Abstract
Background
As recommendations for non-invasive fibrosis risk assessment in nonalcoholic fatty liver disease (NAFLD) emerge, it is not known how often they are performed in primary care.
Aims
We investigated the completion of confirmatory fibrosis risk assessment in primary care patients with NAFLD and indeterminate-risk or greater Fibrosis-4 Index (FIB-4) and NAFLD Fibrosis Scores (NFS).
Methods
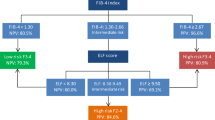
This retrospective cohort study of electronic health record data from a primary care clinic identified patients with diagnoses of NAFLD from 2012 through 2021. Patients with a diagnosis of a severe liver disease outcome during the study period were excluded. The most recent FIB-4 and NFS scores were calculated and categorized by advanced fibrosis risk. Charts were reviewed to identify the outcome of a confirmatory fibrosis risk assessment by liver elastography or liver biopsy for all patients with indeterminate-risk or higher FIB-4 (≥ 1.3) and NFS (≥ − 1.455) scores.
Results
The cohort included 604 patients diagnosed with NAFLD. Two-thirds of included patients (399) had a FIB-4 or NFS score greater than low-risk, 19% (113) had a high-risk FIB-4 (≥ 2.67) or NFS (≥ 0.676) score, and 7% (44) had high-risk FIB-4 and NFS values. Of these 399 patients with an indication for a confirmatory fibrosis test, 10% (41) underwent liver elastography (24) or liver biopsy (18) or both (1).
Conclusions
Advanced fibrosis is a key indicator of future poor health outcomes in patients with NAFLD and a critical signal for referral to hepatology. Significant opportunities exist to improve confirmatory fibrosis risk assessment in patients with NAFLD.

Similar content being viewed by others

Data availability
The study protocol and individual participant data contributing to these reported results reported in this article will be made available to investigators whose proposed use of the data have been approved by an independent review committee. Data will only be made available after de-identification (text, tables, figures, and appendices) and compliance with the Health Insurance Portability and Accountability Act of 1996 and the Institutional Review Board at MUSC is assured.
References
Harrison SA, Gawrieh S, Roberts K et al. Prospective evaluation of the prevalence of non-alcoholic fatty liver disease and steatohepatitis in a large middle-aged US cohort. J Hepatol 2021;75:284–291.
Younossi ZM, Stepanova M, Younossi Y et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut 2020;69:564–568.
Lomonaco R, Godinez Leiva E, Bril F et al. Advanced Liver Fibrosis Is Common in Patients With Type 2 Diabetes Followed in the Outpatient Setting: The Need for Systematic Screening. Diabetes Care 2021;44:399–406.
Ciardullo S, Monti T, Perseghin G. High Prevalence of Advanced Liver Fibrosis Assessed by Transient Elastography Among U.S. Adults With Type 2 Diabetes. Diabetes Care 2020;44:519–25.
Williamson RM, Price JF, Glancy S et al. Prevalence of and risk factors for hepatic steatosis and nonalcoholic Fatty liver disease in people with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetes Care 2011;34:1139–1144.
Targher G, Bertolini L, Padovani R et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care 2007;30:1212–1218.
Rinella ME. Nonalcoholic fatty liver disease: a systematic review. Jama. 2015;313:2263–2273.
Moon AM, Singal AG, Tapper EB. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin Gastroenterol Hepatol. 2020;18:2650–2666.
Noureddin M, Vipani A, Bresee C et al. NASH Leading Cause of Liver Transplant in Women: Updated Analysis of Indications For Liver Transplant and Ethnic and Gender Variances. Am J Gastroenterol. 2018;113:1649–1659.
Le MH, Yeo YH, Li X et al. 2019 Global NAFLD prevalence: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2022;20:2809–2817.e28.
Estes C, Razavi H, Loomba R et al. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology 2018;67:123–133.
Ward ZJ, Bleich SN, Cradock AL et al. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. New England Journal of Medicine 2019;381:2440–50.
Loomba R, Wong R, Fraysse J et al. Nonalcoholic fatty liver disease progression rates to cirrhosis and progression of cirrhosis to decompensation and mortality: a real world analysis of Medicare data. Aliment Pharmacol Ther. 2020;51:1149–1159.
Hagstrom H, Nasr P, Ekstedt M et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol 2017;67:1265–1273.
Sanyal AJ, Van Natta ML, Clark J et al. Prospective Study of Outcomes in Adults with Nonalcoholic Fatty Liver Disease. N Engl J Med 2021;385:1559–1569.
Dulai PS, Singh S, Patel J et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: Systematic review and meta-analysis. Hepatology 2017;65:1557–1565.
Ekstedt M, Hagström H, Nasr P et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 2015;61:1547–1554.
Taylor RS, Taylor RJ, Bayliss S et al. Association Between Fibrosis Stage and Outcomes of Patients With Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. Gastroenterology 2020;158:1611–25 e12.
Angulo P, Kleiner DE, Dam-Larsen S et al. Liver Fibrosis, but No Other Histologic Features, Is Associated With Long-term Outcomes of Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology 2015;149:389–9710.
Kanwal F, Shubrook JH, Younossi Z et al. Preparing for the NASH epidemic: a call to action. Diabetes Care. 2021;44:2162–2172.
