Abstract
Objectives
In patients with unresectable malignant hilar biliary obstruction (UMHBO), drainage of ≥ 50% liver volume correlates with better clinical outcomes. Accurately measuring the liver volume to be drained by biliary stents is required. We aimed to develop a novel method for calculating the drained liver volume (DLV) using a 3D volume analyzer (3D volumetry), and assess the usefulness for drainage in patients with UMHBO.
Methods
Three-dimensional volumetry comprises the following steps: (1) manual tracing of bile duct using 3D imaging system; (2) 3D reconstruction of bile duct and liver parenchyma; and (3) calculating DLV according to the 3D distribution of bile ducts. Using 3D volumetry, we reviewed data of patients who underwent biliary drainage for UMHBO, calculated the DLV, and determined the association between DLV and biliary drainage outcome.
Results
There were 104 eligible cases. The mean DLV was 708 ± 393 ml (53% ± 21%). and 65 patients (63%) underwent drainage of ≥50% liver volume. The clinical success rate was significantly higher in patients with DLV ≥ 50% than in patients with DLV < 50% (89% vs. 28%, P < 0.001). The median time to recurrence of biliary obstruction (TRBO) and survival time were significantly longer in patients with DLV ≥ 50% than in patients with DLV < 50% (TRBO, 292 vs. 119 days, P = 0.03; survival, 285 vs. 65days, P = 0.004, log-rank test, respectively).
Conclusions
Three-dimensional volumetry, a novel method to calculate DLV accurately according to bile duct distribution was useful for drainage in UMHBO patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Effective drainage of obstructive jaundice is essential for improving the quality of life of patients with unresectable malignant hilar biliary obstruction (UMHBO). Over the past years, various procedure of biliary drainage for UMHBO have been performed: percutaneous or endoscopic route, plastic or metallic stents, and single or multiple stenting [1,2,3,4,5,6,7]. In the recent years, endoscopic biliary drainage is considered as first-line treatment for UMHBO. Furthermore, EUS-guided biliary drainage has emerged as a novel method for UMHBO [8, 9]. However, no consensus has been reached on the optimal drainage strategy for treating hilar biliary obstruction due to the anatomical complexity. In UMHBO, the bile ducts are separated into numerous cavities; thus, drainage of the entire liver is very difficult in cases of severe obstruction.
Drainage of > 50% liver volume is reported to be correlated with clinical success of biliary drainage and prolonged survival in patients with UMHBO [10, 11]. The European Society of Gastrointestinal Endoscopy (ESGE) guideline also suggests the above strategy [12]. The appropriate biliary drainage based on liver volume is important for clinical success and prolonged survival time. However, the method for accurately measuring the liver volume to be drained by biliary stents has not been established. Computed tomography (CT) volumetry is the only method for measuring drained liver volume (DLV) reported to date; however, CT volumetry measures the volume of the hepatic segment delimited by the liver veins and portal veins, not the bile duct, which may cause a mismatch with the actual liver volume to be drained from the bile duct. To measure the true DLV, the method for calculating liver volume according to the bile duct distribution is required.
A three-dimensional (3D) volume analyzer (The SYNAPSE VINCENT; Fujifilm) can display 3D images of the liver based on CT and magnetic resonance (MR) images. It also can extract the perfusion area of individual portal vein branches in the liver and can automatically calculate each liver volume according to the portal vein distribution. This method is used to calculate liver volume before liver resection and transplantation [13,14,15,16]. Using this method to manually extract the area of each bile duct in the liver, measuring for the true DLV according to the bile duct distribution could be possible. In this study, we aimed to develop a novel method of calculating DLV using a 3D volume analyzer (3D volumetry) and assess the usefulness for drainage in patients with UMHBO.
Methods
Patients
This single-center retrospective study reviewed data of patients who underwent a biliary drainage procedure for UMHBO between March 2004 and April 2022. The inclusion criteria were as follows: obstructive jaundice caused by UMHBO (Bismuth classification III and IV); abdominal CT scan performed within 2 weeks before drainage; and clinical biochemical tests performed before and 14 days after drainage. The exclusion criteria were as follows: cases of Bismuth classification I and II obstructions; or presence of UMHBO without jaundice before drainage, for which drainage was prophylactically performed. The cases of Bismuth classification I and II in which the drainage of total liver could be easily performed were excluded to assess the drainage of severe obstruction of UMHBO. This study was approved by the University of Yamanashi Hospital Institutional Review Board with approval number 2674.
