Soluble ST2 promotes oxidative stress and inflammation in cardiac fibroblasts: an in vitro and in vivo study in aortic stenosis. Clin Sci (Lond). 2019;133:1537–1548. https://doi.org/10.1042/CS0190475.
Davenport EE, Burnham KL, Radhakrishnan J et al. Genomic landscape of the individual host response and outcomes in sepsis: a prospective cohort study. Lancet Respir Med. 2016;4:259–271. https://doi.org/10.1016/s2213-2600(16)00046-1.
Moriwaki K, Chan FK. The Inflammatory Signal Adaptor RIPK3: Functions Beyond Necroptosis. Int Rev Cell Mol Biol. 2017;328:253–275. https://doi.org/10.1016/bs.ircmb.2016.08.007.
Cui QR, Ling YH, Wen SH et al. Gut Barrier Dysfunction Induced by Aggressive Fluid Resuscitation in Severe Acute Pancreatitis is Alleviated by Necroptosis Inhibition in Rats. Shock. 2019;52:e107–e116. https://doi.org/10.1097/shk.0000000000001304.
Acknowledgments
Antti Turunen, MD, PhD, is acknowledged for great help in data collection.
Funding
Open Access funding provided by University of Helsinki (including Helsinki University Central Hospital). Funding was provided by HUS Abdominal Center—University of Helsinki, Finska läkaresällskapet, The Mary and Georg Ehrnrooth Foundation.
Author information
Authors and Affiliations
Contributions
JL and KK conceived and planned the study. HB, LK, and JL collected the data. KK and AK performed the laboratory analysis. AK performed the statistical analysis. All authors participated in interpretation of the results. The manuscript was drafted by HB, KK, and AK. All authors critically revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Belfrage, H., Kuuliala, K., Kuuliala, A. et al. Circulating Markers of Necroptosis in Acute Pancreatitis. Dig Dis Sci (2024). https://doi.org/10.1007/s10620-024-08530-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10620-024-08530-6