Wong VWS, Zelber-Sagi S, Cusi K et al. Management of NAFLD in primary care settings. Liver international: official journal of the International Association for the Study of the Live. 2022;42:2377–2389.
Kanwal F, Shubrook JH, Adams LA et al. Clinical Care Pathway for the Risk Stratification and Management of Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology 2021;161:1657–1669.
Rinella ME, Neuschwander-Tetri BA, Siddiqui MS et al. AASLD practice guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology (Baltimore, Md). 2023;77:1797–1835.
Angulo P, Hui JM, Marchesini G et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology (Baltimore, Md). 2007;45:846–854.
Vallet-Pichard A, Mallet V, Nalpas B et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology (Baltimore, Md) 2007;46:32–6.
Islam KB, Brandman D, Chu JN et al. Primary care providers and nonalcoholic fatty liver disease: a needs assessment survey. Dig Dis Sci. 2022;68:434–438.
Saeed N, Glass LM, Habbal H et al. Primary care and referring physician perspectives on non-alcoholic fatty liver disease management: a nationwide survey. Therapeutic advances in gastroenterology 2021;14:17562848211042200.
European Association for the Study of the Liver. Easl Clinical practice guidelines (Cpgs) on non-invasive tests For evaluation of liver disease severity and prognosis- 2020 Update. J. Hepatol. 2021;75:659–689.
Schreiner AD LS, Zhang J, Gebregziabher M, Marsden J, Koch DG, Petz CA, Durkalski-Mauldin V, Mauldin PD, Moran WP. Identifying Patients at Risk for Fibrosis in a Primary Care NAFLD Cohort. Journal of clinical gastronenterology. 2021.
Davyduke T, Tandon P, Al-Karaghouli M et al. Impact of Implementing a “FIB-4 First” Strategy on a Pathway for Patients With NAFLD Referred From Primary Care. Hepatol Commun. 2019;3:1322–1333.
Srivastava A, Gailer R, Tanwar S et al. Prospective evaluation of a primary care referral pathway for patients with non-alcoholic fatty liver disease. J Hepatol. 2019;71:371–378.
Schreiner AD, Livingston S, Zhang J et al. Identifying patients at risk for fibrosis in a primary care NAFLD cohort. J. Clin. Gastroenterol. 2023;57:89–96.
Schreiner AD, Zhang J, Durkalski-Mauldin V et al. Advanced liver fibrosis and the metabolic syndrome in a primary care setting. Diabetes Metab Res Rev 2021;37:e3452.
Hagström H, Adams LA, Allen AM et al. Administrative Coding in Electronic Health Care Record-Based Research of NAFLD: An Expert Panel Consensus Statement. Hepatology (Baltimore, Md) 2021;74:474–482.
Sterling RK, Lissen E, Clumeck N et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology (Baltimore, Md) 2006;43:1317–1325.
Nehra MS, Ma Y, Clark C et al. Use of administrative claims data for identifying patients with cirrhosis. Journal of clinical gastroenterology 2013;47:e50–e54.
Mapakshi S, Kramer JR, Richardson P, El-Serag HB, Kanwal F. Positive Predictive Value of International Classification of Diseases, 10th Revision, Codes for Cirrhosis and Its Related Complications. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2018;16:1677–1678.
Shah AG, Lydecker A, Murray K et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2009;7:1104–1112.
Sterling R, Patel K, Asrani S et al. Executive summary: non-invasive liver disease assessments (NILDA) of hepatic fibrosis, steatosis, and portal hypertension: 2021 practice guidelines and guidance from the American association for the study of liver diseases. The Liver Meeting; Anaheim, CA: AASLD; 2021 Nov 12.
Quan H, Li B, Saunders LD et al. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res 2008;43:1424–1441.
Quan H, Sundararajan V, Halfon P et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139.
Alexander M, Loomis AK, Fairburn-Beech J et al. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med 2018;16:130.
Nielsen EM, Anderson KP, Marsden J, Zhang J, Schreiner AD. Nonalcoholic fatty liver disease underdiagnosis in primary care: what are we missing? J. Gen. Intern. Med. 2022;37:2587–2590.
Funding
Effort and time for this study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIH/NIDDK K23DK118200 PI: Schreiner; R03DK129558 PI: Schreiner; P30DK123704 PI: Rockey). This project is also supported in part by the SSCI Research Scholar Award. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Southern Society for Clinical Investigation (SSCI). This project was also supported by the South Carolina Clinical & Translational Research Institute with an academic home at the Medical University of South Carolina CTSA National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) under UL1 TR001450.
Author information
Authors and Affiliations
Contributions
All contributors to this work appear in the author byline. All named authors contributed to the study design, data interpretation, manuscript editing, and submission decision. Dr. ADS and Ms. JZ led the writing of the original draft, and Ms. JZ performed the analyses. Ms. JZ, Mr. JM, and Dr. ADS performed the data collection.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflicts of interest with this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moore, J.A., Wheless, W.H., Zhang, J. et al. Gaps in Confirmatory Fibrosis Risk Assessment in Primary Care Patients with Nonalcoholic Fatty Liver Disease. Dig Dis Sci 68, 2946–2953 (2023). https://doi.org/10.1007/s10620-023-07959-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07959-5