3D Volumetry
We developed a novel method to calculate DLV (3D volumetry) using a 3D volume analyzer (The Synapse Vincent; Fujifilm). This method comprised the following steps: (1) transfer of CT images (axial view) to the 3D imaging system; (2) manual tracing of bile duct using CT images (Fig. 1a); (3) 3D reconstruction of bile duct and liver parenchyma (Fig. 1b); and (4) calculation of DLV by the biliary stents according to the 3D distribution of bile ducts (Fig. 1c). At least 2 gastroenterologists specialized in the bile ducts calculated DLV by using this method.
Three-dimensional (3D) volumetry for calculating drained liver volume. We used a 3D volume analyzer (The SYNAPSE VINCENT; Fujifilm) to calculate the drained liver volume. (a) Manual tracing of bile duct using CT images. (b) Three-dimensional reconstruction of the bile duct and liver parenchyma. (c) Calculation of DLV according to the 3D distribution of bile duct and Bismuth classification. The stent is inserted into the anterior hepatic duct. Each DLV is calculated as the volume of the yellow area in Bismuth classifications IIIa (c1) and IIIb (c2)
Outcome
Using 3D volumetry, we calculated the total liver volume, liver volume of each segment, including the anterior and posterior segments of the right liver and lateral and medial segments of the left liver, and DLV by the biliary stents. To validate the accuracy of the DLV calculation, we assessed the association between the calculated DLV and outcome of biliary drainage. The patients were divided into the following two groups according to the calculated DLV, DLV < 50% and DLV ≥ 50% groups. The clinical success rate, rate of recurrence of biliary obstruction (RBO), time to RBO (TRBO), survival time, and adverse event rate were compared between the two groups. Outcomes were defined as follows according to Tokyo criteria 2014 [17]. Clinical success was defied as cases in which total bilirubin was reduced or normalized by 50% or more within 2 weeks after drainage, RBO as stent occlusion or migration, TRBO as period between drainage and RBO, the patient who had died without RBO were treated as censored cases, and survival time as the time from drainage to death.
Statistical Analysis
The χ2 test or Fisher’s exact test of the contingency table was used for univariate analysis of the categorical data, and for quantitative data, the Student’s t-test was used. Statistical analyses for TRBO and overall survival were performed by using the Kaplan–Meier method with log-rank test. We considered a P value of < 0.05 to be significant.
Results
Patient Characteristics
Among the 164 patients who underwent biliary drainage for UMHBO during the study period, 56 were classified as Bismuth type I or II and 4 patients underwent biliary drainage prophylactically. Excluding these patients, 104 patients who fulfilled the study criteria were included in the final analysis. The patient characteristics are shown in Table 1. Median age of the patients was 75 years (range, 44–92), and the patients comprised 70 men and 34 women. The etiologies included cholangiocarcinoma in 67 patients (64%), hepatocellular carcinoma in 13 patients (13%), gallbladder carcinoma in 8 patients (7%), lymph node metastasis in 2 patients (2%), and metastatic liver carcinoma in 14 patients (24%). According to the Bismuth classification, 37 patients (37%) were classified as type IIIa, 10 (9%) as type IIIb, and 57 (55%) as type IV. Furthermore, 7 patients had bile duct deviations. Regarding to the drainage procedure, endoscopic biliary stenting (plastic stent/ self-expanded metallic stent), endoscopic nasobiliary drainage, and percutaneous transhepatic biliary drainage were performed in 98 (46/52), 6, and 6 patients, respectively.
Calculation of Total Liver Volume and Drained Liver Volume
We first calculated the total liver volume and DLV of 104 patients using 3D volumetry. A representative case of unresectable hilar cholangiocarcinoma with Bismuth classification type IIIa is shown in Fig. 2. Endoscopic retrograde cholangiopancreatography (ERCP) was performed to treat obstructive jaundice, and uncovered self-expandable metallic stents (UC-SEMSs) were successfully placed in the right anterior bile duct and left lateral bile duct by stent in stent method. We manually traced the bile ducts displayed on the enhanced CT images (axial view), and reconstructed the 3D images of bile ducts and liver parenchyma (Fig. 2b). Then, we measured the total liver volume and DLV according to bile duct distribution, in which stents placed and Bismuth classification automatically using 3D volume analyzer. The total liver volume was 1395 ml. The volumes of anterior, posterior, medial, and lateral segment of liver were 555 ml (40%), 388 ml (28%), 151 ml (11%), 297 ml (21%), respectively (Fig. 2c). According to distribution of bile ducts in which stents placed and Bismuth classification, the drained liver areas were anterior segment and left lobe, and DLV was calculated as 1003 ml (72%) (Fig. 2d).
Calculation of drained liver volume in patient with an unresectable hilar cholangiocarcinoma. (a) Biliary obstruction was caused by hilar cholangiocarcinoma, and the Bismuth classification was type IIIa. (b) Three-dimensional (3D) reconstruction of the bile duct and liver parenchyma based on CT images. (c) Liver volume was calculated automatically based on 3D reconstruction images by using a 3D volume analyzer. The total liver volume was 1395 ml, and volumes of each liver segments were calculated as follows: anterior segment (blue area) as 555 ml (40%), posterior segment (orange area) as 388 ml (28%), inferior segment (pink area) as 151 ml (11%), and lateral segment (green area) as 297 ml (21%). (d) According to stent placement and Bismuth classification, the drained liver areas were the anterior segment and left lobe (yellow area), and drained liver volume was calculated as 1003 ml (72%)
Using the abovementioned method, we calculated the total liver volume and DLV of 104 patients (Table 2). The mean total liver volume was 1320 ± 421 ml, and the mean volume of each segments was calculated as follows: anterior segment as 480 ± 223 ml (37%), posterior segment as 395 ± 197 ml (30%), inferior segment as 125 ± 86 ml (10%), and lateral segment as 317 ± 222 ml (23%), respectively. The mean DLV was 708 ± 393 ml (53 ± 21%), and 65 patients (63%) underwent drainage of ≥ 50% liver volume.
Drained Liver Volume and Drainage Outcome
Among the 104 patients, 65 patients (63%) underwent drainage of ≥50% of the liver volume (DLV ≥ 50% group), and 39 patients (37%) underwent drainage of < 50% of the liver volume (DLV < 50% group). The patient characteristics of 2 groups are shown in Table 3. There were no statistically significant differences in median age, gender, performance status (ECOG), rate of distant metastasis, and rate of portal vein involvement between 2 groups. The clinical success rate, rate of RBO, TRBO, survival time, and adverse event rate were compared between the 2 groups. The clinical success rate of patients with DLV ≥ 50% was significantly higher than that of patients with DLV < 50% (89% vs. 28%, P<0.001) (Fig. 3). There were no statistically significant differences in rate of RBO and adverse event rate between 2 groups (Table 4). However, the median TRBO was significantly longer in patients with DLV ≥ 50% than in patients with DLV < 50% [292 (95.0% CI, 186–439) days for DLV ≥ 50% and 119 (95.0% CI, 14–329) days for DLV < 50%]; (P = 0.03) (Fig. 4). Furthermore, the median survival time in patients with DLV ≥ 50% was also longer than that of patients with DLV < 50% (DLV ≥ 50% group, median 285 days [95.0% CI, 176–443]; DLV < 50% group, median 65 days [95.0% CI, 33–139]; P = 0.004, log-rank test) (Fig. 5). Thus, DLV calculated using 3D volumetry was significantly associated with the clinical success rate, TRBO, and survival time in patients with UMHBO.
Discussion
In this study, we developed a novel method to calculate DLV using a 3D volume analyzer (3D volumetry). This method comprises manual tracing of bile ducts on CT images, 3D reconstruction of bile ducts, and automatic calculation of DLV based on 3D images. Using this method, the liver volume can be calculated according to the bile duct distribution, allowing accurate measurement of the liver volume drained by the biliary stent. Furthermore, we assessed the usefulness of DLV calculated by this method for drainage in patients with UMHBO. In patients who underwent drainage of ≥ 50% liver volume calculated by 3D volumetry, the clinical success rate was better, and TRBO and survival time were longer than those of patients who underwent drainage of < 50% liver volume.
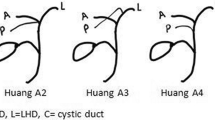
Over the past years, a number of studies concerning the drainage route, the drainage area, the number, size, and material of the stents for drainage in patients with UMHBO have been reported [18,19,20,21,22,23,24,25,26,27]. In particular, several studies have evaluated the drainage area: whether unilateral or bilateral stenting is better [18, 28,29,30]. In those studies, two studies have focused on the importance of liver volume to be drained by biliary stents [10, 11]. Takahashi et al. reported that liver volume drainage of ≥ 33% in patients with preserved liver function and liver volume drainage of ≥ 50% in patients with impaired liver function correlated with better clinical success rate of drainage for UMHBO [10]. Vinnie et al. reported that liver volume drainage of ≥ 50% was associated with better clinical success rate and longer survival time in patients with UMHBO [11]. These studies have shown that DLV is the most important parameter to ensure effective drainage in patients with UMHBO. In these studies, CT volumetry was shown as a method for measuring DLV. However, CT volumetry has two limitations. First, this method measures the volume of the hepatic segment delimited by the liver vein and portal vein, not the bile duct, which may cause a mismatch with the actual liver volume to be drained from the bile duct. Particularly, in cases with bile duct deviations, such as the right posterior branch connecting to the left hepatic duct, CT volumetry cannot accurately measure the DLV. Second, CT volumetry consists of all manual steps. In CT volumetry, DLV is calculated as the summed areas of each section manually traced based on CT images. This step takes a lot of time and could be subjective and lacking in reproducibility.
In the present study, we developed a novel method, 3D volumetry, using a 3D volume analyzer. This method can calculate each liver volume according to the distribution of bile ducts and DLV is calculated semi-automatically just by manually tracing the bile ducts. In clinical practice, the method of stenting (bile duct branches to be drained, number of stents) is based on the subjective judgment of the operator and therefore varies from institution to institution. Using the 3D volumetry method developed in this study, the optimal stenting method can be selected at any institution based on evidence. This allows for safe and effective drainage methods to be selected even in institution without specialists. Furthermore, a fully automatic system is expected to be built by applying 3D volumetry and artificial intelligence technology in the future.
In patients with UMHBO, frequent cholangitis and RBO after stents placement can be fatal. Thus, effective drainage and long-term TRBO are important for prolonged survival time. Furthermore, biliary drainage in UMHBO patients receiving chemotherapy is particularly important. Proper drainage contributes to a prolonged prognosis by allowing chemotherapy to continue without interruption due to cholangitis. Previous studies and guidelines had suggested the importance of the drainage strategy based on DLV for effective drainage in patients with UMHBO [10,11,12]. In this study, we showed that DLV of ≥ 50% calculated by 3D volumetry was associated with better clinical success and longer TRBO and survival time. This result confirmed the importance of the drainage strategy based on DLV in patients with UMHBO. According to the result of this study, the drainage strategy based on DLV, which aims to drain ≥ 50% of liver volume is optimal strategy, and 3D volumetry is considered to be an appropriate method for measuring DLV and for deciding the drainage area in patients with UMHBO. Furthermore, to ensure effective drainage, follow-up CT scan after stents placement is useful to evaluate whether the area anticipated by stent placement has been drained. In particular, in the situation that drainage is not effective after stents placement, follow-up CT scan enables to determine areas where additional stents should be placed.
Our study has 2 limitations. First, because it was retrospective study, the drainage procedures were not uniformed. The drainage procedures were chosen according to patient’s condition of diseases, which might have led to bias. Second, the patients were recruited from a single center; thus, the sample size was small. Further studies are needed to determine the usefulness of this method.
In conclusion, this study provides a novel method for calculating DLV accurately according to the bile duct distribution in patients with UMHBO. Selecting the appropriate drainage area using this method before biliary drainage is important.
References
Kerdsirichairat, T., et al., Endoscopic Drainage of > 50% of Liver in Malignant Hilar Biliary Obstruction Using Metallic or Fenestrated Plastic Stents. Clin Transl Gastroenterol, 2017. 8(8): p. e115.
Mukai, T., et al., Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J Hepatobiliary Pancreat Sci, 2013. 20(2): p. 214–22.
Kanno, Y., et al., Inside Plastic Stents versus Metal Stents for Treating Unresectable Malignant Perihilar Biliary Obstructions: A Retrospective Comparative Study. Clin Endosc, 2020. 53(6): p. 735–742.
Lee, T.H., et al., Prospective comparison of endoscopic bilateral stent-in-stent versus stent-by-stent deployment for inoperable advanced malignant hilar biliary stricture. Gastrointest Endosc, 2019. 90(2): p. 222–230.
de Souza, G.M.V., et al., Endoscopic retrograde cholangiopancreatography drainage for palliation of malignant hilar biliary obstruction - stent-in-stent or side-by-side? A systematic review and meta-analysis. World J Hepatol, 2021. 13(5): p. 595–610.
Kurita, A., et al., Stent placement above the sphincter of Oddi is a useful option for patients with inoperable malignant hilar biliary obstruction. Surg Endosc, 2022. 36(5): p. 2869–2878.
Kitamura, K., et al., Endoscopic side-by-side uncovered self-expandable metal stent placement for malignant hilar biliary obstruction. Ther Adv Gastrointest Endosc, 2019. 12: p. 2631774519846345.
Sundaram, S. and V. Dhir, EUS-guided biliary drainage for malignant hilar biliary obstruction: A concise review. Endosc Ultrasound, 2021. 10(3): p. 154–160.
Nakai, Y., et al., Endoscopic Ultrasound-Guided Biliary Drainage for Unresectable Hilar Malignant Biliary Obstruction. Clin Endosc, 2019. 52(3): p. 220–225.
Takahashi, E., et al., Biliary drainage strategy of unresectable malignant hilar strictures by computed tomography volumetry. World J Gastroenterol, 2015. 21(16): p. 4946–53.
Vienne, A., et al., Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc, 2010. 72(4): p. 728–35.
Dumonceau, J.M., et al., Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy, 2018. 50(9): p. 910–930.
Shimoda, M., et al., Development of new software enabling automatic identification of the optimal anatomical liver resectable region, incorporating preoperative liver function. Oncol Lett, 2019. 18(6): p. 6639–6647.
Kudo, M., et al., Evaluation of liver function using gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid enhanced magnetic resonance imaging based on a three-dimensional volumetric analysis system. Hepatol Int, 2018. 12(4): p. 368–376.
Ohshima, S., Volume analyzer SYNAPSE VINCENT for liver analysis. J Hepatobiliary Pancreat Sci, 2014. 21(4): p. 235–8.
Yasukawa, K., et al., Innovative formulae for the estimation of standard liver volume in the era of widespread imaging analysis software. Clin Transplant, 2023. 37(6): p. e14976.
Isayama, H., et al., TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc, 2015. 27(2): p. 259–64.
Lee, T.H., et al., Bilateral versus unilateral placement of metal stents for inoperable high-grade malignant hilar biliary strictures: a multicenter, prospective, randomized study (with video). Gastrointest Endosc, 2017. 86(5): p. 817–827.
Xia, M.X., et al., Comparison of endoscopic bilateral metal stent drainage with plastic stents in the palliation of unresectable hilar biliary malignant strictures: Large multicenter study. Dig Endosc, 2021. 33(1): p. 179–189.
Fukasawa, M., et al., Endoscopic biliary stenting for unresectable malignant hilar obstruction. Clin J Gastroenterol, 2017. 10(6): p. 485–490.
Zhou, W.Z., et al., Percutaneous stent placement for malignant hilar biliary obstruction: side-by-side versus stent-in-stent technique. BMC Gastroenterol, 2020. 20(1): p. 174.
Van Eecke, E., et al., Outcome of primary ERCP versus primary PTC for biliary drainage in malignant hilar biliary strictures: a systematic review and meta-analysis. Surg Endosc, 2022. 36(10): p. 7160–7170.
Kim, J.Y., et al., The Comparison of Endoscopic Biliary Drainage in Malignant Hilar Obstruction by Cholangiocarcinoma: Bilateral Metal Stents versus Multiple Plastic Stents. Gut Liver, 2021. 15(6): p. 922–929.
Jha, A.K., et al., Plastic versus metal stents for inoperable gallbladder cancer with hilar biliary obstruction: the jury is still out. Ann Gastroenterol, 2021. 34(1): p. 12–19.
Naitoh, I., et al., Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci, 2012. 57(12): p. 3279–85.
Ishigaki, K., et al., Retrospective Comparative Study of Side-by-Side and Stent-in-Stent Metal Stent Placement for Hilar Malignant Biliary Obstruction. Dig Dis Sci, 2020. 65(12): p. 3710–3718.
Cao, Q., et al., Bilateral stenting for hilar biliary obstruction: a meta-analysis of side-by-side versus stent-in-stent. Minim Invasive Ther Allied Technol, 2022. 31(4): p. 525–530.
Ashat, M., et al., Bilateral vs unilateral placement of metal stents for inoperable high-grade hilar biliary strictures: A systemic review and meta-analysis. World J Gastroenterol, 2019. 25(34): p. 5210–5219.
Hakuta, R., et al., Unilateral versus Bilateral Endoscopic Nasobiliary Drainage and Subsequent Metal Stent Placement for Unresectable Malignant Hilar Obstruction: A Multicenter Randomized Controlled Trial. J Clin Med, 2021. 10(2).
Chang, G., et al., Unilateral versus bilateral stent insertion for malignant hilar biliary obstruction. Abdom Radiol (NY), 2017. 42(11): p. 2745–2751.
Acknowledgments
None.
Funding
None.
Open Access funding provided by University of Yamanashi.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Imagawa, N., Fukasawa, M., Takano, S. et al. A Novel Method of Calculating the Drained Liver Volume Using a 3D Volume Analyzer for Biliary Drainage of Unresectable Malignant Hilar Biliary Obstruction. Dig Dis Sci 69, 969–977 (2024). https://doi.org/10.1007/s10620-024-08294-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08294-z